Abstract
Objective: To investigate the changes in expression profile of circulating microRNAs (miRNAs) and the regulatory effect of atrial fibrilation (AF)-related miRNAs on ion channels. Methods: 112 patients with AF were assigned into observation group, and another 112 non-AF people were assigned into control group. Total plasma RNAs were extracted from patients’ blood samples. Differentially expressed miRNA-1s were transfected into primary-cultured neonatal rat cardiac myocytes. Results: Compared with control group, significant differences were observed in 15 kinds of miRNAs in observation group. Down-regulation of the expression of miRNAs included hsa-miR-328, hsa-miR-145, hsa-miR-222, hsa-miR-1, hsa-miR-162, hsa-miR-432, and hsa-miR-493b; Up-regulation of the expression included hsa-miR634, hsa-miR-664, hsa-miR-9, hsa-miR-152, hsa-miR-19, hsa-miR-454, hsa-miR-146, and hsa-miR-374a. The expression level of CACNB2 protein in miRNA-1 group was significantly lower than that in blank control group, negative control group, MTmiRNA-1 group, AMO-1 group and miRNA-1+AMO-1 cotransfection group (P < 0.05), while in AMO-1 group, the expression level of CACNB2 protein was significantly higher than that in other groups (P < 0.05). These results indicated that transfected miRNA-1 could significantly inhibit the expression of CACNB2 protein. Conclusions: Circulating miRNAs can be used in studies concerning on the regulation mechanism of the occurrence and development of AF. MiRNA-1 can decrease the intracellular Ca2+ concentration and prevent the AF.
Keywords: Atrial fibrillation, miRNAs, expression profile of gene, cardiac myocyte, L-type Ca2+ channel
Introduction
Atrial fibrillation (AF) is the most common chronic sustained arrhythmia, of which the occurrence rate increases with age. A sample survey demonstrated that the prevalence of AF in Chinese adults was 0.77%, and in people over 80, the prevalence was 5%~15% [1,2]. AF can aggravate the heart failure, induce ventricular arrhythmia, and increase the risk of stroke and the rate of mortality or disability [3]. However, at present, the mechanism of AF is not fully understood, and the treatment approach is still limited. A lot of hypotheses have been raised to explain the mechanism of the occurrence and maintenance of AF, and the classical theories including multiple-wavelet hypothesis and atrial remodeling (AR) theory. The occurrence of multiple-wavelet was caused by the differences in effective refractive period (ERP) and atrial conduction velocity, which could result in the occurrence of AF. Atrial remodeling includes atrial electrical remodeling (AER) and atrial anatomical remodeling (AAR). AER indicates the shortening of atrial action potential duration (APD), ERP and the decrease of atrial conduction velocity. Changes in structure, function and characteristic of atrial ion channels are thought to be the pivotal mechanism of AER. There are several kinds of Ca2+ channels in atrial tissue, in which L-type Ca2+ channel plays an important role in regulating the rhythm of atrial and the change in atrial APD [4]. Intracellular calcium overload is regarded as a trigger of atrial remodeling. During the course of AF, calcium overload in atrial myocyte can increase the L-type voltage-dependent calcium channel current (Ica-L), elevate the plateau of action potential (AP), contribute to the intracellular calcium overload, and shorten the wavelength of atrial signal conduction, which can form a vicious circle and result in the occurrence of AF. Atrial fibrosis and the apoptosis of atrial myocytes can contribute to the atrial enlargement, which suggests the occurrence of AER. Conversely, AER can also sustain the progression of AF.
MicroRNAs (miRNAs), a kind of endogenous small non-protein-coding RNA, contain 22 nucleotides or so. The expression of target gene is inhibited by the combination of miRNAs and the 3’-untranslated region (3’-UTR) of target RNA, which performs in an incompletely complementary manner [5]. Previous studies reported that AR was partly regulated by miRNAs and some kinds of miRNAs were associated with the regulation of the expression of Ca2+ channel gene. However, few researches have been conducted to study the circulating miRNAs in AF patients [6] and further studies are still necessary. In our study, in order to supply more details about the correlation between miRNAs and AF, we analyzed the changes of the expression profiles in AF patients and the effect of AF-related circulating miRNAs on the Ca2+ channels.
