Abstract
The aim of this study was to evaluate the clinical performance of a magnesium-enriched hydroxyapatite biomaterial used as bone substitute in a case of mandibular ameloblastoma treated with conservative surgery. A 63 year old male patient was treated for an ameloblastoma in the anterior mandibular profile. After tissue excision, the bone defect was filled with a synthetic hydroxyapatite biomaterial enriched with magnesium ions, in order to promote bone tissue regeneration and obtain a good aesthetic result. Twenty-five months after surgery, due to ameloblastoma recurrence in an area adjacent to the previously treated one, the patient underwent to a further surgery. In that occasion the surgeon performed a biopsy in the initially treated area, in order to investigate the nature of the newly-formed tissue and to evaluate the bone regenerative potential of this biomaterial by clinical, radiographic and histological analyses. The clinical, radiographic and histological evaluations showed various characteristics of bone remodeling stage with an ongoing osteogenic formation and a good osteo-integration. In conclusion, magnesium-enriched hydroxyapatite used as bone substitute in a mandibular defect due to ameloblastoma excision showed an effective bone regeneration at 25 months follow-up, demonstrating an excellent biocompatibility and a high osteo-integration property.
Keywords: Bone substitute, bone tissue regeneration, magnesium-enriched hydroxyapatite
Introduction
The jaws are host to a wide variety of large cysts and locally invasive benign tumours, such as ameloblastoma, giant cell granuloma, odontogenic keratocyst and odontogenic myxoma, due in large part to the tissue involved in teeth formation and affecting mostly the mandible [1,2].
The current preferred treatment of large cysts and similar lesions consists in enucleation, the so-called “cystectomy”, with watertight of primary closure. On the other hand, the management of ameloblastoma depends on its invasiveness into the surrounding bone, and may require a compromise between a conservative treatment and an enough radical excision in order to prevent recurrences [3,4].
Despite its benign nature, ameloblastoma is a clinically aggressive tumor with a significant recurrence rate, ranging between 4.5% and 70-85% after en bloc resection or conservative therapy respectively, over periods ranging from 5 to 15 years [2,3].
The enucleation of the tumoral lesions and curettage represents a therapeutic strategy used in patients affected by ameloblastoma to avoid more invasive treatments with following reconstructive phases. Special care is required in young patients in growing phases, in which an interruption in growth and development could interfere with future function and aesthetics, and in elderly patients, particularly in case of co-morbidities [5].
As for large cysts, primary closure without addition of bone substitutes remains the “state of the art” in most cases of ameloblastoma management; several studies reported extensive ossification of defects up to 3 cm in diameter 12 months after excision, and almost complete bone healing of defects exceeding 4 cm in diameter at 24 months follow-up [6,7].
It is well known as spontaneous bone healing occurs even in patients with very large bone defects of the mandible, closely dependent by various parameters as the size of the defects, the anatomical location, the patient’s age and time of rehabilitation [7].
However, in case of large and complex lesions, a bone substitute may accelerate the new bone formation and prevent soft tissue collapse, favoring a better aesthetic and functional Outcome [6].
Autologous bone is still considered the “gold standard” in bone defect repair even though the several drawbacks, as sophisticated surgical techniques, second surgical exposure or longer surgical time, limited supply and shapes, morbidity of the donor site and increased blood loss [8-10].
The study and design of innovative biomimetic materials for filling the surgical defects is an interesting area of research in bone tissue engineering which should take into account the patients’ characteristics, the size and the shape of the surgical defects [6].
Among the wide variety of alternative available biomaterials, synthetic calcium phosphate (CaP) ceramics became widely used in several clinical applications [8,11-18], due to their ability to mimic the human bone composition and architecture, and to induce mesenchymal stem cells differentiation toward osteoblasts [13,19-20].
Tricalcium phosphate and hydroxyapatite (HA) are commonly used as osteo-conductive materials after cyst enucleation to stabilize the blood clot in the defect avoiding infections and promote bone regeneration through an enhanced migration of osteo-progenitor cells. Furthermore superior biomechanical properties should provide early implantation [6,21,22].
