Abstract
Purpose: To establish a classification system for the different types of posterior tibial plateau fractures (PTPF), and to explore the fracture patterns and early results of treatment. Methods: 39 PTPFs patients who received surgeries through posteromedial or (and) posterolateral knee approaches were analyzed retrospectively. Results: There were 5 types of PTPFs identified in the new classification system: posteromedial split fracture (type I, 7 patients), posterolateral split fracture (type II, 5 patients), posterolateral depression fracture (type III, 11 patients), posterolateral split and depression fracture (type IV, 2 patients), and posteromedial split combined with posterolateral depression fracture (type V, 14 patients). All patients underwent surgeries safely without complications. The average follow up was 18.1 months (12-30 months). The average weight-bearing durations were 15.6 weeks (12-20 weeks). Based on Rasmussen functional scoring system, 20 cases were regarded as excellent, 14 were good, 5 were fair, and 0 was poor. There was significant change in the Rasmussen functional score before (8.38 ± 2.87) and after surgery (24.20 ± 3.44). According to Rasmussen radiology system, 28 cases were excellent, 8 cases were good, 3 were fair, and none was poor. There was also a significant difference detected between pre-operation (6.77 ± 2.27) and post-operation (16.41 ± 2.65). Conclusion: This study presents a new classification system for the different types of PTPFs based on the treatment. The classification is clinically relevant and can be used to guide the surgical management.
Keywords: Tibia plateau, fracture, CT scan, classification
Introduction
Fracture classifications help surgeons to make their decisions on treatment and prognosis. Among available classifications for tibial plateau fractures [1-7], the Schatzker classification is the most widely used tool. The AO and the Hohl & Moore systems are still in use.
But posterior tibial plateau fracture (PTPF) is a relatively uncommon injury, with an incidence of 28.8% [8]. This kind of fracture appears confusing on initial radiographs because of the small displacement, so it is a special injury pattern that is not sufficiently included in any type of the classification systems [9]. There are controversies over surgical approaches and fixation methods for PTPF, because it is difficult to reduce and stabilize the injury through conventional strategies.
Three-Column Classification can be used as a recent supplement to the conventional Schatzker Classification, which is useful for multi-planar fractures involving the posterior column [10,11]. However, they did not describe the fracture patterns of the posterior column. Lack of the subgroups, complex PTPF cannot be managed through this classification system.
This article proposed a new classification system by classifying PTPFs into 5 categories, which combined Schatzker classification systems with three-column classification based on the x ray, helical CT scanning and MRI 3D reconstruction.
Materials and methods
Ethics
The study protocol was approved by the Medical Ethics Committee of the Central Hospital of Yiwu City. The procedures were in accord with the Helsinki Declaration of 1975 as revised in 2008. Patients have a right to privacy that should not be infringed without informed consent. All participants did have to sign an informed consent form. The patients’ informed consent and the hospital ethics committee’s approval had been obtained for the above operation.
General data
Thirty-nine patients admitted to our hospital from Jan 2006 to July 2009 (23 males and 16 females, age range 26-68 yrs., mean age 41.6 yrs.) were included in the study. The causes of injury included traffic accidents in 26 patients, fall in 9 patients, and other reasons in 4 patients. All of them were fresh closed fractures. Before operation, all patients had received knee joint lateral X-ray, CT scanning, and MRI 3D reconstruction to identify the displacement and classification of the fractures. A helical scan was performed at 120 kV (tube voltage) and 125 mA, with a 3 mm slice-thickness, at a 1.5 mm reconstruction interval, and at the pitch of 1 by a 16-Slice Whole Body Spiral CT Scanner (Toshiba, Japan).
Injury classification
According to the direction and form of the fracture line Five types were proposed: Type I-split fracture of posteromedial condyle (7 cases, 18.0%); Type II-split fracture of posterolateral condyle (5 cases, 12.8%); Type III-collapse fracture of posterolateral condyle (11 cases, 28.2%); Type IV-split and collapse fracture of posterolateral condyle (2 cases, 5.1%); and Type V-split fracture of posteromedial condyle and collapse fracture of posterolateral condyle (14 cases, 35.9%) (Figures 1 and 2).
