Abstract
Epitheloid hemangioendothelioma (EHE) is an uncommon angiocentric neoplasm of intermediate malignant potential. This tumor is frequently seen in the lungs and liver, but its presentation in the oral cavity is rare. In the oral cavity, gingival region is the common sites of occurrence. We report a rare case of epitheloid hemangioendothelioma in a 48-year-old male, presenting as a growth in the upper anterior gingiva of five months duration along with a review of its clinicopathological and immunohistochemical characteristics.
Keywords: Epithelioid hemangioendothelioma, Neoplasms, Vascular neoplasm
Introduction
The term hemangioendothelioma was introduced by Borrmann who first proposed the concept of vascular neoplasms with intermediate or low malignant potential. Three histological types of hemangioendothelioma are; Kaposiform, Hobnail (or Dabska-retiform), and Epithelioid.1 Epithelioid hemangioendothelioma (EHE) is a very rare vascular neoplasm. It is described as an angiocentric neoplasm characterized by neoplastic proliferation of epithelioid endothelial cells, showing eosinophilic vacuolated cytoplasm, and occasionally, fusiform cells. The cell proliferation is usually arranged as short anastamosing cords, solid lobules or lining primitive appearing vascular channels, with erythrocytes occasionally seen in the lumina. Frequently, the tumor cells are arranged within a fibromyxoid stroma.2
The common site of occurrence of EHE is the lung, liver, soft tissue, and bone.3 Occurrence of epitheloid hemangioendothelioma in oral cavity is rare.2 In oral cavity, it is commonly seen in palate and gingival.4 To the best of our knowledge, the review of the English literature revealed a total of 30 intraoral epitheloid hemangioendothelioma reported cases.1,4,5 Some of these intraoral tumors have shown local recurrences.1 Since only few cases have been reported, the exact clinical behavior of the intraoral EHE is still uncertain.4 In this article, we report a case of intraoral epithelioid hemangioendothelioma masquerading clinically as pyogenic granuloma.
Case Report
A 48-year-old man presented with a chief complaint of localized gum enlargement since 5 months. The patient had no relevant medical history. On examination, a small sessile grayish pink growth of size 7×7 mm on the buccal and palatal aspect of interdental gingiva between 21 and 22 regions was found. The swelling was firm and nontender on palpation. The underlying bone showed no evidence of erosion on radiographic examination. Similar swellings were not present in other parts of the oral cavity or skin and lymph nodes were not palpable. The lesion was provisionally diagnosed as pyogenic granuloma (figure 1). The patient underwent routine blood examination prior to biopsy procedure and the results were within normal limits (Bleeding Time: 2 min, Clotting Time: 10 min, Random Blood Sugar: 70 gm/dl, Hemoglobin Count: 16.5 gm/dl, Total Leucocyte Count: 5700 cells/mm3. Differential Count; Neutrophils: 64%, Lymphocytes: 36%, Erythrocyte Sedimentation Rate: 4 mm/hour). An excision biopsy was performed and on microscopic examination, a fibrovascular connective tissue with a circumscribed tumor mass of epitheloid and spindle shaped endothelial cells. The tumor cells comprised predominantly of epitheloid cells. These cells exhibited intracellular vacuoles, which in some foci contained RBCs (figure 2). The immunohistochemical study on the tumor showed that the cells were positive for vimentin (figure 3), and negative for smooth muscle actin (SMA). The neoplastic cells showed strong staining with CD34 especially by the cells forming intracytoplasmic vacuoles (figure 4 and 5).
Figure 1.

Palatal aspect of the swelling between 21 and 22.
Figure 2.
