Abstract
Background:
The Centers for Medicare and Medicaid Services provide significant incentives to health plans that score well on Medicare STAR metrics for cardiovascular disease risk factor medication adherence. Information on modifiable health system-level predictors of adherence can help clinicians and health plans develop strategies for improving Medicare STAR scores, and potentially improve cardiovascular disease outcomes.
Objective:
To examine the association of Medicare STAR adherence metrics with system-level factors.
Research Design:
A cross-sectional study.
Subjects:
A total of 129,040 diabetes patients aged 65 years and above in 2010 from 3 Kaiser Permanente regions.
Measures:
Adherence to antihypertensive, antihyperlipidemic, and oral antihyperglycemic medications in 2010, defined by Medicare STAR as the proportion of days covered ≥80%.
Results:
After controlling for individual-level factors, the strongest predictor of achieving STAR-defined medication adherence was a mean prescribed medication days’ supply of >90 days (RR=1.61 for antihypertensives, oral antihyperglycemics, and statins; all P<0.001). Using mail order pharmacy to fill medications >50% of the time was independently associated with better adherence with these medications (RR=1.07, 1.06, 1.07; P<0.001); mail order use had an increased positive association among black and Hispanic patients. Medication copayments ≤$10 for 30 days’ supply (RR=1.02, 1.02, 1.02; P<0.01) and annual individual out-of-pocket maximums ≤$2000 (RR=1.02, 1.01, 1.02; P<0.01) were also significantly associated with higher adherence for all 3 therapeutic groupings.
Conclusions:
Greater medication days’ supply and mail order pharmacy use, and lower copayments and out-of-pocket maximums, are associated with better Medicare STAR adherence. Initiatives to improve adherence should focus on modifiable health system-level barriers to obtaining evidence-based medications.
Key Words: adherence, quality measurement, quality improvement
The Center for Medicare and Medicaid Services (CMS) uses its Medicare STAR program to monitor and reward the quality of care in health plans with Medicare Advantage enrollees, and provides substantial incentives to health plans that perform well on its Medicare STAR metrics.1 In 2012, CMS introduced 3 new Medicare STAR metrics to measure medication adherence for cardiovascular disease (CVD) risk factor medications: angiotensin converting enzyme inhibitors and angiotensin receptor blockers (ACEI/ARBs) to control hypertension; statins to control LDL-cholesterol; and oral antihyperglycemics to control glycosylated hemoglobin (HbA1c). The implementation of these new measures emphasizes the responsibility of health plans to monitor and improve medication adherence in their Medicare populations.2,3
Overall performance on these Medicare STAR measures is highly dependent on the adherence of patients with diabetes, who account for almost all oral antihyperglycemic use and much antihypertensive and statin use.4–6 Most research on medication adherence to these CVD risk factor medications has focused on younger populations,7–11 and there is limited information on the correlates of adherence in diabetes patients aged 65 and older.10 Medication adherence research traditionally focuses on patient-level characteristics such as age and sex,7–12 despite the fact that patient characteristics have limited ability to predict adherence.13 In contrast, interventions focused on health care system-level characteristics may hold the most hope for improving appropriate CVD risk factor medication use at the population level,2,14–16 as these characteristics are modifiable through health care benefit and policy changes. Despite the potential for system-level interventions to improve adherence in high-risk patients, the system-level correlates of adherence to CVD risk factor medications in Medicare-aged diabetes patients, and their combined effect on adherence levels, are largely unknown.
The purpose of this study is to examine the relationship between Medicare STAR medication adherence metrics and modifiable health system-level characteristics in a cohort of Medicare-aged diabetes patients.