Subjects and methods
Subjects
During May. 2011 to Apr. 2013, we conducted a cardiovascular survey about the occurrence and risk factors of AF in Chongming County. A total of 18 communities were randomly selected, and necessary information was obtained from local residents whose ages were over 20 years old. A total of 122 AF patients (67 men, 55 women) included 31 paroxysmal AF and 91 persistent AF (including permanent AF) were assigned into observation group. Another 112 non-AF people (67 men, 55 women) were assigned into control group. Patients in both groups were Han nationality and had no kinships between each other. All of them were 1:1 matched according to their age, sex, race, smoking history, urate, CRP, district and concomitant diseases (diabetes, hypertension, coronary heart disease, valve disease) etc.
Experiment animals
A total of 300 SD rats were obtained from shanghai experimental animal center.
Extraction and test of miRNA
A total of 6 ml fasting venous blood sample was taken from each patient in the morning and put into EDTA anticoagulative tube, placed under room temperature for 30 min. The plasma was collected by centrifuge (3000 rpm, 10 min) and preserved in refrigerator (-80°C). The plasma samples of 91 persistent AF patients were randomly divided into 3 subgroups (30, 30, and 31 respectively), and 31 paroxysmal AF patients were regarded as one subgroup. The plasma samples in control group were randomly divided into 4 subgroups (30, 30, 31, and 31 respectively). Four couples of plasma sample mixed pools were formed as follows: (1) plasma samples of 30 persistent AF patients + 30 plasma samples of control subgroup; (2) plasma samples of another 30 persistent AF patients + 30 plasma samples of control subgroup; (3) plasma samples of 31 persistent AF patients+31 plasma samples of control subgroup; (4) plasma samples of 31 paroxysmal AF patients + 31 plasma samples of control subgroup.
Total RNA of each plasma sample mixed pool was extracted following the specification of mirVanaTMPARISTM kit (Applied Biosystem Company, USA). The concentration and purity of RNA were tested by ND1000Spectrophometer (NanoDrop company, USA) and the integrity of RNA was examined by means of 1.2% agarose gel electrophoresis, and then these RNAs were preserved in refrigerator (-80°C). All these operations were performed without the pollution of RNA enzyme.
Gene chips test
Separated RNAs of each blood sample mixed pool were marked following the specification of miRCURY™HY3™/HY5™ Power marker kit, and then hybridization was conducted by using miRCURYTM LNA chip (v.16.0 Exiqon company). Samples from the same mixed pool would be tested for 4 times on each gene chip [7].
Prediction of the target gene of miRNA
In AF group, miRNA-1 was managed by Targetscan software to predict whether the subunits of L-type Ca2+ channel were the target genes of miRNA-1 or not. Our results demonstrated that the gene of CACNB2 was the target gene of miRNA-1 [8].
Culture of experiment animals’ cardiac myocytes and purity identification
A total of 300 newborn (1~3 days) SD rats’ hearts were separated under aseptic condition and cut into fragments (1 mm3) after being washed by DMEM, and then these fragments were dealt with trypsin. After the process of filtration (200 mm filter screen) and centrifugation (3000 r/min, 2 min), all fragments were transferred into 15% DMEM sterile culture of calf serum to be incubated, and then they were put into the incubator (5% CO2, saturated humidity, 37°C). Two hours later, 8-deoxidization bromine glycoside was added into the culture medium, and 48 hours later, all these fragments were transferred into the non-serum DMEM culture medium. After 24 hours, cell climbing slices were taken out of the incubator. These spare slices were fixed by 40 g/L paraformaldehyde (37°C) for 10 min and then BSA (0.01 g) + triton2100 (1 mL 0.4%) were used to perforate for 1 hour. After being blocked with goat’s serum for 1 hour at 37°C, incubated by Rabbit Anti-Rat α-sarcomeric actin antibody for 2 hours at 37°C and HRP-labeled Goat Anti-Rabbit antibody (Zhongshan Company) was conducted to incubate for 2 hours at 37°C. Substrate DAB2H2O2 was added into the culture medium for incubating (2 hours, 37°C) and hematoxylin staining for 10 min. After each step mentioned above, we used PBS solution for washing. Finally, optical microscope (OLYMPUSIX50 inverted microscope, Olympus Company) was used to observe and take photograph [9].