HA is a mineral constituent of the human bone present in percentages ranging between 65% and 80%. Moreover, magnesium (Mg2+) is naturally present in the composition of biological apatite and it is extremely important for the maintenance of HA non-stoichiometric crystal structure, with a critical role in modulating bone resorption and remodeling [20]. Indeed, Mg2+ ions into the apatite crystals may contribute to the acceleration of osteoblast adhesion onto bioceramic matrices, to the promotion of extracellular matrix synthesis and deposition, and to the molecular cross-talk between progenitor cells and osteoblasts [23].
The present case report describes the clinical, radiographic and histological aspects of a synthetic HA biomaterial, enriched with Mg2+ ions, used as bone filler after an ameloblastoma enucleation.
Case report
On March 2009, a 63 year old male patient was treated for an anterior mandibular profile excision due to an ameloblastoma at San Camillo Hospital (Milan, Italy). Due to the clinical condition of the patient and his refusal to mandible resection, a conservative treatment was preferred, and after excision and curettage the bone defect was filled with a synthetic CaP ceramic, made of HA enriched with Mg2+ ions (SINTlife® putty, Fin-Ceramica Faenza S.p.A, Faenza, Italy) in order to support the bone tissue regeneration. SINTlife® putty is a biomimetic nano-crystalline non-stoichiometric magnesium-HA (Mg-HA) bone substitute, doped with Mg2+ ions introduced in a similar amount as physiologically found in human bones. The putty format is a highly moldable mixture of nano-structured powder and granules (diameter 450÷900 μm) enriched with magnesium in phosphate buffered saline (PBS), to be used for regeneration of bone defects resulting from trauma, degenerative pathologies or surgical removals. Twenty-five months later, on April 2011, the patient came back to the same hospital for a recurrence adjacent to the previously treated area, requiring a further resection. The defect was then filled with the same bone substitute. In this circumstance, with the patient’s informed consent, the surgeon performed a biopsy of the newly-formed tissue in the area initially treated, in order to investigate histological and immunohistochemical quality of the repaired tissue and to evaluate the ability of the biomaterial to regenerate the bone defect. Patient’s clinical analysis takes into account intra and extra-oral examinations at the time of ameloblastoma recurrence. Further analyses by panoramic X-ray and CT scan were carried out. In both surgical interventions surgeons removed integrally the lesions, cutting the mucosa and performing an accurate curettage of the bone defect after the excision of the pathological tissue. In the second surgery, a sample of the previously treated and regenerated area was taken, immediately stored in 10% neutral buffered formalin, washed and decalcified with a 4% (v/v) HCl and 5% (v/v) formic acid solution at Room Temperature (RT) for about five days. The sample was then dehydrated through a graded series of alcohol and embedded in paraffin. Serial sections were cut at up to 5 μm thickness (microtome HM 340E, Zeiss) and stained with Haematoxylin/Eosin to evaluate general morphology. Mallory Trichrome staining was performed to evaluate bone tissue formation. Immunohistochemical analyses were carried out on the bioptic sample to evaluate typical osteogenic markers: collagen I, alkaline phosphatase and osteocalcin. Negative controls were performed either by omitting the primary antibody (for all the antibodies tested) or using an isotype-matched control. Slices were counterstained with Haematoxylin and mounted in glycerol gel. All the samples were analyzed with Eclipse 90i. As concern clinical results, mild painless asymmetry of the face, with a slight swelling in the chin region extending from right up to left canine was observed. The edges were not clearly defined, but the swelling was hard in consistency with a smooth surface. Skin and oral mucosa that covered the interested area were normal. Intra-oral examination revealed swelling of the mouth vestibule and high tooth mobility, with presence of intercalated edentulous areas. Pre-operative CT scan performed before the ameloblastoma recurrence treatment (Figure 1) showed a multi-locular radiolucent area, extended from right up to left canine, representing the focal erosion of buccal cortical bone underwent to the first excision and filled with the Mg-HA biomaterial. Clinical evidence (Figure 2), panoramic X-ray and CT scan (Figure 3) performed before the ameloblastoma recurrence treatment, showed good bone regeneration and adequate volume preservation in the previously treated area filled with the bone substitute (Figure 3, black arrows). Right next to this, a first new osteolytic area with irregular and fringed edges determined roots spreading apart, partial erosion and buccal fenestration (Figure 3, upper red arrows). Moreover, a second osteolytic lesion with irregular edges, particularly at the vestibular profile, and with a thinned discontinued cortical perimeter was detected (Figure 3, lower red arrows).
