Abstract
The associations of dietary patterns with coronary heart disease (CHD) risk remain unclear. Thereby, a meta-analysis was conducted to examine potential relations between dietary patterns and CHD. PubMed and EMBASE databases were searched up to March 2014 for eligible prospective cohort studies regarding the relationships between common dietary patterns and CHD. Random-effects models were applied to calculate the summary relative risk estimates (SRRE) for the highest versus the lowest category of dietary pattern. Sensitivity analyses were conducted and publication bias was assessed using Begg or Egger’s tests. Twelve prospective cohort studies were included involving 409,780 participants and 6298 CHD cases. There was an inverse association between prudent/healthy dietary pattern and CHD risk (SRRE = 0.80, 95% CI: 0.74-0.87, P-value for heterogeneity = 0.497, I2 = 0%). Furthermore, no significant association was observed between western/unhealthy dietary pattern and risk of CHD (SRRE = 1.05, 95% CI: 0.86-1.27, P-value for heterogeneity = 0.007, I2 = 61.9%). However, increased risk was detected between western/unhealthy dietary pattern and CHD in the United States (USA) (SRRE = 1.45, 95% CI: 1.15-1.82, P-value for heterogeneity = 0.930, I2 = 0%). In conclusion, our analysis provides evidence of an inverse association between prudent/healthy dietary pattern and CHD risk, and suggests null association between western/unhealthy dietary pattern and CHD. However, greater adherence to western/unhealthy pattern possibily increases by 45% the risk of CHD in USA. Further efforts are warranted to confirm these findings and clarify the role of dietary patterns and CHD risk.
Keywords: Coronary heart disease, dietary patterns, meta-analysis, nutrition
Introduction
Coronary heart disease (CHD) is the leading cause of death in adults throughout their lifetime, affecting millions of people in both developed and developing countries. Furthermore, it causes substantial mortality and morbidity [1,2]. During the past decades, diagnostic intensity and treatment is improving, but prognosis is still poor. In addition, the rising incidence of CHD is alarming and there are little effective preventive measures against it [3]. In recent decades, the roles of dietary factors in the development of CHD have been received growing attention in epidemiologic investigations. Dietary factors are considered as the modifiable factors for CHD like smoking, physical inactivity, or alcohol [4].
Traditionally, the association of single nutrients with CHD has been widely studied. A major limitation of this approach is the little correlations between intakes of various nutrients or food items. To overcome the limitations of this approach, the studies of dietary patterns emerged, which could yield a more comprehensive understanding of how this complex factor affects the etiology of disease compared with analyzing single nutrient and food [5]. Dietary patterns can be defined either a priori or a posteriori. A posteriori methods derive patterns empirically based on the actual diet in a population, of these methods, factor analysis (FA) and/or principal component analysis (PCA) has reasonable reproducibility and validity compared with other approaches [6,7].
Since 2000, the association between dietary patterns on CHD has been more frequently studied. Furthermore, several prospective cohort studies, which are not prone to recall and selection bias, have explored the influence of dietary patterns on CHD risk [8-18]. However, their findings varied substantially across studies. Hence, to examine the association of dietary patterns with CHD risk, we performed this first meta-analysis of the existing prospective cohort studies on the relationship between dietary patterns and the risk of CHD.
Methods and materials
Literature search strategy
We performed this meta-analysis in accordance with Meta-analysis of Observatio0nal Studies in Epidemiology (MOOSE) guidelines [19]. We searched PubMed and EMBASE databases through March 2014 for the eligible prospective cohort studies that had evaluated the associations between dietary patterns and risk of CHD in humans. The keywords used in this study were: cardiovascular disease, coronary heart disease, myocardial infarction, ischemic heart disease, IHD, CHD, morbidity, incidence, risk, death, mortality, diet, dietary, patterns, factor analysis and principal component analysis. The two reviewers used no language or date restrictions in the searches. Furthermore, we assessed and searched the reference lists of all retrieved publications again for additional relevant publications. We identified articles for eligibility by a full-text review after initially screening by titles or abstracts.
Inclusion and exclusion criteria
Studies would be included in this meta-analysis if they met the following criteria: (1) There were prospective cohort studies that examined the relationship between dietary patterns and CHD in human being; (2) The outcome was risk of CHD, including incidence of CHD and CHD mortality; (3) The study has reported risk estimates (i.e., relative risk RRs or odds ratios ORs) and its variability (i.e., 95% confidence intervals CI). If the study has provided sufficient information (e.g.: raw data and P-value) for estimation, it would be included as well; (4) Food or dietary patterns in studies were examined by factor analysis (FA) and/or principal component analysis (PCA); (5) Only the most recent and informative one was included if there were more than one publications of the same or overlapping cohort.
