Abstract
Associations between Obstructive sleep apnea/hypopnea syndrome (OSAHS) and risk of glaucoma remained controversial. Therefore, we performed this meta-analysis to investigate this association. We searched Pubmed, EMBASE, and Wangfang databases for studies before Oct. 10 2014. Odds ratios (ORs) with 95% confidence intervals (CIs) were used to calculate the strength of association. A total of 12 studies with 36909 subjects on the association between OSAHS and glaucoma risk were included for this meta-analysis. OSAHS was associated with a significantly increased risk of glaucoma (OR = 1.65; 95% CI, 1.44-1.88; I 2 = 43%). In the race subgroup analysis, both Asians (OR = 1.78; 95% CI, 1.49-2.12; I 2 = 0%) and Caucasians (OR = 2.03; 95% CI, 1.12-3.69; I 2 = 57%) with OSAHS had increased glaucoma risk. In the subgroup analysis according to gender, both women and men were significantly associated with risk of glaucoma (OR = 1.81; 95% CI, 1.27-2.57; I 2 = 22% and OR = 1.62; 95% CI, 1.29-2.03; I 2 = 0%, respectively). In the subgroup analysis by glaucoma type, OSAHS patients showed increased primary open-angle glaucoma (POAG) risk (OR = 1.87; 95% CI, 1.54-2.33; I 2 = 0%) but not normal tension glaucoma (NTG) risk (OR = 3.57; 95% CI, 0.89-14.43; I 2 = 0%). In addition, severe OSAHS patients had an increased glaucoma risk (OR = 5.49; 95% CI, 1.04-33.83; I 2 = 0%), while mild and moderate OSAHS patients did not show significantly increased glaucoma risk. This meta-analysis suggested that the OSAHS may be a risk factor for glaucoma.
Keywords: OSAHS, glaucoma, meta-analysis, association
Introduction
Obstructive sleep apnea/hypopnea syndrome (OSAHS) is by far the most common respiratory disorder of sleep. OSAHS is caused by the loss of upper airway dilating muscle activity during sleep that is superimposed on a narrow upper airway, resulting in recurrent nocturnal asphyxia [1]. Termination of these events usually requires arousal from sleep to re-establish upper airway tone, eliminate obstruction and allow ventilation to resume. This sleep fragmentation and hypoxaemia lead to poor quality sleep, excessive daytime sleepiness, reduced vigilance, accidents, neurocognitive dysfunction, decreased work productivity, and reduced quality of life [2]. Furthermore, patients with untreated sleep apnoea are at increased risks of hypertension, stroke, heart failure and atrial fibrillation [3].
Glaucoma is a group of eye diseases characterized by a multifactorial progressive optic neuropathy that can result in irreversible vision loss and blindness [4]. The biological basis of glaucoma includes the degeneration of retinal ganglion cells resulting in characteristic cupping of the optic nerve with an accompanying pattern of visual field loss. A number of papers investigated the association between OSAHS and glaucoma risk. However, the results remained inconclusive [5-16]. Meta-analysis is a useful method for investigating associations between genetic factors and diseases, because a quantitative approach is used to combine the results from different studies on the same topic, thereby providing more reliable conclusions. Thus, we performed a meta-analysis to clarify the association of OSAHS and glaucoma risk. To our knowledge, this is the first meta-analysis of the association between OSAHS and glaucoma risk.
Methods
Publication search
Online electronic databases (PubMed, EMBASE, and Wanfang database) was searched using the search terms: (“Obstructive sleep apnea/hypopnea syndrome” or OSAHS or “sleep apnoea syndrome” or OSA or “Obstructive Sleep Apnea”) and glaucoma. Additional studies were identified by a hand search from reference of original studies or review articles on this topic. There was no language restriction.
Inclusion and exclusion criteria
The following inclusion criteria were used: (1) the study should have evaluated the association between the OSAHS and glaucoma risk; (2) the study should have a case-control or cohort design; (3) sufficient data should have been provided in order to calculate odds ratios (OR) and 95% confidence interval (CI). Studies were excluded if any of the following conditions applied: (1) only abstracts or reviews were available, without sufficient data; (2) animal studies; (3) studies were repeated or publications overlapped.