Figure 1.
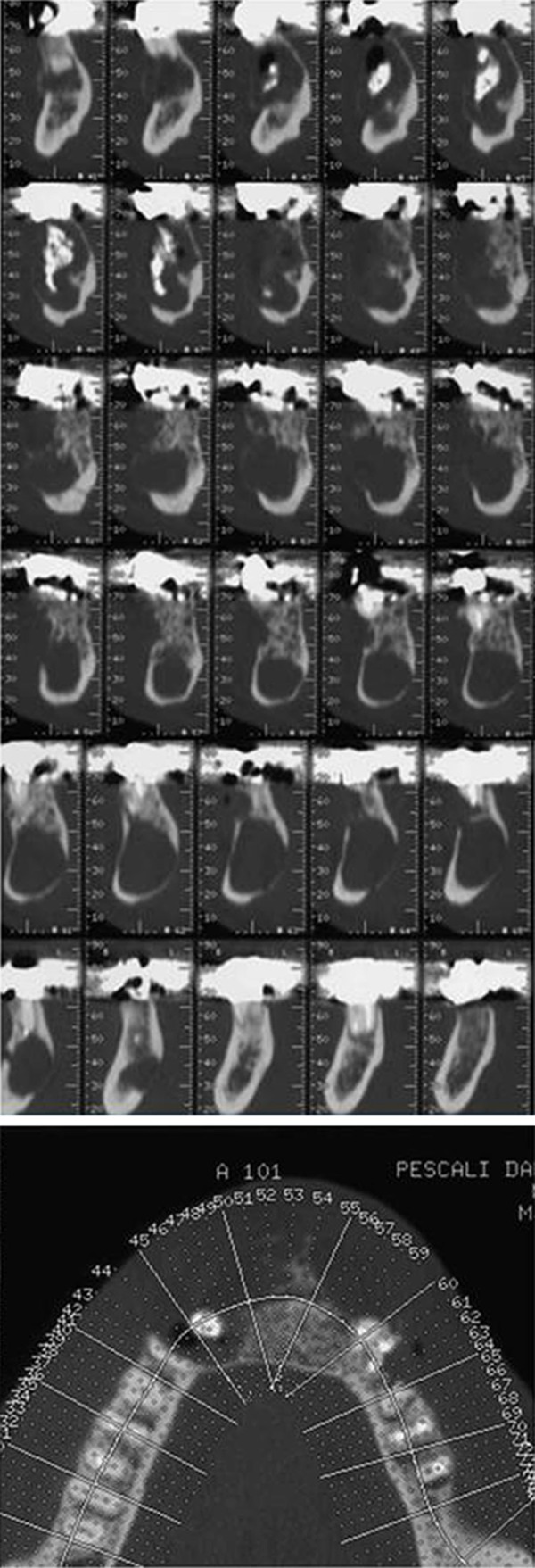
Preoperative CT scan showing the large defect of the anterior mandibular profile with focal erosion of the cortical bone (radiolucent area) underwent to excision on March 2009 and then filled with SINTlife putty.
Figure 2.