METHODS
Study Setting and Population
The population and data for this study were derived from the Surveillance, Prevention, and Management of Diabetes Mellitus (SUPREME-DM) DataLink, a multisite data resource for research that accesses electronic health record, clinical, and administrative data from 2005 to 2011.17–20 The current study drew data from 3 SUPREME-DM integrated, group-model health care delivery systems sites that collectively serve 4.1 million members: Kaiser Permanente Northern California (KPNC), Kaiser Permanente Colorado (KPCO), and Kaiser Permanente Northwest (KPNW; Northwest Oregon and Southwest Washington). Patients were eligible for the current study if they had diabetes in 2010, and were 65 years of age and above as of January 1, 2010. Patients were defined as having diabetes if they had ≥2 outpatient diabetes ICD-9 diagnosis codes (250.xx) within a 2-year window since the start of 2000.21–23
Medicare STAR Medication Adherence
We calculated the Medicare STAR adherence metrics following CMS specifications to obtain the Proportion of Days Covered (PDC) measure in 2010 for all patients for each of the 3 therapeutic groupings covered by the measures: ACEI/ARBs, statins, and oral diabetes medications.3,24 PDC is defined as the percent of days in the measurement period “covered” by prescription fills for the same medication or medications in the same therapeutic category.25 Per CMS specifications, the measurement period began with patients’ first fill in 2010 through December 31, 2010, and applies only to patients with ≥2 fills in the therapeutic grouping within that period; also per CMS specifications, the PDC calculation for oral diabetes medications excludes patients taking insulin.3 The PDC ranges from 0 to 1; the Medicare STAR adherence measure considers patients to be “adherent” if their PDC is ≥0.8.
Health System-level Independent Variables
This study focused on 4 health system-level predictors of Medicare STAR medication adherence: mean days’ supply of medications, annual individual out-of-pocket maximum costs, generic drug copayment, and percent of medications delivered through mail order pharmacy. These variables are considered “system level” because they are directly influenced by the benefit and pharmacy delivery structures of a patient’s health plan that are potentially modifiable. Days’ supply was derived from the pharmacy electronic medication dispensing record. Annual individual out-of-pocket cost maximum and generic drug copayments per 30 days of medication supply were obtained from membership files. The rate of mail order pharmacy use to fill a specific medication in 2010 was calculated as the percent of time a patient used the mail order service (vs. a KP “brick and mortar” pharmacy) to fill a medication in the 12-month period; details on the KP mail order pharmacy system have been published elsewhere.14,15
Statistical Analyses
To examine the relationship between adherence and health system-level characteristics and patient characteristics, we obtained relative risks using 3 Poisson regression models, 1 for each of the 3 therapeutic groupings, using PDC≥0.8 (vs. <0.8) as the dichotomous-dependent variable; this method is appropriate for determining risk in cross-sectional data where the outcome is relatively common.26 Each model was adjusted for the 4 health system-level independent variables defined above, and also adjusted for patient age, sex, race/ethnicity, census block-level median household income and education, delivery system region, and total number of medications the patient was concurrently taking in 2010. To test the combined effect of all 4 health system-level variables on adherence, we obtained predicted percentages27 of patients achieving “good” (ie, PDC≥0.8) Medicare STAR adherence in each of the therapeutic groupings when all 4 system-level variables were at the specified values “optimized” at the cutpoints used in the regression models (days’ supply >90; 30 day copayment ≤$10; out-of-pocket maximum ≤$2000; >50% of fills delivered through mail order pharmacy), versus when all 4 system-level variables were at the least optimized specified values (days’ supply <31; copay >$10; out-of-pocket maximum >$2000; no fills through mail order pharmacy) after adjusting for patient demographic, clinical, and socioeconomic characteristics. To further our understanding of the role of the health system-level variables that may affect potential disparities in adherence, we tested whether any of our health system-level variables had a statistically significant (P<0.01) interaction with race/ethnicity; significant interaction terms were included in the final models. All analyses were performed using Stata v10.1.
This study was approved by the KPNC Institutional Review Board; KPCO and KPNW ceded IRB oversight to KPNC.
RESULTS
Table 1 presents the demographic and clinical characteristics of the patients in the sample by each CVD risk factor medication therapeutic grouping. On the basis of the Medicare STAR metric definition, 81%, 82%, and 79% of patients were considered adherent to medications in the therapeutic groupings for ACEI/ARBs, oral diabetes medications, and statins, respectively.
TABLE 1.