Figure 1.
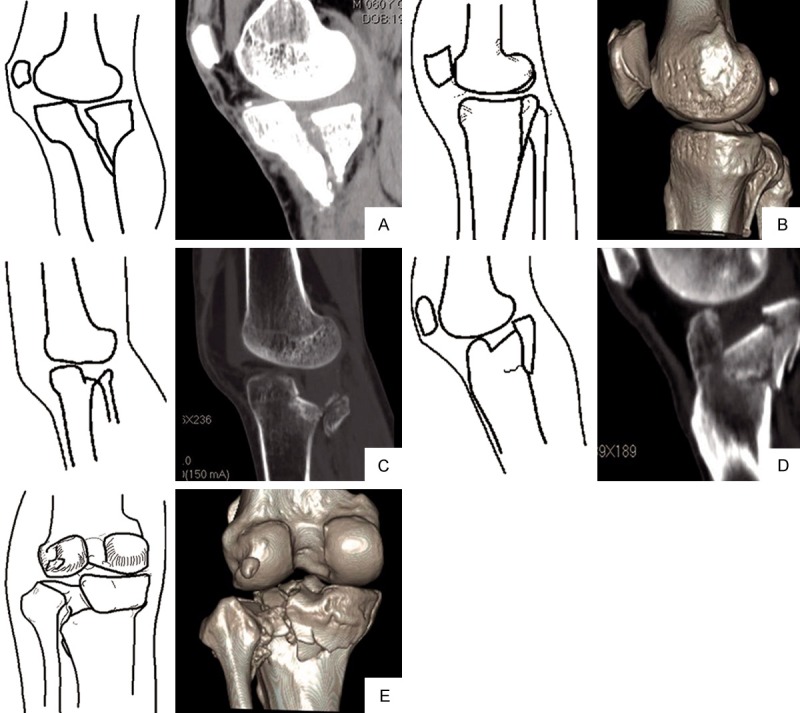
Diagrammatic sketch showing five fracture patterns of posterior tibial plateau. A. Type I-split fracture of posteromedial condyle; B. Type II-split fracture of posterolateral condyle); C. Type III-collapse fracture of posterolateral condyle; D. Type IV-split and collapse fracture of posterolateral condyle; E. Type V-split fracture of posteromedial condyle and collapse fracture of posterolateral condyle.
Figure 2.

Based on CT classification, type I: posteromedial condylar tibial plateau split fracture (A); type II: posterolateral condylar split fracture of tibial plateau (B, C); type III: posterolateral condylar depression fracture of tibial plateau (D, E); type IV: posterolateral condylar split and depression fracture of tibial plateau (F, G); type V: Combined posteromedial split with posterolateral depression fracture of tibial plateau. (H, I-CT; J, K-X Ray; L-MRI).
Selection of surgical procedures
Operative approaches were chosen according to the fracture type: the posteromedial inverted “L” incision for posteromedial condylar fracture of tibial plateau, posterolateral inverted “L” incision for posterolateral condylar fracture of tibial plateau, and a combination of medial and lateral approaches for bilateral posterior condylar fractures (Figure 3).
Figure 3.
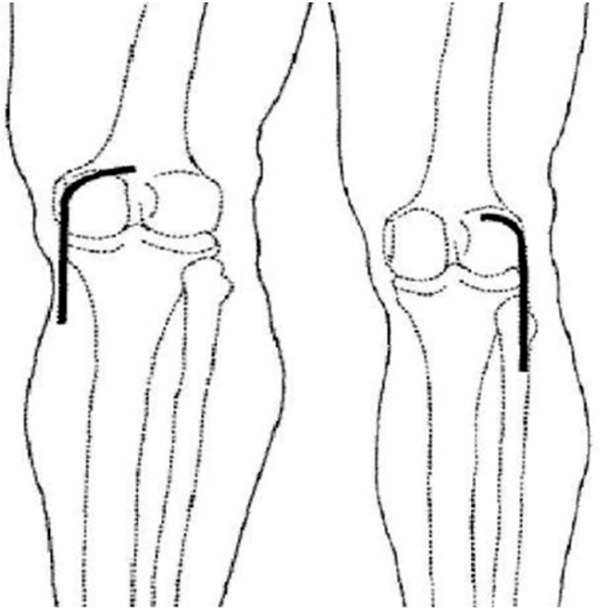
Diagrammatic sketch showing posteromedial inverted “L” incision and posterolateral inverted “L” incision.
