Abstract
Rationale, aims and objectives
Complex and chronic disease is placing significant pressure on hospital outpatient departments. Novel ways of delivering care have been developed recently and are often described as ‘triage’ services. This paper reviews the literature pertaining to definitions and descriptions of orthopaedic/musculoskeletal triage processes, in order to provide information on ‘best practice’ to assist health care facilities.
Method
A comprehensive open-ended search was conducted using electronic databases to identify studies describing models of triage clinics for patients with a musculoskeletal/orthopaedic complaint, who have been referred to hospital outpatient clinics for a surgical consultation. Studies were critically appraised using the McMaster quality appraisal tool and ranked using the National Health and Medical Research Council hierarchy of evidence. A thematic analysis of the definitions, processes and procedures of triage described within the literature was undertaken.
Results
1930 studies were identified and 45 were included in the review (including diagnostic and evaluative research). The hierarchy of evidence ranged from I to IV; however, the majority were at low levels of evidence and scored poorly on the critical appraisal tool. Three broad themes of triage were identified: presence of a referral, configuration of the triage (who, how and where) and the aim of triage. However, there were significant inconsistencies across these themes.
Conclusions
This systematic review highlighted the need for standardization of the definition of triage, the procedures of assessment and management and measures of outcome used in orthopaedic/musculoskeletal triage to ensure best-practice processes, procedures and outcomes for triage clinics.
Keywords: orthopaedic/musculoskeletal triage, role substitution, systematic review, triage clinics, workforce redesign
Introduction
There are increasing pressures on hospital outpatient departments to provide timely medical and allied health care for increasing numbers of patients with orthopaedic/musculoskeletal complaints [1–4]. These changes are linked to a rise in chronic and complex diseases particularly in an aging population [1,5]. For instance, it has been projected that by 2020, osteoarthritis will be the fourth leading cause of disability [6]. The Australian Institute of Health and Welfare [7] identified that osteoarthritis currently affects approximately 23% of males and 40% of females aged 75 years and over. Thus, the pressures on hospital outpatient departments are likely to continue to rise to deal with increasing population need.
For the purpose of this paper, orthopaedics is defined by the Collins English Dictionary [8] as
“The branch of surgery concerned with disorders of the spine and joints and the repair of deformities of these parts”
While musculoskeletal is defined by the Collins English Dictionary [8] as issues relating
“Of or to the skeleton and musculature”
Health departments and hospitals particularly in the United Kingdom and in Australia have been exploring alternative workforce models of care to meet the increasing need for health services for patients with chronic orthopaedic/musculoskeletal complaints 3,9–10. These include new pathways of care and changes in the traditional models of care within the health workforce [2,12]. The common goals of these workforce reform initiatives are to provide timely appointments, with appropriately qualified health care professionals, to direct patients towards the optimal treatment pathway, to streamline valuable medical consultant time and minimize time ‘wasted’ on waiting lists [2]. However many of the workforce reforms have been driven by individual hospital administrators, department heads or clinicians and as such, there is considerable variation reported in the literature regarding the construct and delivery of such initiatives.
Consequently, despite the increasing prevalence of workforce reform initiatives, little is known about how they have been constructed, operationalized or evaluated. There is also a lack of consistency at national/international level regarding the processes, outcome measures and effectiveness of such initiatives [12]. This constrains opportunities for widespread adoption and standardization of best practices. For instance, workforce reform initiatives, within the context of outpatient services for patients with an orthopaedic/musculoskeletal complaint, are commonly reported as a form of triage. However, there are no clear descriptions of effective triage processes within this context, how the triage occurs, which health professionals are responsible for it and what the outcomes are.
This paper aims to synthesize all available information described in the literature about triage processes within the context of outpatient services, regarding procedures, interventions and structures for patients referred for surgical consultation with an orthopaedic/musculoskeletal complaint. A collation and synthesis of this information will provide current comprehensive best-practice information to assist hospitals to set up new triage initiatives, and review existing initiatives appropriately.
Methods
Review purpose
The purpose of this research was to systematically review all available, relevant literature, which described models of triage clinics for patients with a musculoskeletal/orthopaedic complaint, who have been referred to a hospital outpatient clinic for a surgical consultation.
Aim of this paper
This paper reports the definitions and descriptions of the triage process, in order to provide information on ‘best practice’ to assist health care facilities in the establishment of new triage services or the review of existing services.
Search strategy
A PI approach (participants, interventions) was used to underpin the search strategy. No comparator or outcome measure was specified. Electronic library databases of MEDLINE, Embase, CINAHL and Scopus were searched with no start or end date set, and with broad search terms and inclusion criteria; in an attempt to identify all relevant papers regarding the use of triage for patients with orthopaedic complaints. The database searches were undertaken between 13 January 2014 and 22 January 2014. Duplicates were removed prior to considering full text papers for inclusion in the review.
Table 1 outlines the search terms. Additional relevant papers were pearled from the reference lists of the papers identified by the electronic library database search.
Table 1.
Definition of PI and MESH terms
| Definition | MESH terms | |
|---|---|---|
| Population | Patients with an orthopaedic complaint | Orthop?dic Musculoskeletal |
| Intervention | Triage, assessment | Triag Ambulatory Care Assessment Clinic |
Population
Studies were included if they described adults with an orthopaedic and/or a musculoskeletal complaint who had been referred for a surgical/specialist consultation to an outpatient clinic. No limitations were applied in terms of diagnostic categories.
Intervention
Studies were included if they described an intervention in the form of a triage clinic or triage process, including review of paper referrals and/or face-to-face review in clinics. Triage clinics could include single or multidisciplinary configurations which offered any form of triage/assessment service for patients with a musculoskeletal/orthopaedic complaint.