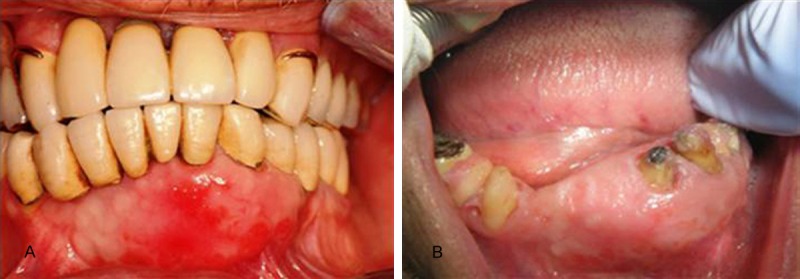
Clinical evidence of the ameloblastoma recurrence before the treatment performed on April 2011, showing good bone regeneration and adequate volume preservation; A. Patient with prosthesis; B. Patient without prosthesis.
Figure 3.
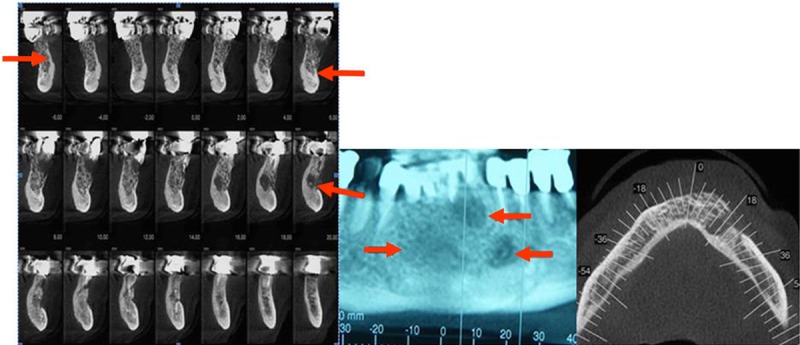
X-ray and CT scan performed before the recurrence treatment showing the outcome of the previous bone grafting (black arrow), with a trabecular aspect and an exophytic profile in the region of 33; the multi-locular radiolucency highlighted the new osteolytic areas due to ameloblastoma recurrence (red arrows).
From the histological report resulted partially cystic fibrous tissue with inflammatory infiltrates in the soft peri-dental tissue of 32/33 and on the apical region of 34. The satisfactory clinical outcome of the second surgery and filling with the same biomaterial was evident in the X-ray performed 18 months after the second treatment, on November 2012 (Figure 4) indicating an excellent behavior of the used material in terms of biocompatibility, with absence of adverse event, inflammation reaction or tissue hypertrophy. Histological analysis gave evidence of a bone remodeling process, showing mature and compact bone tissue close to small residues of unresorbed and not osteo-integrated synthetic bone substitute. Hematoxylin/Eosin staining (Figure 5A) revealed the presence of a bone substitute well integrated in the host bone tissue. Mallory Trichrome staining showed the presence of bone neoformation (orange staining), collagen fibrils and residues of bone substitute (Figure 5B). Further analysis by immunohistochemistry confirmed the presence of a good bone tissue, reporting the typical features of bone component with positivity for the typical osteogenic markers. In particular, immunohistochemical analysis for type I collagen (Figure 6A) highlighted a strong positivity at cellular and extracellular matrix levels. A strong positivity was also evident for osteocalcin marker (Figure 6B) in particular at cellular level, whereas a slight positivity was recorded for alkaline phosphatase located at cellular level (Figure 6C). This slight positivity is in agreement with the presence of this protein in the precocious stage of bone remodeling. Overall, histological and immunohistochemical evaluations demonstrated a good bone tissue remodeling, due to the ongoing osteogenic process and to the osteo-integration of the bone substitute.
Figure 4.

X-ray performed 18 months after the ameloblastoma recurrence treatment showing a good healing of both areas filled with the same bone substitute.
Figure 5.