Patient Characteristics
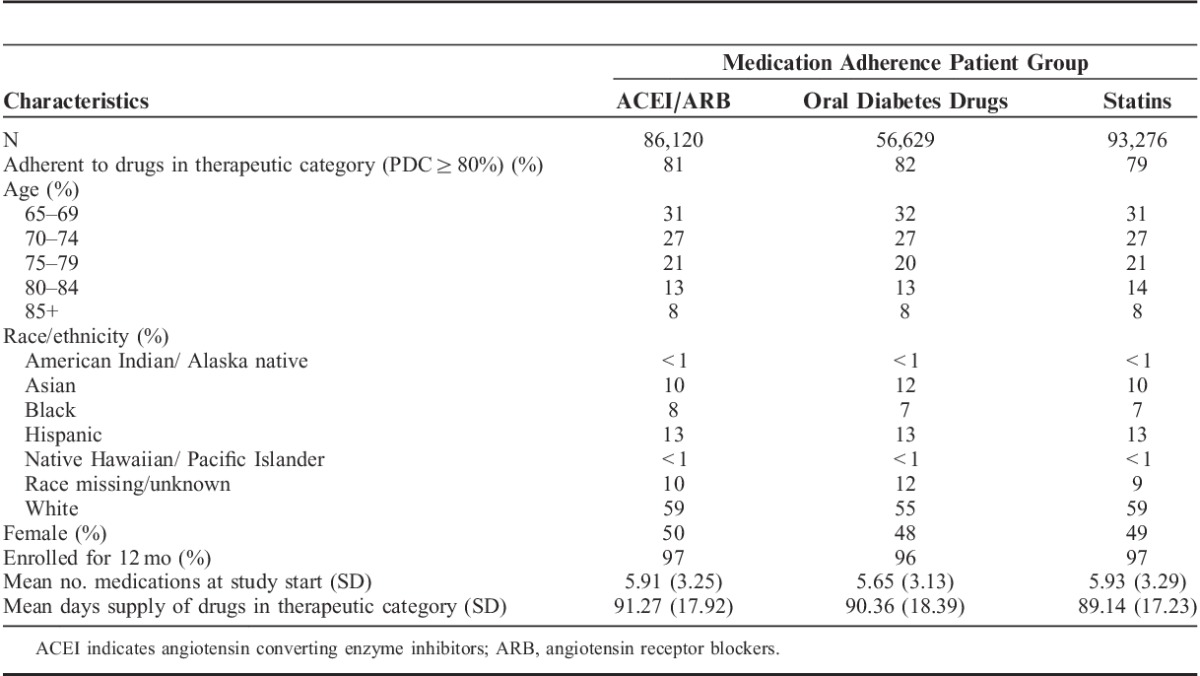
Table 2 shows predictors of whether a patient achieved the Medicare STAR adherence target of PDC≥0.8 in each therapeutic grouping. After controlling for individual-level predictors of adherence, the strongest predictor of achieving STAR-defined medication adherence was a median prescribed days’ supply of >90 days of medication in each therapeutic group (RR=1.61 for each; all P<0.001). Using mail order pharmacy to fill medications >50% of the time was independently associated with better adherence with these therapeutic groupings (RR=1.07, 1.06, 1.07 for antihypertensives, oral diabetes medications, and statins, respectively; P<0.001). Medication copays ≤$10 (RR=1.02, 1.02, 1.02; P<0.001) and annual out-of-pocket maximums ≤$2000 (RR=1.02, 1.01, 1.02; P<0.001) were also significantly associated with higher adherence for all 3 therapeutic groups. Hispanic and black patients were significantly less adherent across each therapeutic grouping. In addition, there were also a significant positive interactions between mail order pharmacy use and black race/ethnicity (RR=1.05, P<0.05; 1.05, P<0.01 for oral diabetes medications and statins, respectively), and a significant positive interaction between mail order pharmacy use and Hispanic race/ethnicity for ACEI/ARBS and statins (RR=1.03, 1.04 respectively, both P<0.001).
TABLE 2.