Eligible studies
To ensure that the maximum information was obtained, studies at all levels of evidence were included, ranging from randomized controlled trials to letters to the editors and opinion pieces. Each potentially relevant paper was then screened via the titles and abstract by the two researchers working together, for relevance to the overall study purpose. All papers that described any aspect of service delivery model, in any context or configuration, that described assessment/management of patients with an orthopaedic and/or musculoskeletal complaint who had been referred for a surgical/specialist consultation, were included. Articles were excluded if they did not pertain to the management of orthopaedic conditions or describe a process of triage for patients with a musculoskeletal/orthopaedic complaint. Specific exclusion criteria were set, related to studies that referred to post-surgical follow-up or patient review appointments (thus, the focus was on new patients and patients prior to surgery), and non-refereed conference abstracts. Only papers in English language and reported on adult populations (age 18 and over) were included.
Hierarchy of evidence
The hierarchy of evidence of each included study was determined according to the National Health and Medical Research Council (NHMRC) Hierarchy of Evidence for intervention studies [13].
Quality appraisal
The McMaster quality appraisal tool [14] was used to critically appraise the methodological quality of included papers. This tool was chosen due to its relevance to all levels of evidence. The McMaster tool comprises 15 items that assess studies for purpose, design, sample, outcomes, interventions, results and clinical implications. Fourteen of the 15 items have a ‘yes’, ‘no’, ‘not addressed’ or ‘not applicable’ response, while the remaining item allows for a description of the design of the study (this question is not included in the scoring). The two reviewers awarded one point for a ‘yes’ response and no point for ‘no’ or ‘not addressed’. For questions that received a ‘not applicable’ response (where the McMaster question was not relevant for any study), the denominator was adjusted accordingly. The per-paper raw score was expressed as a percentage, considering the number of criteria on which a paper could possibly score ‘yes’ as a percentage of the total possible relevant criteria, which could be scored for that paper.
Any discrepancies between authors for hierarchy of evidence rating or McMaster tool score were resolved through discussion and, if required, arbitration by a third independent reviewer to reach consensus.
Data extraction and analysis
Where reported, data was extracted verbatim from papers in relation to definitions and processes of triage and entered into a purpose-built Microsoft Excel spreadsheet.
The data on triage purpose, processes and types was largely descriptive. We attempted to qualitatively analyse this information for emergent key themes using independent hand-coding by the researchers, in the manner described by Rice & Ezzy [15]. Discussion between the researchers regarding the appropriate classifications and interpretations of triage purpose, process and type then occurred and the resultant key agreed themes were retained.
The key themes, the hierarchy of evidence of the papers that generated them, and their methodological quality were linked, and patterns that emerged from the types and quality of research studies, and key themes were explored.
Results and discussion
The search found a total of 1930 studies, which were potentially eligible for this review (see Fig. 1). Of these, 204 were duplicates, 1673 were removed as not relevant through analysis of title and abstract, six more were pearled from reference lists, 14 were excluded on review of full text, resulting in 45 papers relevant for this review.
Figure 1.
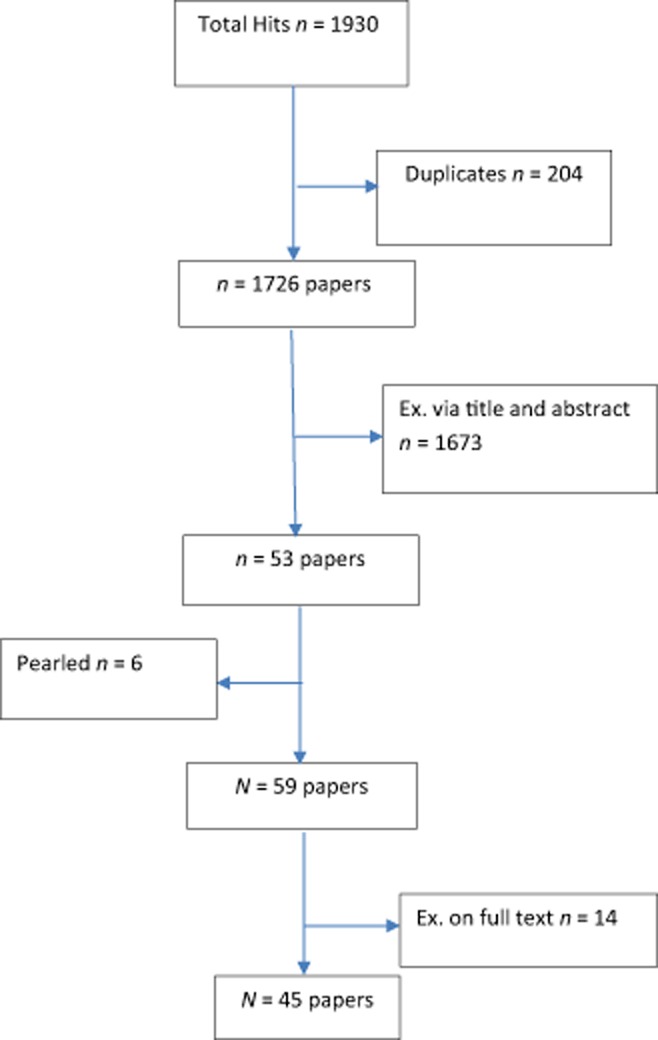
Consort diagram for these review findings reported in this paper.
Excluded studies
The main reason for exclusion was that the papers did not report on studies related to triage of new or pre-surgical patients.
Hierarchy of evidence and methodological quality
The included papers were low on the hierarchy of evidence (ranked III-3 or IV) and most scored poorly on critical appraisal. Considering the hierarchy of evidence, one paper was at levels I, II and III-1 paper, three level III-2 papers, eight papers ranked III-3 (comprising two quasi-experimental studies, one validation study, two prospective studies, one cross-sectional survey and two cohort studies) and 29 papers ranked IV (comprising three opinion pieces, 10 audits and 17 case series). The research design of one paper could not be scored on the NHMRC system, as it was a letter to the editor.
The percentage methodological quality scores ranged from 13% to 100%. Most differences in assigning critical appraisal scores between the two reviewers were due to misinterpretation of the scoring system, and were readily reconciled with discussion (Table 2).
Table 2.
