Abstract
Background: Diagnosis of acute appendicitis remains to be challenging with up to 30% negative exploration rates. In addition to careful clinical history and physical examination, we still need easily applicable, cheap and effective biomarker. Patients and methods: A retrospective case-controlled study was designed in two groups, both containing 100 patients, acute appendicitis and control. Leukocyte count, neutrophil percentage, platelet count and meal platelet volume (MPV) were compared. Results: MPV values for acute appendicitis and control groups were 7.4 ± 0.9 fL (5.6-10.6) and 9.1 ± 1.6 fL (5.1-13.1). For the diagnosis of acute appendicitis, ROC analysis revealed 74% sensitivity and 75% specificity for a cut-off value of 7.95 fL of MPV, however, the diagnostic value of leukocyte count and/or neutrophil ratio was superior. Conclusion: Our results suggest that, MPV value is an important parameter in the diagnosis of acute appendicitis, but in terms of sensitivity and specificity, leukocyte count and/or neutrophil percentage is superior.
Keywords: Acute appendicitis, mean platelet volume, sensitivity, specificity
Introduction
Acute appendicitis is one of the most frequent cause of emergent exploration due to acute surgical abdomen. Despite, the improvements in diagnostic techniques, negative laparotomy or laparoscopy rates can be reached up to 30% [1]. Efforts to avoid unnecessary explorations were enforced surgeons to find reliable biomarkers for accurate diagnosis of acute appendicitis [2-4]. Although, the value of careful clinical history, physical examination and commonly used laboratory parameters (white blood cell count, neutrophil percentage and C-reactive protein) are upmost important, a reliable biomarker could help the physician to make a clear final decision. Up to date, a lot of markers have been proposed, but none of them were commonly accepted, so we still need easily applicable, cheap and effective biomarker for helping the diagnosis of acute appendicitis [5,6]. The mean platelet volume (MPV) is a routinely reported parameter in complete blood count (CBC). CBC, was generally thought to unimportant by physicians for the diagnosis of acute appendicitis, except white blood cell (WBC) count and neutrophil predominance. MPV is a commonly used marker of platelet production and function, and it has been shown to reflect inflammatory burden. Detected value of MPV has been shown to be affected in many clinical scenarios and reflects disease activity in systemic inflammation, acute pancreatitis, unstable angina and myocardial infarction [7]. Changes in the value of MPV was found to be significant in cardiovascular, cerebrovascular and rheumatoid joint diseases and in some other inflammatory disorders [8-10]. Once it was recognized that, an inflammatory condition can alter the MPV value, the thoughts arise that it could be used for the diagnosis of acute appendicitis as a biomarker [2,5,11-13].
In this retrospective case-controlled study, we compared WBC count, neutrophil ratio, platelet count, and MPV values of a group of pathologically confirmed acute appendicitis with a group of elective herniorrhaphy patients.
Materials and methods
Patient selection
The study was approved by the local ethics committee (ANEAH.EK.2013/58). Between January 2011 and March 2013, 132 patients with pathologically confirmed acute appendicitis in our institute were retrospectively analysed. Younger than 15 years old, alcohol consumption, tobacco smoking, diabetes mellitus, ischemic heart disease, hypertension, morbid obesity and patients with severe comorbidities were excluded. According to aforementioned exclusion criteria, a total of 100 patients (58 males and 42 females), were determined as the acute appendicitis (AA) group. Control group were consisted of 100 patients (60 males and 40 females), who were admitted to our general surgery department for elective herniorrhaphy in the same time period, with respect of defined exclusion criteria. All CBC’s were obtained from patients file. Only CBC’s which were taken in a period of 24 hours prior to surgery were accepted for AA group. WBC count, neutrophil ratio, platelet count, and MPV values were evaluated. MPV values were measured in femtoliter (fL).
Statistical analysis
Continuous data were presented as mean ± standard deviation (SD) and the range (minimum-maximum). Normally distributed continuous data were assessed with Student T-test. If the data were not normally distributed, continuous data were assessed with Mann-Whitney U test. WBC count, neutrophil ratio and MPV values were found to be statistically different between groups, and they were analyzed for their diagnostic value in acute appendicitis using ROC analysis. A two-tailed P value < 0.05 was considered statistically significant. Statistical analyses were performed with the SPSS, version 17.00 (Chicago, IL, USA).