Type I was managed with a posterolateral approach as follows. A posteromedial inverted-L incision was made at 3 cm above the popliteal stripes till reaching the posterior margin of the posteromedial condyle, and then along this margin to 10 cm below the joint line. After the skin and subcutaneous tissue were incised, skin flap was lifted to expose semitendinosus and gastrocnemius medial head. In this process, special attention should be paid to protect the saphenous nerve and great saphenous vein in the superficial fascia. Then the gastrocnemius medial head and the popliteal vessels and tibial nerves on its lateral surface were drawn outward. The semitendinosus tendon was pulled inward to expose the semimembranosus attachment on the posterior articular capsule. Then, the semimembranosus attachment was cut off from the joint line. After subperiosteal dissection, posterior tibial condyle was revealed. After the posterior joint capsule was incised along the joint line, the posterior horn of medial meniscus was pulled upward. Then the articular facet of posterior tibial condyle was disclosed. If the incision needed extension to the distal end to expose the proximal tibia, the soleus starting point could be incised for subperiosteal dissection.
Type II-IV were managed with a posterolateral approach as follows. The patients were placed in a prone position. Under epidural or general anesthesia, an upside-down “L” incision was made horizontally following the popliteal fossa striae laterally for approximately 3 cm, with the vertical limb of the incision extending along the medial side of the femoral biceps tendon downwards to the joint line for approximately 7 cm. After the skin and the subcutaneous tissues were incised, the peroneal nerve was bluntly dissected free along the medial side of the biceps femoris and the fibular head. The peroneal nerve and the biceps femoris tendon were then retracted laterally. The inferior lateral genicular vascular bundle was ligated. Precautions were taken to protect the peroneal nerve and artery in the distal end of the incision. The proximal end of the soleus muscle was separated sub-periosteally and retracted medially together with the lateral end of the gastrocnemius. The joint capsule and posterolateral condyles of the tibial plateau were exposed between the popliteal muscle and the soleus muscle, all internal fixations were then performed below the popliteal muscle. Along the joint line, the posterior joint capsule was incised horizontally, and the lateral posterior horn of the meniscus was displaced upwards so that the entire lateral tibial plateau including the posterolateral articular surface could be adequately viewed. In the process of fracture reduction, the knee joint was kept as extended as possible with appropriate axial traction added as needed, to optimize exposure of the fracture surface. When an extended incision was needed, the proximal end of the soleus was partially incised and a sub-periosteal detachment was performed to allow for an adequate exposure.
Collapse fractures of posterolateral condyle, i.e, type III, IV and V fractures, require bone-graft filling. The defect must be completely pressurized and filled to prevent loss of reduction after surgery. For patients with meniscus or cruciate ligament injury, anterior exploratory operation was undertaken.
Postoperative management and follow up
Routine use of antibiotics was administered for 3 d after the surgery. Postoperatively, all patients were mobilized under 15 kg of weight bearing for 6 weeks. A continuous-passive-motion (CPM) device (Kinetec®) was recommended for patients from the postoperative day onwards, except those with collateral ligament injury or extensive suturing of the periphery of the meniscus. For patients with meniscus or cruciate ligament injury, long leg brace fixation was conducted after operation, followed by joint exercise for 4-6 w.
In addition, active-assisted range of motion exercises were started as soon as the wounds were healed and a daily injection of 5,000 IU low molecular heparin was applied to prevent deep vein thrombosis. Radiological and clinical examinations were conducted 6 and 12 weeks after the surgery. After 12 weeks, all patients showed a good radiological fracture healing, and as a result, were able to be mobilized under full weight bearing. All discharged patients were followed-up monthly for the first three months.
Statistical analysis
All data analysis was performed using SPSS 11.0 (SPSS Inc, Chicago IL). Descriptive statistics were used to determine ranges, means, and standard deviations. One-way analysis of variance and Student t tests were used to determine the difference between two means. P < 0.05 was considered statistically significant.