Hierarchy of evidence and critical appraisal scores
| McMaster | 1 | 2 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | Total | % McMaster | NHMRC rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aiken [24] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | N/A | 0 | 1 | 1 | 1 | 1 | 1 | 12/13 | 92 | IV |
| Aiken [53] | 1 | 1 | 0 | 0 | 1 | 1 | 1 | N/A | 1 | 1 | 1 | 1 | 0 | 1 | 10/13 | 77 | III-3 |
| Aiken [25] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | 0 | 0 | 0 | 1 | 0 | 1 | 6/13 | 46 | III-3 |
| Aiken [54] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | N/A | 0 | 0 | 1 | 1 | 0 | 1 | 6/13 | 46 | N/A |
| Bath [26] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | N/A | 0 | 1 | 1 | 1 | 0 | 1 | 11/13 | 85 | IV |
| Bath [27] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | N/A | 0 | 1 | 1 | 1 | 0 | 1 | 9/13 | 69 | IV |
| Bernstein [55] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | N/A | N/A | 1 | 1 | 1 | 0 | 1 | 9/12 | 75 | IV |
| Blackburn [2] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | N/A | N/A | 0 | 0 | 1 | N/A | 1 | 8/11 | 73 | IV |
| Brand [16] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | N/A | 0 | 1 | 1 | 1 | 0 | 1 | 10/13 | 77 | IV |
| Busse [28] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | 1 | 1 | 1 | 11/12 | 92 | IV |
| Curley [29] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | N/A | N/A | 0 | 1 | 1 | N/A | 1 | 10/12 | 83 | IV |
| Daker-White [30] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14/14 | 100 | II |
| Desmeules [31] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | N/A | 1 | 1 | 1 | 1 | 1 | 12/13 | 92 | III-1 |
| Durrell [32] | 0 | 1 | 0 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | N/A | 1 | 0 | 1 | 3/11 | 27 | IV |
| Griffiths [17] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 8/12 | 67 | IV |
| Morris [3] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | N/A | 0 | 1 | 1 | 1 | 1 | 1 | 11/13 | 85 | III-3 |
| Stanhope [44] | 1 | 1 | N/A | N/A | 1 | 1 | 1 | N/A | N/A | N/A | 1 | 1 | N/A | 1 | 8/8 | 100 | I |
| Hattam [56] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | 1 | N/A | 1 | 10/11 | 91 | IV |
| Hattam [33] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | 0 | 0 | 1 | 1 | 1 | 1 | 8/13 | 62 | III-3 |
| Heyes-Moore [18] | N/A | ||||||||||||||||
| Heywood [34] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 8/12 | 67 | IV |
| Homeming [35] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | N/A | 1 | 7/11 | 64 | IV |
| Hourigan [36] | 1 | 0 | 1 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 6/12 | 50 | III-2 |
| Hourigan [52] | 1 | 0 | 1 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 6/12 | 50 | IV |
| Kennedy [19] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 12/14 | 86 | III-3 |
| Klett [37] | 1 | 0 | 0 | 0 | 1 | 1 | 0 | N/A | N/A | 1 | 1 | 1 | 0 | N/A | 8/12 | 67 | IV |
| MacKay [12] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | N/A | 1 | 1 | 1 | 1 | 1 | 10/13 | 77 | III-2 |
| Maddison [10] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | N/A | 1 | 0 | 0 | 2/12 | 17 | IV |
| Napier [38] | 1 | 1 | 1 | 1 | N/A | N/A | 0 | 0 | N/A | 1 | 1 | 1 | 1 | 1 | 9/11 | 82 | III-2 |
| O'Brien [39] | 1 | 0 | 1 | 1 | 0 | 0 | 0 | N/A | N/A | 1 | 1 | 1 | 1 | 1 | 8/12 | 67 | III-3 |
| Oldmeadow [4] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | N/A | 1 | 1 | 1 | 1 | 1 | 9/12 | 75 | III-3 |
| Parfitt [20] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | 0 | 1 | 7/12 | 58 | IV |
| Pearse [48] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | 0 | 1 | N/A | 1 | 3/11 | 27 | IV |
| Poder [21] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | N/A | N/A | 1 | 0 | 1 | 0 | 0 | 7/12 | 58 | III-2 |
| Rabey [40] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | 0 | 1 | 6/12 | 50 | IV |
| Razmjou [41] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | N/A | 1 | 1 | 1 | 1 | 1 | 9/13 | 69 | III-3 |
| Reeve [42] | 1 | 1 | 1 | 0 | 0 | 0 | 1 | N/A | N/A | N/A | 1 | 1 | 1 | 1 | 8/11 | 73 | IV |
| Rogers [22] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | 0 | 1 | 0 | 1 | 4/12 | 33 | IV |
| Rymaszewski [43] | 1 | 0 | 0 | 0 | N/A | N/A | 1 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 6/10 | 60 | IV |
| Schoch [49] | 1 | 0 | 0 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 6/12 | 50 | IV |
| Sephton [50] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | N/A | 0 | 1 | 1 | 1 | 1 | 1 | 10/13 | 77 | IV |
| Speed [51] | 1 | 1 | 1 | 0 | 0 | 0 | 0 | N/A | N/A | 0 | 1 | 1 | 0 | N/A | 5/12 | 42 | IV |
| Vizzini [23] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | N/A | N/A | 1 | 1 | 1 | 0 | N/A | 7/13 | 54 | IV |
| Weatherley [45] | 1 | 0 | 0 | 0 | 0 | 0 | 1 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 6/12 | 50 | IV |
| Weston-Simons [46] | 1 | 1 | 0 | 0 | N/A | N/A | 1 | N/A | N/A | 0 | 1 | 1 | 1 | 1 | 7/10 | 70 | IV |
| Wright [47] | 0 | 0 | 0 | 0 | N/A | N/A | 0 | N/A | N/A | 0 | N/A | 0 | 1 | N/A | 1/8 | 13 | IV |
Data synthesis
Considering the use of the term ‘triage’ in the context of the management of patients with an orthopaedic/musculoskeletal complaint, our thematic analysis demonstrated that this word has a variety of meanings, descriptions and definitions and is applied within, different health care settings, in a variety of methods. Of the 45 papers, eight did not provide adequate descriptions of triage and were therefore removed from the thematic analysis 16–23.