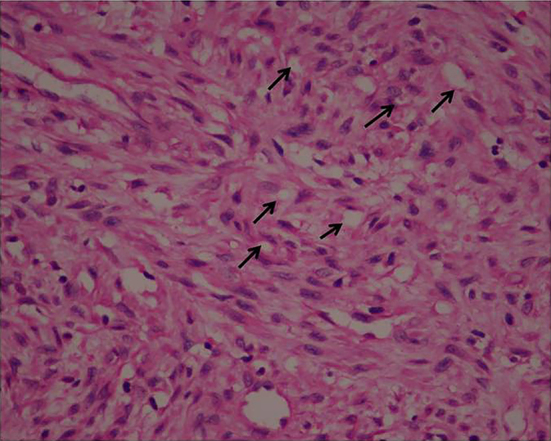
Tumor showing spindle and epitheloid cells with intracytoplamic vacuoles indicated by black arrows (×40).
Figure 3.
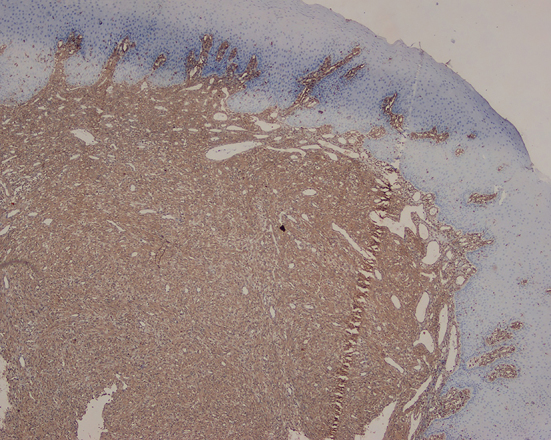
Tumor tissue showing vimentin immuno positivity (×4).
Figure 4.
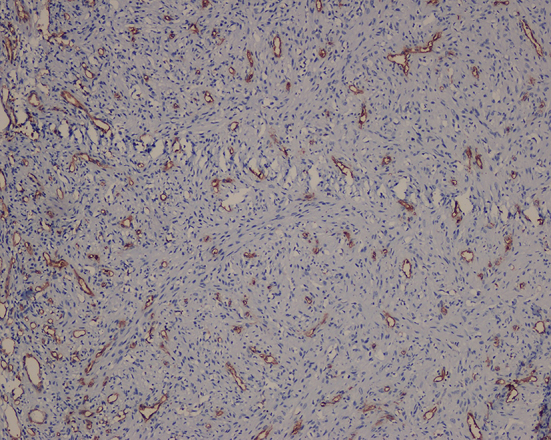
Tumor cells especially the ones forming small vessels and intracytoplamic vacuoles showed strong staining with CD34 (×10).
Figure 5.
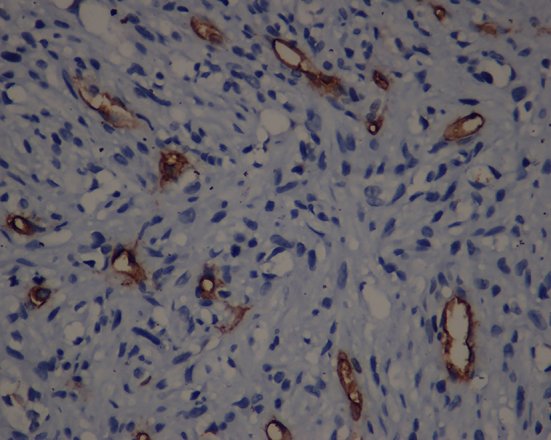
Tumor cells especially the ones forming small vessels and intracytoplamic vacuoles showed strong staining with CD34 (×40).
Based on histopathological and immunohistochemical findings, the lesion was diagnosed as epithelioid hemangioendothelioma. Computerized tomography of the chest and ultrasound of the abdomen was done to rule out any hidden primaries and no abnormalities were detected. The patient is under a regular follow-up for 10 months and there is no evidence of recurrence. We had obtained consent from the patient for publishing this report.
