Abstract
A significant number of patients suffering from traumatic brain injury (TBI) have a high blood alcohol level at the time of injury. Furthermore, drinking alcohol in a binge-like pattern is now recognized as a national problem, leading to a greater likelihood of being injured. Our objective was to determine the consequences of a binge paradigm of alcohol intoxication at the time of TBI on long-term functional outcome using a sensitive test of sensorimotor function. We trained adult, male, Sprague Dawley rats on the skilled forelimb reaching task and then administered a single binge dose of ethanol (2g/kg, i.p.) or saline for three consecutive days (for a total of 3 doses). One hour after the final ethanol dose, rats underwent a TBI to the sensorimotor cortex corresponding to the preferred reaching forelimb. Animals were then tested for seven weeks on the skilled forelimb reaching task to assess the profile of recovery. We found that the group given ethanol prior to TBI displayed a slower recovery curve with a lower recovery plateau as compared to the control group. Therefore, even a relatively short (3 day) episode of binge alcohol exposure can negatively impact long-term recovery from a TBI, underscoring this significant public health problem.
Introduction
1.7 million Americans suffer a traumatic brain injury (TBI) every year[1]. Of those hospitalized, approximately 50,000 die [1,2], and those who survive face a difficult path to recovery. Many TBIs lead to permanent functional deficits, with approximately 5.3 million Americans in need of lifelong assistance for daily living as a result of a TBI [3].
Given the significance of this health crisis, there has been considerable research attempting to assess the degree to which lifestyle factors may influence the outcome of TBI. One such factor investigated is alcohol use, and in this regard, the “binge” pattern of alcohol consumption is currently on the rise among certain demographics [4]. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines alcohol binge as a mode of consumption that leads to a blood alcohol level greater than the legal limit 0.08% (80 mg/dl, ie, 5 drinks for men and 4 drinks for women in two hours) [5]. Binge drinking is a common practice among Americans; a recent study found that approximately 1 out of every 6 adults in America binge drink four times a month [6]. Furthermore, binge alcohol consumption is correlated with increased risky behavior that can lead to injuries, including TBI [7]. Accordingly, it has been estimated that 30–50% of TBI patients have a blood alcohol level above the legal limit at the time of injury [8]. In fact, intoxicated TBI patients entering the emergency room typically have a blood alcohol level much higher than the legal limit at approximately 170mg/dl [9].
The few animal studies of behavioral recovery after binge ethanol combined with TBI have given equivocal results. Depending on the injury severity and the dose of ethanol administered, recovery after TBI may or may not be hindered [10, 11]. In one report, four weeks of binge ethanol treatment followed by ethanol intoxication at the time of TBI worsened some aspects of spatial learning in rats [12]. Earlier work has shown that a high single binge dose of ethanol can worsen recovery of sensorimotor function.[10, 13] However, these deficits may be transient [13]. Therefore, it remains unclear whether binge ethanol given prior to TBI affects long-term functional outcome, especially given that most studies focused on short recovery time points.
Given these findings, we set out to examine whether a repeated binge regimen of ethanol delivered prior to TBI would lead to an impaired long-term sensorimotor functional recovery. We used a rodent model of TBI, the controlled cortical impact (CCI), and evaluated the outcome with a sensitive measure of sensorimotor function, the skilled forelimb reaching task. We found that rats treated with a three day regimen of binge ethanol prior to TBI exhibited worse sensorimotor recovery on this skilled task as compared to rats with TBI only.
Methods
Ethics Statement
Animal use was approved by the Institutional Animal Care and Use Committee (IACUC) of Edward Hines Veterans Affairs Hospital permit #H13–001.
Animals
23 Sprague Dawley male rats (Harlan, IN) 10 weeks old and weighing approximately 260grams at the beginning of training, were used in this study. Rats were housed two in a cage in a fully accredited animal care facility with a 12-hour light/dark cycle. Rats were food-restricted to 95% of their predicted weight by age in order to encourage learning the behavioral task. All animals were number coded and investigators were blind to the animal treatment groups.