To minimize error and combine the results, only the patterns sharing most foods with similar factor loadings were identified. In this analysis, we identified two common dietary patterns: Prudent/healthy dietary pattern was characterized by having high loadings of foods such as vegetables, fruits, fish, poultry, whole grains and low-fat dairy. While western/unhealthy dietary pattern tended to have a high intake of processed and/or red meat, refined grains, sweets, desserts, eggs and high-fat diary. Studies with dietary pattern having similar loadings of the foods common to prudent/healthy or western/unhealthy were also included in spite of naming differently [20,21].
The exclusion criteria were (1) The studies were duplicates; (2) They had irrelevant data reported; (3) The studies were methodological studies, experimental studies, narrative reviews, editorial papers, case control or cross-sectional; (4) An identified dietary pattern did not fit into healthy or unhealthy dietary pattern categories; (5) The dietary patterns were not indentified by FA or PCA.
Data extraction
Two independent authors independently conducted literature search and extracted the data from all studies that were in the meta-analysis using an investigator-designed data extraction form. This included information about the first author, year of publication, geographic area, number of CHD cases, sample size, age range, study duration, follow-up duration, number of exposed cases, dietary assessment, identification method, naming dietary patterns, endpoints, RR or OR, 95% CIs, number of food items in Food Frequency Questionnaire (FFQ) and description of healthy and unhealthy dietary pattern adjustment variables. When one study presented different adjustment variables, we used the results from the main multivariable model that included the maximum number of adjusted confounders. The discrepancy in data extraction was resolved by repeating the study review and discussion.
Quality assessment of each study was performed by reporting following crucial components of eligible studies: clear definition of participant characteristics, clear examination of exposure and outcome, study duration, sufficient follow-up duration, person-years of follow-up, no selective loss during follow-up and control for potential confounding factors. If a study did not clearly mention these key points, we considered that it had not been performed, but it’s probably underestimated the reported characteristics.
Statistical analysis
We used summary relative risk estimate (SRRE) for a comparison of the highest with the lowest adherence of each dietary pattern intake type (prudent/healthy and western/unhealthy) in terms of tertiles, quartiles, or quintiles of dietary pattern in the included studies. The random effects meta-analysis models, which take into account within-and between-study variances considering the extent of variation, or heterogeneity, were applied to pool the study results and presented forest plots. Furthermore, we assessed the statistical heterogeneity across studies with a chi-square test (significant with a P-value of < 0.10), and quantified the inconsistencies using the I2 statistic. Values of 25%, 50% and 75% for I2 are defined to demonstrate low, moderate and high levels of heterogeneity, respectively [22].
Some studies provided more than one pattern models (i.e. vegetables, fruits, sweets, meat) that met the inclusion criteria in our meta-analysis for the prudent/healthy or western/unhealthy dietary pattern. The separate risk estimates in individual study were combined to obtain a unique study-specific estimate for this pattern.
Sensitivity analyses were performed to assess the robustness of the effect estimates by excluding one study in turn from the analyses. Publication bias was assessed through the visual inspection of a funnel plot combined with Begg’s rank correlation and Egger’s linear regression test [23]. In addition, to explore potential sources of heterogeneity, subgroup analyses were also conducted on the basis of geographic area, number of cases (≥ 500 or < 500 cases) or participants (≥ 50,000 or < 50,000 persons), follow-up duration (≥ 10 or < 10 years), the number of food items in FFQ (≥ 100 or < 100 items) and whether energy intake was adjusted/unadjusted in studies. All statistical analyses were performed with STATA Statistical Software, version 11.0.
Results
Study selection
The initial search strategy identified 684 papers, of which 563 articles were excluded after screening by abstracts, titles or duplicate articles. Furthermore, 75 papers were excluded because of ecological studies, review articles or studies nutrients, whereas 46 papers were eligible for full text review. 23 articles were excluded because their effect sizes and the corresponding 95% confidence intervals were not reported or could not be estimated due to insufficient information. In addition, twelve papers were excluded because dietary patterns in those studies were not examined by FA/PCA, or the studies were not prospective cohort studies. The studies reported by Maruyama et al. [8] reported risk estimates for men and women individually. Thus, it was considered two separate studies when the observed items were pooled respectively. Finally, twelve prospective cohort studies form eleven papers were included in our meta-analysis, which were published between 2000 and 2014 [8-18]. Figure 1 provides a flow summary of our selection proce.
Figure 1.