Discussion
The epithelioid hemangioendothelioma (EHE) is a rare angiocentric vascular tumor of intermediate malignancy that usually arises in the superficial or deep soft tissues of the extremities. In the head and neck area, EHE is commonly seen in the submandibular region.5 Ellis and Kratochvil in 1986 first reported EHE in the oral cavity.6 Most common oral site was in the gingiva.7 It can occur at any age and they are predominantly seen in fourth and fifth decades of life. There is no sex predilection or associated predisposing factors for EHE.8
Most cases were clinically diagnosed as benign entities like pyogenic granuloma, fibroma, peripheral giant cell granuloma, peripheral ossifying fibroma, inflammatory fibrous hyperplasia and necrotizing ulcerative gingivitis.7 The case reported here was also diagnosed clinically as pyogenic granuloma.
The microscopic differential diagnosis includes carcinoma, angiosarcoma and Hemangio- pericytoma.9 Vimentin will be negative for carcinomas.1 In our case the tumor cells were vimentin positive and thus the possibility of being a carcinoma as the diagnosis was ruled out. Epitheloid angiosarcomas present with marked cytologic atypia and pleomorphism and high mitotic rate.8 In our case, the tumor was well circumscribed, lacked mitotic figures and cytological atypia, excluding the possibility of angiosarcoma. Tumor cells in hemangiopericytoma are positive for SMA and in our case, the tumor cells were SMA negative ruling out hemangiopericytoma from the histopathological differential diagnosis.9 The tumor cells were positive for vascular marker CD34 confirming that they are endothelial cells.3 Majority of EHEs are clinically diagnosed as benign lesions. It’s important to make a proper histopathological examination and come to a correct diagnosis, since it is a neoplasm with malignant biological behavior, intermediate between the hemangioma and conventional angiosarcoma.3,10
It is reported that when EHE’s present with increased mitotic figures, cellular atypia, spindle tumor cells, metaplastic bone formation and areas of necrosis; they can behave in a more aggressive manner.1 The case reported here showed no relevant cellular atypia or mitotic activity and was predominantly composed of epitheloid cells suggestive of a less aggressive variant of the tumor.
Epitheloid hemangioendothelioma exhibits different biological behavior depending upon the anatomical position. There are no consistent clinical or histological criteria for predicting the behavior and prognosis of intraoral EHE.4 According to Chi et al., the average age of occurrence of intraoral EHE is 28 years, but in our case the patient was in his 5th decade.9 When the cases of intraoral EHE reported up to 2012 were analyzed, the common site of occurrence was gingiva (13/30 cases) ( table 1).1,2,4,5 In our case, also the site of occurrence of the tumor was the same. Manuel-Antonio Gordón-Núñez et al. analyzed 27 reported cases of intraoral EHE of which 23 cases (85.2%) had clinical follow-up information. Only eight lesions (29.6%) recurred locally and there were no reported local or distant metastasis. These findings suggest that intraoral EHE’s are less aggressive in nature.1
Table 1.
Clinical data for cases of intraoral oral EHE reported in English literature
| Serial No | Author | Age | Sex | Localization | Clinical and radiographic history | Follow-up |
|---|---|---|---|---|---|---|
| 1 | Wesley et al.11 | 18 | F | Mandibular gingiva | Reddish erosive lesion, (34 to 36), bone resorption | 2 years SFL |
| 2 | Ellis et al.6 | 13 | F | Maxillary gingiva | Swelling, pink, tooth mobility, 4 years | 6 years SFL |
| 3 | Ellis et al.6 | 4 | F | Mandibular gingiva | Tooth mobility, bone resorption | NI |
| 4 | Moran et al.12 | 25 | F | Palate | Swelling, 1.0 cm, 1 year | 21 months SFL |