Data extraction
The following data were recorded from each article: first author, years of publication, country, ethnicity of participants, gender, age, diagnose of OSAHS, type of glaucoma, numbers of subjects. The data were extracted by two of the authors independently. Discrepancies between these two authors were resolved by discussion.
Statistical analysis
The strength of association between the OSAHS and glaucoma risk was assessed by calculating OR with 95% CI. A statistical test for heterogeneity was performed based on the Q statistic. The P > 0.10 of the Q-test indicated a lack of heterogeneity among studies. The summary OR estimate of each study was calculated by the random-effects model or fixed-effects model. Stratified analysis was performed by race, gender, glaucoma type, and severity of OSAHS. Potential publication bias was examined by funnel plot and Egger’s test [17]. Cumulative meta-analysis and sensitivity analysis were performed. All statistical tests were performed with the software STATA version 11.0 (Stata Corporation, College station, TX, USA). A P value < 0.05 was considered statistically significant.
Results
Study characteristics
A total of 12 studies (Figure 1) with 36909 subjects on the association between OSAHS and glaucoma risk were included for this meta-analysis [5-16]. There were 3 studies of Asian population and 8 studies of Caucasian population. Diagnose of OSAHS was based on apnea-hypopnea index (AHI) or ICD-9CM. The characteristics of each study are presented in Table 1.
Figure 1.
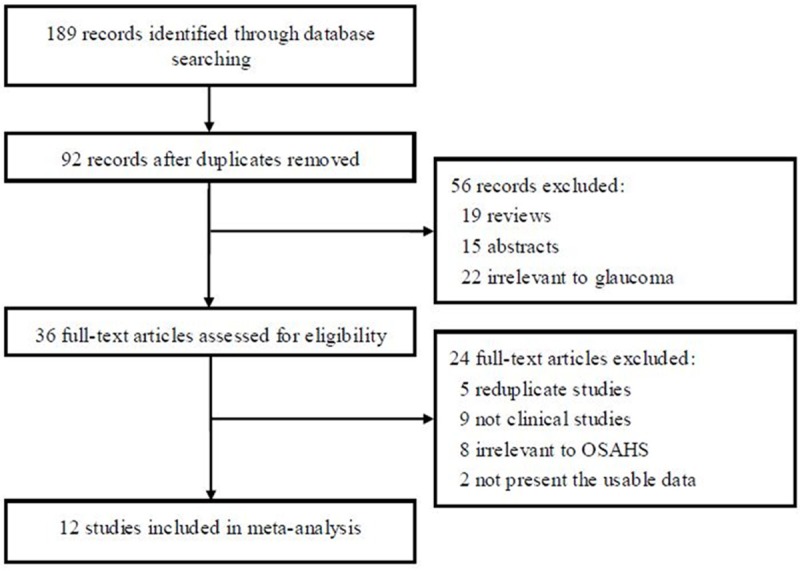
Flow of study identification, inclusion, and exclusion.
Table 1.