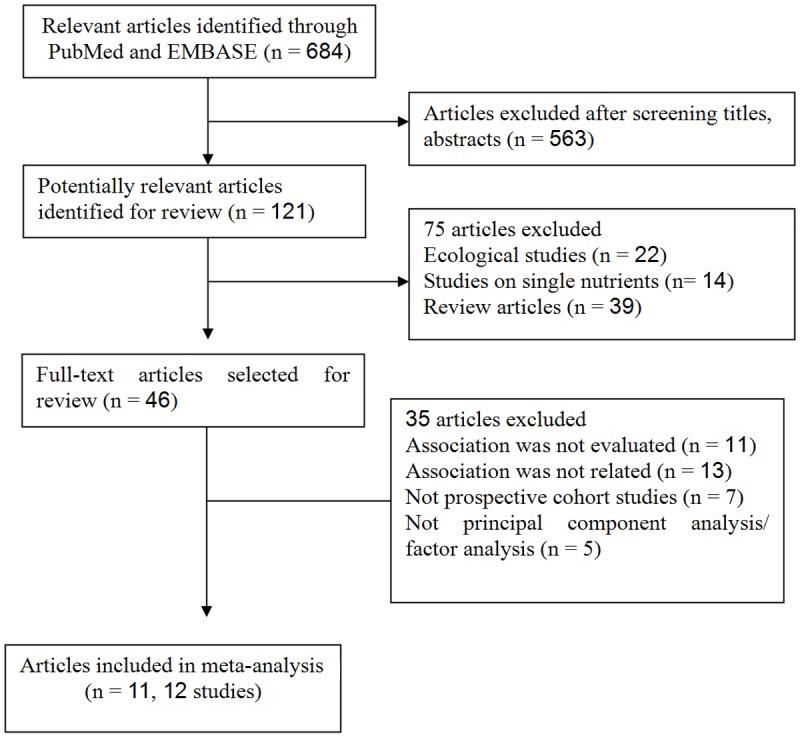
Flow chart of study selection.
Study characteristics
All of the included twelve studies were prospective cohort studies, three studies were conducted in the United States (USA) [11,17,18], three in Japan [8,13], two in Denmark [9,16], one each in Spain [10], Australia [12], Sweden [15] and China [14]. Most of studies in our analysis used FFQ based on self-report or interviewer-administered questionnaires to ascertain dietary information, despite the length of items list in the questionnaire varied across studies. In summary, twelve studies were included in the present analysis with a sample size of 409,780 individuals and 6298 cases of CHD. Table 1 has shown the characteristics of the included studies.
Table 1.
Characteristics of studies included in meta-analysis of dietary patterns and coronary heart disease (CHD) risk
| First author and year | Study location | Casesa/Subjiects | following-up/Period | FFQ list | Dietary pattern | Endpoints | RR (95% CI)/Trend | P | Adjustments |
|---|---|---|---|---|---|---|---|---|---|
| Maruyama 2013 men [8] | Japan | 272/26598 | 12.6/1998-2003 | 40 | Vegetable | CHD mortality | 0.73 (0.49-1.08) | 0.150 | Age, smoking, BMI, total energy intake, walking time, hours of sports, education, perceived mental stress, sleep duration, history of hypertension and diabetes |
| Animal food | CHD mortality | 0.72 (0.48-1.08) | 0.140 | ||||||
| Maruyama 2013 women [8] | Japan | 207/37439 | 12.6/1998-2003 | 40 | Vegetable | CHD mortality | 0.67 (0.43-1.06) | 0.050 | |
| Animal food | CHD mortality | 0.73 (0.42-1.26) | 0.380 | ||||||
| Stricker 2013 [9] | Denmark | 1843/40011 | 13/1993-2008 | 79 | Prudent | CHD incidence | 0.87 (0.75-1.00) | 0.058 | Age, gender, smoking, BMI, energy, education, type II diabetes, waist-hip-ratio, PA, blood pressure |
| Western | CHD incidence | 0.91 (0.76-1.08) | 0.342 | ||||||
| Guallar-Castillón 2012 [10] | Spain | 606/40757 | 11/1992-2004 | Mediterranean | CHD incidence | 0.73 (0.57-0.94) | 0.013 | Age, sex, smoking, BMI, energy intake, PA, center, hypercholesterolemia, diabetes, hypertension, cancer, waist, menopausal status, oral contraceptives, hormone replacement therapy, education | |
| Western | CHD incidence | 0.86 (0.60-1.24) | 0.510 | ||||||
| Nettleton 2009 [11] | USA | 207/5316 | 4.6/2000-2007 | 120 | Whole Grains and Fruit | CHD incidence | 0.63 (0.34-1.16) | 0.050 | Age, sex, smoking, energy intake, PA, race-ethnicity, education, study center, weekly dietary supplement use |
| Harriss 2007 [12] | Australia | 407/40653 | 10.4/1990-2003 | 121 | Mediterranean foods | IHD mortality | 0.59 (0.39-0.89) | 0.030 | Sex, smoking, BMI, total energy intake, PA, country of birth, education, waist-to-hip ratio, social isolation, dietary factors, CVD history, and family history of CVD, diabetes, hypertension |
| Vegetables | IHD mortality | 1.02 (0.73-1.42) | 0.710 | ||||||