Estimated Risk Ratios of Being Adherent (PDC≥80%) to Medications in Therapeutic Category
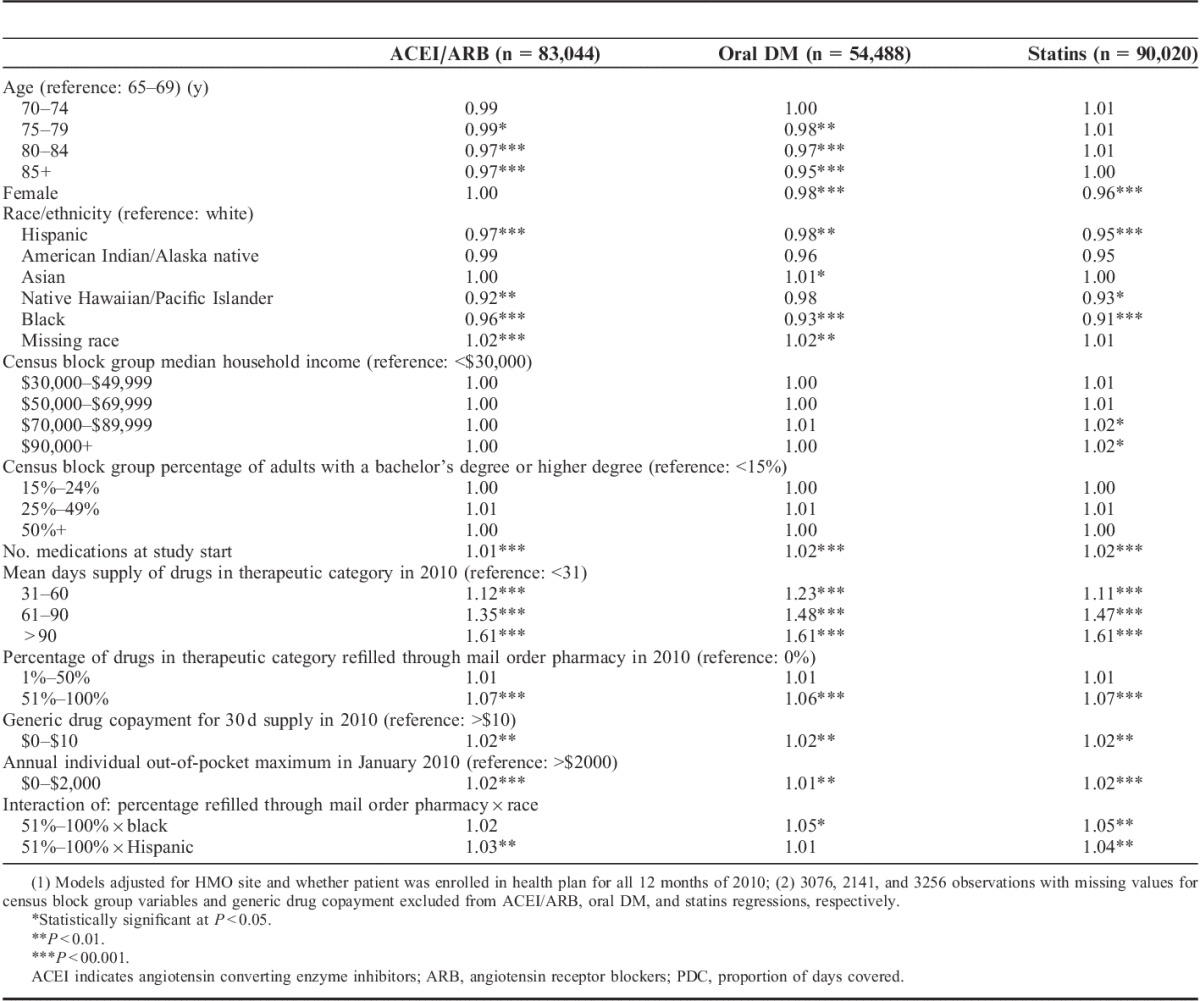
Figure 1 shows that the predicted percentage of patients who achieved medication adherence with optimized values for each of these system-level predictors was 91%, 90%, and 90% for antihypertensives, oral diabetes medications, and statins, respectively, compared with 51%, 51%, and 50%, respectively, in patients with the least optimized values for these factors.
FIGURE 1.