Transfection of cardiac myocytes
Cultured cardiac myocytes were divided into six groups, (1) for miRNA group, miRNA was transfected into cardiac myocytes; (2) for blank control group, DEPC was added; (3) for negative control group, a section of unrelated miRNA was transfected into cardiac myocytes; (4) for MTmiRNA-1 group, mutant miRNA was transfected into cardiac myocytes; (5) for AMO-1 group, antisense strand of miRNA-1 was transfected into cardiac myocytes; (6) for miRNA-1 and AMO-1 cotransfected group, both miRNA-1 and antisense strand of miRNA-1 were transfected into cardiac myocytes, respectively. Culture medium was changed one day before transfection. In order to famish cardiac myocytes, only DMEM (excluding serum and antibiotics) was added. A total of 1 ml (20 pmol) oligomers (from each group above mentioned) was mixed with LipofectaminTM 2000 (Invitrogen Company) at the proportion of 1:1.5 and incubated under room temperature for 20 min. Then these mixtures were added into cardiac myocytes and put into incubator. Twenty-four hours later, normal culture medium (excluding antibiotics) was used to replace the old one. Another 24 hours later, all these cells could be used for detection [10]. MiRNA, MTmiRNA-1 and the antisense strand of miRNA-1 were obtained from Majorbio Company.
Examination of the β2 subunit of L-type Ca2+ channel
Transfected cardiac myocytes were taken out for cracking, and supernatants were collected into Eppendorf tube after being centrifuged (12500 rpm, 15 min). Then BCA Protein Assay Kit was used to extract and quantify proteins. Western blot (WB) method was performed. After electrophoresis, transmembrane, immunodetection, development and fixation, Image Lab (an agarose image analyzer system) was conducted to achieve semi-quantitative analyse [11].
Statistical analysis
Images were collected after the hybridization of gene chip, and gene scan analysis software was used to analyze the data. Modified value was calculated as initial value subtracted background value. Furthermore, we calculated the mid-value of non-control probe when modified value>50 and regarded the mid-value as a standard factor. All points on the same gene chip were handled by following it. Then the standard values and ratio of miRNAs in two kinds of samples were calculated. If the standard values of observation group were 1.5 times higher or 0.5 times lower than control group, the up-regulation or down-regulation trend was supposed to be significant.
SPSS 15.0 software was conducted to analyze other data. Measurement data with normal distribution were demonstrated as x ± s, and median value was used to evaluate the data with skew distribution. Kolmogorov-Smirnov method was performed for the test of normality and Levene test of homogeneity of variance was also conducted. If measurement data were normally distributed and demonstrated the homogeneity of variance, t test or analysis of variance would be used for statistical analysis; if not, rank-sum test would be selected. Enumeration data were showed by frequency and percent, and evaluated by χ2 test. The statistical significance level was set at 0.05.
Results
Results of plasma RNAs
Electrophoresis strip of RNAs could be seen clearly, and the maximum absorption peak appeared at 280 nm. The ratio of 260 nm/280 nm was between 1.60 and 2.02. The purity of RNA met the requirement for experimental study (Figure 1).
Figure 1.
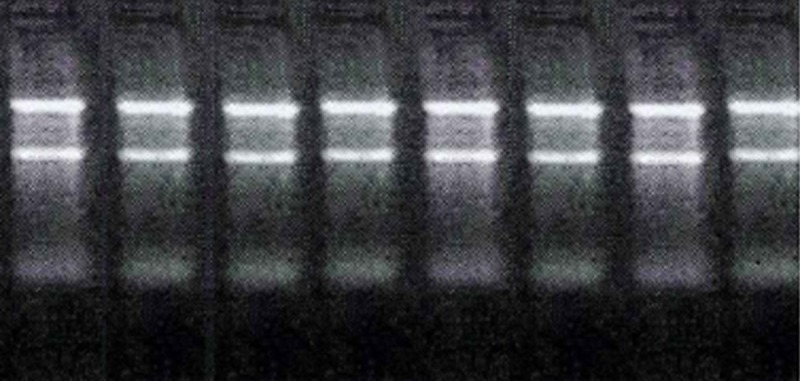
Gel electrophoresis of total RNAs in both observation and control groups.