Results
All the 39 patients were followed for 12-30 months (average, 18.1 months). Union of fractures took 11-16 months (mean, 15.2 months), with full weight bearing occurring at 12-20 w (average, 15.6 w). In this group of cases, fractures were fixed by screws (8 cases), reconstruction plates (4 cases) or T-shaped plate (27 cases). In 5 cases accompanied by anterior cruciate ligament avulsion fracture from the tibial spin, bone tunnels were constructed under the tibial plateau followed by wire fixation. In the 4 cases with meniscus injuries, 2 received meniscus repair and the other 2 underwent partial excision of the meniscus.
There were no cases of infection, intraoperative vascular nerve injuries, internal fixation loose or breakage, disunion, knee varus/valgus deformity, or fracture re-displacement. Knee function results were evaluated by patients’ self-assessment (pain and walking ability) and clinicians’ examination (knee joint range of movements and knee joint stability) according to the Rasmussen functional scoring system [12]. In this group, 20 cases were evaluated as excellent, 14 cases as good, 5 as fair, and 0 case as poor (rang: 16-30 points; average: 24.2 points; excellent and good rate: 87.2%). There was significant difference (t = 20.31, P < 0.001) in the Rasmussen functional score between pre-operation (8.38 ± 2.87) and post-operation (24.20 ± 3.44).
Evaluation of the reduction were made using Rasmussen radiology scoring system 12, 28 cases were evaluated after surgery by Rasmussen system as excellent, 8 cases as good, 3 as fair, 0 case as poor (range: 10-18 points; average: 16.41 points; excellent and good rate: 92.3%). There was significant difference (t = 17.253, P = 0.0025) in the Rasmussen radiology score between pre-operation (6.77 ± 2.27) and post-operation (16.41 ± 2.65). All patients were satisfied with the surgical results (Figures 4 and 5).
Figure 4.
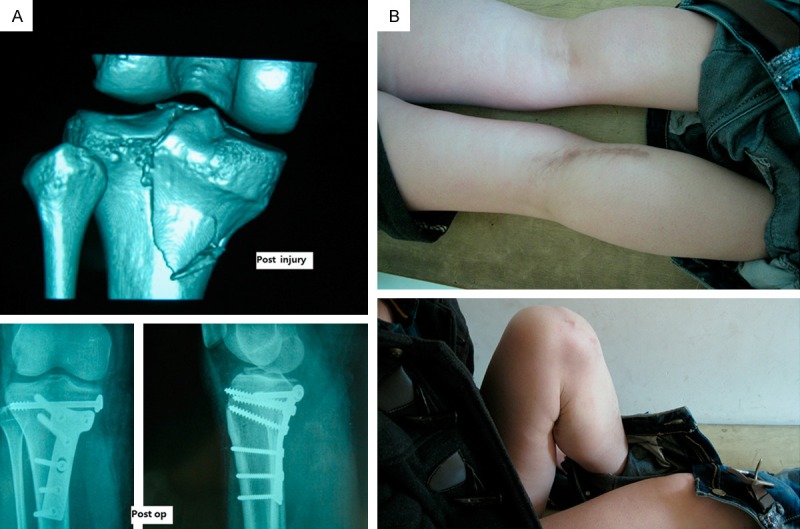
A 41-year-old female with left split fracture of posteromedial condylar tibial plateau fracture (type I). Preoperative CT 3D-reconstruction showed posteromedial condylar split fracture of tibial plateau. Postoperative X radiographs showing anatomical reduction (A). Knee function results were excellent after 22 months (B).
Figure 5.
