Abstract
Background: transurethral resection of bladder tumor (TURBT) is the first-line treatment fornon-muscle-invasive bladder cancer. We aimed to investigate the effect of probable risk factors on the positive rate of the repeated transurethral resection of bladder tumor performed 4-6 weeks after an initial TURBT in patients with non-muscle invasive bladder cancer in China. Methods: 134 patients with non-muscle invasive bladder cancer who underwent repeated TURBT within 4-6 weeks after an initial resection were included in this study. The presence of residual tumor and the correlated risk factors, the complications of the second procedure and the changes of stage and grade between the two different TURBTs were analyzed. As showed in the manuscript, of the total 134 patients, 52 had residual tumor, and upgrading occurred in 41 patients. Patients with high grade, T1 stageand residual tumor with multi-focality at the initial transurethral resection were found to be at higher risk after the second opinion. The progression and recurrence rate was significantly higher in patients with residual tumor in Re TURBT. Conclusion:a high rate of occurrence of residual tumor was reported in the repeated TURBT. We suggest repeated TURBT is to be recommended in patients with high grade, T1 stage or multi-focality non-muscle-invasive bladder cancer.
Keywords: Multi-focality, non-muscle invasive bladder cancer, transurethral resection of bladder tumor (TURBT)
Introduction
In China, bladder cancer has the highest incidence among all urogenital cancers, 80% of which are initially diagnosed at Ta or T1 stage or are classified as non-muscle invasive, also called superficial bladder cancer [1]. Of these, approximately 20% to 25% of initially with non-muscle invasive cancers will progress to invasive types during the person’s lifetime. The remaining 30% of bladder cancers are muscle invasive, and generally require surgery to remove the bladder (cystectomy) and the surrounding organs.
Transurethral resection of bladder tumor (TURBT) is the first-line treatment fornon-muscle-invasive bladder cancer. Even in patients who have their bladder tumor completely removed with TURBT, up to 50% of these will have a recurrence of the cancer within 12 months. Due of this high recurrence rate, adjuvant (additional) therapy is usually recommended which reduces the chances of the cancer recurrence. Many scholars support a Re-TURBT 2-6 weeks after the initial TURBT. This includes visibly recurred or residual tumor and muscular tissue around the scar of the initial TURBT, which requires random biopsy if necessary [2]. This report is based on treatment of patients with non-muscle invasive bladder cancer with Re-TURBT from 2004 to 2009. The present study aimed to investigate the effect of probable risk factors on the positive rate of the repeated transurethral resection of bladder tumor performed 4-6 weeks after an initial transurethral resection of bladder tumor (TURBT) in patients with non-muscle invasive bladder cancer in China.
Methods
Patient selection
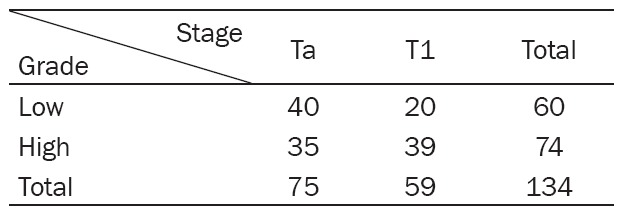
From March 2004 to June 2009, a total of 134 patients (111 males, 23 females) with urothelial bladder carcinoma were treated with Re-TURBT in Shanghai Renji Hospital, Shanghai, China. The age of the patients widely ranged from 33 to 88 years with an average of 64.93±9.65 years. Of the 134 patients, 106 were diagnosed with bladder cancer for the first time and 28 were with recurrence. Also, 85 patients had single tumor, and 49 patients had multiple tumors in the bladder. All were diagnosed with non-muscle invasive bladder cancer according to TURBT and postoperative pathological diagnosis. Pathological stages and grades were diagnosed by pathologists with preserved paraffin section (Table 1). All visible tumors were removed from the bladder wall in the initial TURBT.
Table 1.
Pathological Stage and Grade (Cases)
|
The study protocol was approved by the local Institution Review Board at the authors’ affiliated institution, and meets the standards of the Declaration of Helsinki.