Differences in the expression of plasma RNAs in both groups
A total of 15 kinds of miRNAs, which were selected from the plasma of paroxysmal and persistent AF patients according to the results of miRCURYTM LNA gene chip, proved to be existing differences in expression. The expression of 8 kinds of miRNAs (hsa-miR-328, hsa-miR-145, hsa-miR-222, hsa-miR-1, hsa-miR-162, hsa-miR-432, hsa-miR-493b, hsa-miR-874) was down-regulated, and significant differences (P< 0.05) were observed in 7 of them except has-miR-874. The expression another 7 kinds of miRNAs (hsa-miR634, hsa-miR-664, hsa-miR-9, hsa-miR-152, hsa-miR-19, hsa-miR-454, hsa-miR-146, hsa-miR-374a) was up-regulated, and significant differences (P< 0.05) were observed in all of them when compared with control group. In a word, significant differences (P< 0.05) were observed in 15 kinds of miRNAs’ expression profiles in both observation and control groups, and details were demonstrated in Table 1 and Figure 2 (The value of miRNAs in 3 subgroups of persistent AF patients and their control groups).
Table 1.
Circulating miRNAs of differential expression in both persistent and paroxysmal AF patients (P< 0.05)
| miRNA | Differential fold | P value | Expression tendency | ||
|---|---|---|---|---|---|
|
| |||||
| Pers-AF | Paro-AF | Pers-AF | Paro-AF | ||
| hsa-miR-328 | 0.4912 | 0.4804 | 0.0321 | 0.0484 | Down-regulated |
| hsa-miR-145 | 0.4256 | 0.3987 | 0.0012 | 0.0234 | Down-regulated |
| hsa-miR-222 | 0.3987 | 0.4021 | 0.0120 | 0.0352 | Down-regulated |
| hsa-miR-162 | 0.2781 | 0.2654 | 0.0465 | 0.0372 | Down-regulated |
| hsa-miR-432 | 0.4781 | 0.4934 | 0.0461 | 0.0372 | Down-regulated |
| hsa-miR-493b | 0.3612 | 0.2987 | 0.0238 | 0.0315 | Down-regulated |
| hsa-miR-1 | 0.382 | 0.400 | 0.0380 | 0.0427 | Down-regulated |
| has-miR634 | 2.870 | 3.245 | 0.0232 | 0.0011 | Up-regulated |
| hsa-miR-664 | 1.825 | 1.938 | 0.0052 | 0.0124 | Up-regulated |
| hsa-miR-9 | 4.687 | 3.214 | 0.0487 | 0.0449 | Up-regulated |
| hsa-miR-152 | 2.278 | 2.059 | 0.0425 | 0.0372 | Up-regulated |
| hs a-mi R-19 | 1.987 | 1.556 | 0.0474 | 0.0363 | Up-regulated |
| hsa-miR-454 | 4.765 | 4.238 | 0.0317 | 0.0293 | Up-regulated |
| hsa-miR-146 | 2.865 | 2.794 | 0.0547 | 0.0473 | Up-regulated |
| hsa-miR-374a | 3.214 | 2.976 | 0.0251 | 0.0198 | Up-regulated |
Figure 2.

Differentially expressed circulating miRNAs in both pers-AF and paro-AF patients compared to non-atrial fibrillation.