The only consistent theme, mentioned in 29 of the included articles, was that the purpose of triage was to address extensive waiting times for specialty services through a streamlined, screening process 3,4,10–12,16,24–47. The broad themes, descriptions and processes of triage revealed by the thematic analysis of the reviewed papers are summarized in Table 3 and discussed in detail in subsequent sections.
Table 3.
Themes, descriptions and processes of triage
| Frequently reported themes of triage |
|---|
| The presence of a referral: |
| Who it was from? |
| The configuration of the triage: |
| Who undertakes triage? |
| How is triage undertaken? |
| Where is triage undertaken? |
| Aim/purpose of triage |
Referrals
Where mentioned, the information in relation to the referral processes, including who the referral was to and who was involved in the processing of the referral, was extrapolated from each paper and those which reported on the referral process are expressed in Table 4.
Table 4.
Papers that reported on a referral process
| Paper | Referral from | Who was involved in triage |
|---|---|---|
| Aitken [24] | GP | Physio, surgeon |
| Aiken [53] | Not mentioned | Physio, surgeon |
| Aiken [25] | Not mentioned | Physio |
| Bath [26] | GP | Physio |
| Bath [27] | GP | Physio |
| Bernstein [55] | GP | Physio, surgeon |
| Blackburn [2] | GP | Physio, surgeon |
| Brand [16] | GP | Surgeon |
| Busse [28] | Not mentioned | Clinicians, surgeons |
| Curley [29] | GP | Physio, registrars |
| Daker-White [30] | GP | Physio, doctor |
| Desmeules [31] | Not mentioned | Advanced practice physiotherapists, surgeon |
| Durrell [32] | GP | Extended scope physio, surgeon |
| Griffiths [17] | GP | Extended scope physiotherapist |
| Morris [3] | Medical practitioner | Physio |
| Stanhope [44] | Medical doctor (usually GP) | Extended scope practitioner physiotherapist |
| Hattam [56] | GP | Extended scope physiotherapists |
| Hattam [33] | GP | Physio |
| Heyes-Moore [18] | GP and physio | Physio and surgeon |
| Heywood [34] | Not mentioned | Physiotherapist extended scope practitioner, surgeon |
| Homeming [35] | Not mentioned | Podiatrists, physiotherapists and clinical nurses. |
| Hourigan [36] | GP | Physio |
| Hourigan & Weatherley [52] | GP | Physio |
| Kennedy [19] | Not mentioned | Advanced practice physiotherapist (APP) and orthopaedic surgeon |
| Klett [37] | Various doctors | Doctors |
| MacKay [12] | Not mentioned | Physiotherapists and orthopaedic surgeons |
| Maddison [10] | GP | General practitioners, extended scope physiotherapist |
| Napier [38] | GP | Physio |
| O'Brien [39] | GP | OT |
| Oldmeadow [4] | GP | Physio, surgeon |
| Parfitt [20] | GP | extended scope physiotherapist, surgeon |
| Pearse [48] | GP | Extended scope physiotherapist |
| Poder [21] | GP | Nurse practitioners, extended scope practitioners, doctor assistants Pivot nurse, physio, ergotherapist, orthopaedic doctor, GP, nutritionist and/or psychologist |
| Rabey [40] | GP | Physio, practitioner |
| Razmjou [41] | Not mentioned | Advanced-practice physiotherapists, surgeons |
| Reeve [42] | GP | Extended scope practitioner (ESP) physiotherapists |
| Rogers [22] | GP | Multi-professional triage teams – general Practitioners with special interests, physios, surgeon |
| Rymaszewski [43] | GP | Nurses, physios, podiatrist to orthopaedic surgeon and rheumatologist |
| Schoch [49] | GP | Physio, nurse, surgeon |
| Sephton [50] | GP National Health Care Service Centres |
Musculoskeletal clinical assessment service (physio, advanced musculoskeletal physiotherapy practitioners or podiatrist) |
| Speed [51] | GP | Rheumatologist or orthopaedic surgeon |
| Vizzini [23] | Doctor | Doctor and surgeon |
| Weatherley [45] | GP | Physio and surgeon |
| Weston-Simons [46] | Not mentioned | Extended scope practitioner (ESP) and surgeon |
| Wright [47] | GP | Physio |
The majority of the literature reports that triage was undertaken in the context of a referral being made from one health care provider to another. The referral was usually to a specialist for an expert opinion, which often occurred in a tertiary health care setting. Also reported were within-specialists referrals (e.g. one orthopaedic surgeon to another).
A summary of whom the referral was from is summarized in Fig 2:
Figure 2.
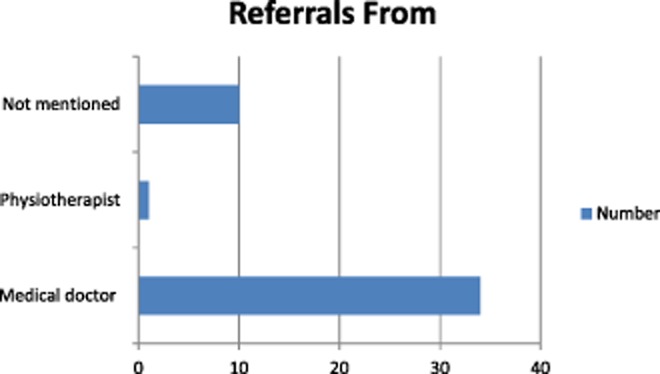
Summary of whom referrals were from.
Configuration of triage
Where the ways in which triage were delivered was reported, there was considerable variability in context, staffing and methods of triage. Triage was reported in the context of team-based triage and single discipline (most commonly reported as physiotherapists when single discipline was reported). The referral data in Table 4 has been further extrapolated and presented in Fig 3, which details the different health professions undertaking triage.
Figure 3.