Performance of transurethral tumor re-resection of the bladder
A Re-TURBT was performed 4-6 weeks after initial TURBT in all the patients. The procedure was performed under general anesthesia using a laryngeal mask. The Re-TURBT was performed by the same surgeon who was involved in the initial TURBT. The resection included visibly recurred or residual tumor and muscular tissue around the scar of the initial TURBT in bladder. Random biopsies were performed at normal bladder mucosa under microscope in 26 patients, and the pathological samples were tested separately.
Follow-up procedure
Patients who were not treated with radical cystectomy were subjected to follow-up in out patient service once every three months for the first two years, and then every six months for the next two years. The follow-up examination included routine urine test, cystoscopy and upper urinary tract ultrasonography. Patients with tumor progression and radical cystectomies were excluded from follow-up.
Statistical analysis
All data were analyzed with SPSS 11.5 software package. Chi-square test and Binarylogistic model analysis were also used. Statistical significance was at P < 0.01.
Results
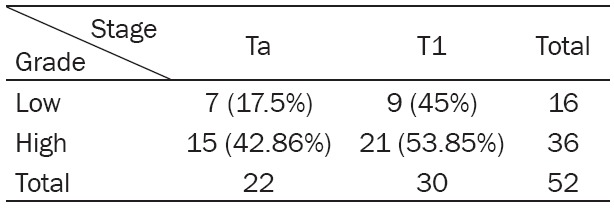
Out of the total 134 patients treated with Re-TURBT, positive tumors were found in 52 patients, and the total positive rate was 38.81%. Among them, in the Re-TURBT, the positive rate of the patients who were diagnosed Ta stage in the initial TURBT was 28.21% (22/78), and that of patients diagnosed at T1 stage was 53.57% (30/56), while the positive rate of low-graded patients was 23.53% (16/68), and that of high-graded patients, 54.55% (36/66) (Table 2). The positive rate of patients diagnosed with single tumor in the initial TURBT was 25.88% (22/85, 4 patients presented with low grade, and 18 patients with high grade), and that of patients with multiple tumor, 61.22% (30/49, 12 patients with low grade, and 18 patients with high grade). In the Re-TURBT, the positive rate of patients diagnosed with tumors for the first time was 37.74% (40/106, 10 patients with low grade, and 30 patients with high grade), and that of patients with recurred tumors, 42.86% (12/28, 6 patients with low grade, and 6 patients with high grade). According to logistic-regression model analysis, multiple tumors in the initial TURBT (P < 0.01), high-graded tumor (P < 0.01) and tumor in T1 stage (P=0.011) were independent risks for positive tumors in Re-TURBT.
Table 2.
Positive cases in Re-TURBT of different stage and grade (rate)
|
Among the 52 positive patients in Re-TURBT, four were pathologically diagnosed with carcinoma in situ; six had different grade from that in initial TURBT, in which, one was higher, and five were lower; 41 were clinically or pathologically diagnosed muscle invasive bladder cancer after Re-TURBT. Among them, 37 went under radical cystectomies within half the year after electrotomy, and four rejected radical operation.
Two of the four patients were followed up and treated in outpatient service, two patients missed the follow-up; 11 were still diagnosed with non-muscle invasive bladder cancer, and were further followed-up and treated in outpatient service. Random biopsies were done in 26 patients, 54 tissue samples were checked and no positive tumor was found.
Till December, 2009, except for patients treated by radical cystectomy in 37 cases and 10 cases missing follow-up, there were 87 patients accepting follow-up in outpatient service. The mean follow-up time was 24.70±15.44 months. During follow-up period, tumors recurred in 31 cases (35.63%), among which, nine were positive in Re-TURBT and 22 were negative. Chi-square test shows that the recurrence rate of the patients positive in Re-TURBT was apparently higher than the negative patients (χ2=7.52, P=0.01). In 11 patients which developed into muscle invasive bladder cancer and undergone radical cystectomy, six were positive in Re-TURBT (including two upgrading cases after Re-TURBT), and five were negative. The tumor progression rate of the patients positive in Re-TURBT was significantly higher than that of the negatives ones (χ2=15.54, P=0.01). There was no metastasis or death from bladder cancer in the 87 cases during follow-up period.