Expression level of CANCNB2
Cultured cardiac myocytes of neonatal rats were brown after immunohistochemical staining, which suggested that they were cardiac myocytes indeed. The CANCNB2 miRNA band in miRNA-1 group on the gel image of post-transfection was thinner and lighter than the bands of other groups (Figure 3). Image Lab software was conducted to calculate the ratio of the grey value of RNA band in each group/the grey value of internal reference GAPDH, and results of semi-quantitative analysis demonstrated as following: AMO-1 group: 1.37 ± 0.25; Blank control group: 1.05 ± 0.24; Negative control group: 1.07 ± 0.18; MTmiRNA-1 group: 1.08 ± 0.21; MiRNA-1+AMO-1 cotransfection group: 1.05 ± 0.23, MiRNA-1group: 0.8 ± 0.32. Furthermore, the expression level of CANCNB2 protein in miRNA-1 group was significantly lower than that in other groups (P< 0.05), while in the AMO-1 group, the expression of CANCNB2 protein was significantly higher than that in other groups (P< 0.05) (Figure 3).
Figure 3.

The expression results of CANCNB2 protein. A: AMO-1 group; B: Blank control group; C: Negative control group; D: MTmiRNA-1 group; E: miRNA-1+AMO-1 cotransfection group; F: miRNA-1 group.
Discussion
During the course of AF, atrial muscle vibrates at the speed of 350-600/min without any rhythm, which results in the loss of atrial contraction and promotes the occurrence of serious arrhythmias. Besides, the risk of thrombosis and embolism also influence the prognosis of AF patients. As one of the most common arrhythmias, AF has become a hot and difficult clinical problem, and a lot of therapies have been conducted in the treatment of AF, especially the antiarrhythmic drugs. Up to now, antiarrhythmic drugs are still the major treatment to AF. The definite mechanism of AF is still unknown, while there are many hypotheses including multiple-wavelet hypothesis, focal impulse hypothesis, atrial remodeling and neurohumoral regulation mechanism, etc. However, it is a pity that the efficient drugs which were developed based on these hypotheses haven’t been produced, so it is necessary to find new therapeutic targets of AF. Nowadays, many kinds of miRNAs which were associated with cardiovascular disease (CVD) have been identified, and several miRNAs may be able to influence the progression of AAR and AER on different steps, which affect the occurrence and maintenance of AF, respectively.
Circulating miRNAs, which can be repeatedly and easily extracted from plasma or serum without any injury, are very stable for owning the activity of anti-RNA-hydrolase. During the course of diseases, changes will appear on the expression profiles of miRNAs. Previous studies reported that miRNAs could be regarded as the biomarker of coronary artery disease (CAD), acute myocardial infarction (AMI), pulmonary artery hypertension (PAH) and heart failure (HF) etc [12,13]. The influence of circulating miRNAs on the occurrence, progression and recurrence of AF has been gradually concerned. In our study, an epidemiological investigation was conducted in Chongming County, and the results suggested that 8 kinds of miRNAs (hsa-miR634, hsa-miR-664, hsa-miR-9, hsa-miR-152, hsa-mi R-19, hsa-miR-454, hsa-miR-146, hsa-miR-374a) were up-regulated, while 7 kinds of miRNAs (hsa-miR-328, hsa-miR-145, hsa-miR-222, hsa-miR-1, hsa-miR-162, hsa-miR-432, hsa-miR-493b) were down-regulated in the serum of AF patients. Among these miRNAs, miRNA-328 and miRNA-1 have been studied a lot. Lu et al. [14] found significant up-regulation of miRNA-328 in the atrial tissue of AF patients and experimental AF dogs (AF was triggered by right ventricular pacing), which resulted in the occurrence of AF by regulating the L-type Ca2+ channel. Similarly, in our study, miRNA-328 was also up-regulated significantly. Others reported that the significant increase of miRNA-1 had been observed in AMI rats and was generally associated with ischemic arrhythmia [15], while miRNA-1 decreased in the aorta of hypertension rats [16], which promoted the differentiation of embryonic stem cells to cardiac myocytes, accelerated the apoptosis and inhibited the progression of cardiac hypertrophy [17,18]. Girmatsion et al. [19] found decrease of miRNA-1 in the atrial tissue of AF patients, which was similar to our results (down-regulation of miRNA-1 in Chongming AF patients). Terentyev D et al. [20,21] revealed that miRNA-1 could inhibit the expression of HCN2/HCN4 and down-regulate the expression of KCNJ2 and GJA1, which would slow the velocity of atrial conduction, repolarization and inhibit the occurrence of arrhythmia [20,21]. Wu et al. [22] found down-regulation of miRNA-1 in hypertrophied myocytes and low expression of CANCNB2 in miRNA-1 transfected myocytes, which suggested that miRNA-1 prevented the atrial remodeling by inhibiting the expression of CANCNB2.