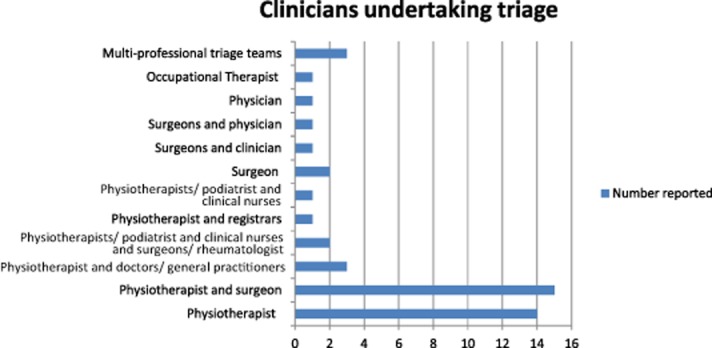
Health professions undertaking triage.
How is triage undertaken?
A small number of papers reported the use of a standardized tool in the process of triage [3,35,37,43,48]. Standardized tools were reported in the context of triage, using paper referral [3,43,48] and, in a small number of cases, a standardized tool within the clinical setting for direct patient assessment [35,37,41]. The remaining papers identified that the clinical assessment being undertaken as part of the triage was at the discretion of the clinician undertaking the triage. The expert clinical skills of the health professionals undertaking the triage were frequently identified as appropriate and reportedly negated the need for a standardized approach [12,31,36,38]. A number of the identified studies were undertaken for the purpose of skill validation of allied health clinicians undertaking a role traditionally done by a medical specialist, reported as role substitution [12,26,33,34,35,38,42]. In these studies, assessment was completed by two clinicians, with the medical practitioner's assessment used as the ‘gold standard’ assessment.
Role substitution was frequently described as a means of streamlining patient flow by using other non-traditional health professions in the management of the referred patients. One of the key reasons reported for role substitution was to reserve more complex tasks for the specialist practitioner (predominantly surgeons). Repeatedly, physiotherapists were reported to undertake a role traditionally reserved for a surgeon. One component of this role mentioned in the literature was direct listing for surgery by the ‘role substitution’ practitioners [20,46].
Where is triage undertaken?
Most commonly, the papers reported that triage occurs in the context of an outpatient clinic setting, in primary and secondary care. However, a small number of papers reported triage of the paper referral 48–51, sometimes as a pre-cursor to a clinic-based triage process, at times as a standalone process.
Aims of triage
The broad purposes of triage appear to be to address areas of high demand, evidenced by long waiting times for appointments, and to assist with directing patients to the most relevant clinicians for their care 3,4,10,16,24–26,28–34,36,39,41,44,45,47. Triage was repeatedly reported as a waiting list management strategy in order to meet organizational or government-set targets.
Additionally, triage was reportedly undertaken to enhance effectiveness and best care/practice. This predominantly referred to timely access to the right care from the right clinicians [4,10,24,35,46,49]. A component of this was streamlining/screening patients to most appropriate care; in this context, this was broadly identified as surgical or conservative treatment. The screening was either of referrals or patients (one reports [29] of use of a standardized tool to do this) 3,4,10,12,16,24–47.
Eight papers 4,32,35,40–42,46,49 specifically reported that the triage process is used to assess, diagnose and develop management plans for patients referred to a speciality service. A component of this process is reported to be ordering and interpreting investigations. In some cases, it was reported that the triage process also includes the provision of treatment, including medications and injections, in the context of primary care. In some instances this included offering services to patients previously unavailable in their local community.
A summary of the reported aims of triage is detailed in the chart below (Fig. 4).
Figure 4.
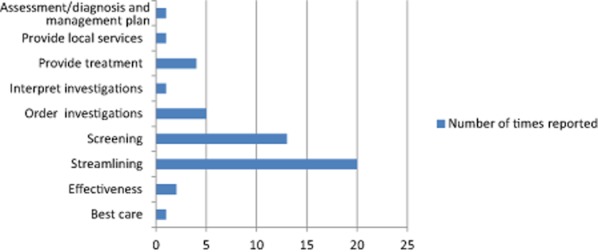
Aims of triage.
Common diagnoses described
The literature identified described a wide variety of conditions diagnosed as an outcome of the triage process. A number of studies reported that inclusion into the triage clinics were restricted to specific areas of injury, most commonly reported were clinics that assessed patients with hip, knee, shoulder and spinal problems 2,8,25–29,31,36,52, specific diagnoses were infrequently reported as papers pertained to service delivery.
Summary of results
The literature cited in this paper identified three themes of triage in the context of patients with an orthopaedic/musculoskeletal complaint, who have been referred for a surgical/specialist consultation; the presence of a referral, the configuration of the triage (who, how and where) and the aim of triage. Within these, however, there is variability in how triage is defined, the methods by which triage is undertaken and the practitioners involved in undertaking triage. No standardized, evidence-based or recognized approach in the assessment, management and subsequent treatment of patients with an orthopaedic/musculoskeletal condition undertaken in the triage process was described, nor the consistent use of recognized outcome measures and methods of evaluation. Therefore, translation of these processes and procedures from one health care facility to another is exceptionally difficult.
There are consistent themes regarding the purpose of triage: the screening/streamlining of patients to the most suitable care pathway for their condition. However overall, the processes, procedures and measures of outcome are poorly described and lack consistency and an evidence-based approach.
Limitations of the study
This review attempted to provide a comprehensive summary of the current peer-reviewed literature to describe models of triage clinics for patients with a musculoskeletal/orthopaedic complaint, who have been referred to a hospital outpatient clinic for a surgical consultation. The databases searched were those that we believed would provide access to the most relevant peer-reviewed literature; however, relevant studies published in databases that were not searched would not have been identified. The qualitative approach to theme the definitions of orthopaedic triage review was undertaken in an attempt to draw out the subtleties of how, who, when and why orthopaedic triage occurred; however, we may have overlooked specific issues that could have better informed the synthesis from this review. This review did not attempt to measure the effectiveness of orthopaedic triage; however, given the complexities of orthopaedic triaging processes identified in this review, we believe that this could be the subject of future research.