Characteristics of the studies included in meta-analysis
| First author | Year | Country | Ethnicity | Age | Gender | Diagnose of OSAHS | Glaucoma type | Total number (n) |
|---|---|---|---|---|---|---|---|---|
| Onen | 2000 | France | Caucasian | 65 | Mixed | NA | POAG | 430 |
| Girkin | 2006 | USA | Mixed | 69 | Mixed | ICD-9 CM | Mixed | 7334 |
| Sergi | 2007 | Italy | Caucasian | 64 | Mixed | AHI ≥ 10 | NTG | 91 |
| Karakucuk | 2008 | Turkey | Caucasian | 52 | Mixed | AHI ≥ 5 | POAG, NTG | 56 |
| Kadyan | 2010 | UK | Caucasian | 55 | Mixed | NA | NA | 115 |
| Lin PW | 2011 | China | Asian | 42 | Mixed | AHI ≥ 5 | NTG | 247 |
| Nowak | 2011 | Poland | Caucasian | 51 | Mixed | AHI ≥ 5 | POAG, NTG | 86 |
| Lin CC | 2013 | China | Asian | 56 | Mixed | ICD-9 CM | POAG | 6072 |
| Moghimi | 2013 | Iran | Caucasian | 47 | Mixed | AHI ≥ 5 | POAG, NTG | 106 |
| Aptel | 2014 | France | Caucasian | 63 | Mixed | AHI ≥ 15 | NA | 9580 |
| Chen | 2014 | China | Asian | 45 | Mixed | ICD-9 CM | NA | 12640 |
| Muniesa | 2014 | Spain | Caucasian | 54 | Mixed | AHI ≥ 10 | POAG, NTG | 152 |
OSAHS, obstructive sleep apnea/hypopnea syndrome; RDI, respiratory disturbance index; AHI, apnea-hypopnea index; POAG, primary open-angle glaucoma; NTG, normal tension glaucoma; NA, not available.
Results of meta-analysis
The evaluations of the association between OSAHS and glaucoma risk are summarized in Table 2. OSAHS was associated with a significantly increased risk of glaucoma (OR = 1.65; 95% CI, 1.44-1.88; I 2 = 43%; Figure 2). In the race subgroup analysis, both Asians (OR = 1.78; 95% CI, 1.49-2.12; I 2 = 0%) and Caucasians (OR = 2.03; 95% CI, 1.12-3.69; I 2 = 57%) with OSAHS had increased glaucoma risk. In the subgroup analysis according to gender, both women and men were significantly associated with risk of glaucoma (OR = 1.81; 95% CI, 1.27-2.57; I 2 = 22% and OR = 1.62; 95% CI, 1.29-2.03; I 2 = 0%, respectively). In the subgroup analysis by glaucoma type, OSAHS patients showed increased primary open-angle glaucoma (POAG) risk (OR = 1.87; 95% CI, 1.54-2.33; I 2 = 0%) but not normal tension glaucoma (NTG) risk (OR = 3.57; 95% CI, 0.89-14.43; I 2 = 0%). In addition, severe OSAHS patients had an increased glaucoma risk (OR = 5.49; 95% CI, 1.04-33.83; I 2 = 0%), while mild and moderate OSAHS patients did not show significantly increased glaucoma risk.
Table 2.
Results of meta-analysis and subgroup analyses
| No. of studies | Test of association | Heterogeneity | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| OR (95% CI) | Z | P Value | Model | χ 2 | P Value | I 2 (%) | ||
| Overall | 12 | 1.65 (1.44-1.88) | 7.40 | < 0.00001 | R | 19.15 | 0.06 | 43 |
| Race | ||||||||
| Asian | 3 | 1.78 (1.49-2.12) | 6.35 | < 0.00001 | F | 0.91 | 0.63 | 0 |
| Caucasian | 8 | 2.03 (1.12-3.69) | 2.33 | 0.02 | R | 16.46 | 0.02 | 57 |
| Gender | ||||||||
| Male | 2 | 1.62 (1.29-2.03) | 4.15 | < 0.0001 | F | 0.64 | 0.42 | 0 |
| Female | 2 | 1.81 (1.27-2.57) | 3.30 | 0.001 | F | 1.28 | 0.26 | 22 |
| Glaucoma type | ||||||||
| POAG | 6 | 1.87 (1.54-2.33) | 6.09 | < 0.00001 | F | 3.79 | 0.58 | 0 |
| NTG | 5 | 3.57 (0.89-14.43) | 1.79 | 0.07 | F | 0.49 | 0.97 | 0 |
| Severity of OSAHS | ||||||||
| Mild | 3 | 2.60 (0.27-25.40) | 0.82 | 0.41 | F | 0.04 | 0.85 | 0 |
| Moderate | 2 | 5.44 (0.27-108.60) | 1.11 | 0.27 | F | 0.54 | 0.76 | 0 |
| Severe | 4 | 5.49 (1.04-33.83) | 2.01 | 0.04 | F | 0.20 | 0.91 | 0 |
POAG, primary open-angle glaucoma; NTG, normal tension glaucoma; OSAHS, obstructive sleep apnea/hypopnea syndrome; R, random-effects model; F, fixed-effects model.