| 5 | de Araujo et al.13 | 4 | M | Mandibular gingiva | Swelling, ulceration, tooth mobility, 9 months | NI |
| 6 | Marrogi et al.10 | 45 | M | Maxillary gingiva | Erythematous lesion, 1.5 cm | 3,6 months Rec |
| 7 | Marrogi et al.10 | 36 | F | Tongue | Painful nodules, 0.2 cm, 2 months | 17 months SFL |
| 8 | Flaitz et al.14 | 7 | F | Mandibular gingiva | Reddish swelling, 1.5 cm, tooth mobility, bone destruction | 52 months SFL |
| 9 | Hamakawa et al.15 | 76 | F | Mandibular anterior region | Submucous swelling, soft, 4.5 cm, bone destruction | 6 years SFL |
| 10 | Orsini et al.7 | 18 | F | Buccal mucosa | Asymptomatic swelling, 1.5 cm, 7 months | 9 months Rec |
| 11 | Ramer et al.16 | 32 | M | Maxilla | Swelling, 3.5 cm | 6 months Rec |
| 12 | Molina Palma et al.17 | 65 | F | Tongue | Swelling, 0.5 cm, 2 months | 21 months SFL |
| 13 | Machalka et al.18 | 65 | M | Jaw | Swelling at the anterior region of jaw, tooth mobility | 4.8 years Rec |
| 14 | Anderson et al.19 | 18 | F | Lower lip | Asymptomatic swelling, 6 months | 4 months Rec |
| 15 | Chi et al9 | 28 | F | Maxillary gingiva | Purple swelling, 0.6 cm | 8 months SFL |
| 16 | Chi et al.9 | 23 | F | Jaw | 2.0 cm, bone destruction | NI |
| 17 | Sun et al.20 | 12 | M | Maxillary gingiva | Ulcerated swelling, 3.0 cm, 3 months, bone destruction, tooth mobility | 6 months SFL |
| 18 | Sun et al.20 | 53 | M | Buccal mucosa | Swelling, 1.5, 6 months | 9 months Rec |
| 19 | Sun et al.20 | 17 | M | Tongue | Soft swelling, 0.5 cm, 2 months | 18 months SFL |
| 20 | Sun et al.20 | 52 | F | Upper lip | Purple swelling, 2.0 cm, 1 year | 3 years SFL |
| 21 | Sun et al.20 | 21 | M | Tongue | Reddish swelling, 0.5 cm, 2 months | 2 years SFL |
| 22 | Sun et al.20 | 34 | M | Tongue | Swelling, 1.0 cm, 4 months | 6 years SFL |
| 23 | Sun et al.20 | 11 | M | Mandibular gingiva | Painful swelling, 2.0 cm, 1 month, bone destruction, tooth mobility | 8 years SFL |
| 24 | Sun et al.20 | 46 | M | Tongue | Reddish swelling, 1.2 cm | 4 months Rec |
| 25 | Sun et al.20 | 6 | M | Floor of mouth and tongue | Reddish swelling, 7.0 cm, 6 months | 2 years SL |
| 26 | Mohtasham et al.5 | 9 | M | Maxillary gingiva | Ulcerated reddish swelling, asymptomatic, 1.0 cm, 6 months | 1 year, Rec |
| 27 | Gordón-Núñez et al.1 | 17 | F | Mandibular gingiva | Swelling, pink, 2,0 cm, 1 year | 9 months, SFL |
| 28 | Nooshin Mohtasham et al.5 | 9 | M | Maxillary gingiva | Pedunculated, reddish swelling; 1 cm; 6 months. | NI |
| 29 | Bhari Manjunatha et al.4 | 20 | M | Floor of the mouth | Pedunculated, reddish swelling; 3×4 cm; 6 months | NI |
| 30 | Manuel-Antonio et al.1 | 17 | F | Mandibular gingiva | Pedunculated, exophytic pink swelling; 1year | 14 months SFL |
M: Male; F: Female; NI: No information; SFL: Survival free of lesion; SL: Survival with lesion; Rec: Recurrence
The treatment of choice for epitheloid hemangioendothelioma is complete surgical excision along with wide margins. The follow up data of Intraoral EHE reported until 2012 shows that 13% cases had local recurrences before 10 months (table1) but our patient had a disease free period of 10 months. Machalka et al. in 2003 reported intraoral EHE with recurrence after a disease free period of 8 years, so a long term follow up is recommended.1,4,5,9
Conclusion
Intraoral EHE is an intermediate malignancy, which has a tendency for local recurrence and distant metastasis. It is often diagnosed clinically as other benign lesions. Hence, clinicians should be aware of pathological features and behavior of this lesion in order to ensure prompt diagnosis and appropriate management for the patient. Since very few reported cases of intraoral epithelioid hemangioendothelioma are available, the exact biological behavior of the lesion is yet to be ascertained.