| Fresh fruit | IHD mortality | 0.82 (0.60-1.11) | 0.360 | ||||||
| Meat | IHD mortality | 0.85 (0.60-1.21) | 0.650 | ||||||
| Shimazu 2007 [13] | Japan | 181/40547 | 7/1994-2001 | 40 | Japanese | CHD mortality | 0.82 (0.52-1.29) | 0.290 | Age, sex, smoking, BMI, total energy intake, walking duration, education, History of hypertension |
| Animal food | CHD mortality | 1.50 (0.95-2.37) | 0.050 | ||||||
| Cai 2007 [14] | China | 77/74942 | 5.7/1996-2004 | 71 | Vegetable-rich | CHD mortality | 1.10 (0.61-1.99) | 0.504 | Age, smoking, BMI, education, marriage, income per person, alcohol consumption, tea consumption, ginseng intake, PA, energy expenditure |
| Fruit-rich | CHD mortality | 0.71 (0.33-1.53) | 0.550 | ||||||
| Meat-rich | CHD mortality | 1.58 (0.81-3.08) | 0.176 | ||||||
| Akesson 2007 [15] | Sweden | 308/24444 | 6.2/1997-2003 | 96 | Health food | Myocardial infarction incidence | 0.58 (0.39-0.88) | NR | Age, smoking, energy intake, PA, educational achievement, family history of MI, hormone therapy, aspirin, waist to hip ratio, cholesterol level, hypertension |
| Osler 2002 [16] | Denmark | 280/5834 | 13/1982-1996 | 28 | Healthy food index | CHD incidence | 1.21(0.80-1.82) | 0.229 | Smoking, BMI, exercise, alcohol intake, education |
| Fung 2001 [17] | USA | 821/69017 | 12/1984-1996 | 116 | Prudent | CHD incidence | 0.76 (0.60-0.98) | 0.030 | Age, smoking, BMI, caloric intake, hormone replacement therapy, PA, period, aspirin, family history, hypertension, multivitamin and vitamin E |
| Western | CHD incidence | 1.46 (1.07-1.99) | 0.020 | ||||||
| Hu 2000 [18] | USA | 1089/44875 | 8/1986-1994 | 131 | Prudent | CHD incidence | 0.75 (0.59-0.95) | 0.020 | Age, smoking, BMI, energy intake, PA, parental history of MI before age 60, multivitamin and vitamin E, alcohol, history of hypertension, profession, cereal fiber, folate intake |
| Western | CHD incidence | 1.43 (1.01-2.01) | 0.004 |
Number of cases in study;
IHD: ischemic heart disease; CVD: cardiovascular disease; USA: the United States; FFQ: Food Frequency Questionnaire; NR: not reported; BMI: body mass index; PA: physical activity.
Prudent/healthy dietary patterns and CHD risk
The overall meta-analysis results are presented in Table 2. The pooled results showed an inverse association between prudent/healthy diet pattern and CHD risk (SRRE = 0.80, 95% CI: 0.74-0.87), and little variability was observed (P-value for heterogeneity = 0.497, I2 = 0%) (Table 2; Figure 2). Furthermore, similar inverse associations were found in the subgroup analyses. The Begg (P = 0.837) and Egger (P = 0.382) tests, as well as visual inspection of the funnel plot (not shown), did not suggest a publication bias. Furthermore, further sensitivity test by exclusion each study at a time suggested that no single study could materially influence the overall results in our meta-analysis, with a narrow range from 0.75 (95% CI: 0.67-0.82) to 0.80 (95% CI: 0.73-0.86).
Table 2.