Figure 2.
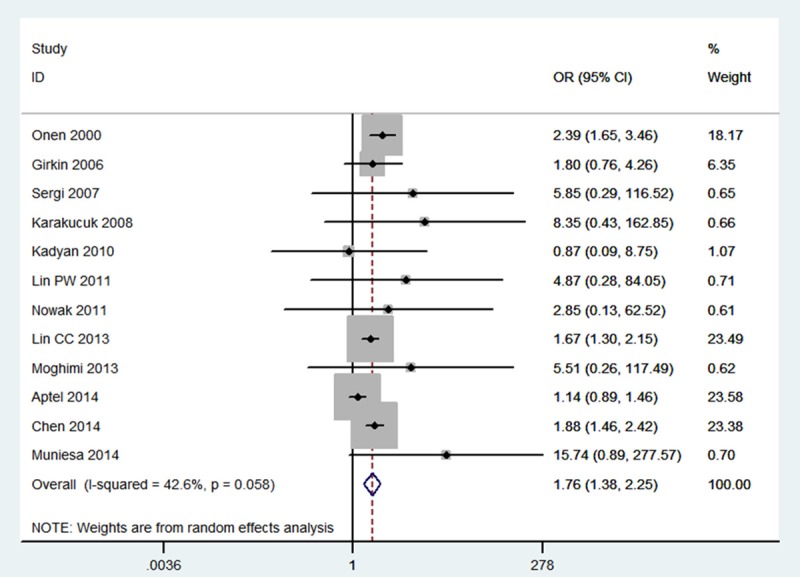
Meta-analysis for the association between OSAHS and glaucoma risk.
As shown in Figure 3, significant associations were evident with each addition of more data over time. The results showed that the pooled ORs tended to be stable. A single study involved in the meta-analysis was deleted each time to reflect the influence of the individual data set to the pooled ORs, and the corresponding pooled ORs were not materially altered (Figure 4). The Galbraith plot was used to find the source of the heterogeneity. As shown in Figure 5, two studies were the outliers. After excluding these studies, the between-study heterogeneity effectively decreased and there was no obvious heterogeneity among the twenty-four remaining studies (I 2 = 0%, P = 0.77). Besides, the result was still statistically significant (OR = 1.81; 95% CI, 1.52-2.15).
Figure 3.
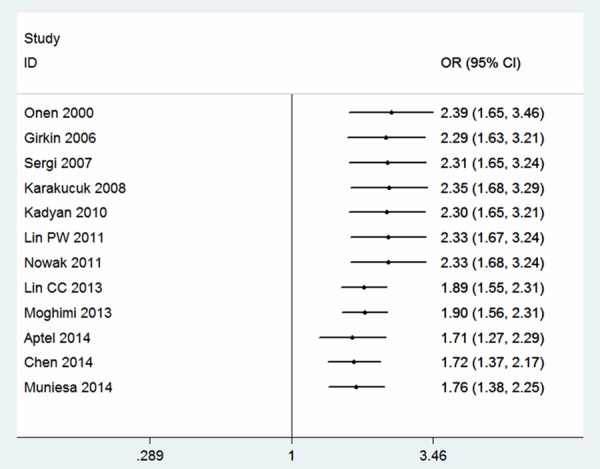
Cumulative meta-analysis for the association between OSAHS and glaucoma risk.
Figure 4.