Implications of findings
This review highlighted an urgent need to develop a consistent approach to triage of patients with an orthopaedic/musculoskeletal complaint, in the outset, an agreed definition of triage and components used when describing triage is recommended. The literature indicates that when describing triage, there are key factors that should be included, such as which clinicians can refer to the triage service, which clinicians are involved in triage and the development of a standardized, safe, evidence-based and consistent approach to triage, which may include the use of recognized outcome measures and assessment tools. In addition, there needs to be a clearly stated and measurable aim of the triage process, which allows hospital/health administrators to articulate to patients, carers and key stakeholders the purpose of triage in terms of safety, best practice and economic principles.
Conclusion
This systematic review is a first of its kind to describe the various ways in which triage is undertaken for patients with an orthopaedic/musculoskeletal complaint, who have been referred for a surgical/specialist consultation. There is no consistent definition of triage described in the literature and there are institution-by-institution differences in how triage is undertaken, in terms of location, staffing and use of standardized tools for triage. As such, an evidence-based, consistent approach that is applicable across a broad range of health care providers, which ensures that patients are receiving an appropriate standard of care, cannot be defined or described.
There is some consistency regarding the aim of triage, which is frequently described as a means of addressing lengthy waiting times for specialist appointments through a streamlining/screening approach. This has proven to provide an effective and efficient service to patients at reduced cost and has assisted with the streamlining of valuable medical consultant time and improving pathways of care for patients 2,3,12]. However, there are inconsistencies in its aims such as provision of treatment, ordering and interpreting imaging and onward referral patterns.
This systematic review highlighted the need for standardization of the definition of triage, the procedures of assessment and management and measures of outcome in the context of patients with an orthopaedic/musculoskeletal complaint whom have been referred for a surgical/specialist consultation and agreement regarding the processes of triage. Agreement around these factors and standardization of care will ensure best-practice processes for triage clinics, which should lead to improved health and cost outcomes, with greater consistency and agreement across different health care facilities. Such standardization will provide assistance to health care facilities developing a new triage service or reviewing an existing service.
Acknowledgments
The authors thank Professor Karen Grimmer and Mr Robert Marshall.
References
- 1.Birch S, Mason T, Sutton M. Whittaker W. Not enough doctors or not enough needs? Refocusing health workforce planning from providers and services to populations and needs. Journal of Health Services and Research Policy. 2013;18(2):107–113. doi: 10.1177/1355819612473592. doi: 10.1177/1355819612473592. (last accessed 3 March 2014). [Internet] [DOI] [PubMed] [Google Scholar]
- 2.Blackburn M, Cowan S, Cary B. Nall C. Physiotherapy-led triage clinic for low back pain. Australian Health Review. 2009;33(4):663–670. doi: 10.1071/ah090663. doi: 10.1071/AH090663. [DOI] [PubMed] [Google Scholar]
- 3.Morris J, Grimmer-Somers K, Kumar S, Murphy K, Gilmore L, Ashman B, Perera C. Coulter C. Effectiveness of a physiotherapy-initiated telephone triage of orthopaedic waitlist patients. Patient Related Outcome Measures. 2:151–159. doi: 10.2147/PROM.S2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oldmeadow LB, Bedi HS, Burch HT, Smith JS, Leahy ES. Goldwasser M. Experienced physiotherapists as gatekeepers to hospital orthopaedic outpatient care. Medical Journal of Australia. 2011;186(12):625–628. doi: 10.5694/j.1326-5377.2007.tb01079.x. 2007. [DOI] [PubMed] [Google Scholar]
- 5.Borland J. 2011. Report to the Australian Competition and Consumer Commission on: Australian Medical Workforce Advisory Committee –The Orthopaedic Surgery Workforce in Australia, an Update: 1998 to 2009’. Canberra: Australian Competition and Consumer Commission. [Internet] Available at: http://www.accc.gov.au/system/files/Report to ACCC – AMWAC Orthopaedic Surgery Workforce in Australia.pdf (last accessed 2 February 2014)
- 6.Woolf AD. Pfleger B. Burden of major musculoskeletal conditions. Bulletin of the World Health Organization. 2003;81(9):646–656. doi: http://dx.doi.org/10.1590/S0042-96862003000900007. [PMC free article] [PubMed] [Google Scholar]
- 7.Australian Institute of Health and Welfare. 2013. AIHW: Web snapshot on osteoarthritis [Internet] 2013 [updated 2013 May 17]. Available at: http://www.aihw.gov.au/osteoarthritis/ (last accessed 20 March 2014)
- 8.Collins English Dictionary. 2014. ). Available at: http://www.collinsdictionary.com/ (last accessed 3 August 2014)
- 9.Harrison J, Rangan A, Shetty A. Robinson C. Reducing waiting times: physiotherapy shoulder assessment clinic. British Journal of Therapy and Rehabilitation. 8(2):57–59. [Google Scholar]
- 10.Maddison P, Jones J, Breslin A, et al. Improved access and targeting of musculoskeletal services in northwest Wales: targeted early access to musculoskeletal services (TEAMS) programme. British Medical Journal. 329(7478):1325–1327. doi: 10.1136/bmj.329.7478.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moloney A, Dolan M, Shinnick L, Murphy M. Wallace L. A 6-month evaluation of a clinical specialist physiotherapist's role in a fracture clinic. Physiotherapy Ireland. 2001;30(1):8–15. 2004-2009. doi: 10.3233/PPR-20009-30104. [Google Scholar]