Summary of meta-analysis results for dietary patterns (high intake vs. low intakea) and coronary heart disease (CHD) risk
| Analysis specifications | Studies | SRRE (95% CI) | P b | I2 |
|---|---|---|---|---|
| Prudent/health dietary pattern | ||||
| CHD risk | 12 | 0.80 (0.74-0.87) | 0.497 | 0 |
| USA | 3 | 0.75 (0.63-0.88) | 0.854 | 0 |
| Europe | 4 | 0.82 (0.65-0.99) | 0.104 | 30.7 |
| Asia | 4 | 0.72 (0.62-0.97) | 0.767 | 0 |
| Cases < 500 | 8 | 0.80 (0.73-0.89) | 0.521 | 0 |
| Cases ≥ 500 | 4 | 0.79 (0.67-0.92) | 0.326 | 13.3 |
| Participants < 50,000 | 7 | 0.81 (0.72-0.91) | 0.221 | 27.2 |
| Participants ≥ 50,000 | 5 | 0.75 (0.63-0.89) | 0.843 | 0 |
| Follow-up duration < 10 years | 5 | 0.74 (0.62-0.87) | 0.596 | 0 |
| Follow-up duration ≥ 10 years | 7 | 0.82 (0.74-0.91) | 0.380 | 6.3 |
| FFQ < 100 items | 7 | 0.76 (0.66-0.88) | 0.905 | 0 |
| FFQ ≥ 100 items | 4 | 0.82 (0.71-0.96) | 0.232 | 0 |
| Adjustment with energy | 10 | 0.78 (0.66-0.88) | 0.761 | 0 |
| Adjustment without energy | 2 | 1.08 (0.79-1.47) | 0.405 | 0 |
| Western/unhealthy dietary pattern | ||||
| CHD risk | 9 | 1.05 (0.86-1.27) | 0.007 | 61.9 |
| Europe | 2 | 0.90 (0.77-1.06) | 0.784 | 0 |
| USA | 2 | 1.45 (1.15-1.82) | 0.930 | 0 |
| Asia | 4 | 1.03 (0.67-1.59) | 0.035 | 65.1 |
| Cases < 500 | 5 | 1.12 (0.85-1.48) | 0.011 | 73.1 |
| Cases ≥ 500 | 4 | 0.98 (0.71-1.34) | 0.058 | 56.2 |
| Participants < 50,000 | 5 | 1.04 (0.83-1.80) | 0.045 | 59.0 |
| Participants ≥ 50,000 | 4 | 1.04 (0.68-1.61) | 0.014 | 71.9 |
| Follow-up duration < 10 years | 3 | 0.92 (0.75-1.13) | 0.054 | 54.0 |
| Follow-up duration ≥ 10 years | 6 | 1.05 (0.86-1.27) | 0.962 | 0 |
| FFQ < 100 items | 5 | 0.98 (0.75-1.29) | 0.063 | 55.3 |
| FFQ ≥ 100 items | 3 | 1.22 (0.87-1.71) | 0.046 | 67.6 |
| Adjustment with energy | 8 | 1.02 (0.83-1.25) | 0.007 | 63.7 |
| Adjustment without energy | 1 | 1.58 (0.81-3.08) | - | - |
The intake contrast (i.e., exposure vs. referent group) for each study is reported in Table 1.
P: P-value for heterogeneity;
SRRE: summary relative risk estimate; 95% CI: 95% confidence intervals.
Figure 2.
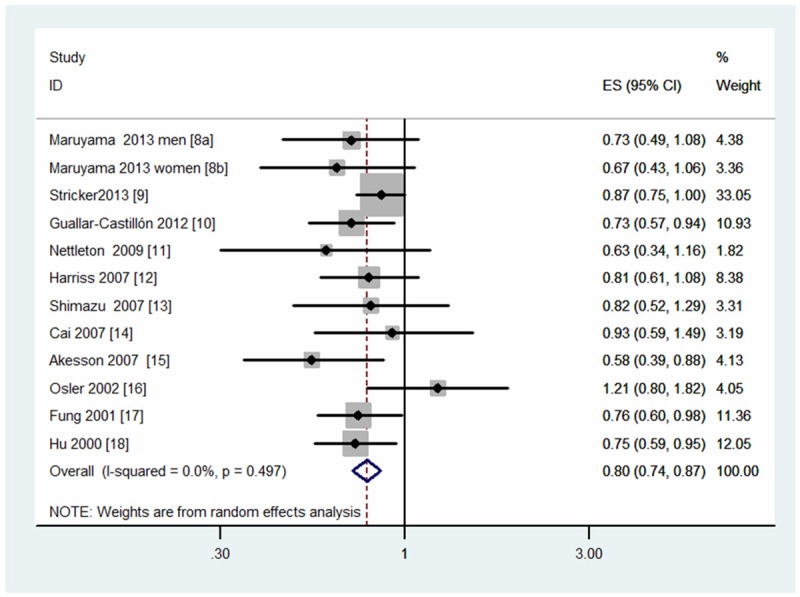
Meta-analysis of studies that examined the associations of prudent/health dietary pattern with coronary heart disease (CHD) risk.
Western/unhealthy dietary patterns and CHD risk
The pooled results indicated that there was no evidence of a difference in the risk of CHD in the highest category compared with the lowest category of western/unhealthy diet pattern (SRRE = 1.05, 95% CI: 0.86-1.27). Substantial heterogeneity was observed between studies (P-value for heterogeneity = 0.007, I2 = 61.9%) (Table 2; Figure 3). No significant summary association was observed in most of subgroup analyses. To be noted, summarized results from a limited number of studies showed a positive association between CHD risk and western/unhealthy pattern in USA (SRRE = 1.45, 95% CI: 1.15-1.82; P-value for heterogeneity = 0.930, I2 = 0%) (Table 2).
Figure 3.