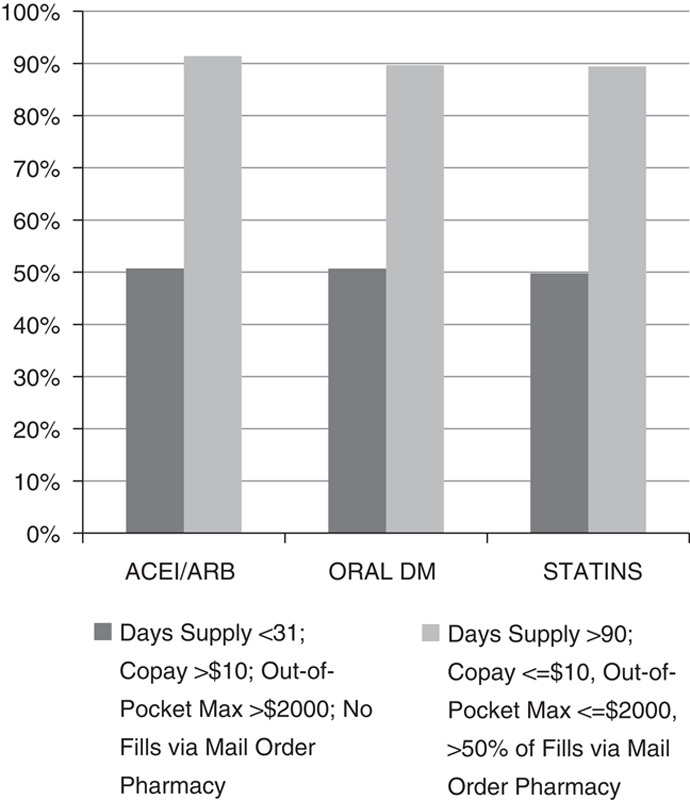
Predicted percentages of diabetes patients with good adherence at optimized versus least optimized values of health care system-level factors. Adjusted for patient age, sex, race/ethnicity, number of medications prescribed, and geocoded socioeconomic status.
DISCUSSION
We found that the strongest predictor of greater Medicare STAR adherence in 3 large Medicare Advantage providers was a greater days’ supply of medications. System-level interventions that focus on increasing the standard days’ supply of medications, especially low-cost generic medications, may be an important lever for increasing access to medications for patients at risk for low adherence.2,28–31 Having lower copays and lower annual individual out-of-pocket maximums were also associated with higher levels of medication adherence, consistent with prior work showing that diabetes patients may be vulnerable to cost-related nonadherence.32 This suggests that “value-based” insurance designs that are sensitive to the out-of-pocket costs of diabetes care may improve medication adherence for patients,33 and subsequently improve Medicare STAR adherence scores for the health plans that offer such benefit designs.
We found that medication adherence was higher among individuals with greater use of mail order pharmacy to deliver medications. Although this relationship has been demonstrated in previous research in younger patients,14–16,34 our study is the first to indicate that mail order pharmacy use is related to better adherence in Medicare-aged diabetes patients as well.
To the best of our knowledge, this study is the first to examine the cumulative effect of these 4 system-level factors on medication adherence. The predicted percentage of patients who achieved Medicare STAR adherence on these medications was approximately 90% in patients with all 4 system-level factors optimized: a level of adherence at the population level that exceeds what is required to achieve a 5-star Medicare STAR rating on these measures,24 and is almost twice the level of patients predicted to have good adherence when these health system-level factors were at the least optimized level. This suggests that multifactorial efforts to lower system-level barriers to obtaining medications can profoundly impact health plan Medicare STAR scores for CVD risk factor medication adherence. Within our study cohort, <15% of patients (data not shown) had the defined maximized values for all 4 system-level variables, suggesting that close to 90% of patients with diabetes could potentially benefit if health system-level barriers to optimizing their use of these chronic illness medications were addressed.
In this study, black and Hispanic patients derived an even greater adherence benefit from mail order pharmacy use than white patients, as demonstrated by the positive interaction between mail order pharmacy use and race/ethnicity. Mail order pharmacy use may mitigate disparities in adherence16: as mail order use eliminates the need for travel to a local pharmacy, it may have a stronger benefit for patients with transportation issues, time constraints, or other barriers to access that may particularly affect minority patients.35 However, despite this potential for increased benefit of mail order use by black and Hispanic patients compared with non-Hispanic whites, previous research suggests that nonwhite patients with diabetes are the least likely to use the mail order pharmacy.14 Understanding the reasons for these disparities in the use of mail order pharmacy, and developing effective interventions to encourage the use of mail order pharmacy among Medicare-aged patients, particularly among nonwhite patients, are important areas of future research.
Limitations
Our study included only diabetes patients; Medicare STAR metrics are also applied to hypertension or hyperlipidemia patients without diabetes. Adherence based on Medicare STAR measures in this study setting was generally high, which is consistent with this system’s high scores on other STAR metrics3; the relationship between adherence and system-level factors may be different in other settings. It is possible that the Medicare-aged diabetes patients in our study may have characteristics that differ from those in other settings, which could impact the generalizability of our findings. These findings are based on cross-sectional data: while the relationship between system-level factors and adherence suggest approaches for a trial intervention, we are unable to establish whether change in these same factors would in fact improve STAR ratings.