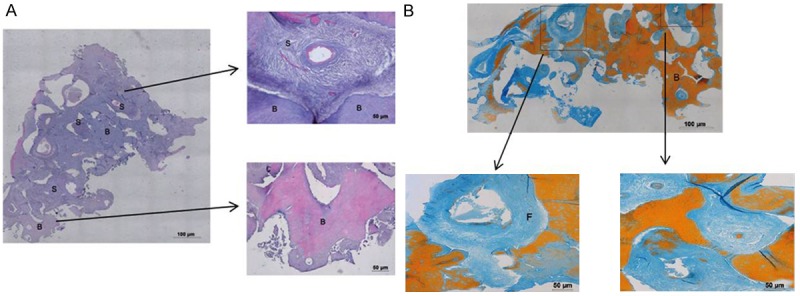
Haematoxylin-Eosin staining (5A) showing the presence of a bone substitute (S) well integrated in the host bone tissue (B); Trichrome Mallory staining (5B) showing the presence of newly formed bone tissue indicated by orange staining (B) and collagen fibrils (F) represented in blue.
Figure 6.
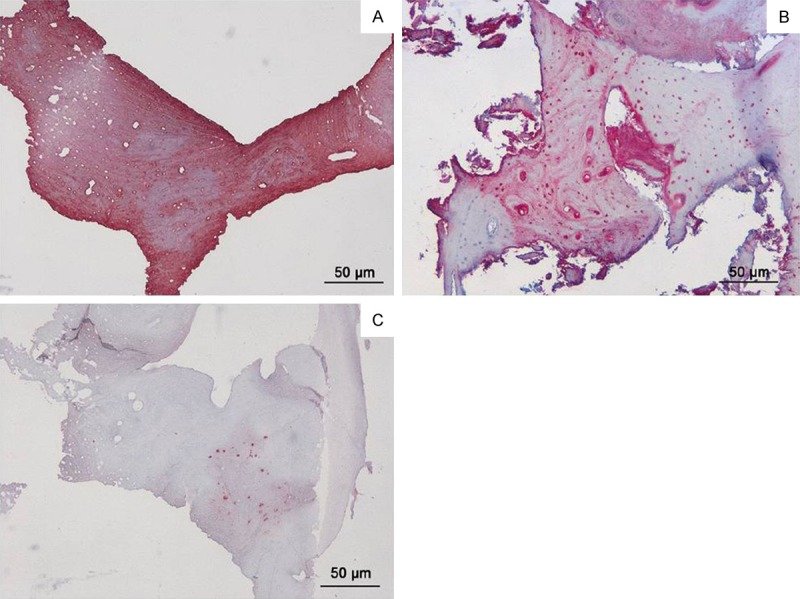
Immunohistochemical analysis for type I collagen (A) showing a strong positivity at cellular and extracellular matrix level; immunohistochemical analysis for osteocalcin (B) showing a strong positivity at cellular level in almost the entire thickness of the bone areas within biopsy; immunohistochemical analysis for alkaline phosphatase (C) showing a slight positivity at cellular level.
Discussion
Ameloblastoma is a locally invasive benign tumor of the jaws that predominantly affects the mandible [1]. Despite the benign nature of this lesion, there is a high rate of recurrence after curettage, which usually requires resection. Consequently, the adequate therapy of ameloblastoma may require a compromise between a less destructive treatment and a radical method to prevent recurrences [3,4].
The best treatment modality is still controversial, and management depends on the extent of tumor infiltration through the cyst wall and into the surrounding bone. However, it is widely accepted that a more conservative treatment results in the highest recurrence rate [3,4,10].
In our case, the patient’s clinical condition and his clear refusal to mandibular resection forced the surgeon to a conservative surgery. Unfortunately, but in agreement with literature data, the ameloblastoma recurred 25 months after surgery, thus a further surgery was necessary for an adequate control of the disease.
Primary closure without bone grafts addition represents the standard treatment in case of cyst and similar lesions such as ameloblastoma, even in defects with a diameter larger than 3 cm2. However, bone resorption poses a critical problem for clinicians both from aesthetic and surgical standpoint particularly after dental extraction; bone preservation is desirable, particularly in case of large lesions [24]. In our case report, the use of a bone substitute composed of HA enriched with magnesium provided an adequate bone volume preservation and satisfactory clinical, radiological and histological outcomes.