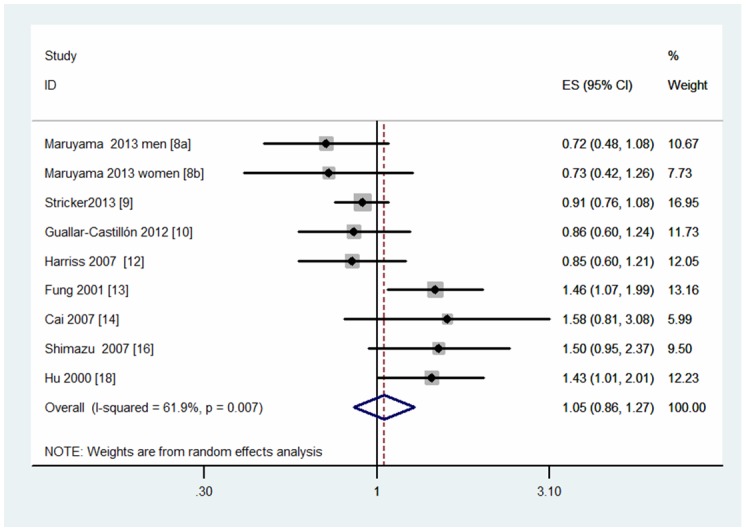
Meta-analysis of studies that examined the associations of western/unhealthy dietary pattern with coronary heart disease (CHD) risk.
Visual inspection of the funnel plot (not shown) did not suggest substantial asymmetry. There was no statistical evidence of publication bias based on the Begg’s rank correlation (P = 0.754) and the Egger’s linear test (P = 0.541). None of any single study would affect the overall estimates of western/unhealthy dietary pattern and CHD risk, and the results indicated by sensitivity analyses ranged between 0.90 (95% CI: 0.79-1.02) and 0.96 (95% CI: 0.85-1.08).
Subgroup analyses
Subgroup analyses were conducted to examine the stability of our overall findings (Table 2). The associations of dietary patterns with risk of CHD were similar in most of our subgroup analyses, which were defined by study location, number of cases or participants, follow-up duration, number of food items in FFQ, and whether energy intake was adjusted in models.
Discussion
It has been suggested that dietary habits play a vital role in the development of CHD. Given the complex interaction between intakes of various nutrients or food items, and that nutrients and foods could never be eaten in isolation, The results revealing the effects through individual foods or nutrients consumption on a given health outcome may be spurious resulting in masking true associations [5,24]. Recently, there has been growing attention in the identification of dietary patterns, representing a combination of nutrients and foods, as an alternative or complementary approach to single-food/nutrient analysis in relation to risk of disease or death. The study examined dietary patterns has the advantage of studying the effect of the whole diet and may be a better predictor of health outcomes than analyzing single nutrient or food [25]. Up to date, considerable controversy exists regarding the associations of dietary patterns with CHD risk.
Therefore, we performed this fist meta-analysis of the existing prospective cohort studies on the associations of dietary patterns with risk of CHD. Twelve prospective cohort studies were included in our analysis with a total of 409,780 participants and 6298 cases of CHD. The summarized findings showed that greater adherence to prudent/healthy dietary pattern had an inverse association with CHD risk. However, there was an absence of significant association between western/unhealthy dietary pattern and risk of CHD. The findings were consistent with most of our subgroup analyses. To be noted, we found that higher adherence to western/unhealthy pattern was associated with 45% increased risk of CHD in USA.
Substantial heterogeneity was detected across studies of western/unhealthy pattern compared with prudent/healthy pattern. This might be caused by variability among the study populations, follow-up period, analytic methodology, dietary assessment method and adjustment for confounding factors. Based on our subgroups by geographical region, number of cases or participants, follow-up duration, number of food items in FFQ as well as adjustment for energy intake or not, little heterogeneity was observed among studies conducted in Europe and USA, and studies with follow-up period more than 10 years. In addition, our sensitivity analyses indicated that no individual study had a particularly large influence on the pooled estimates. Furthermore, there was no evidence of publication bias either with the Begg’s or Egger’s tests in the present study.
Considering the number and description of dietary patterns identified has varied widely, we identified two common dietary patterns named prudent/healthy or western/unhealthy dietary pattern in our analysis, which shares most foods with similar factor loadings. The dietary patterns could be identified according to several approaches including FA, PCA, cluster analysis, reduced rank regression, dietary scores and so on. Of these methods, FA/PCA used to derive dietary patterns has long term reproducibility, stability and validity compared with other approaches [5,7]. Thereby, we only included the studies of FA/PCA as the dietary patterns identification method to could minimize the risk of bias and combine the result accurately.
High intakes of fresh fruits, vegetables, cereals, fish and olive oils are defining characteristics of the prudent/healthy dietary pattern. Because this pattern is rich in vitamins, minerals, antioxidants, fiber, monounsaturated fatty acids and n-3 fatty acids, it seems protective in people’s cardiac health. The prudent/healthy pattern was found to be associated with a lower risk of CHD. The underlying mechanism could be favorably correlated with facilitating weight maintenance, markers of inflammation and endothelial dysfunction caused by greater adherence to the prudent pattern [17]. Furthermore, other biological mechanisms like lipid abnormalities or effects on oxidative stress, systolic and diastolic blood pressure rise, arrhythmias, and insulin sensitivity would be a possible explanation for this finding [25].