In our research, the complications encountered after Re-TURBT were: prolonged hospitalization (longer than two days) due to hematuria after operation or repeated hospitalization within two weeks in nine patients (6.71%), surgical treatment due to severe hematuria occurred within two weeks after operation in one patient (0.01%), postoperative fever (the temperature was higher than 38°C, lasting more than two days) in 11 patients (8.21%), retaining urethral catheter for more than one week due to various reasons after operation in 21 patients (15.67%). Uroschesis occurred within two weeks after catheter was removed in 10 patients (7.46%), and dilation or surgery due to postoperative urethral stricture in 6 patients (4.48%). In all 134 cases, there was no severe complication such as bladder perforation or rupture.
Discussion
Transurethral resection of bladder tumor has always been used widely as the standard surgical procedure for non-muscle invasive bladder urothelial carcinoma. Recent data suggests that primary TURBT cannot completely remove the tumor or its recurrence but certainly some of its percentage. According to some reports, the rate of positive tumor in Re-TURBT performed within eight weeks after initial TURBT was as high as 18-77% [3-6], and in about 40% of the patients a change in tumor stage was reported [7]. The factors affecting positive rate in Re-TURBT included stage and grade of tumor, size of tumor, interval between two TURBTs, tumor recurrencehistory, operation by surgeon, etc [8,9]. Various reports show that positive rate isrelatively high in Re-TURBT, so of now, most scholars believe that under the condition of TURBT, the features of the tumor itself are the key factor of residual tumor, and that the patients showing positive rates in Re-TURBT have higher risk of tumor recurrence or progression [10].
This research shows that a high rate of residual tumor can be found in the repeated TURBT performed 4-6 weeks after initial TURBT in patients with non-muscle invasive bladder urothelial carcinoma. As our research was a retrospective analysis, the doctors selected patients to be treated with repeated TURBT with some specific selection criteria, leading to the positive rate being higher. According to logistic-regression model analysis, the patients with multiple tumor, high-graded tumor or tumor in T1 stage in the initial TURBT had a much higher risk of reporting residual tumor in the repeated TURBT, which indicated that it was necessary to perform Re-TURBT on the patients with these risk factors. The pathological grade of tumor was the main factor of the positive rate in the repeated TURBT. Our study showed recurrence of tumor does not greatly affect the positive rate in the repeated TURBT (P=0.62).
In terms of surgical complications, there was no bladder perforation or rupture lead by Re-TURBT, and relevant documents at home and abroad [3,6,11] also firm that the complications of Re-TURBT are basically the same as those of routine electrotomy. Therefore, we believe that it is safe to perform Re-TURBT 4-6 weeks after the initial TURBT.
It is noteworthy that in our retrospective study, that 78.85% (41/52) of the patients with positive tumor in Re-TURBT were at a higher pathological stage, and 82.69% (43/52) patients needed radical cystectomy during follow-up period, which is higher than those in abroad documents [4,12,13]. It indicates that there might be suspected condition of high stage when the patients were selected in, and also that there were some defects in our pathological diagnosis. Under this condition, Re-TURBT was also important in accurate diagnosis of different stage. Besides, we also discovered that patients with positive tumor in Re-TURBT tend to have higher risk of tumor recurrence and progression in short term, which indicates that those patients may need more active strategy of treatment and follow-up. Our study had the limitation of small sample size and hence further studies in more number of patients may be required to support the present findings.
Conclusions
The authors concluded that a high rate of residual tumor presence would be found in the repeated TURBT for urothelial bladder carcinoma and transurethral resection could increase the pathological stage accuracy. Further, repeated TURBT can be a safe option. Routine re-TURBT can be recommended in non-muscle invasive bladder cancer patients with high risks such as multiple tumor, T1 tumor or high grade carcinoma in the initial transurethral resected sample within 4 to 6 weeks after initial resection.
Acknowledgements
We thank all the people who gave us help in the research.
Disclosure of conflict of interest
None.