Behavioral Testing
To examine complex sensorimotor forelimb function, the skilled forelimb reaching test was used (Fig. 1B), as previously designed [14]. Briefly, rats were weighed and placed in a Plexiglas chamber (30x36x30 cm) with a small rectangular opening (1.5 x 3 cm) on one wall with an external shelf underneath the opening. Rats were trained to reach through the opening for pellets placed on the shelf. A single trial consisted of 20 sugar pellets (45 mg; BioServ, Flemington, NJ) placed successively on the shelf. A successful reach was defined as one in which the animal, in one attempt, reached through the opening, grasped the pellet, and brought it back to its mouth. During the course of training, limb preference was first determined for each animal. Rats were trained to a baseline success rate of 14 out of 20 successful reaches using the preferred forelimb. Once baseline scores were achieved, the animal received a TBI to the sensorimotor cortical area corresponding to the preferred forelimb, resulting in impairment on this task. Animals were tested Mon-Fri for seven weeks post-TBI and sessions were video recorded for further analysis.
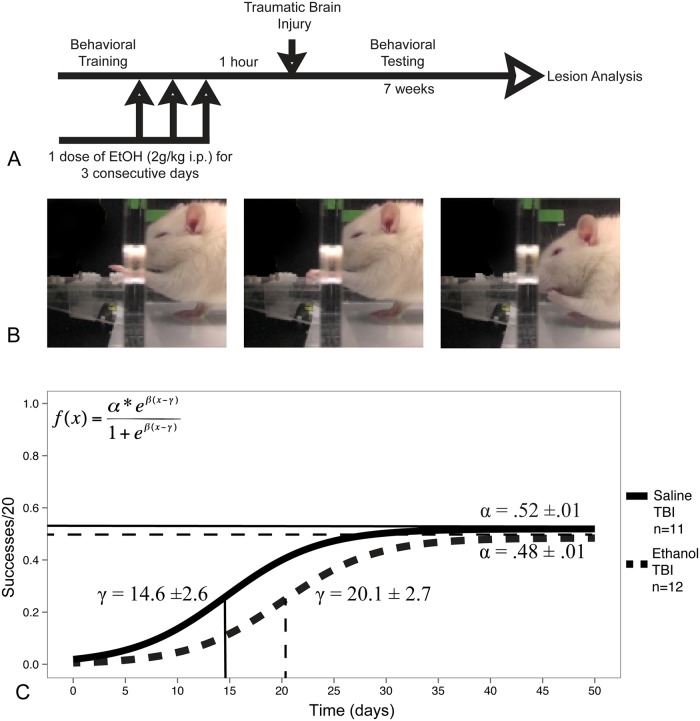
Fig 1. A. Experimental design schematic.
B. Representative kinematic sequence of a non-injured rat during the skilled reaching task. C. Fitted curves of the estimated group-level logistic recovery for rats given either three doses of binge ethanol (2g/kg) or vehicle control prior to TBI. The group differences in the midpoint (γ) and asymptote (α) of recovery were found to be statistically significant (p<.05).
Alcohol Administration
Following behavioral training and prior to TBI, rats in the ethanol treatment group (n = 12) were administered 3 consecutive doses of ethanol (2g/kg, i.p.) once per day for 3 days. Control animals (n = 11) received an equal volume of 0.9% saline, given using an identical dosing schedule. This ethanol dose leads to blood alcohol levels typical of a TBI patient entering the emergency room (~170 mg/dl) (Bombardier and Thurber, 1998) and is well tolerated in rats.
Blood Alcohol Concentration Quantification
100μl of blood was drawn from the tail vein of each rat one hour after the last dose was given, and the blood alcohol concentration (BAC) was quantified using an oxygen-rate alcohol analyzer (Analox Instruments, London, UK).
TBI model-Controlled Cortical Impact (CCI)
All rats were anesthetized with 3% isoflurane delivered as an inhalant with 5% oxygen. During surgery, animal body temperature was maintained at 38°C using the physitemp TCAT-2DF Controller system (Physitemp Instruments Inc, Clifton, NJ). Rats were placed in a stereotaxic instrument, followed by a small scalp incision. Using a trephine, a 5mm diameter disc of skull was removed to expose the primary forelimb motor cortex (1.5mm anterior, 2.5 mm lateral from bregma, [15]) of the hemisphere opposite the preferred reaching forelimb. The CCI was delivered using a double acting electromagnetic piston mounted on a stereotaxic crossbar, angled for cortical impact (diameter: 3mm, velocity: 2.5m/sec, depth: 2mm, dwell time: 250 msec)(Impact One, MyNeurolab, St. Louis, MO). The CCI model results in a reproducible lesion, typified by both focal and diffuse brain damage. Following impact, the disk of bone was put back in place and the scalp incision closed with sutures. Animals were returned to their home cages.