A frequent consumption of red meat, processed meat, refined grains, sweets, French fries, desserts, eggs and high high-fat dairy products characterizes the western/unhealthy dietary pattern. No significant association was found between the western dietary pattern and CHD. The pooled risk estimate was in line with most results emerging from the included studies. One explanation may be that cardioprotective roles mediated primarily through plants are reduced because of greater intakes of meat products in place of more beneficial plant foods in diet [26].
However, a positive association was observed between adherence to western dietary pattern and CHD risk in USA. The underlying mechanism involved in this association is uncertain. One plausible reason is the characteristics of the typical American diet by containing more red meat, high-fat dairy products and other animal products, less fish and plant-rich foods [27]. Many studies have demonstrated some foods or nutrients consumption of this pattern were significantly related to an increased CHD risk, such as heme iron, red meat, whole milk and a high glycemic index from carbohydrate-loading foods [28-31]. In addition, we could not exempt the possibility that the associations could be explained by terms of genetic background and lifestyle in this area. Noticeably, the studies included in this model were limited. Therefore, the results should be interpreted with caution.
Several potential limitations in our current study should be acknowledged. First, although most included studies were adjusted for a wide range of dietary and lifestyle variables and established risk factor, we could not exempt the possibility that other variables are relevant to the observed outcomes. Second, there was substantial heterogeneity across studies that examined unhealthy dietary patterns, though we were able to partly find that geographic region and follow-up duration are potential source of heterogeneity through subgroup analyses. In addition, all the included studies in our analysis were prospective cohort designed. However, differences among follow-up period, measurement of CHD end point, etc, may lead us to misreport the true associations of dietary patterns on CHD risk.
In conclusion, our meta-analysis on the basis of 409,780 participants provides evidence of an inverse association between prudent/healthy dietary pattern and CHD risk, and suggests null association between western/unhealthy dietary pattern and risk of CHD. However, our findings indicates that greater adherence to western/unhealthy pattern possibily increases by 45% the risk of CHD in USA. Further studies are warranted to confirm these findings and clarify the role of dietary patterns and CHD risk.
Disclosure of conflict of interest
None.
References
- 1.Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol. 2012;60:1207–16. doi: 10.1016/j.jacc.2012.03.074. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U. S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–32. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 3.Rong Y, Chen L, Zhu T, Song Y, Yu M, Shan Z, Sands A, Hu FB, Liu L. Egg consumption and risk of coronary heart disease and stroke: dose-response meta-analysis of prospective cohort studies. BMJ. 2013;346:e8539. doi: 10.1136/bmj.e8539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dontas AS, Zerefos NS, Panagiotakos DB, Vlachou C, Valis DA. Mediterranean diet and prevention of coronary heart disease in the elderly. Clin Interv Aging. 2007;2:109–15. doi: 10.2147/ciia.2007.2.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, Hu FB. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94:1088–96. doi: 10.3945/ajcn.111.018978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Bertuccio P, Rosato V, Andreano A, Ferraroni M, Decarli A, Edefonti V, La Vecchia C. Dietary patterns and gastric cancer risk: a systematic review and meta-analysis. Ann Oncol. 2013;24:1450–8. doi: 10.1093/annonc/mdt108. [DOI] [PubMed] [Google Scholar]
- 8.Maruyama K, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A JACC Study Group. Dietary patterns and risk of cardiovascular deaths among middle-aged Japanese: JACC Study. Nutr Metab Cardiovasc Dis. 2013;23:519–27. doi: 10.1016/j.numecd.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Stricker MD, Onland-Moret NC, Boer JM, van der Schouw YT, Verschuren WM, May AM, Peeters PH, Beulens JW. Dietary patterns derived from principal component-and k-means cluster analysis: long-term association with coronary heart disease and stroke. Nutr Metab Cardiovasc Dis. 2013;23:250–6. doi: 10.1016/j.numecd.