In our study, hsa-miR-145 and hsa-miR-222, which were supposed to be associated with endothelial cells, were observed down-regulation [23]. MiRNA-222 was up-regulated on the region of artery balloon injury, while the miRNA-145 was down-regulated. The inhibition of miRNA-222 could prevent the endothelial hyperplasia which resulted from balloon injury, and the same phenomenon could be observed in the recovery of the expression of miRNA-145. Nevertheless, the relations between miRNA-222, miRNA-145 and AF haven’t been studied, so further studies were necessary. In addition, another 11 kinds of miRNAs which were differentially expressed in Chongming AF patients observed in our study hadn’t been reported yet.
AER affects the occurrence and maintenance of AF seriously, which mainly includes the shortening of atrial ERP and APD, the slow of atrial conduction velocity, the increase of discrete rate of refractory period and the decline of rate adaptive [24]. The shortening of APD results from the shortening of plateau. During the action potential plateau, Ca2+ flows into cells through L-type Ca2+ channel which affects the ICaL seriously, while K+ flows out of cells [25]. ICaL increases the intracellular Ca2+ concentration, which triggers the release of Ca2+ from sarcoplasmic reticulum and causes the constriction of myocytes. During the diastole, Ca2+ will be partly taken back to the sarcoplasmic reticulum and the rest may be transferred out with the help of Ca2+ transporters. All above steps form one systolic-diastolic motion, completely.
At present, calcium overload is thought to be a mechanism of the occurrence and maintenaince of AF, which is also an important influence factor in AER [26]. Ca2+ is the central link of the regulation of cardiac electromechanical coupling and could stimulate the constriction of heart under physiological condition, while calcium overload will inhibit the systolic and diastolic function of heart under pathological condition, promote the lipid peroxidation and induce irreversible injury to cardiac myocytes.
The α and β subunits of L-type Ca2+ channel work together to regulate the efflux or influx of Ca2+. Up to now, there are 4 kinds of β subunits (β1~β4) have been found, but only β2 subunit (CACNB2) expresses on cardiac myocytes. CACNB2 regulates the ICaL and the expression of CACNB2 is related with the occurrence of AF. Our study showed that the expression level of CACNB2 increased significantly in AMO-1 group (antisense strand of miRNA-1 was transfected into cardiac myocytes), while the expression level of CACNB2 decreased significantly in miRNA-1 group (P< 0.05). The expression level of miRNA-1 was decreasing in the plasma of AF patients. With the down-regulation of miRNA-1, the expression level of CACNB2 protein increased, which promoted the occurrence of intracellular calcium overload, accelerated the deactivation of L-type Ca2+ channel, decreased the ICaL, resulted in the shortening of action potential plateau and ERP, and led to the onset of AF, eventually [27].
In summary, the changes of expression profiles of plasma miRNAs in AF patients from Chongming County were observed. The down-regulation of miRNA-1 could inhibit the expression of CACNB2, which suggested that the occurrence of AF may be related with the regulation of miRNAs to the CACNB2. Therefore, specific plasma miRNAs may be regarded as new biomarkers of AF. Moreover, with the advance of antisense and gene recombinant technology (exogenous genes are introduced into cells), new cardiovascular drugs which put the miRNAs as a target could be developed to treat AF in the future. However, as the extraction and detection of miRNAs need the participation of professionals and the expense may be pretty expensive. Nowadays, the mechanism of the regulation of miRNA to AF was mostly studied in animal experiment, and only a few studies were conducted in atrial tissues of AF patients obtained from human’s operation or peripheral blood samples. In addition, the regulation mechanism of miRNA is complicated and the function of ion channels is also regulated by different factors. We can only obtain a little information from recent studies. Before the new drugs affecting the expression of specific miRNAs can be widely applied in the treatment of AF, more studies with large subjects and novel technology need to be conducted to clarify the regulation mechanisms of miRNA in AF.