- 12.MacKay C, Davis AM, Mahomed N. Badley EM. Expanding roles in orthopaedic care: a comparison of physiotherapist and orthopaedic surgeon recommendations for triage. Journal of Evaluation in Clinical Practice. 2009;15(1):178–183. doi: 10.1111/j.1365-2753.2008.00979.x. doi: 10.1186/1472-6963-8-147. [DOI] [PubMed] [Google Scholar]
- 13.National Health and Medical Research Council. NHMRC Levels of Evidence and Grade for Recommendations for the Developers of Guidelines. Canberra: Australian Government; 2009. Available at: https://www.nhmrc.gov.au/_files_nhmrc/file/guidelines/developers/nhmrc_levels_grades_evidence_120423.pdf (last accessed 1 April 2014). [Internet] [Google Scholar]
- 14.Law M, Stewart D, Pollock N, Letts L, Bosch J. Westmorland M. 1998. & Critical review form-quantitative studies. [Internet]. Available at: http://www.srs-mcmaster.ca/Portals/20/pdf/ebp/quanreview.pdf (last accessed 3 February 2014)
- 15.Rice PL. Ezzy D. Qualitative Research Methods: A Health Focus. Oxford: Oxford University Press; 1999. [Google Scholar]
- 16.Brand CA, Amatya B, Gordon B, Tosti T. Gorelik A. Redesigning care for chronic conditions: improving hospital-based ambulatory care for people with osteoarthritis of the hip and knee. Internal Medicine Journal. 2010;40(6):427–436. doi: 10.1111/j.1445-5994.2009.01960.x. doi: http://dx.doi.org/10.1111/j.1445-5994.2009.01960.x. [DOI] [PubMed] [Google Scholar]
- 17.Griffiths S, Taylor C. Yohannes AM. Conversion rates and perceived barriers to referral: views of extended scope physiotherapists in the primary care setting. Musculoskeletal Care. 2012;10(4):221–231. doi: 10.1002/msc.1023. [DOI] [PubMed] [Google Scholar]
- 18.Heyes-Moore GH. Triage of back pain by physiotherapists in orthopaedic clinics [4] Journal of the Royal Society of Medicine. 1998;91(10):560. doi: 10.1177/014107689809101031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kennedy DM, Robarts S. Woodhouse L. Patients are satisfied with advanced practice physiotherapists in a role traditionally performed by orthopaedic surgeons. Physiotherapy Canada. 2010;62(4):298–305. doi: 10.3138/physio.62.4.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parfitt N, Smeatham A, Timperley J. Hubble M. Direct listing for total hip replacement (THR) by primary care physiotherapists. Clinical Governance. 17(3):210–216. [Google Scholar]
- 21.Poder TG, Bellemare C, Bédard SK, He J. Lemieux R. New design of care: assessment of an interdisciplinary orthopaedic clinic with a pivot nurse in the province of Quebec. Orthopaedic Nursing. 2012;29(6):381–389. doi: 10.1097/NOR.0b013e3181f83783. 2010. [DOI] [PubMed] [Google Scholar]
- 22.Rogers BA, Kabir C. Bradley N. An audit of orthopaedic referrals via multi-professional triage teams. Annals of the Royal College of Surgeons of England. 2008;90(8):671–674. doi: 10.1308/003588408X318174. doi: 10.1308/003588408X318174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vizzini MR. O'Connor MI. Increasing surgeon productivity: the effect of the addition of musculoskeletal physicians to an orthopedic surgery department. The Journal of Medical Practice Management: MPM. 2011;27(1):29–35. [PubMed] [Google Scholar]
- 24.Aiken AB. 2007. The design, implementation, and evaluation of a model of collaborative care to improve treatment options for people with musculoskeletal impairments in Ontario. PhD thesis, Queen's University, Canada.
- 25.Aiken AB, Harrison MM. Hope J. Role of the advanced practice physiotherapist in decreasing surgical wait times. Healthcare Quarterly. 12(3):80–83. doi: 10.12927/hcq.2013.20881. [DOI] [PubMed] [Google Scholar]
- 26.Bath B, Grona SL. Janzen BA. Spinal triage programme delivered by physiotherapists in collaboration with orthopaedic surgeons. Physiotherapy Canada. 2009;64(4):356–366. doi: 10.3138/ptc.2011-29. 2012 doi: 10.3138/ptc.2011-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bath B. Janzen B. Patient and referring health care provider satisfaction with a physiotherapy spinal triage assessment service. Journal of Multidisciplinary Healthcare. 5:1–15. doi: 10.2147/JMDH.S26375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Busse JW, Riva JJ, Nash JV, et al. Surgeon attitudes toward nonphysician screening of low back or low back-related leg pain patients referred for surgical assessment: a survey of Canadian spine surgeons. Spine (Phila Pa 1976) 2012;38(4):402–408. doi: 10.1097/BRS.0b013e318286c96b. 2013. doi: 10.1097/BRS.0b013e318286c96b. [DOI] [PubMed] [Google Scholar]
- 29.Curley AE, Cassells M, Cooke G. Dowling F. Physiotherapy-led low back pain triage: results of the first two years. Physiotherapy Ireland. 25(2):3–9. [Google Scholar]
- 30.Daker-White G, Carr AJ, Harvey I, Woolhead G, Bannister G, Nelson I. Kammerling M. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. Journal of Epidemiology and Community Health. 53(10):643–650. doi: 10.1136/jech.53.10.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desmeules F, Toliopoulos P, Roy JS, Woodhouse LJ, Lacelle M, Leroux M, Girard S, Feldman DE. Fernandes JC. Validation of an advanced practice physiotherapy model of care in an orthopaedic outpatient clinic. BMC Musculosskeletal Disorder. 1999;14:162. doi: 10.1186/1471-2474-14-162. 2013 doi: http://dx.doi.org/10.1186/1471-2474-14-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Durrell S. Expanding the scope of physiotherapy: clinical physiotherapy specialists in consultants’ clinics. Manual Therapy. 1996;1(4):210–213. doi: 10.1054/math.1996.0271. [DOI] [PubMed] [Google Scholar]
- 33.Hattam P. Smeatham A. Evaluation of an orthopaedic screening service in primary care. Clinical Performance and Quality Health Care. 1999;7(3):121–124. doi: 10.1108/14664109910306749. [PubMed] [Google Scholar]