Among the wide variety of bone substitute currently used, autologous bone is still considered the “gold standard” in bone defect repair, even though the several drawbacks previously reported [8-10].
As alternative, a wide range of natural and synthetic biomaterials are currently used as bone substitutes, including HA and CaP compounds [9,12], and biomaterials research is ongoing to improve their mechanical properties, the biocompatibility, the osteoblast adhesion, the growth and differentiation in order to allow vascular ingrowth and bone tissue neo-formation.
One of the major challenging for clinicians is the discovery and development of novel bio-mimetic bone substitutes able to mimic the chemical, physical and structural properties of bone tissue [19]. The synthetic Mg2+-HA biomaterial used in our case report is already widely used as bone graft due to its ability to mimic the natural human bone composition and architecture and induce osteogenic differentiation of mesenchymal stem cells [16,17]. Moreover, the excellent biocompatibility together with its osteo-conductivity and osteo-integration properties render it an optimal candidate for several clinical applications [8,11-15,18].
Histological assessments can provide important information to clinicians regarding the healing potential of the employed graft materials. This could direct them to the choice of the most suitable bone substitute for specific therapeutic strategies.
Several preclinical and clinical studies on Mg2+-HA bone substitute were performed to fill extraction sockets and for sinus augmentation, providing in general good results [12,16,17,25,26]. In the current report, a bone substitute has been applied for a clinical application different from those previously reported in literature. In particular, we investigated the effectiveness of a Mg2+-HA bone substitute for the management of mandibular ameloblastoma.
The bone sample, harvested 25 months after the surgery in the first treated area, appeared firm in consistency, well incorporated and blood perfused, demonstrating its vitality. X-ray and CT scan evaluations confirmed the healing potential of this material showing the neo-formation of bone tissue with physical and biological aspects similar to natural bone.
Our clinical, radiographic and histological evaluations reported overall no inflammatory and adverse events and moreover showed bone tissue formation. The efficacy of this biomaterial, already used in other clinical settings, was confirmed also in this disease, observing a high expression of typical bone markers as collagen type I and osteocalcin, allowing in this way effective tissue regeneration inside the defect.
As concern the presence of small residues of unresorbed material noticed in the last follow-up, there is a lack of literature data about CaP based biomaterial degradation and rate of resorption, with few long-term studies and it is a topic of debate [27]. HA is generally believed to be unresorbable, even over periods of many years [8,27]. Therefore, it can be suitable for long-term restorative and conservative clinical procedures, such as repair of periodontal defects and augmentation of deficient alveolar ridges [27]. However, other authors consider ceramics as resorbable materials, but with different resorption rates according to their physical characteristics. It is well known, indeed, that the surface area affects the resorption rate of HA substitutes, and for this reason high-density ceramics, which possess smaller surface areas than porous ones, show a lower resorption rate, while HA sintered at a lower temperature and with a higher porosity tend to have bigger surfaces and so higher degradation rate [27]. We are aware of the inherent limitations of a case report. A further application of this approach on a cohort of patients in a randomized controlled study could provide more information on the use of this material in the same applications. Moreover, a biomolecular analysis of different osteogenic markers onto the biopsy sample would be useful to better define the potential of the biomaterial in the osteogenic processes. However, data obtained from this case report would support the healing potential of this Mg2+-HA bone substitute in dental practice for the management of mandibular ameloblastoma.
Acknowledgements
All authors would sincerely thank Dr. Luigi Costa, prematurely died, who treated the patient at San Camillo Hospital in Milan, and who contributed to the publication of this case report. Authors would like to remember him for his high professionality and deep sense of humanity.
Disclosure of conflict of interest
None.