Disclosure of conflict of interest
None.
References
- 1.den Hoed M, Eijgelsheim M, Esko T, Brundel BJ, Peal DS, Evans DM, Nolte IM, Segre AV, Holm H, Handsaker RE. Identification of heart rate-associated loci and their effects on cardiac conduction and rhythm disorders. Nat Genet. 2013;45:621–631. doi: 10.1038/ng.2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guo JH. The new concept of atrial fibrillation. J Clin Elctrocardio. 2010;5:381–391. [Google Scholar]
- 3.Santulli G. Epidemiology of cardiovascular disease in the 21st century: updated numbers and updated facts. J Cardiovasc Dis. 2013;1:1–2. [Google Scholar]
- 4.Liu YS, Guo LN, Guo JH. Calcium channel gene mRNA expression effects in atrial fibrillation mechanisms. J Clin Cardio. 2009;25:170–173. [Google Scholar]
- 5.Gan Z, Rumsey J, Hazen BC, Lai L, Leone TC, Vega RB, Xie H, Conley KE, Auwerx J, Smith SR, Olson EN, Kralli A, Kelly DP. Nuclear receptor/microRNA circuitry links muscle fiber type to energy metabolism. J Clin Invest. 2013;123:2564–2575. doi: 10.1172/JCI67652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li RQ. MicroRNAs and atrial fibrillation. J Inte Patho and Clin Med. 2011;31:507–512. [Google Scholar]
- 7.Smyth GK. Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat Appl Genet Mol Biol. 2004;3:Article3. doi: 10.2202/1544-6115.1027. [DOI] [PubMed] [Google Scholar]
- 8.Christ T, Boknik P, Wohrl S, Wettwer E, Graf EM, Bosch RF, Knaut M, Schmitz W, Ravens U, Dobrev D. L-type Ca2+ current downregulation in chronic human atrial fibrillation is associated with increased activity of protein phosphatases. Circulation. 2004;110:2651–2657. doi: 10.1161/01.CIR.0000145659.80212.6A. [DOI] [PubMed] [Google Scholar]
- 9.Fu J, Gao J, Pi R, Liu P. An optimized protocol for culture of cardiomyocyte from neonatal rat. Cytotechnology. 2005;49:109–116. [Google Scholar]
- 10.Pang L, Koren G, Wang Z, Nattel S. Tissue-specific expression of two human Ca(v)1.2 isoforms under the control of distinct 5’ flanking regulatory elements. FEBS Lett. 2003;546:349–354. doi: 10.1016/s0014-5793(03)00629-x. [DOI] [PubMed] [Google Scholar]
- 11.Yin C, Salloum FN, Kukreja RC. A novel role of microRNA in late preconditioning: upregulation of endothelial nitric oxide synthase and heat shock protein 70. Circ Res. 2009;104:572–575. doi: 10.1161/CIRCRESAHA.108.193250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roy S, Khanna S, Hussain SR, Biswas S, Azad A, Rink C, Gnyawali S, Shilo S, Nuovo GJ, Sen CK. MicroRNA expression in response to murine myocardial infarction: miR-21 regulates fibroblast metalloprotease-2 via phosphatase and tensin homologue. Cardiovasc Res. 2009;82:21–29. doi: 10.1093/cvr/cvp015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang GK, Zhu JQ, Zhang JT, Li Q, Li Y, He J, Qin YW, Jing Q. Circulating microRNA: a novel potential biomarker for early diagnosis of acute myocardial infarction in humans. Eur Heart J. 2010;31:659–666. doi: 10.1093/eurheartj/ehq013. [DOI] [PubMed] [Google Scholar]
- 14.Lu Y, Zhang Y, Wang N, Pan Z, Gao X, Zhang F, Zhang Y, Shan H, Luo X, Bai Y, Sun L, Song W, Xu C, Wang Z, Yang B. MicroRNA-328 contributes to adverse electrical remodeling in atrial fibrillation. Circulation. 2010;122:2378–2387. doi: 10.1161/CIRCULATIONAHA.110.958967. [DOI] [PubMed] [Google Scholar]