Conflict of Interest: None declared.
References
- 1.Gordón-Núñez MA, Silva eM, Lopes MF, de Oliveira-Neto SF, Maia AP, Galvão HC. Intraoral epithelioid hemangioendothelioma: a case report and review of the literature. Med Oral Patol Oral Cir Bucal. 2010;15:e340–6. PubMed PMID: 20038915. [PubMed] [Google Scholar]
- 2.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970–81. doi: 10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z. doi:10:1002/1097-0142(19820901)50:5%3C970::AID-CNCR2820500527%3E3.0.CO;2-Z. PubMed PMID: 7093931. [DOI] [PubMed] [Google Scholar]
- 3.Bollinger BK, Laskin WB, Knight CB. Epithelioid hemangioendothelioma with multiple site involvement. Literature review and observations. Cancer. 1994;73:610–5. doi: 10.1002/1097-0142(19940201)73:3<610::aid-cncr2820730318>3.0.co;2-3. doi:10.1002/1097-0142(19940201)73:3%3C610::AID-CNCR2820730318%3E3.0.CO;2-3. PubMed PMID: 7507796. [DOI] [PubMed] [Google Scholar]
- 4.Manjunatha BS, Kumar GS, Vandana R. Intraoral epithelioid hemangioendothelioma: an intermediate vascular tumor- a case report. Dent Res J. 2009;6:99–102. PubMed PMID: 21528039; PubMed Central PMCID: PMC3075463. [PMC free article] [PubMed] [Google Scholar]
- 5.Mohtasham N, Kharrazi AA, Jamshidi S, Jafarzadeh H. Epithelioid hemangioendothelioma of the oral cavity: a case report. J Oral Sci. 2008;50:219–23. doi: 10.2334/josnusd.50.219. doi: 10.2334/josnusd.50.219. PubMed PMID: 18587215. [DOI] [PubMed] [Google Scholar]
- 6.Ellis GL, Kratochvil FJ 3rd. Epithelioid hemangioendothelioma of the head and neck: a clinicopathologic report of twelve cases. Oral Surg Oral Med Oral Pathol. 1986;61:61–8. doi: 10.1016/0030-4220(86)90204-5. doi: 10.1016/0030-4220(86)90204-5. PubMed PMID: 3456142. [DOI] [PubMed] [Google Scholar]
- 7.Orsini G, Fioroni M, Rubini C, Piattelli A. Epithelioid hemangioendothelioma of the oral cavity: report of case. J Oral Maxillofac Surg. 2001;59:334–7. doi: 10.1053/joms.2001.21007. doi: 10.1053/joms.2001.21007. PubMed PMID: 11243620. [DOI] [PubMed] [Google Scholar]
- 8.Naqvi J, Ordonez NG, Luna MA, Williams MD, Weber RS, El-Naggar AK. Epithelioid hemangioendothelioma of the head and neck: role of podoplanin in the differential diagnosis. Head Neck Pathol. 2008;2:25–30. doi: 10.1007/s12105-007-0035-0. doi: 10.1007/s12105-007-0035-0. PubMed PMID: 20614338; PubMed Central PMCID: PMC2807604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chi AC, Weathers DR, Folpe AL, Dunlap DT, Rasenberger K, Neville BW. Epithelioid hemangioendothelioma of the oral cavity: report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:717–24. doi: 10.1016/j.tripleo.2005.05.066. doi: 10.1016/j.tripleo.2005.05.066. PubMed PMID: 16301153. [DOI] [PubMed] [Google Scholar]
- 10.Marrogi AJ, Boyd D, el-Mofty S, Waldron C. Epithelioid hemangioendothelioma of the oral cavity: report of two cases and review of literature. J Oral Maxillofac Surg. 1991;49:633–8. doi: 10.1016/0278-2391(91)90346-n. doi: 10.1016/0278-2391(91)90346-N. PubMed PMID: 2037920. [DOI] [PubMed] [Google Scholar]