Results
The mean age was similar in between the groups, 33.6 ± 12.2 (18-71) and 30.8 ± 9.7 (15-53), for AA group and control group (P = 0.507). Age, WBC count, neutrophil ratio, platelet count and MPV values are presented in Table 1.
Table 1.
Comparison of the groups regarding to demographic characteristics and laboratory data
| Control group (n = 100) | AA group (n = 100) | P value | |||
|---|---|---|---|---|---|
| Age | 30.8 ± 9.7 | 15-53 | 33.6 ± 12.2 | 18-71 | 0.507 |
| Mean ± SD/range (min-max) | |||||
| WBC (uL) | 8018 ± 1968 | 3320-13000 | 12959 ± 4558 | 3800-29000 | < 0.001 |
| Mean ± SD/range (min-max) | |||||
| Neutrophil (%) | 62 ± 8.4 | 42-82 | 74.8 ± 11.6 | 42.2-92.4 | < 0.001 |
| Mean ± SD/range (min-max) | |||||
| PLT (× 103/uL) | 241.6 ± 72 | 82-624 | 232 ± 59 | 45-418 | 0.320 |
| Mean ± SD/range (min-max) | |||||
| MPV (fL) | 9.1 ± 1.6 | 5.1-13.1 | 7.4 ± 0.9 | 5.6-10.6 | < 0.001 |
| Mean ± SD/range (min-max) | |||||
Briefly, the mean WBC count in AA group was 12.95 ± 4.55 (3.80-29.00) 103/uL and in control group was 8.01 ± 1.96 (3.32-13.00) × 103/uL (P < 0.001); neutrophil ratio in AA group and control group were 74.8% ± 11.6 and 62.3% ± 8.4 (P < 0.001); and the mean platelet count in AA group and control group were 232.3 ± 59.1 (45-418) × 103/uL and 241.6 ± 71.6 (82-624) × 103/uL (P = 0.320). MPV values in the AA group and control group were 7.4 ± 0.9 (5.6-10.6) fL and 9.1 ± 1.6 (5.1-13.1) fL (P < 0.001).
In order to define the value of statistically significant parameters as a biomarker for the diagnosis of acute appendicitis, we performed ROC analysis. For WBC count, the area under the curve was 85.7%. When it’s cut-off value was higher than 8.85 103/uL, the sensitivity and specificity of the WBC count were 85.7% and 85.9%. The same analysis was performed for the neutrophil ratio, the area under curve was 80.7%. When the neutrophil ratio cut-off value was higher than 69.5%, the sensitivity and specificity of the test were found to be 75.8% and 80.0%. Finally, for MPV value, calculated area under the curve was 82.4%. When the MPV cut-off value was below 7.95 fL, the sensitivity and specificity of the test were 74% and 75%, respectively (Figure 1). The results of ROC analysis were presented in Table 2.
Figure 1.
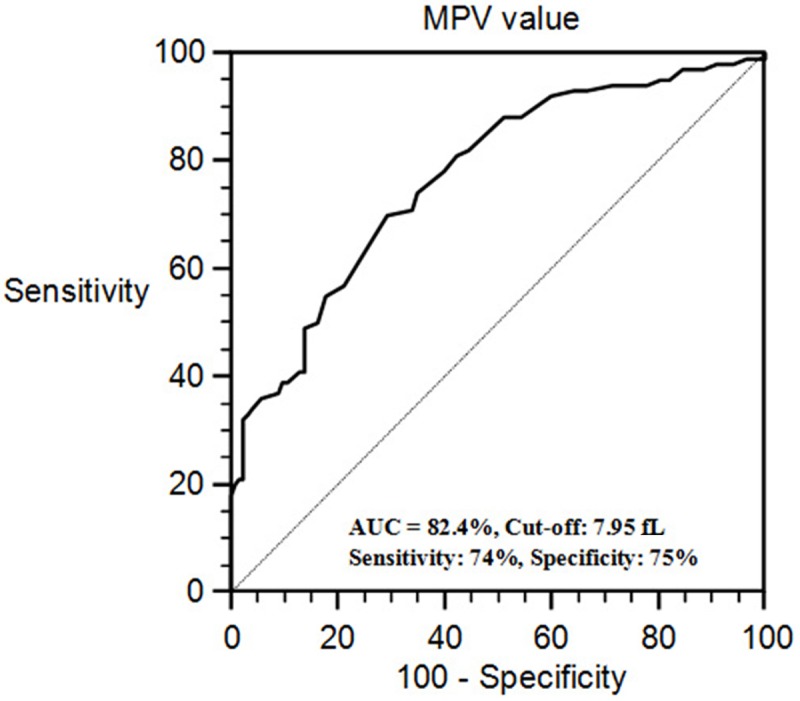
ROC curve for MPV value.