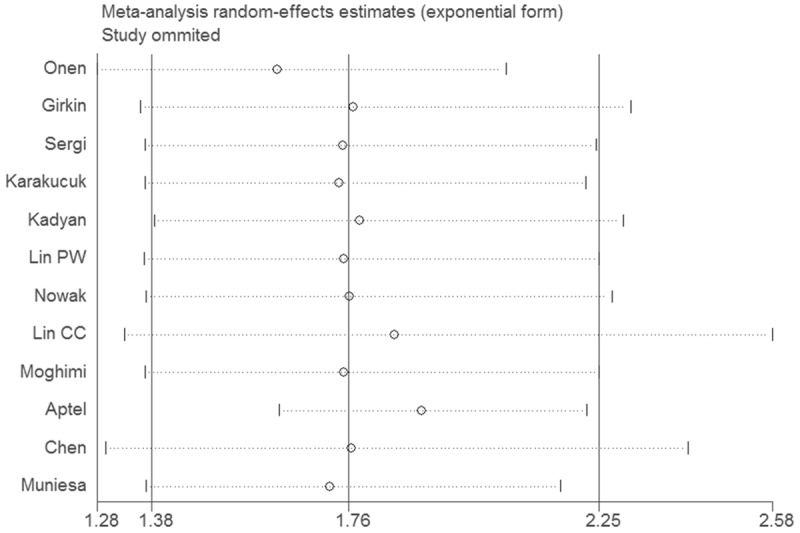
Sensitivity meta-analysis for the association between OSAHS and glaucoma risk.
Figure 5.
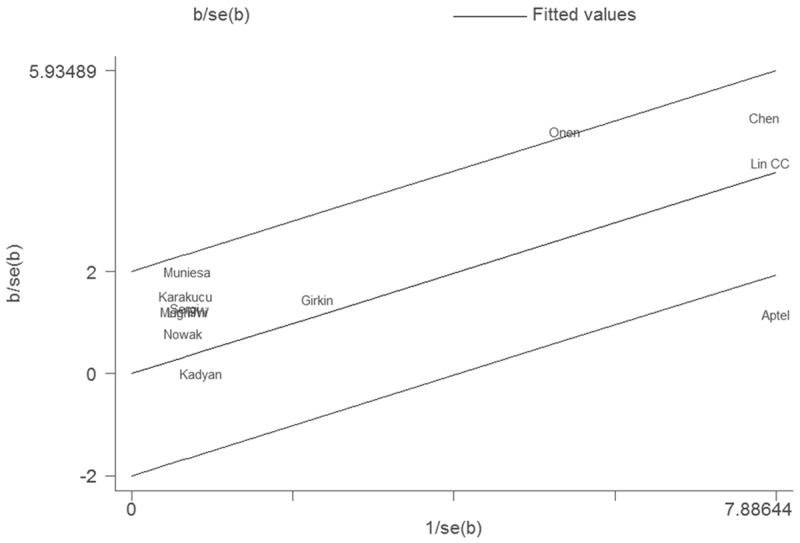
Galbraith plot of OSAHS and glaucoma risk.
Funnel plot was performed to assess the publication bias of literatures. The shape of the funnel plot showed symmetry (Figure 6). Egger’s test found no evidence of publication bias (P = 0.335).
Figure 6.
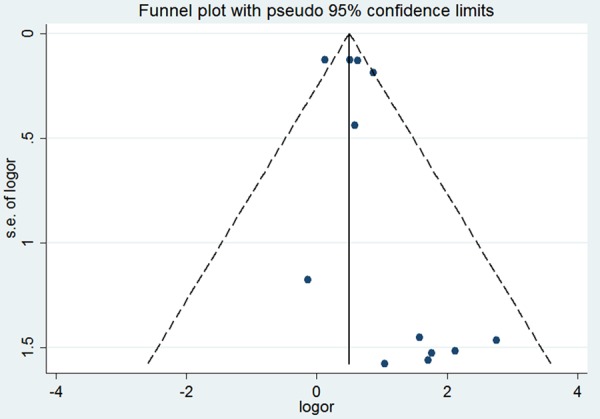
Funnel plot for the association between OSAHS and glaucoma risk.
