Abstract
Background
Pseudomyxoma peritonei is a rare condition consisting of mucinous ascites, most commonly arising from mucinous tumors of the appendix and occasionally from the ovary. Very rarely mucinous implants arise in the retroperitoneum without any intra-peritoneal involvement. This has been termed as pseudomyxoma extraperitonei.
Case presentation
We report a case of a 57 year old man who developed pseudomyxoma extraperitonei, 35 years after undergoing an appendicectomy for a perforated appendix.
Conclusions
Pseudomyxoma extraperitonei has been previously reported, however we report the longest incubation period of 35 years for this condition.
Keywords: Appendix, pseudomyxoma extraperitonei, pseudomyxoma peritonei, mucinous adenocarcinoma; ovary.
Background
Pseudomyxoma peritonei is a rare condition consisting of mucinous ascites, most commonly arising from mucinous tumors of the appendix and occasionally from the ovaries. Literally translated it means a false mucinous tumor of the peritoneum. Very rarely mucinous implants arise in the retroperitoneum without any intra-peritoneal involvement. This has been termed as pseudomyxoma extraperitonei. Only 9 cases of pseudomyxoma extraperitonei have been reported in the English literature. [1-9]
We report a case of pseudomyxoma extraperitonei associated with mucinous adenocarcinoma in a patient who had an appendicectomy performed 35 years previously. This is the longest interval reported between appendicectomy and diagnosis of pseudomyxoma extraperitonei.
Case presentation
A 57 years old Caucasian male was referred to the surgical clinic with vague lower abdominal pain. He had no systemic or bowel symptoms. Abdominal examination revealed a large, fixed mass in the right iliac fossa. The only significant past history was an appendicectomy 35 years ago, in March 1966, when he presented with abdominal pain, fever and vomiting. On examination he was found to have a mass in the right iliac fossa. A diagnosis of an appendicular mass was made and he underwent an interval appendicectomy a few weeks later. At operation a high retro-caecal perforated appendix was seen and the operation to remove the appendix was "difficult" necessitating an extension of the 'grid-iron' incision and insertion of a drain. Postoperatively he developed cellulites and a cutaneous fistula, which subsequently closed. He had remained well and symptom free thereafter until the current presentation. In spite of an extensive search for his past records the histology of the appendix was unavailable.
At present his routine hematological and biochemical tests were within normal limits. A computed tomographic (CT) scan of the chest and abdomen showed a well-defined mass with low attenuation measuring 11 × 6 cm on the right side of the abdomen, extending from the level of the renal hilum to the anterior superior iliac spine. It was closely related to, and distorting, the right psoas muscle. The mass had displaced the ascending colon anteriorly (Figure 1). A CT guided aspiration of the mass yielded mucin and degenerate cellular debris.
Figure 1.
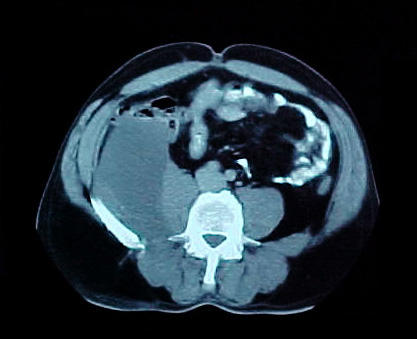
Computed tomographic scan of the abdomen showing the mass to be closely related to the right psoas muscle and displacing the colon anteriorly.
At exploratory laparotomy, an encapsulated large mass extending from the right 12th rib to the right lateral pelvic wall was excised intact. It was free from all surrounding structures, including pancreas, kidneys and bowel. The mass was attached to a 2 cm area on the anterior aspect of the quadratus lumborum muscle.
On gross examination the specimen consisted of a partly solid and partly cystic mass measuring 17 × 11 × 6 cm. The cut surface showed myxoid change with areas of necrosis, hemorrhage and calcification. On microscopic examination there was extensive infiltration of the skeletal muscle and fatty tissue by a mucinous adenocarcinoma. Pools of mucin were seen lined by malignant epithelium (Figure 2). There were areas of inflammation; fibrosis, calcification and cholesterol cleft formation.
Figure 2.
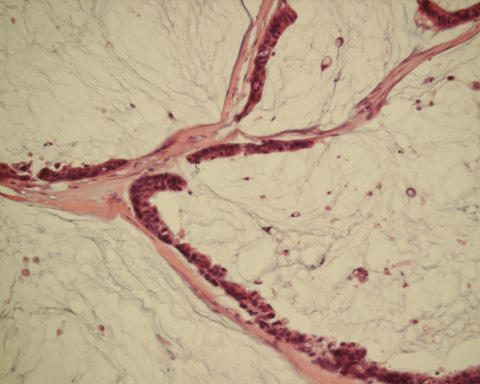
Photomicrograph showing pools of mucin lined by malignant glandular epithelium. (Hematoxylin & Eosin, ×10).