- 34.Heywood JW. Specialist physiotherapists in orthopaedic triage – the results of a military spinal triage clinic. Journal of the Royal Army Medical Corps. 151(3):152–156. doi: 10.1136/jramc-151-03-04. [DOI] [PubMed] [Google Scholar]
- 35.Homeming LJ, Kuipers P. Nihal A. Orthopaedic podiatry triage: process outcomes of a skill mix initiative. Australian Health Review. 2005;36(4):11–460. doi: 10.1071/AH11102. doi: 10.1071/AH11102. [DOI] [PubMed] [Google Scholar]
- 36.Hourigan PG. Weatherley CR. Initial assessment and follow-up by a physiotherapist of patients with back pain referred to a spinal clinic. Journal of the Royal Society of Medicine. 1994;87:213–214. doi: 10.1177/014107689408700412. [PMC free article] [PubMed] [Google Scholar]
- 37.Klett MJ, Frankovich R, Dervin GF. Stacey D. Standardize screening using WOMAC to access for eligibility for TKR pg1-2. Clinical Journal of Sport Medicine. 2012;22(3):274–277. doi: 10.1097/JSM.0b013e318248ed24. doi: http://dx.doi.org/10.1097/JSM.0b013e318248ed24. [DOI] [PubMed] [Google Scholar]
- 38.Napier C, McCormack RG, Hunt MA. Brooks-Hill A. A physiotherapy triage service for orthopaedic surgery: an effective strategy for reducing wait times. Physiotherapy Canada. Physiotherapie Canada. 2013;65(4):358–363. doi: 10.3138/ptc.2012-53. doi: 10.3138/ptc.2012-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O'Brien L, Hardman A. Goldby S. The impact of a hand therapy screening and management clinic for patients referred for surgical opinion in an Australian public hospital. Journal of Hand Therapy. 26(4):318–322. doi: 10.1016/j.jht.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 40.Rabey M, Morgans S. Barrett C. Orthopaedic physiotherapy practitioners: Surgical and radiological referral rates. Clinical Governance. 14(1):15–19. [Google Scholar]
- 41.Razmjou H, Robarts S, Kennedy D, McKnight C, MacLeod AM. Holtby R. Evaluation of an advanced-practice physical therapist in a specialty shoulder clinic: diagnostic agreement and effect on wait times. Physiotherapy Canada. 2013;65(1):46–55. doi: 10.3138/ptc.2011-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reeve S. May S. Exploration of patients' perspectives of quality within an extended scope physiotherapists' spinal screening service. Physiotherapy Theory and Practice. 2009;25(8):533–543. doi: 10.3109/09593980802664869. 2011. [DOI] [PubMed] [Google Scholar]
- 43.Rymaszewski LA, Sharma S, McGill PE, Murdoch A, Freeman S. Loh T. A team approach to musculo-skeletal disorders. Annals of the Royal College of Surgeons of England. 2005;87(3):174–180. doi: 10.1308/1478708051793. doi: 10.1308/1478708051793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stanhope J, Grimmer-Somers K, Milanese S, Kumar S. Morris J. Extended scope physiotherapy roles for orthopaedic outpatients: an update systematic review of the literature. Journal of Multidisciplinary Healthcare. 2012;5:37–45. doi: 10.2147/JMDH.S28891. doi: http://dx.doi.org/10.1111/j.1445-5994.2012.02760.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weatherley CR. Hourigan PG. Triage of back pain by physiotherapists in orthopaedic clinics. Journal of the Royal Society of Medicine. 91(7):377–379. doi: 10.1177/014107689809100709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weston-Simons JS, McClatchie W. Ricketts D. The role of the ESP in orthopaedics. International Musculoskeletal Medicine. 1998;34(3):87–91. [Google Scholar]
- 47.Wright K. Triaging of musculoskeletal patients: is this resource efficient? Physiotherapy. 88(3):189–189. [Google Scholar]
- 48.Pearse EO, Maclean A. Ricketts DM. The extended scope physiotherapist in orthopaedic out-patients – an audit. Annals of the Royal College of Surgeons of England. 88(7):653–655. doi: 10.1308/003588406X149183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schoch PA. Adair L. Successfully reforming orthopaedic outpatients. Australian Health Review. 2002;36(2):233–237. doi: 10.1071/AH11040. doi: 10.1071/AH11040. [DOI] [PubMed] [Google Scholar]
- 50.Sephton R, Hough E, Roberts SA. Oldham J. Evaluation of a primary care musculoskeletal clinical assessment service: a preliminary study. Physiotherapy. 2010;96(4):296–302. doi: 10.1016/j.physio.2010.03.003. doi: 10.1016/j.physio.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 51.Speed CA. Crisp AJ. Referrals to hospital-based rheumatology and orthopaedic services: seeking direction. Rheumatology (Oxford, England) 2005;44(4):469–471. doi: 10.1093/rheumatology/keh504. doi: 10.1093/rheumatology/keh504. [DOI] [PubMed] [Google Scholar]
- 52.Hourigan PG. Weatherley CR. The physiotherapist as an orthopaedic assistant in a back pain clinic. Physiotherapy. 1995;81(9):546–548. [Google Scholar]
- 53.Aiken AB. McColl MA. Diagnostic and treatment concordance between a physiotherapist and an orthopedic surgeon – a pilot study. Journal of Interprofessional Care. 2008;22(3):253–261. doi: 10.1080/13561820801984134. doi: 10.1080/13561820801984134. [DOI] [PubMed] [Google Scholar]
- 54.Aiken A. Improved use of allied health professionals in the health care system: the case of the advanced practice physiotherapist in orthopedic care. World Hospitals and Health Services: The Official Journal of the International Hospital Federation. 48(1):28–30. [PubMed] [Google Scholar]
- 55.Bernstein I. Integrated musculoskeletal service design by GP consortia. London Journal of Primary Care. 1:16–26. doi: 10.1080/17571472.2011.11493323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hattam P. The effectiveness of orthopaedic triage by extended scope physiotherapists. Clinical Governance: An International Journal. 2012;9(4):244–252. [Google Scholar]