Discussion
In this meta-analysis, we investigated the association between the OSAHS and glaucoma risk including 36909 subjects. We found that individuals with OSAHS showed an increased risk of glaucoma in the overall population. The result from our meta-analysis suggested that OSAHS patients had a 65% increased glaucoma risk compared to those normal individuals. In the stratified analysis by ethnicity, the significant association was observed in Asians and Caucasians. Only three studies conducted in Asians population were searched in our meta-analysis. Thus, more studies with Asians and other ethnic groups are still needed to address the role of OSAHS on glaucoma risk. In the subgroup analysis by gender, we found that OSAHS exhibited increased glaucoma risk in men and women. This result indicated that the role of glaucoma was not selective by gender. The subgroup analysis based on glaucoma type found that OSAHS showed increased POAG risk but not NTG risk. This meta-analysis included only 5 studies using NTG patients, the positive association between OSAHS and NTG could not be ruled out because studies with small sample size may have insufficient statistical power to detect a slight effect. In the future, more studies should be performed focusing on NTG patients with OSAHS. When subgroup analysis was performed according to severity of OSAHS, a significant association was showed in severe OSAHS patients. Since the number of studies included in this subgroup analysis was small, the results lacked sufficient reliability to confirm or refute an association in a definitive manner. In the future, more studies should be designed to analyze these associations.
The pathogenesis of ocular complications in OSAHS is likely to have a multifactorial origin, in which both vascular and mechanical factors may be present. Among the vascular factors, it has been postulated that there may be insufficient blood supply to nourish the retinal nerve fiber layer (RNFL) and/or optic nerve [8]. Repetitive or prolonged episodes of hypoxia may cause direct damage to the optic nerve [18]. Besides, the repetitive prolonged upper airway obstruction followed by arousal produces transient hypoxemia and hypercapnia, as well as increased sympathetic tone, which activates the renin-angiotensin system [19] and can lead to an increase in blood pressure and vascular resistance [20].
Results from one-way sensitivity analysis and cumulative meta-analysis suggested high stability and reliability of our results. Besides, we had to mention the importance of heterogeneity and publication bias, which might influence the results of meta-analysis. In our study, significant heterogeneity was observed. We used Galbraith plots to explore the sources of heterogeneity. We found that I 2 value was decreased after excluding the outliers. The results suggested that the 2 outlying studies might be the major source of the heterogeneity. However, heterogeneity did not seem to influence the results, because the significance of the result was not altered after excluding the outliers. Additionally, funnel plots and Egger’s tests were used to find potential publication bias. The results indicated that there was no significant publication bias.
In conclusion, this meta-analysis suggested that OSAHS may be associated with the risk of glaucoma.
Acknowledgements
This work was supported by Natural Science Foundation of Hainan province (No. 814393).
Disclosure of conflict of interest
None.
References
- 1.White DP. Sleep-related breathing disorder. 2. Pathophysiology of obstructive sleep apnoea. Thorax. 1995;50:797–804. doi: 10.1136/thx.50.7.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wenner JB, Cheema R, Ayas NT. Clinical manifestations and consequences of obstructive sleep apnea. J Cardiopulm Rehabil Prev. 2009;29:76–83. doi: 10.1097/HCR.0b013e31819a00f1. [DOI] [PubMed] [Google Scholar]
- 3.Gottlieb DJ, Yenokyan G, Newman AB, O’Connor GT, Punjabi NM, Quan SF, Redline S, Resnick HE, Tong EK, Diener-West M, Shahar E. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–20. doi: 10.1016/S0140-6736(04)16257-0. [DOI] [PubMed] [Google Scholar]