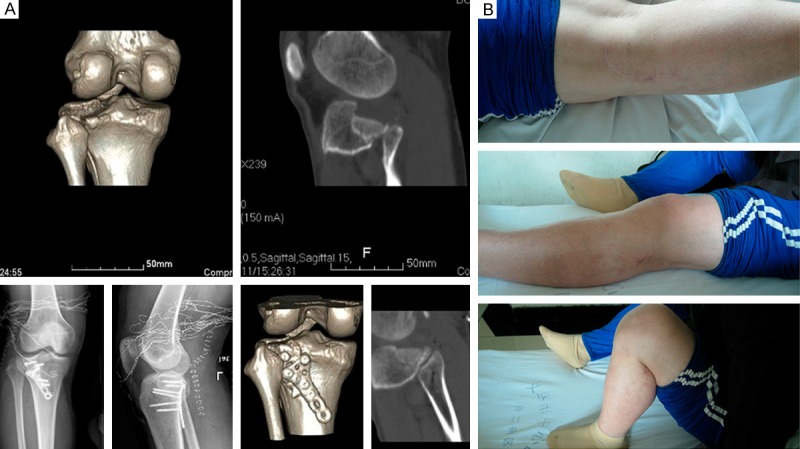
A 39-year-old male with left posterolateral condylar tibial plateau split and depression fracture (type IV). Preoperative CT 3D-Reconstruction showed posterolateral condylar split depression fracture of tibial plateau. Postoperative X radiographs and CT showing anatomical reduction (A). Knee function results were excellent after 19 months (B).
Discussion
Posterior tibial plateau fracture (PTPF) is caused when the posterior tibia plateau is stricken by the femoral condyle while the knee joint, in semi flexion or flexed position, suffers from a varus-valgus stress [13,14]. It have been uncommon, as PTPFs were found in 151 cases and had an incidence of 28.8%. Except for type III, PTPFs were observed in each type of the Schatzker classification system. The Schatzker type VI, V, and IV fractures had the three highest percentages of PTPFs, with 76.1, 51.2, and 22.4%, respectively [15].
These injuries form a special injury pattern of primarily posterior displacement is not well described by the AO/Orthopaedic Trauma Association classification or Schatzker classification systems [7,16-18].
Proper analysis of the lateral radiograph and CT scans clarifies the fracture pattern and allows planning of appropriate treatment. In this group of cases, there were 21 cases of posteromedial condylar fractures and 32 cases of posterolateral fractures, and also 14 cases of both posteromedial and posterolateral fractures. In the position of genuflex, the lateral condyle has a larger posterior displacement than the medial condyle (medial condyle: 5-6 mm; lateral condyle: 10-12 mm), with simultaneous femoral external rotation. The connection between the two points (before and after the left-and-right displacement) forms an angle of 20°. Therefore, the bone blocks of lateral posterior condylar splits are smaller while those of posterior medial condylar splits are larger.
Mostly, the lateral posterior condyle suffers from compression, while the medial posterior condyle endures split. Medial condylar compression is rare. In this group, there was one case of compression fracture of medial posterior condyle. This fact might be associated with the greater strength of medial cortex, and also with the external rotation stress in the knee flection movement.
PTPF is difficult to adequately reduce and stabilize by conventional techniques and approaches. A modified posterior approach is an ideal approach for such injuries according to different fracture patterns [8,11,13,19-22].
As for Type I (split fracture of posteromedial condyle), anteromedial approach is adopted in the Type I fracture to expose the medial posterior condyle traditionally. In this approach, the fracture site was shown from the lateral side; however, the medial collateral ligament (MCL) is easily injured during dissection. When the dissection was over a large area, flap margin necrosis is possibly to occur. Moreover, the limited exposure also adds the difficulty of reduction and fixation. Currently, the knee posteromedial approach has been widely applied in the treatment of posterior medial condylar fracture [23]. Using this incision to expose the posterior medial condylar tibial plateau fracture, satisfactory results have been achieved.
To fix Type I fractures, posterior T-shaped plate or reconstruction plate internal fixation is a possible choice. Brunner et al [24] advocated a posterior T-shaped anti-glide plate, which they thought offered better stability. Its effect was later confirmed biomechanically by Zeng et al [25].
As to Type II, III, and IV fractures, Chang et al [13] present a case series of 8 patients with isolated posterior coronal fractures of lateral tibial plateau. Tao et al think the modified posterolateral approach could help to expand the surgical options for an optimal treatment of the posterolateral shearing tibial plateau fracture, and plating of posterolateral shearing fractures would result in restoration and maintenance of alignment1.