Lesion Analysis
After completion of behavioral testing, rats were overdosed with sodium pentobarbital (100 mg/kg, i.p.) and transcardially perfused with 0.9% saline followed by 4% paraformaldehyde. Brains were extracted and cryosectioned at 40 microns and stained for Nissl. To determine the lesion size, every 12th section between 2.7mm anterior and -1.7 mm posterior to bregma was scanned using a flatbed scanner and traced in Adobe Photoshop to provide an area. The percentage of hemisphere damage was computed using the following formula:
This method has been used extensively by us [16–19] and others [20–22].
Statistical analysis
All data analysis was performed using either SAS (SAS Institute, Cary, NC, USA) or R: A Language and Environment for Statistical Computing. Skilled reaching data was fit using a nonlinear, 3-parameter, binomial logistic, mixed effects model:. α is the horizontal asymptote as x → ∞, β is the slope, and γ is the x value at which the response is α/2. α and β were modeled by fixed effects and allowed to vary by group while γ was modeled by random effects. Thus, our model constitutes a nonlinear mixed model approach, which has been shown by us and others to exhibit greater sensitivity to real effects and directly models parameters of interest including final recovery and rate of recovery [17, 23, 24]. Group parameters were compared using a likelihood based chi squared test with an alpha level of 0.05. Lesion volume comparisons were done using an unpaired t-test, with α = .05 as the cutoff for statistical significance.
Results
Repeated Binge Ethanol and Sensorimotor Recovery
After TBI, all animals in both groups showed a significant deficit in performance on the skilled forelimb reaching task. Furthermore, over the course of seven weeks of testing, all animals showed some increase in spontaneous sensorimotor recovery (Fig. 1C), and the difference in the estimated slopes of recovery (β) were not statistically significant between the saline and ethanol treated groups. However, the midpoint (γ) and the recovery asymptote (α) were found to be significantly different, with ethanol treated rats reaching the midpoint of recovery at a later time point (20.1±2.6 days compared to 14.61±2.7 days in saline treated rats, p<0.05). The asymptote of recovery was also found to be lower in the ethanol treated group (0.48 ± 0.01 compared to 0.52 ± 0.01 in saline treated rats, p<0.05). Thus, binge ethanol treated rats took significantly longer to reach their recovery plateau, and their final level of recovery was less than that of saline treated rats.
Lesion Analysis
TBI lesion size was quantified at the end of the behavioral testing (Fig. 2) and taken together with the exhibited behavioral deficits indicated a mild to moderate TBI in all animals. No statistically significant difference was found between groups (9.9% ± 2.0 in ethanol treated rats vs. 8.7% ± 1.4 in saline treated rats, unpaired t-test, p>.05).
Fig 2. A. Representative nissl stained coronal sections of saline treated and ethanol treated seven weeks post traumatic brain injury.
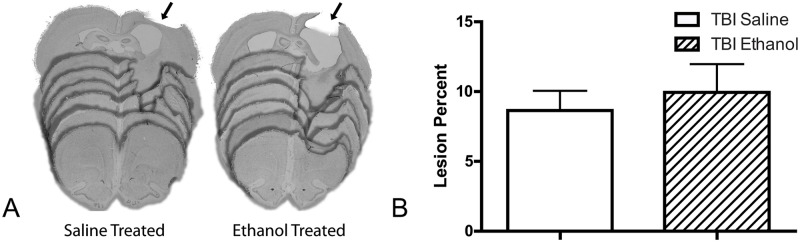
The arrows indicate the location of the lesion. B. Lesion size expressed as a percent of the unlesioned hemisphere. No significant difference was found between saline and ethanol treated animals p>.05 (unpaired t-test). Error bars denote the ± SEM.
Blood Alcohol Concentration
Blood ethanol concentrations were 185 ±20.7 mg/dl (mean ± SEM) at 1 hour after i.p. injection (the time of the TBI).
Rat Weight
The weights of alcohol and saline treated animals were not significantly different on the day of injury (349.6 ± 10.98g in ethanol treated rats vs. 347.8 ± 13.3g in saline treated rats, mean ±SEM, unpaired t-test, p>.05) or 24 hours later (343.0 ± 10.17g in ethanol treated rats vs. 343.4 ± 10.2g in saline treated rats, mean ± SEM, unpaired t-test, p>.05). Furthermore, we did not find a statistically significant difference in the number of days until each animal reached their respective pre-injury baseline weight after injury (5.5 ± 1.4 days in ethanol treated rats vs. 4.7 ± 1.3 days in saline treated rats, unpaired t-test, p>.05).