Table 2.
The results of ROC analysis for WBC, neutrophil ratio and MPV
| AUC | Cut-off value | Sensitivity (%) | Specificity (%) | P value | |
|---|---|---|---|---|---|
| WBC (uL) | 0.857 | 8850 | 86% | 73% | < 0.001 |
| Neutrophil (%) | 0.807 | 69.45 | 76% | 80% | < 0.001 |
| MPV (fL) | 0.824 | 7.95 | 74% | 75% | < 0.001 |
AUC: area under the curve.
Discussion
While certain traditionally agreed upon CBC values such as increased leukocyte count and/or neutrophil percentage are well known to clinicians as biomarkers in the diagnosis of acute appendicitis, recently MPV values were investigated in very limited number of studies for the purpose of providing clear differential diagnosis. Some of these studies were suggested MPV alteration as a valuable diagnostic marker when it was combined with WBC and neutrophile percentage, but the alteration of MPV was controversial, some of them reported MPV decrease and some of them reported MPV increase in acute appendicitis [2,11-13]. On the other hand, in one study MPV value was found to have no diagnostic value in pediatric acute appendicitis cases [5].
MPV is easily measured in CBC analysis and it presumably reflects the functional and activation status of platelets and their production rate from megakaryocytes as well. In the literature, MPV value was shown to be significantly higher in patients with sepsis, myocardial ischemia and cerebrovascular diseases compared to MPV values in healthy individuals [7-9]. Similarly, high MPV values were found to be independent risk factor in patients with coronary artery disease and cerebrovascular pathology [8,9]. Slavka et al. reported a 1.5 fold higher mortality rate in patients with high MPV (> 11.01 fL) compared to patients with lower MPV (< 8.7 fL) and they concluded that an increase in MPV reflected increased platelet activity [14].
Reportedly, while increased MPV values were observed in chronic disease conditions, decreased MPV values were observed in acute activation settings [15]. That is, some studies showed that while decreased MPV values were detected in the acute phase, higher values were observed after the condition were treated in the chronic phase [10,16]. Kısacık etal. reported that low MPV values were increased to normal after the treatment in patients with flared ankylosing spondylitis and rheumatoid arthritis [10]. Moreover, it was reported that in some inflammatory bowel diseases, such as in ulcerative colitis, the MPV values decreased in parallel with increased disease activity [10,16-18]. Similarly, Kapsoritakis etal. reported that MPV values were lower in patients with active Crohn’s disease compared to patients with inactive disease [15].
It should be noted that, despite recent interest in investigating possible relationship between MPV value and inflammatory or infectious conditions, the pathogenesis and mechanistic explanations of variations in MPV values has not been clearly understood and this matter deserve further basic research. Danese et al. proposed that the decrease in MPV values in patients with IBD was because of the sequestration and eventually the consumption of large platelets in the vascular bed of inflamed bowel segments [19]. Of note, reported difference of MPV values according to the onset of symptoms in acute appendicitis patients in the study of Albayrak et al. could be associated with this mechanism [2]. They were showed statistically significant difference in MPV values in acute appendicitis, between admission of first 24 hour or later. The MPV values in our study were measured in blood that was withdrawn within 24 hours of laparotomy. As related studies have had not investigated the patients, who were classified as negative exploration, addition of a negative exploration group in our study, could help the recognition of underlying mechanisms.