The patient was treated with adjuvant radiotherapy (40 Gy in 20 fractions) and chemotherapy (weekly injections of 5-fluorouracil and folinic acid given for 30 weeks) making an uneventful recovery. At follow-up three years later there was no sign of recurrence.
Discussion
This unusual case of pseudomyxoma extraperitonei is the tenth reported in the English literature. In this case, a large mucinous adenocarcinoma was attached to a tiny area of the quadratus lumborum muscle, without any involvement of neighboring structures.
Werth [10] in 1884 first described pseudomyxoma peritonei as characterized by the presence of mucinous and gelatinous material in the peritoneal cavity. Earlier hypothesis of the etiology included an inflammatory response with peritoneal metaplasia [11] and active secretions by peritoneal metastases [2,12,13]. Some authors use the term pseudomyxoma peritonei only when mucinous ascites is caused by benign peritoneal deposits and metastatic mucinous adenocarcinoma, when malignant cells are identified in the mucinous material [7,10]. Others however, consider all pseudomyxoma peritonei to be low-grade mucinous adenocarcinoma [1,10]. More recently, Ronnett et al, [14] have suggested a classification based on tumor pathology where they place all pseudomyxoma peritonei in three groups in order of decreasing prognosis: disseminated peritoneal adenomucinosis (DPAM), peritoneal mucinous carcinoma with intermediate or discordant features (PMCA-I/D) and peritoneal mucinous carcinoma (PMCA) [15].
In 1948 Bonann [3] reported pseudomyxoma involving only the retroperitoneum. This was later termed as pseudomyxoma extraperitonei by Moran [4] in 1988. In eight of the nine case reports of pseudomyxoma extraperitonei the cause was a rupture of an appendiceal mucinous tumor into the retroperitoneum (Table 1). In one, information regarding status of the appendix was not available as the appendicectomy was performed several years previously. An inflammatory response to the mucin leads to fibrosis and encapsulation limiting it to the retroperitoneum.
Table 1.
Brief details of previous cases of pseudomyxoma extraperitonei reported in literature
| Author | Age / Sex | Clinical Presentation | Treatment | Outcome | Perforated Appendix? | Histology |
| Brady [1] | 67 M | abdominal pain and mass | - debulking of tumor - further debulking 2 years later with chemotherapy - additional debulking 3 years later |
recurrence after 3 years | yes | mucinous mucocele |
| Edrees [2] | 53 F | abdominal mass | right hemicolectomy & debulking of tumor with chemotherapy | alive and well at 1 year | yes | mucinous adenocarcinoma |
| Bonann [3] | 37 M | tender abdominal mass | evacuation of cyst in 2 stage procedure | not available | yes | mucocoele of appendix |
| Moran [4] | 57 M | tender abdominal mass | - extraperitoneal drainage of cyst - drained again 3 weeks later with appendicectomy - further drainage 5 years later with radiotherapy & chemotherapy |
alive and well 10 years later | yes | mucocoele of appendix |
| Mor [5] | 65 M | abdominal mass | excision of mass with intraperitoneal spillage of mucus | not available | yes | cyst-adenocarcinoma |
| Early [6] | 57 M | abdominal mass | debulking of tumor | alive and well 2 years later | yes | mucocoele of appendix |
| Koizumi [7] | 46 M | abdominal mass | - right hemicolectomy - chemotherapy |
recurrence of tumor 3 months later | yes | mucinous adenocarcinoma |
| Matsuoka [8] | 58 F | abdominal mass | resection of tumor | not available | possible | mucinous cystadenoma |
| Shelton [9] | 81 M | abdominal mass | removal of all pseudomyxoma deposits and appendicectomy | persistent discharge from wound, survival not available | yes | mucinous cystadenoma |
Several treatment modalities with radiotherapy and chemotherapy have been used in treating pseudomyxoma peritonei with varying degrees of success. Recently, Sugarbaker et al, [16] have advocated radical surgery together with perioperative intra-peritoneal and systemic chemotherapy. The reported 5-year survival rate of patients with pseudomyxoma peritonei varies from 11% to 75% (mean 50%) [17]. The role of adjuvant treatment in pseudomyxoma extraperitonei and the survival rates are not known due to the paucity of the reported cases. The prognosis however, is likely to be better than pseudomyxoma peritonei as the vital abdominal structures are not involved [4].
Mucinous implants in the peritoneal cavity are almost always of appendiceal or ovarian origin [6]. Unusual sources of mucinous adenocarcinoma causing pseudomyxoma peritonei have included colon, uterus, common bile duct, pancreas and the stomach [18]. However, a recent report by van Ruth et al, [15] suggests that the appendix is the primary source of most pseudomyxoma peritonei, which may then spread to other sites like the ovaries.
In the absence of any other precipitating cause it seems likely that pseudomyxoma extraperitonei had originated from the perforated appendix in this patient 35 years ago. It appears that a perforation of an appendix containing a mucinous tumor leads to pseudomyxoma and therefore the authors recommend, wherever possible, complete removal of the appendix at appendicectomy and thorough cleansing of the surrounding areas to prevent the occurrence this serious long-term complication.