References
- 1.Regezi JA. Odontogenic cysts, odontogenic tumors, fibro-osseous, and giant cell lesions of the jaws. Mod Pathol. 2002;15:331–341. doi: 10.1038/modpathol.3880527. [DOI] [PubMed] [Google Scholar]
- 2.Dandriyal R, Gupta A, Pant S, Baweja HH. Surgical management of ameloblastoma: Conservative or radical approach. Natl J Maxillofac Surg. 2011;2:22–27. doi: 10.4103/0975-5950.85849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan PR. Odontogenic tumors: a review. Periodontol 2000. 2011;57:160–176. doi: 10.1111/j.1600-0757.2011.00393.x. [DOI] [PubMed] [Google Scholar]
- 4.Ramesh RS, Manjunath S, Ustad TH, Pais S, Shivakumar K. Unicystic ameloblastoma of the mandible-an unusual case report and review of literature. Head Neck Oncol 2010; 14; 2:1. doi: 10.1186/1758-3284-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feinberg SE, Steinberg B. Surgical management of ameloblastoma. Current status of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:383–388. doi: 10.1016/s1079-2104(96)80012-6. [DOI] [PubMed] [Google Scholar]
- 6.Ettl T, Gosau M, Sader R, Reichert TE. Jaw cysts-filling or no filling after enucleation? A review. J Cranio-Maxillo-Fac Surg Off Publ Eur Assoc Cranio-Maxillo-Fac Surg. 2012;40:485–493. doi: 10.1016/j.jcms.2011.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Ihan Hren N, Miljavec M. Spontaneous bone healing of the large bone defects in the mandible. Int J Oral Maxillofac Surg. 2008;37:1111–1116. doi: 10.1016/j.ijom.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Dallari D, Savarino L, Albisinni U, Fornasari P, Ferruzzi A, Baldini N, Giannini S. A prospective, randomised, controlled trial using a Mg-hydroxyapatite - demineralized bone matrix nanocomposite in tibial osteotomy. Biomaterials. 2012;33:72–79. doi: 10.1016/j.biomaterials.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 9.Dimitriou R, Jones E, McGonagle D, Giannoudis PV. Bone regeneration: current concepts and future directions. BMC Med. 2011;9:66. doi: 10.1186/1741-7015-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dash H, Little JR, Zaino R, Colao DJ, Chaurushiya P, Schoolwerth AC, O’Neill MJ, Hart JC, Martin GB. Mandibular ameloblastoma treated by bone resection and immediate reconstruction. Braz J Otorhinolaryngol. 2008;74:155–157. doi: 10.1016/S1808-8694(15)30768-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crespi R, Capparè P, Addis A, Gherlone E. Injectable magnesium-enriched hydroxyapatite putty in peri-implant defects: a histomorphometric analysis in pigs. Int J Oral Maxillofac Implants. 2012;27:95–101. [PubMed] [Google Scholar]
- 12.Checchi V, Savarino L, Montevecchi M, Felice P, Checchi L. Clinical-radiographic and histological evaluation of two hydroxyapatites in human extraction sockets: a pilot study. Int J Oral Maxillofac Surg. 2011;40:526–532. doi: 10.1016/j.ijom.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Manfrini M, Di Bona C, Canella A, Lucarelli E, Pellati A, D’Agostino A, Barbanti-Bròdano G, Tognon M. Mesenchymal stem cells from patients to assay bone graft substitutes. J Cell Physiol. 2013;228:1229–1237. doi: 10.1002/jcp.24276. [DOI] [PubMed] [Google Scholar]
- 14.Martini L, Staffa G, Giavaresi G, Salamanna F, Parrilli A, Serchi E, Pressato D, Arcangeli E, Fini M. Long-term results following cranial hydroxyapatite prosthesis implantation in a large skull defect model. Plast Reconstr Surg. 2012;129:625e–35e. doi: 10.1097/PRS.0b013e318244220d. [DOI] [PubMed] [Google Scholar]