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Guallar-Castillón P, Rodríguez-Artalejo F, Tormo MJ, Sánchez MJ, Rodríguez L, Quirós JR, Navarro C, Molina E, Martínez C, Marín P, Lopez-Garcia E, Larrañaga N, Huerta JM, Dorronsoro M, Chirlaque MD, Buckland G, Barricarte A, Banegas JR, Arriola L, Ardanaz E, González CA, Moreno-Iribas C. Major dietary patterns and risk of coronary heart disease in middle-aged persons from a Mediterranean country: the EPIC-Spain cohort study. Nutr Metab Cardiovasc Dis. 2012;22:192–9. doi: 10.1016/j.numecd.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Nettleton JA, Polak JF, Tracy R, Burke GL, Jacobs DR Jr. Dietary patterns and incident cardiovascularm disease in the Multi- Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2009;90:647–54. doi: 10.3945/ajcn.2009.27597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harriss LR, English DR, Powles J, Giles GG, Tonkin AM, Hodge AM, Brazionis L, O’Dea K. Dietary patterns and cardiovascular mortality in the Melbourne Collaborative Cohort Study. Am J Clin Nutr. 2007;86:221–9. doi: 10.1093/ajcn/86.1.221. [DOI] [PubMed] [Google Scholar]
- 13.Shimazu T, Kuriyama S, Hozawa A, Ohmori K, Sato Y, Nakaya N, Nishino Y, Tsubono Y, Tsuji I. Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int J Epidemiol. 2007;36:600–9. doi: 10.1093/ije/dym005. [DOI] [PubMed] [Google Scholar]
- 14.Cai H, Shu XO, Gao YT, Li H, Yang G, Zheng W. A prospective study of dietary patterns and mortality in Chinese women. Epidemiology. 2007;18:393–401. doi: 10.1097/01.ede.0000259967.21114.45. [DOI] [PubMed] [Google Scholar]
- 15.Akesson A, Weismayer C, Newby PK, Wolk A. Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women. Arch Intern Med. 2007;167:2122–7. doi: 10.1001/archinte.167.19.2122. [DOI] [PubMed] [Google Scholar]
- 16.Osler M, Helms Andreasen A, Heitmann B, Høidrup S, Gerdes U, Mørch Jørgensen L, Schroll M. Food intake patterns and risk of coronary heart disease: a prospective cohort study examining the use oftraditional scoring techniques. Eur J Clin Nutr. 2002;56:568–74. doi: 10.1038/sj.ejcn.1601360. [DOI] [PubMed] [Google Scholar]
- 17.Fung TT, Willett WC, Stampfer MJ, Manson JE, Hu FB. Dietary patterns and the risk of coronary heart disease in women. Arch Intern Med. 2001;161:1857–62. doi: 10.1001/archinte.161.15.1857. [DOI] [PubMed] [Google Scholar]
- 18.Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000;72:912–21. doi: 10.1093/ajcn/72.4.912. [DOI] [PubMed] [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 20.Alhazmi A, Stojanovski E, McEvoy M, Garg ML. The association between dietary patterns and type 2 diabetes: a systematic review and meta-analysis of cohort studies. J Hum Nutr Diet. 2014;27:251–60. doi: 10.1111/jhn.12139. [DOI] [PubMed] [Google Scholar]
- 21.Brennan SF, Cantwell MM, Cardwell CR, Velentzis LS, Woodside JV. Dietary patterns and breast cancer risk: a systematic review and meta-analysis. Am J Clin Nutr. 2010;91:1294–302. doi: 10.3945/ajcn.2009.28796. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 23.Li F, An SL, Zhou Y, Liang ZK, Jiao ZJ, Jing YM, Wan P, Shi XJ, Tan WL. Milk and dairy consumption and risk of bladder cancer: a meta-analysis. Urology. 2011;78:1298–305. doi: 10.1016/j.urology.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Magalhaes B, Peleteiro B, Lunet N. Dietary patterns and colorectal cancer:systematic review and meta-analysis. Eur J Cancer Prev. 2012;21:15–23. doi: 10.1097/CEJ.0b013e3283472241. [DOI] [PubMed] [Google Scholar]
- 25.Tourlouki E, Matalas AL, Panagiotakos DB. Dietary habits and cardiovascular disease risk in middle-aged and elderly populations: a review of evidence. Clin Interv Aging. 2009;4:319–30. doi: 10.2147/cia.s5697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trichopoulos D, Lagiou P. Dietary patterns and mortality. Br J Nutr. 2001;85:133–4. doi: 10.1079/bjn2000282. [DOI] [PubMed] [Google Scholar]
- 27.Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000;72:912–21. doi: 10.1093/ajcn/72.4.912. [DOI] [PubMed] [Google Scholar]
- 28.Ascherio A, Willett WC, Rimm EB, Giovannucci EL, Stampfer MJ. Dietary iron intake and risk of coronary heart disease among men. Circulation. 1994;89:969–74. doi: 10.1161/01.cir.89.3.969. [DOI] [PubMed] [Google Scholar]
- 29.Snowdon DA, Phillips RL, Fraser GE. Meat consumption and fatal ischemic heart disease. Prev Med. 1984;13:490–500. doi: 10.1016/0091-7435(84)90017-3. [DOI] [PubMed] [Google Scholar]
- 30.Fraser GE, Sabate J, Beeson WL, Strahan TM. A possible protective effect of nut consumption on risk of coronary heart disease. The Adventist Health Study. Arch Intern Med. 1992;152:1416–24. [PubMed] [Google Scholar]
- 31.Fraser GE. Diet and coronary heart disease: beyond dietary fats and low-density-lipoprotein cholesterol. Am J Clin Nutr. 1994;59:1117S–23S. doi: 10.1093/ajcn/59.5.1117S. [DOI] [PubMed] [Google Scholar]