- 11.Wesley RK, Mintz SM, Wertheimer FW. Primary malignant hemangioendothelioma of the gingiva. Report of a case and review of the literature. Oral Surg Oral Med Oral Pathol. 1975;39:103–12. doi: 10.1016/0030-4220(75)90400-4. PubMed PMID: 1053668. [DOI] [PubMed] [Google Scholar]
- 12.Moran WJ, Dobleman TJ, Bostwick DG. Epithelioid hemangioendothelioma (histiocytoid hemangioma) of the palate. Laryngoscope. 1987;97:1299–302. doi: 10.1288/00005537-198711000-00009. doi: 10.1288/00005537-198711000-00009. PubMed PMID: 3669841. [DOI] [PubMed] [Google Scholar]
- 13.de Araújo VC, Marcucci G, Sesso A, de Araújo NS. Epithelioid hemangioendothelioma of the gingiva: case report and ultrastructural study. Oral Surg Oral Med Oral Pathol. 1987;63:472–7. doi: 10.1016/0030-4220(87)90261-1. PubMed PMID: 3472148. [DOI] [PubMed] [Google Scholar]
- 14.Flaitz CM, McDaniel RK, Mackay B, Kennady MC, Luna MA, Hicks MJ. Primary intraoral epithelioid hemangioendothelioma presenting in childhood: review of the literature and case report. Ultrastruct Pathol. 1995;19:275–9. doi: 10.3109/01913129509064231. doi: 10.3109/01913129509064231. PubMed PMID: 7571085. [DOI] [PubMed] [Google Scholar]
- 15.Hamakawa H, Omori T, Sumida T, Tanioka H. Intraosseous epithelioid hemangioendothelioma of the mandible: a case report with an immunohistochemical study. J Oral Pathol Med. 1999;28:233–7. doi: 10.1111/j.1600-0714.1999.tb02030.x. doi: 10.1111/j.1600-0714.1999.tb02030.x. PubMed PMID: 10226947. [DOI] [PubMed] [Google Scholar]
- 16.Ramer MA, Lumerman H, Kopp W, Fisher KS, Cohen SA. Epithelioid hemangioendothelioma of the maxilla: case report and review of literature. Periodontal Clin Investig. 2001;23:31–5. PubMed PMID: 11575111. [PubMed] [Google Scholar]
- 17.Molina Palma MI, Cervantes Góngora JA, García de la Torre E, Conde Pérez de la Blanca I, Ramírez Tortosa CL. Primary intraoral epithelioid hemangioendothelioma. Case report and review of the literature. Acta Otorrinolaringol Esp. 2002;53:215–8. doi: 10.1016/s0001-6519(02)78303-9. PubMed PMID: 12073682. [DOI] [PubMed] [Google Scholar]
- 18.Machálka M, Procházková L, Husek K. Epithelioid hemangioendothelioma of the mandible. Mund Kiefer Gesichtschir. 2003;7:180–3. doi: 10.1007/s10006-003-0470-3. doi: 10.1007/s10006-003-0470-3. PubMed PMID: 12764686. [DOI] [PubMed] [Google Scholar]
- 19.Anderson PJ, Ross G, Felix D, Camilleri IG. The use of sentinel node biopsy in the management of epitheloid haemangioendothelioma of the lip. Oral Oncol. 2003;39:531–3. doi: 10.1016/s1368-8375(03)00009-5. doi: 10.1016/S1368-8375(03)00009-5. PubMed PMID: 12747979. [DOI] [PubMed] [Google Scholar]
- 20.Sun ZJ, Zhang L, Zhang WF, Chen XM, Lai FM, Zhao YF. Epithelioid hemangioendothelioma of the oral cavity. Oral Dis. 2007;13:244–50. doi: 10.1111/j.1601-0825.2006.01281.x. doi: 10.1111/j.1601-0825.2006.01281.x. PubMed PMID: 17305630. [DOI] [PubMed] [Google Scholar]