CONCLUSIONS
We found that system-level factors had a consistent relationship with medication adherence in Medicare-aged patients, and that optimizing these factors almost doubled the level of “good” adherence in this population. Interventions that focus on improving adherence and reducing medication adherence disparities by providing behavioral “nudges” to large populations36 should focus modifying these types of system-level barriers to obtaining evidence-based medications.
ACKNOWLEDGMENTS
The authors would like to gratefully acknowledge the contributions of Dr Michael Chase, Associate Medical Director for Quality at Kaiser Permanente Colorado; Dr Alan Whippy, Medical Director of Quality and Safety, The Permanente Medical Group, Oakland, CA; and Dr Elizabeth A. McGlynn, Director of the Kaiser Permanente Center for Effectiveness and Safety Research.
Footnotes
Supported by the Kaiser Permanente Center for Effectiveness and Safety Research, contract no. KR021125, and the Agency for Healthcare Research and Quality (AHRQ) grant R01 HS019859. J.A.S. and A.J.K. were supported by the Health Delivery Systems Center for Diabetes Translational Research (CDTR) (NIDDK grant 1P30-DK092924).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. AHRQ had no role in the design, conduct, or reporting of this work.
G.A.N. has received outside research support from AstraZeneca, Boehringer Mannheim, Merck, and Novartis. The other authors declare no conflict of interest.
REFERENCES
- 1.Kaiser Family Foundation. Reaching for the Stars: Quality Ratings of Medicare Advantage Plans, 2011. Issue Brief. Available at: http://www.kff.org/medicare/upload/8151.pdf. Accessed October 2, 2012.
- 2.Steiner JF. Rethinking adherence. Ann Intern Med. 2012;157:580–585. [DOI] [PubMed] [Google Scholar]
- 3.Schmittdiel J, Raebel M, Dyer W, et al. The Medicare STAR adherence measure excludes diabetes patients with poor CVD risk factor control. Am J Manag Care. 2015;20:e581–e589. [PMC free article] [PubMed] [Google Scholar]
- 4.Wienbergen H, Senges J, Gitt AK. Should we prescribe statin and aspirin for every diabetic patient? Is it time for a polypill? Diabetes Care. 2008;31suppl 2S222–S225. [DOI] [PubMed] [Google Scholar]
- 5.Johnson ML, Singh H. Patterns of antihypertensive therapy among patients with diabetes. J Gen Intern Med. 2005;20:842–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Konzem SL, Devore VS, Bauer DW. Controlling hypertension in patients with diabetes. Am Fam Physician. 2002;66:1209–1214. [PubMed] [Google Scholar]
- 7.Schmittdiel JA, Uratsu CS, Karter AJ, et al. Why don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. J Gen Intern Med. 2008;23:588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schmittdiel JA, Uratsu CS, Fireman BH, et al. The effectiveness of diabetes care management in managed care. Am J Manag Care. 2009;15:295–301. [PubMed] [Google Scholar]
- 9.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. [DOI] [PubMed] [Google Scholar]
- 10.Wiegand P, McCombs JS, Wang JJ. Factors of hyperlipidemia medication adherence in a nationwide health plan. Am J Manag Care. 2012;18:193–199. [PubMed] [Google Scholar]
- 11.Walker EA, Molitch M, Kramer MK, et al. Adherence to preventive medications: predictors and outcomes in the Diabetes Prevention Program. Diabetes Care. 2006;29:1997–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang Y, Thumula V, Pace PF, et al. Predictors of medication nonadherence among patients with diabetes in Medicare Part D programs: a retrospective cohort study. Clin Ther. 2009;31:2178–2188discussion 2150-2171. [DOI] [PubMed] [Google Scholar]
- 13.Raebel MA, Ellis JL, Carroll NM, et al. Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med. 2012;27:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duru OK, Schmittdiel JA, Dyer WT, et al. Mail-order pharmacy use and adherence to diabetes-related medications. Am J Manag Care. 2010;16:33–40. [PMC free article] [PubMed] [Google Scholar]