Discussion
Our results show that ethanol administered in a repeated binge fashion (2g/kg, i.p.) over three days before a mild to moderate TBI primarily involving the forelimb motor cortex led to a significantly slower recovery and a worse overall performance on a test of skilled forelimb function.
To our knowledge, this is the first study to demonstrate that binge ethanol given prior to a TBI and at the time of injury leads to long-term deficits on a sensorimotor task with less spontaneous recovery when compared to rats with no ethanol and the same TBI. The limited previous work evaluating the effects of pre-TBI ethanol on sensorimotor recovery has given equivocal results. For example, research using the horizontal beam walk task found that rats given a single dose of 1.5g/kg, i.p. or 2.5g/kg, i.p. ethanol delivered 40 minutes prior to a TBI (CCI) exhibited a faster recovery over the first post-TBI week than animals given saline or 3 g/kg ethanol i.p., indicating a neuroprotective effect of those lower doses of ethanol [10]. We did not find a similar effect when assessing recovery during the first two weeks post injury. In our study, even in the first weeks post-injury, binge ethanol treated rats exhibited a trend towards poorer performance when compared to the control group. Importantly, we used a similar dose to Kelly et al but with a three day dosing schedule. Therefore, the repeated binge regimen as done in our study may have been the reason for the lack of neuroprotection and the overall worse outcome. Another study using a chronic binge model (6 weeks of 35% ethanol derived calories, liquid diet) followed by a lateral fluid percussion (LFP) TBI, also showed no significant difference on beam walk task performance when compared to pair-fed controls [25]. However, examination of their injury parameters showed a location in the lateral and posterior aspects of the parietal and temporal cortex, a different location as compared to the neocortical sensorimotor location of the lesions in our study. Furthermore, the beam walk task is a different type of behavioral assessment as compared to the skilled reaching task, which may be more sensitive to recovery [26]. Our study is in support of a previous report using a battery of neurologic tests to evaluate sensorimotor outcome. Rats given a single dose of ethanol (3g/kg per gavage) prior to a severe TBI (LFP) displayed a worse neuroscore 24 hours after injury [13]. Taking these studies together, one interpretation is that binge ethanol impairs sensorimotor recovery when the binge is repeated (3 days as in our study) or when the TBI is severe in the context of a single binge dose of ethanol. Our work is continuing to investigate this important question of lesion location and severity in regard to neurological outcome when under the influence of binge ethanol.
Given the above findings, how might binge ethanol worsen sensorimotor recovery without an apparent effect on lesion volume? It has been shown that ethanol modulates a number of processes involved in CNS recovery, including adrenergic, purinergic [27] and glutamatergic signaling (for a review see [28]). More recent work has demonstrated that even without a TBI a single binge ethanol exposure is enough to induce brain damage as measured by glial reactivity and neurodegeneration [29]. Interestingly, another mechanism by which binge ethanol may worsen recovery is through effects on neural stem cells. It has been suggested that neural precursor cells integrate into the dentate gyrus to enhance functional recovery [30]. Pertinent to our work, studies have demonstrated that ethanol may suppress neurogenesis, thereby repressing this mode of post-injury compensation [31]. Our current studies are aimed at determining the mechanism of how binge ethanol affects neural precursor cells in the setting of TBI.
How our results in this study translate to the human condition is still unclear. Among the many variables that make our rodent model different from humans is the route of administration of ethanol, where human consumption is by the oral route. However, this route can result in a wider range of blood levels as compared to the i.p. route primarily due to variables in absorption and metabolism. Therefore, we chose to begin our studies using the i.p. route of administration to achieve the most consistent blood alcohol levels as possible in all rats at the time of TBI in order to give the clearest interpretation of our behavioral results. In our current studies we have added the oral gavage route to better emulate the human mode of ethanol consumption.
In conclusion, this study demonstrates that even a short (3 day) repeated binge ethanol exposure prior to a TBI leads to a slower and worse overall outcome on a skilled task of forelimb function in young adult rats. If these results are translatable to humans, given that the overall prevalence of binge drinking among American adults is estimated at 17% (even higher among younger demographic groups) and that binge drinkers have a greater risk of TBI, a slowed and reduced recovery represents a significant public health concern [6, 32].