An inverted L-shaped posterior approach was recommended by Luo et al 11 in the treatment of posterolateral condylar fractures. Still, owing to the blocking of medial gastrocnemius muscle, there is difficulty dealing with the posterolateral condylar fracture. Sometimes, it is required to cut the medial gastrocnemius muscle, which restricts early functional exercise. An anterolateral approach was adopted by Fernandez DL [26] to treat posterolateral fracture with percutaneous reduction by leverage at the tibial condyle, but anatomic reduction was difficult to achieve.
Yu et al [27] developed a new method by removing partial or full heads of the fibula, which they considered beneficial to reduction and fixation of posterolateral tibial plateau fractures. The fibular head is the attachment point of lateral collateral ligament, biceps femoris tendon, and arcuate ligaments. The osteotomy will inevitably ruin the normal anatomy of the fibular head. Such an approach, providing exposure and internal fixation but at the cost of adjacent structures, certainly cannot be the best choice.
Bhattacharyya described the posterior shearing tibial plateau fracture patterns and early results of treatment via a posterior approach 8. But his popliteal approach was posteromedial indeed and required a large skin flap with extensive medial dissection and the tendotomy of the medial head of the gastrocnemius. Carlson’s approach was less invasive, but it was more advantageous to expose the lateral plateau rather than the posterior aspect [22].
Our classification was based on 3D-CT reconstruction images, offering more detailed categorization of PTPF. It can significantly improve the reliability of fracture classification 5 and facilitates clinicians to understand the fracture better. Moreover, being helpful in fracture diagnosis, this classification provides reliable basis for the selection of treatment plan, operative approach and internal fixation method. Therefore, better outcome can be expected in the treatment of PTPFs. Nevertheless, the classification isolates posterior condylar tibial plateau fractures from other fractures, which actually are often accompanied by anterior medial and lateral condylar tibial plateau fractures (23/39, 59% in this group of cases). Therefore, there are still some defects in it. In addition, owing to the limited number of cases in this study, this fracture classification is not perfect. Further studies were essential to complete and refine it with multicentric statistical analyses of a large quantity of cases.
Acknowledgements
The authors thank Yiwu Municipal Science and Technology Bureau and Wenzhou Medical University for the generous support of us. We thank Drs. NaiFeng Tian and Majid Farooqi for their assistance in preparation of the manuscript.
Disclosure of conflict of interest
None.
References
- 1.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res. 1979:94–104. [PubMed] [Google Scholar]
- 2.Honkonen SE, Jarvinen MJ. Classification of fractures of the tibial condyles. J Bone Joint Surg Br. 1992;74:840–847. doi: 10.1302/0301-620X.74B6.1447244. [DOI] [PubMed] [Google Scholar]
- 3.Muller ME, Allgower M, Schneider R, Willenegger H. Manual of Internal Fixation. Berlin: Springer-Verlag; 1979. [Google Scholar]
- 4.Hohl M. Tibial condylar fractures. J Bone Joint Surg Am. 1967;49:1455–1467. [PubMed] [Google Scholar]
- 5.Moore TM. Fracture--dislocation of the knee. Clin Orthop Relat Res. 1981:128–140. [PubMed] [Google Scholar]
- 6.Wahlquist M, Iaguilli N, Ebraheim N, Levine J. Medial tibial plateau fractures: a new classification system. J Trauma. 2007;63:1418–1421. doi: 10.1097/TA.0b013e3181469df5. [DOI] [PubMed] [Google Scholar]
- 7.Khan RM, Khan SH, Ahmad AJ, Umar M. Tibial plateau fractures. A new classification scheme. Clin Orthop Relat Res. 2000:231–242. [PubMed] [Google Scholar]
- 8.Bhattacharyya T, McCarty LP 3rd, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, Smith RM. The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma. 2005;19:305–310. [PubMed] [Google Scholar]