- 15.Rebaudi A, Maltono AA, Pretto M, Benedicenti S. Sinus grafting with magnesium-enriched bioceramic granules and autogenous bone: a microcomputed tomographic evaluation of 11 patients. Int J Periodontics Restorative Dent. 2010;30:53–61. [PubMed] [Google Scholar]
- 16.Crespi R, Capparè P, Gherlone E. Dental implants placed in extraction sites grafted with different bone substitutes: radiographic evaluation at 24 months. J Periodontol. 2009;80:1616–1621. doi: 10.1902/jop.2009.090156. [DOI] [PubMed] [Google Scholar]
- 17.Crespi R, Capparè P, Gherlone E. Magnesium-enriched hydroxyapatite compared to calcium sulfate in the healing of human extraction sockets: radiographic and histomorphometric evaluation at 3 months. J Periodontol. 2009;80:210–218. doi: 10.1902/jop.2009.080400. [DOI] [PubMed] [Google Scholar]
- 18.Pryor LS, Gage E, Langevin CJ, Herrera F, Breithaupt AD, Gordon CR, Afifi AM, Zins JE, Meltzer H, Gosman A, Cohen SR, Holmes R. Review of bone substitutes. Craniomaxillofacial Trauma Reconstr. 2009;2:151–160. doi: 10.1055/s-0029-1224777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tampieri A, Sprio S, Sandri M, Valentini F. Mimicking natural bio-mineralization processes: a new tool for osteochondral scaffold development. Trends Biotechnol. 2011;29:526–535. doi: 10.1016/j.tibtech.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Landi E, Logroscino G, Proietti L, Tampieri A, Sandri M, Sprio S. Biomimetic Mg-substituted hydroxyapatite: from synthesis to in vivo behaviour. J Mater Sci Mater Med. 2008;19:239–247. doi: 10.1007/s10856-006-0032-y. [DOI] [PubMed] [Google Scholar]
- 21.Horch HH, Sader R, Pautke C, Neff A, Deppe H, Kolk A. Synthetic, pure-phase beta-tricalcium phosphate ceramic granules (Cerasorb) for bone regeneration in the reconstructive surgery of the jaws. Int J Oral Maxillofac Surg. 2006;35:708–713. doi: 10.1016/j.ijom.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Velich N, Németh Z, Hrabák K, Suba Z, Szabó G. Repair of bony defect with combination biomaterials. J Craniofac Surg. 2004;15:11–15. doi: 10.1097/00001665-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Yamasaki Y, Yoshida Y, Okazaki M, Shimazu A, Kubo T, Akagawa Y, Uchida T. Action of FGMgCO3Ap-collagen composite in promoting bone formation. Biomaterials. 2003;24:4913–4920. doi: 10.1016/s0142-9612(03)00414-9. [DOI] [PubMed] [Google Scholar]
- 24.Camargo PM, Lekovic V, Weinlaender M, Klokkevold PR, Kenney EB, Dimitrijevic B, Nedic M, Jancovic S, Orsini M. Influence of bioactive glass on changes in alveolar process dimensions after exodontia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:581–586. doi: 10.1067/moe.2000.110035. [DOI] [PubMed] [Google Scholar]
- 25.Pettinicchio M, Traini T, Murmura G, Caputi S, Degidi M, Mangano C, Piattelli A. Histologic and histomorphometric results of three bone graft substitutes after sinus augmentation in humans. Clin Oral Investig. 2012;16:45–53. doi: 10.1007/s00784-010-0484-9. [DOI] [PubMed] [Google Scholar]
- 26.Mangano C, Scarano A, Iezzi G, Orsini G, Perrotti V, Mangano F, Montini S, Piccirilli M, Piattelli A. Maxillary sinus augmentation using an engineered porous hydroxyapatite: a clinical, histological, and transmission electron microscopy study in man. J Oral Implantol. 2006;32:122–131. doi: 10.1563/796.1. [DOI] [PubMed] [Google Scholar]
- 27.Mangano C, Piattelli A, Perrotti V, Iezzi G. Dense hydroxyapatite inserted into postextraction sockets: a histologic and histomorphometric 20-year case report. J Periodontol. 2008;79:929–933. doi: 10.1902/jop.2008.070245. [DOI] [PubMed] [Google Scholar]