Supporting Information
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by a grant from the National Institute of Health R21 AA020951, an National Institute on Alcohol Abuse and Alcoholism training grant T32 AA013526, the Department of Veterans Affairs and the Office of Academic Affiliations. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Coronado VG, McGuire LC, Sarmiento K, Bell J, Lionbarger MR, Jones CD, et al. Trends in Traumatic Brain Injury in the U.S. and the public health response: 1995–2009. Journal of safety research. 2012;43(4):299–307. 10.1016/j.jsr.2012.08.011 [DOI] [PubMed] [Google Scholar]
- 2. Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. The Journal of head trauma rehabilitation. 2010;25(2):72–80. 10.1097/HTR.0b013e3181ccc8b4 [DOI] [PubMed] [Google Scholar]
- 3. Thurman DJC, V.; Selassie A The Epidemiology of TBI: Implications for Public Health In: Zasler NDK, K. I.; Zafonte R.D., editor. Brain Injury Medicine. New York: Demos Medical Publishing; 2007. [Google Scholar]
- 4. Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. Journal of studies on alcohol and drugs Supplement. 2009;(16):12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Olthuis JV, Zamboanga BL, Ham LS, Van Tyne K. The utility of a gender-specific definition of binge drinking on the AUDIT. Journal of American college health: J of ACH. 2011;59(4):239–45. 10.1080/07448481.2010.497523 [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease C, Prevention. Vital signs: binge drinking prevalence, frequency, and intensity among adults—United States, 2010. MMWR Morbidity and mortality weekly report. 2012;61(1):14–9. [PubMed] [Google Scholar]
- 7. Savola O, Niemela O, Hillbom M. Alcohol intake and the pattern of trauma in young adults and working aged people admitted after trauma. Alcohol and alcoholism (Oxford, Oxfordshire). 2005;40(4):269–73. [DOI] [PubMed] [Google Scholar]
- 8. Parry-Jones BL, Vaughan FL, Miles Cox W. Traumatic brain injury and substance misuse: a systematic review of prevalence and outcomes research (1994–2004). Neuropsychological rehabilitation. 2006;16(5):537–60. [DOI] [PubMed] [Google Scholar]
- 9. Bombardier CH, Thurber CA. Blood alcohol level and early cognitive status after traumatic brain injury. Brain Inj. 1998;12(9):725–34. [DOI] [PubMed] [Google Scholar]
- 10. Kelly DF, Lee SM, Pinanong PA, Hovda DA. Paradoxical effects of acute ethanolism in experimental brain injury. Journal of neurosurgery. 1997;86(5):876–82. [DOI] [PubMed] [Google Scholar]
- 11. Janis LS, Hoane MR, Conde D, Fulop Z, Stein DG. Acute ethanol administration reduces the cognitive deficits associated with traumatic brain injury in rats. Journal of neurotrauma. 1998;15(2):105–15. [DOI] [PubMed] [Google Scholar]
- 12. Prasad RM, Doubinskaia I, Singh DK, Campbell G, Mace D, Fletcher A, et al. Effects of binge ethanol administration on the behavioral outcome of rats after lateral fluid percussion brain injury. Journal of neurotrauma. 2001;18(10):1019–29. [DOI] [PubMed] [Google Scholar]
- 13. Yamakami I, Vink R, Faden AI, Gennarelli TA, Lenkinski R, McIntosh TK. Effects of acute ethanol intoxication on experimental brain injury in the rat: neurobehavioral and phosphorus-31 nuclear magnetic resonance spectroscopy studies. Journal of neurosurgery. 1995;82(5):813–21. [DOI] [PubMed] [Google Scholar]
- 14. Seymour AB, Andrews EM, Tsai SY, Markus TM, Bollnow MR, Brenneman MM, et al. Delayed treatment with monoclonal antibody IN-1 1 week after stroke results in recovery of function and corticorubral plasticity in adult rats. J Cereb Blood Flow Metab. 2005;25(10):1366–75. [DOI] [PubMed] [Google Scholar]
- 15. O'Donoghue DL, Kartje-Tillotson G, Neafsey EJ, Castro AJ. A study of forelimb movements evoked by intracortical microstimulation after hemicerebellectomy in newborn, young and adult rats. Brain research. 1986;385(2):311–20. [DOI] [PubMed] [Google Scholar]