References
- 1.Ro JY, Staerkel GA, Ayala AG. Cytologic and histologic features ofsuperficial bladder cancer. Urol Clin North Am. 1992;19:435–453. [PubMed] [Google Scholar]
- 2.Babjuk M, Burger M, Zigeuner R. EAU guidelines on non-muscleinvasive urothelial carcinoma of the bladder. Eur Urol. 2008;54:303–314. doi: 10.1016/j.eururo.2008.04.051. [DOI] [PubMed] [Google Scholar]
- 3.Herr H. The value of a second transurethral resection in evaluating patients with bladder tumors. J Urol. 1999;162:74–76. doi: 10.1097/00005392-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Divrik RT, Yildirim U, Zorlu F, Eroglua AS, Zorlua F, Ozenb H. Is a second transurethral resection necessary for newly diagnosed pT1 bladder cancer. J Urol. 2006;175:1258–1261. doi: 10.1016/S0022-5347(05)00689-0. [DOI] [PubMed] [Google Scholar]
- 5.Schwaibold HE, Sivalingam S, May F, Hartung R. The value of a secondtransurethral resection for T1 bladder cancer. BJU Int. 2006;97:1199–1201. doi: 10.1111/j.1464-410X.2006.06144.x. [DOI] [PubMed] [Google Scholar]
- 6.Miladi M, Peyromaure M, Zerbib M. The value of a secondtransurethral resection in evaluating patients with bladder tumours. Eur Urol. 2003;43:241–245. doi: 10.1016/s0302-2838(03)00040-x. [DOI] [PubMed] [Google Scholar]
- 7.Amling CL, Thrasher JB, Frazier HA. Robertson JE and Paulson DF. Radical cystectomy for stages Ta, Tis, and T1 transitional cell carcinomaof the bladder. J Urol. 1994;51:31–35. doi: 10.1016/s0022-5347(17)34865-6. [DOI] [PubMed] [Google Scholar]
- 8.Orsola A, Cecchini L, Raventós CX, Trilla E, Planas J, Landolfi S, Torres ID, Morote J. Risk factors for positive findings in patients with high-grade T1 bladder cancer treated with transurethral resection of bladder tumour (TUR) and bacilleCalmette-Guérin therapy and thedecision for a repeat TUR. BJU Int. 2010;105:202–207. doi: 10.1111/j.1464-410X.2009.08694.x. [DOI] [PubMed] [Google Scholar]
- 9.Sivalingam S, Probert JL, Schwaibold H. The role of repeat transurethral resection in the management of high-risk superficial transitional cell bladder cancer. BJU Int. 2005;96:759–762. doi: 10.1111/j.1464-410X.2005.05710.x. [DOI] [PubMed] [Google Scholar]
- 10.Han KS, Joung JY, Cho KS, Seo HK, Chung J, Park WS. Results of repeated transurethral resectionfor a second opinion in patients referred for nonmuscle invasive bladdercancer: the referral cancer center experience and review of the literature. J Endourol. 2008;22:2699–2704. doi: 10.1089/end.2008.0281. [DOI] [PubMed] [Google Scholar]
- 11.Mersdorf A, Brauers A, Wolff JM. Second transurethral resection for superficial bladder cancer: A must? J Urol. 1998;159:143. [Google Scholar]
- 12.Efstathiou JA, Spiegel DY, Shipley WU, Heney NM, Kaufman DS, Niemierko A, Coen JJ, Skowronski RY, Paly JJ, Mcgovern FJ, Zietman AL. Long-term outcomes ofselective bladder preservation by combined-modality therapy for invasivebladder cancer: the MGH experience. Eur Urol. 2012;61:705–711. doi: 10.1016/j.eururo.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Yucel M, Hatipoglu NK, Atakanli C, Yalcinkaya S, Dedekarginoglu G, Saracoglu U, Aras E. Is repeat transurethral resection effective and necessary in patients with T1 bladder carcinoma? Urol Int. 2010;85:276–280. doi: 10.1159/000316073. [DOI] [PubMed] [Google Scholar]