- 15.Lu Y, Zhang Y, Shan H, Pan Z, Li X, Li B, Xu C, Zhang B, Zhang F, Dong D, Song W, Qiao G, Yang B. MicroRNA-1 downregulation by propranolol in a rat model of myocardial infarction: a new mechanism for ischaemic cardioprotection. Cardiovasc Res. 2009;84:434–441. doi: 10.1093/cvr/cvp232. [DOI] [PubMed] [Google Scholar]
- 16.Xu CC, Han WQ, Xiao B, Li NN, Zhu DL, Gao PJ. Differential expression of microRNAs in the aorta of spontaneously hypertensive rats. Acta Physio Sin. 2008;60:553–560. [PubMed] [Google Scholar]
- 17.Xu C, Lu Y, Pan Z, Chu W, Luo X, Lin H, Xiao J, Shan H, Wang Z, Yang B. The muscle-specific microRNAs miR-1 and miR-133 produce opposing effects on apoptosis by targeting HSP60, HSP70 and caspase-9 in cardiomyocytes. J Cell Sci. 2007;120:3045–3052. doi: 10.1242/jcs.010728. [DOI] [PubMed] [Google Scholar]
- 18.Small EM, Olson EN. Pervasive roles of microRNAs in cardiovascular biology. Nature. 2011;469:336–342. doi: 10.1038/nature09783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girmatsion Z, Biliczki P, Bonauer A, Wimmer-Greinecker G, Scherer M, Moritz A, Bukowska A, Goette A, Nattel S, Hohnloser SH, Ehrlich JR. Changes in microRNA-1 expression and IK1 up-regulation in human atrial fibrillation. Heart Rhythm. 2009;6:1802–1809. doi: 10.1016/j.hrthm.2009.08.035. [DOI] [PubMed] [Google Scholar]
- 20.Terentyev D, Belevych AE, Terentyeva R, Martin MM, Malana GE, Kuhn DE, Abdellatif M, Feldman DS, Elton TS, Gyorke S. miR-1 overexpression enhances Ca(2+) release and promotes cardiac arrhythmogenesis by targeting PP2A regulatory subunit B56alpha and causing CaMKII-dependent hyperphosphorylation of RyR2. Circ Res. 2009;104:514–521. doi: 10.1161/CIRCRESAHA.108.181651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Voigt N, Trausch A, Knaut M, Matschke K, Varro A, Van Wagoner DR, Nattel S, Ravens U, Dobrev D. Left-to-right atrial inward rectifier potassium current gradients in patients with paroxysmal versus chronic atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3:472–480. doi: 10.1161/CIRCEP.110.954636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Y, Geng P, Wang YQ, Liu Y. [Effects of microRNA-1 on negatively regulating L-type calcium channel beta2 subunit gene expression during cardiac hypertrophy] . Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2012;28:304–308. [PubMed] [Google Scholar]
- 23.Cordes KR, Sheehy NT, White MP, Berry EC, Morton SU, Muth AN, Lee TH, Miano JM, Ivey KN, Srivastava D. miR-145 and miR-143 regulate smooth muscle cell fate and plasticity. Nature. 2009;460:705–710. doi: 10.1038/nature08195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li YD, Tang BP. Advances in Research of Calcium Channel Current and Atrial Electrical Remodeling of Atrial Fibrillation. Adv Cardiovasc Dis. 2011;32:718–720. [Google Scholar]
- 25.Van Wagoner DR, Pond AL, Lamorgese M, Rossie SS, McCarthy PM, Nerbonne JM. Atrial L-type Ca2+ currents and human atrial fibrillation. Circ Res. 1999;85:428–436. doi: 10.1161/01.res.85.5.428. [DOI] [PubMed] [Google Scholar]
- 26.Allessie M, Ausma J, Schotten U. Electrical, contractile and structural remodeling during atrial fibrillation. Cardiovasc Res. 2002;54:230–246. doi: 10.1016/s0008-6363(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 27.Findlay I. Physiological modulation of inactivation in L-type Ca2+ channels: one switch. J Physiol. 2004;554:275–283. doi: 10.1113/jphysiol.2003.047902. [DOI] [PMC free article] [PubMed] [Google Scholar]