- 5.Onen SH, Mouriaux F, Berramdane L, Dascotte JC, Kulik JF, Rouland JF. High prevalence of sleep-disordered breathing in patients with primary open-angle glaucoma. Acta Ophthalmol Scand. 2000;78:638–41. doi: 10.1034/j.1600-0420.2000.078006638.x. [DOI] [PubMed] [Google Scholar]
- 6.Girkin CA, McGwin G Jr, McNeal SF, Owsley C. Is there an association between pre-existing sleep apnoea and the development of glaucoma? Br J Ophthalmol. 2006;90:679–81. doi: 10.1136/bjo.2005.086082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sergi M, Salerno DE, Rizzi M, Blini M, Andreoli A, Messenio D, Pecis M, Bertoni G. Prevalence of normal tension glaucoma in obstructive sleep apnea syndrome patients. J Glaucoma. 2007;16:42–6. doi: 10.1097/01.ijg.0000243472.51461.24. [DOI] [PubMed] [Google Scholar]
- 8.Karakucuk S, Goktas S, Aksu M, Erdogan N, Demirci S, Oner A, Arda H, Gumus K. Ocular blood flow in patients with obstructive sleep apnea syndrome (OSAS) Graefes Arch Clin Exp Ophthalmol. 2008;246:129–34. doi: 10.1007/s00417-007-0656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kadyan A, Asghar J, Dowson L, Sandramouli S. Ocular findings in sleep apnoea patients using continuous positive airway pressure. Eye (Lond) 2010;24:843–50. doi: 10.1038/eye.2009.212. [DOI] [PubMed] [Google Scholar]
- 10.Lin PW, Friedman M, Lin HC, Chang HW, Wilson M, Lin MC. Normal tension glaucoma in patients with obstructive sleep apnea/hypopnea syndrome. J Glaucoma. 2011;20:553–8. doi: 10.1097/IJG.0b013e3181f3eb81. [DOI] [PubMed] [Google Scholar]
- 11.Nowak MS, Jurowski P, Gos R, Prost ME, Smigielski J. Pulsatile ocular blood flow in subjects with sleep apnoea syndrome. Arch Med Sci. 2011;7:332–6. doi: 10.5114/aoms.2011.22087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin CC, Hu CC, Ho JD, Chiu HW, Lin HC. Obstructive sleep apnea and increased risk of glaucoma: a population-based matched-cohort study. Ophthalmology. 2013;120:1559–64. doi: 10.1016/j.ophtha.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Moghimi S, Ahmadraji A, Sotoodeh H, Sadeghniat K, Maghsoudipour M, Fakhraie G, Latifi G, Nassiri N, Giaconi JA. Retinal nerve fiber thickness is reduced in sleep apnea syndrome. Sleep Med. 2013;14:53–7. doi: 10.1016/j.sleep.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Aptel F, Chiquet C, Tamisier R, Sapene M, Martin F, Stach B, Grillet Y, Levy P, Pépin JL. Sleep Registry of the French Federation of Pneumology Paris, France. Association between glaucoma and sleep apnea in a large French multicenter prospective cohort. Sleep Med. 2014;15:576–81. doi: 10.1016/j.sleep.2013.11.790. [DOI] [PubMed] [Google Scholar]
- 15.Chen HY, Chang YC, Lin CC, Sung FC, Chen WC. Obstructive sleep apnea patients having surgery are less associated with glaucoma. J Ophthalmol. 2014;2014:838912. doi: 10.1155/2014/838912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muniesa M, Sánchez-de-la-Torre M, Huerva V, Lumbierres M, Barbé F. Floppy eyelid syndrome as an indicator of the presence of glaucoma in patients with obstructive sleep apnea. J Glaucoma. 2014;23:e81–5. doi: 10.1097/IJG.0b013e31829da19f. [DOI] [PubMed] [Google Scholar]
- 17.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsang CS, Chong SL, Ho CK, Li MF. Moderate to severe obstructive sleep apnoea patients is associated with a higher incidence of visual field defect. Eye (Lond) 2006;20:38–42. doi: 10.1038/sj.eye.6701785. [DOI] [PubMed] [Google Scholar]
- 19.Barceló A, Elorza MA, Barbé F, Santos C, Mayoralas LR, Agusti AG. Angiotensin converting enzyme in patients with sleep apnoea syndrome: plasma activity and gene polymorphisms. Eur Respir J. 2001;17:728–32. doi: 10.1183/09031936.01.17407280. [DOI] [PubMed] [Google Scholar]
- 20.Kario K. Obstructive sleep apnea syndrome and hypertension: ambulatory blood pressure. Hypertens Res. 2009;32:428–32. doi: 10.1038/hr.2009.56. [DOI] [PubMed] [Google Scholar]