- 16. Tsai SY, Papadopoulos CM, Schwab ME, Kartje GL. Delayed anti-nogo-a therapy improves function after chronic stroke in adult rats. Stroke; a journal of cerebral circulation. 2011;42(1):186–90. 10.1161/STROKEAHA.110.590083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gillani RL, Tsai SY, Wallace DG, O'Brien TE, Arhebamen E, Tole M, et al. Cognitive recovery in the aged rat after stroke and anti-Nogo-A immunotherapy. Behavioural brain research. 2010;208(2):415–24. 10.1016/j.bbr.2009.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andrews EM, Tsai SY, Johnson SC, Farrer JR, Wagner JP, Kopen GC, et al. Human adult bone marrow-derived somatic cell therapy results in functional recovery and axonal plasticity following stroke in the rat. Experimental neurology. 2008;211(2):588–92. 10.1016/j.expneurol.2008.02.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wolf WA, Martin JL, Kartje GL, Farrer RG. Evidence for fibroblast growth factor-2 as a mediator of amphetamine-enhanced motor improvement following stroke. PloS one. 2014;9(9):e108031 10.1371/journal.pone.0108031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Morales D, McIntosh T, Conte V, Fujimoto S, Graham D, Grady MS, et al. Impaired fibrinolysis and traumatic brain injury in mice. Journal of neurotrauma. 2006;23(6):976–84. [DOI] [PubMed] [Google Scholar]
- 21. Pu H, Guo Y, Zhang W, Huang L, Wang G, Liou AK, et al. Omega-3 polyunsaturated fatty acid supplementation improves neurologic recovery and attenuates white matter injury after experimental traumatic brain injury. J Cereb Blood Flow Metab. 2013;33(9):1474–84. 10.1038/jcbfm.2013.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen X, Duan XS, Xu LJ, Zhao JJ, She ZF, Chen WW, et al. Interleukin-10 mediates the neuroprotection of hyperbaric oxygen therapy against traumatic brain injury in mice. Neuroscience. 2014;266:235–43. 10.1016/j.neuroscience.2013.11.036 [DOI] [PubMed] [Google Scholar]
- 23. Young ME, Clark MH, Goffus A, Hoane MR. Mixed effects modeling of Morris water maze data: Advantages and cautionary notes. Learning and Motivation. 2009;40(2):160–77. [Google Scholar]
- 24. Wainwright PE, Leatherdale ST, Dubin JA. Advantages of mixed effects models over traditional ANOVA models in developmental studies: a worked example in a mouse model of fetal alcohol syndrome. Developmental psychobiology. 2007;49(7):664–74. [DOI] [PubMed] [Google Scholar]
- 25. Zhang L, Maki A, Dhillon HS, Barron S, Clerici WJ, Hicks R, et al. Effects of six weeks of chronic ethanol administration on the behavioral outcome of rats after lateral fluid percussion brain injury. Journal of neurotrauma. 1999;16(3):243–54. [DOI] [PubMed] [Google Scholar]
- 26. Klein A, Sacrey LA, Whishaw IQ, Dunnett SB. The use of rodent skilled reaching as a translational model for investigating brain damage and disease. Neuroscience and biobehavioral reviews. 2012;36(3):1030–42. 10.1016/j.neubiorev.2011.12.010 [DOI] [PubMed] [Google Scholar]
- 27. Ostrovskaya O, Asatryan L, Wyatt L, Popova M, Li K, Peoples RW, et al. Ethanol is a fast channel inhibitor of P2X4 receptors. The Journal of pharmacology and experimental therapeutics. 2011;337(1):171–9. 10.1124/jpet.110.176990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Opreanu RC, Kuhn D, Basson MD. Influence of alcohol on mortality in traumatic brain injury. Journal of the American College of Surgeons. 210(6):997–1007. 10.1016/j.jamcollsurg.2010.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hayes DM, Deeny MA, Shaner CA, Nixon K. Determining the threshold for alcohol-induced brain damage: new evidence with gliosis markers. Alcoholism, clinical and experimental research. 2013;37(3):425–34. 10.1111/j.1530-0277.2012.01955.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Blaiss CA, Yu TS, Zhang G, Chen J, Dimchev G, Parada LF, et al. Temporally specified genetic ablation of neurogenesis impairs cognitive recovery after traumatic brain injury. J Neurosci. 2011;31(13):4906–16. 10.1523/JNEUROSCI.5265-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hansson AC, Nixon K, Rimondini R, Damadzic R, Sommer WH, Eskay R, et al. Long-term suppression of forebrain neurogenesis and loss of neuronal progenitor cells following prolonged alcohol dependence in rats. The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP). 2010;13(5):583–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Taylor LA, Kreutzer JS, Demm SR, Meade MA. Traumatic brain injury and substance abuse: A review and analysis of the literature. Neuropsychological rehabilitation. 2003;13(1–2):165–88. 10.1016/S0960-9822(02)01374-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.