- 15.Schmittdiel JA, Karter AJ, Dyer W, et al. The comparative effectiveness of mail order pharmacy use vs. local pharmacy use on LDL-C control in new statin users. J Gen Intern Med. 2011;26:1396–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams AS, Uratsu C, Dyer W, et al. Health system factors and antihypertensive adherence in a racially and ethnically diverse cohort of new users. JAMA Intern Med. 2013;173:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nichols GA, Desai J, Elston Lafata J, et al. Construction of a multisite DataLink using electronic health records for the identification, surveillance, prevention, and management of diabetes mellitus: the SUPREME-DM project. Prev Chronic Dis. 2012;9:E110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raebel MA, Xu S, Goodrich GK, et al. Initial antihyperglycemic drug therapy among 241 327 adults with newly identified diabetes from 2005 through 2010: a surveillance, prevention, and management of diabetes mellitus (SUPREME-DM) study. Ann Pharmacother. 2013;47:1280–1291. [DOI] [PubMed] [Google Scholar]
- 19.Schmittdiel J, Raebel M, Dyer W, et al. Prescription medication burden in patients with newly-diagnosed diabetes: the SUrveillance, PREvention, and ManagEment of Diabetes Mellitus (SUPREME-DM) cohort. J Am Pharm Assoc. 2014;54:374–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raebel MA, Ellis JL, Schroeder EB, et al. Intensification of antihyperglycemic therapy among patients with incident diabetes: a Surveillance Prevention and Management of Diabetes Mellitus (SUPREME-DM) study. Pharmacoepidemiol Drug Saf. 2014;23:609–618. [DOI] [PubMed] [Google Scholar]
- 21.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27suppl 2B10–B21. [DOI] [PubMed] [Google Scholar]
- 22.O’Connor PJ, Rush WA, Pronk NP, et al. Identifying diabetes mellitus or heart disease among health maintenance organization members: sensitivity, specificity, predictive value, and cost of survey and database methods. Am J Manag Care. 1998;4:335–342. [PubMed] [Google Scholar]
- 23.Zgibor JC, Orchard TJ, Saul M, et al. Developing and validating a diabetes database in a large health system. Diabetes Res Clin Pract. 2007;75:313–319. [DOI] [PubMed] [Google Scholar]
- 24.Medicare Health and Drug Plan Quality and Performance Ratings, 2013 Part C and Part D Technical Notes—First Plan Preview–Draft. CMS website. Available at: http://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/Technical-Notes-2013-.pdf. Updated August 9, 2012.
- 25.Pharmacy Quality Alliance. Proportion of Days Covered (PDC) as a preferred method of measuring medication adherence. Available at: http://www.pqaalliance.org/images/uploads/files/PQA%20PDC%20vs%20%20MPR.pdf. Accessed January 16, 2015.
- 26.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 27.Cameron AC, Trivedi PK. Microeconometrics Using Stata, Revised Edition. 2010College Station, TX: STATA Press. [Google Scholar]
- 28.Shrank WH, Stedman M, Ettner SL, et al. Patient, physician, pharmacy, and pharmacy benefit design factors related to generic medication use. J Gen Intern Med. 2007;22:1298–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steiner JF, Robbins LJ, Roth SC, et al. The effect of prescription size on acquisition of maintenance medications. J Gen Intern Med. 1993;8:306–310. [DOI] [PubMed] [Google Scholar]
- 30.Batal HA, Krantz MJ, Dale RA, et al. Impact of prescription size on statin adherence and cholesterol levels. BMC Health Serv Res. 2007;7:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foster DG, Hulett D, Bradsberry M, et al. Number of oral contraceptive pill packages dispensed and subsequent unintended pregnancies. Obstet Gynecol. 2011;117:566–572. [DOI] [PubMed] [Google Scholar]
- 32.Schmittdiel JA, Ettner SL, Fung V, et al. Medicare Part D coverage gap and diabetes beneficiaries. Am J Manag Care. 2009;15:189–193. [PMC free article] [PubMed] [Google Scholar]
- 33.Choudhry NK, Avorn J, Glynn RJ, et al. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–2097. [DOI] [PubMed] [Google Scholar]
- 34.Choudhry NK, Fischer MA, Smith BF, et al. Five features of value-based insurance design plans were associated with higher rates of medication adherence. Health Aff (Millwood). 2014;33:493–501. [DOI] [PubMed] [Google Scholar]
- 35.Duru OK, Gerzoff RB, Selby JV, et al. Identifying risk factors for racial disparities in diabetes outcomes: the translating research into action for diabetes study. Med Care. 2009;47:700–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thaler RH, Sunstein CR. Nudge: Improving Decisions About Health, Wealth, and Happiness. 2008New Haven, CT: Yale University Press. [Google Scholar]