It should be emphasized that there are very limited studies on this subject and they are observational in nature, like ours. Albayrak et al. reported considerable decrease in MPV values in adult acute appendicitis cases compared to MPV values in healthy subjects [2]. They suggested the importance of the diagnostic value of MPV levels and accordingly they emphasized that MPV values must be studied in the first 24 hours in acute appendicitis cases. The decrease in MPV values that were reported by Bilici et al. in pediatric acute appendicitis cases and the ones that were reported by Albayrak et al. in adult cases were in agreement with the results of our study [2,11]. However, to establish the value of MPV as a biomarker in definitive manner, controlled prospective studies and further mechanistic clinical and basic research are needed.
The value of increase in leukocyte count and neutrophil percentage in the diagnosis of acute appendicitis as biomarkers are widely accepted and used in the daily practice by physicians. In fact, an increase in leukocyte and neutrophil counts are considered to be in parallel to the increase in the severity of inflammation [2,15,20]. Birchley was found that, a higher leukocyte and neutrophil count could be observed in complicated appendicitis cases compared to non-complicated ones [20]. In our study, a significant increase was observed in leukocyte and neutrophil counts in acute appendicitis cases compared to healthy individuals.
In conclusion, we have found MPV value as an important parameter in the diagnosis of acute appendicitis at the calculated cut-off level, 7.4 fL. However, ROC analysis showed that MPV, as a biomarker, was a less superior marker in terms of sensitivity and specificity compared to leukocyte count and/or neutrophil percentage in the diagnosis of acute appendicitis. Accordingly, we believe that further research is needed to be done to find more specific and more reliable biomarkers or biomarker combinations for their utilization in the diagnosis of acute appendicitis besides studies focused on MPV.
Acknowledgements
This manuscript was accepted and presented as a poster (no: 0086) in 19th National Surgery Congress 16-20 April 2014, Rixos Sungate Hotel Antalya, Turkey.
Disclosure of conflict of interest
None.
References
- 1.Jess P, Bjerregaard B, Brynitz S, Holst-Christensen J, Kalaja E, Lund-Kristensen J. Acute appendicitis. Prospective trial concerning diagnostic accuracy and complications. Am J Surg. 1981;141:232–234. doi: 10.1016/0002-9610(81)90164-1. [DOI] [PubMed] [Google Scholar]
- 2.Albayrak Y, Albayrak A, Albayrak F, Yildirim R, Aylu B, Uyanik A, Kabalar E, Guzel IC. Mean platelet volume: a new predictor in confirming acute appendicitis diagnosis. Clin Appl Thromb Hemost. 2011;17:362–366. doi: 10.1177/1076029610364520. [DOI] [PubMed] [Google Scholar]
- 3.Schellekens DH, Hulsewé KW, van Acker BA, van Bijnen AA, de Jaegere TM, Sastrowijoto SH, Buurman WA, Derikx JP. Evaluation of the diagnostic accuracy of plasma markers for early diagnosis in patients suspected for acute appendicitis. Acad Emerg Med. 2013;20:703–170. doi: 10.1111/acem.12160. [DOI] [PubMed] [Google Scholar]
- 4.Kaya B, Sana B, Eris C, Karabulut K, Bat O, Kutanis R. The diagnostic value of D-dimer, procalcitonin and CRP in acute appendicitis. Int J Med Sci. 2012;9:909–915. doi: 10.7150/ijms.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uyanik B, Kavalci C, Arslan ED, Yilmaz F, Aslan O, Dede S, Bakir F. Role of mean platelet volume in diagnosis of childhood acute appendicitis. Emerg Med Int. 2012;2012:823095. doi: 10.1155/2012/823095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sack U, Biereder B, Elouahidi T, Bauer K, Keller T, Tröbs RB. Diagnostic value of blood inflammatory markers for detection of acute appendicitis in children. BMC Surg. 2006;6:15. doi: 10.1186/1471-2482-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beyazit Y, Sayilir A, Torun S, Suvak B, Yesil Y, Purnak T, Oztas E, Kurt M, Kekilli M, Ibis M. Mean platelet volume as an indicator of disease severity in patients with acute pancreatitis. Clin Res Hepatol Gastroenterol. 