- 9.Maripuri SN, Rao P, Manoj-Thomas A, Mohanty K. The classification systems for tibial plateau fractures: how reliable are they? Injury. 2008;39:1216–1221. doi: 10.1016/j.injury.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 10.Zhu Y, Yang G, Luo CF, Smith WR, Hu CF, Gao H, Zhong B, Zeng BF. Computed tomography-based Three-Column Classification in tibial plateau fractures: introduction of its utility and assessment of its reproducibility. J Trauma Acute Care Surg. 2012;73:731–737. doi: 10.1097/TA.0b013e31825c17e7. [DOI] [PubMed] [Google Scholar]
- 11.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 12.Rasmussen PS. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–1350. [PubMed] [Google Scholar]
- 13.Chang SM, Zheng HP, Li HF, Jia YW, Huang YG, Wang X, Yu GR. Treatment of isolated posterior coronal fracture of the lateral tibial plateau through posterolateral approach for direct exposure and buttress plate fixation. Arch Orthop Trauma Surg. 2009;129:955–962. doi: 10.1007/s00402-009-0829-5. [DOI] [PubMed] [Google Scholar]
- 14.Tao J, Hang DH, Wang QG, Gao W, Zhu LB, Wu XF, Gao KD. The posterolateral shearing tibial plateau fracture: treatment and results via a modified posterolateral approach. Knee. 2008;15:473–479. doi: 10.1016/j.knee.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Yang G, Zhai Q, Zhu Y, Sun H, Putnis S, Luo C. The incidence of posterior tibial plateau fracture: an investigation of 525 fractures by using a CT-based classification system. Arch Orthop Trauma Surg. 2013;133:929–934. doi: 10.1007/s00402-013-1735-4. [DOI] [PubMed] [Google Scholar]
- 16.Georgiadis GM. Combined anterior and posterior approaches for complex tibial plateau fractures. J Bone Joint Surg Br. 1994;76:285–289. [PubMed] [Google Scholar]
- 17.Lobenhoffer P, Gerich T, Bertram T, Lattermann C, Pohlemann T, Tscheme H. [Particular posteromedial and posterolateral approaches for the treatment of tibial head fractures] . Unfallchirurg. 1997;100:957–967. doi: 10.1007/s001130050218. [DOI] [PubMed] [Google Scholar]
- 18.Hoppenfeld S, deBoer P. Surgical Exposures in Orthopaedics. Philadelphia: JB Lippincott; 1984. [Google Scholar]
- 19.Padanilam TG, Ebraheim NA, Frogameni A. Meniscal detachment to approach lateral tibial plateau fractures. Clin Orthop Relat Res. 1995:192–198. [PubMed] [Google Scholar]
- 20.Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res. 1993:87–100. [PubMed] [Google Scholar]
- 21.Kenneth AE. Split depression posterolateral tibial plateau fracture: direct open reduction and internal fixation. Tech Knee Surg. 2005;4:257–263. [Google Scholar]
- 22.Carlson DA. Posterior bicondylar tibial plateau fractures. J Orthop Trauma. 2005;19:73–78. doi: 10.1097/00005131-200502000-00001. [DOI] [PubMed] [Google Scholar]
- 23.De Boeck H, Opdecam P. Posteromedial tibial plateau fractures. Operative treatment by posterior approach. Clin Orthop Relat Res. 1995:125–128. [PubMed] [Google Scholar]
- 24.Brunner A, Honigmann P, Horisberger M, Babst R. Open reduction and fixation of medial Moore type II fractures of the tibial plateau by a direct dorsal approach. Arch Orthop Trauma Surg. 2009;129:1233–1238. doi: 10.1007/s00402-009-0841-9. [DOI] [PubMed] [Google Scholar]
- 25.Zeng ZM, Luo CF, Putnis S, Zeng BF. Biomechanical analysis of posteromedial tibial plateau split fracture fixation. Knee. 2011;18:51–54. doi: 10.1016/j.knee.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 26.Fernandez DL. Anterior approach to the knee with osteotomy of the tibial tubercle for bicondylar tibial fractures. J Bone Joint Surg Am. 1988;70:208–219. [PubMed] [Google Scholar]
- 27.Yu B, Han K, Zhan C, Zhang C, Ma H, Su J. Fibular head osteotomy: a new approach for the treatment of lateral or posterolateral tibial plateau fractures. Knee. 2010;17:313–318. doi: 10.1016/j.knee.2010.01.002. [DOI] [PubMed] [Google Scholar]