2012;36:162–168. doi: 10.1016/j.clinre.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Sarikaya S, Sahin S, Akyol L, Borekci E, Yilmaz YK, Altunkas F, Karaman K, Karacavus S, Erbay AR. Mean platelet volume is associated with myocardial perfusion defect in diabetic patients. Cardiovasc J Afr. 2014;25:110–113. doi: 10.5830/CVJA-2014-013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li B, Liu X, Cao ZG, Li Y, Liu TM, Wang RT. Elevated mean platelet volume is associated with silent cerebral infarction. Intern Med J. 2014;44:653–657. doi: 10.1111/imj.12454. [DOI] [PubMed] [Google Scholar]
- 10.Kisacik B, Tufan A, Kalyoncu U, Karadag O, Akdogan A, Ozturk MA, Kiraz S, Ertenli I, Calguneri M. Mean platelet volume (MPV) as an inflammatory marker in ankylosing spondylitis and rheumatoid arthritis. Joint Bone Spine. 2008;75:291–294. doi: 10.1016/j.jbspin.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Bilici S, Sekmenli T, Göksu M, Melek M, Avci V. Mean platelet volume in diagnosis of acute appendicitis in children. Afr Health Sci. 2011;11:427–432. [PMC free article] [PubMed] [Google Scholar]
- 12.Narci H, Turk E, Karagulle E, Togan T, Karabulut K. The role of mean platelet volume in the diagnosis of acute appendicitis: a retrospective case-controlled study. Iran Red Crescent Med J. 2013;15:e11934. doi: 10.5812/ircmj.11934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanrikulu CS, Tanrikulu Y, Sabuncuoglu MZ, Karamercan MA, Akkapulu N, Coskun F. Mean platelet volume and red cell distribution width as a diagnostic marker in acute appendicitis. Iran Red Crescent Med J. 2014;16:e10211. doi: 10.5812/ircmj.10211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slavka G, Perkmann T, Haslacher H, Greisenegger S, Marsik C, Wagner OF, Endler G. Mean platelet volume may represent a predictive parameter for overall vascular mortality and ischemic heart disease. Arterioscler Thromb Vasc Biol. 2011;31:1215–1218. doi: 10.1161/ATVBAHA.110.221788. [DOI] [PubMed] [Google Scholar]
- 15.Kapsoritakis AN, Koukourakis MI, Sfiridaki A, Potamianos SP, Kosmadaki MG, Koutroubakis IE, Kouroumalis EA. Mean platelet volume: a useful marker of inflammatory bowel disease activity. Am J Gastroenterol. 2001;96:776–781. doi: 10.1111/j.1572-0241.2001.03621.x. [DOI] [PubMed] [Google Scholar]
- 16.Yüksel O, Helvaci K, Başar O, Köklü S, Caner S, Helvaci N, Abayli E, Altiparmak E. An overlooked indicator of disease activity in ulcerative colitis: mean platelet volume. Platelets. 2009;20:277–281. doi: 10.1080/09537100902856781. [DOI] [PubMed] [Google Scholar]
- 17.Shah A, Morgan G, Rose JD, Fifield R, Rhodes J. Platelet number and size in relation to serum orosomucoid concentration in Crohn’s disease. Med Lab Sci. 1989;46:79–80. [PubMed] [Google Scholar]
- 18.Järemo P, Sandberg-Gertzen H. Platelet density and size in inflammatory bowel disease. Thromb Haemost. 1996;75:560–561. [PubMed] [Google Scholar]
- 19.Danese S, Motte Cd Cdl, Fiocchi C. Platelets in inflammatory bowel disease: clinical, pathogenic, and therapeutic implications. Am J Gastroenterol. 2004;99:938–945. doi: 10.1111/j.1572-0241.2004.04129.x. [DOI] [PubMed] [Google Scholar]
- 20.Birchley D. Patients with clinical acute appendicitis should have pre-operative full blood count and C-reactive protein assays. Ann R Coll Surg Engl. 2006;88:27–32. doi: 10.1308/003588406X83041. [DOI] [PMC free article] [PubMed] [Google Scholar]