Conclusions
It is recommended that in an encapsulated pseudomyxoma extraperitonei it is imperative that an intact and complete removal of the mass is achieved without spillage of the mucinous contents in the peritoneum to prevent intraperitoneal extension of the disease.
Competing interests
None declared.
Author's contributions
MHS collated the information, searched literature and wrote the manuscript.
NA assisted in literature search and writing of the manuscript.
ZK contributed to the pathological aspect of the manuscript.
MCP managed the patient and helped in preparing the manuscript and edited the final version.
All authors have read and approved the final version of the manuscript.
Acknowledgments
Acknowledgement
Patient consent was obtained for publication of this case report.
Contributor Information
Mamoon H Solkar, Email: mamoonsolkar@hotmail.com.
Naveed M Akhtar, Email: naveed1701@doctors.org.uk.
Zareen Khan, Email: zareen.khan@kingsch.nhs.uk.
Michael C Parker, Email: mike.parker@dag-tr.sthames.nhs.uk.
References
- Brady MB, Ewing RH, Robinson AE, Dowling EA. Flank mass and pain in a 72 year old man. Invest Radiol. 1986;21:419–423. doi: 10.1097/00004424-198605000-00012. [DOI] [PubMed] [Google Scholar]
- Edrees WK, Hannon RJ. Pseudomyxoma extraperitonei: a rare presentation mimicking an iliacus abscess. The Ulster Med J. 1999;68:38–39. [PMC free article] [PubMed] [Google Scholar]
- Bonnan LJ, Davis JG. Retroperitoneal mucocoele of the appendix. A case report with characteristic roentgen features. Radiology. 1948;51:375–382. doi: 10.1148/51.3.375. [DOI] [PubMed] [Google Scholar]
- Moran CJ, Morgan RH. Pseudomyxoma extraperitonei. J Roy Soc Med. 1988;81:668–669. doi: 10.1177/014107688808101121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor Y, Leibovitch I, Garnick A, Avigad I, Jonas P, Goldwasser B. Pseudomyxoma extraperitonei: an unusual presentation mimicking a huge hydronephrotic kidney. Clin Radiol. 1996;51:221–222. doi: 10.1016/s0009-9260(96)80327-8. [DOI] [PubMed] [Google Scholar]
- Early KS, Stephenson DV, Davis WC. Giant retroperitoneal mucocoele simulating pseudomyxoma peritonei and mucinous adenocarcinoma. Am J Surg. 1968;116:439–443. doi: 10.1016/0002-9610(68)90238-9. [DOI] [PubMed] [Google Scholar]
- Koizumi J, Noguchi H. Pseudomyxoma retroperitonei with spontaneous skin fistula. Abdom Imaging. 1999;24:193–195. doi: 10.1007/s002619900475. [DOI] [PubMed] [Google Scholar]
- Matsuoka Y, Masumoto T, Suzuki K, Terada K, Ushimi T, Yokoyama Y, Abe K, Kamata N, Yasuno M, Hishima T. Pseudomyxoma retroperitonei. Eur Radiol. 1999;9:457–459. doi: 10.1007/s003300050692. [DOI] [PubMed] [Google Scholar]
- Shelton MW, Morian JP, Radford DM. Pseudomyxoma retroperitonei associated with appendiceal cystadenoma. Am Surg. 1994;12:958–960. [PubMed] [Google Scholar]
- Werth R. Pseudomyxoma peritonei. Arch Gynaecol. 1884;24:100–118. [Google Scholar]
- Cheng KK. An experimental study of mucocoele of the appendix and pseudomyxoma peritonei. J Pathol Bacteriol. 1949;61:217–225. doi: 10.1002/path.1700610209. [DOI] [PubMed] [Google Scholar]
- Fernandez RN, Daly JM. Pseudomyxoma peritonei. Arch Surg. 1980;115:409–414. doi: 10.1001/archsurg.1980.01380040037006. [DOI] [PubMed] [Google Scholar]
- Limber GK, King RE, Silverberg SG. Pseudomyxoma peritonei: a report of 10 cases. Ann Surg. 1973;178:587–593. doi: 10.1097/00000658-197311000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronnett BM, Yan H, Kurman RJ, Shmookler BM, Wu L, Sugarbaker PH. Patients with pseudomyxoma peritonei associated with disseminated peritoneal adenomucinosis have a significantly more favorable prognosis than patients peritoneal mucinous carcinomatosis. Cancer. 2001;92:85–91. doi: 10.1002/1097-0142(20010701)92:1<85::AID-CNCR1295>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Van Ruth S, Acherman YIZ, van de Vijwer MJ, Hart AA, Verwaal VJ, Zoetmulder FA. Pseudomyxoma peritonei: a review of 62 cases. Eur J Surg Oncol. 2003;29:682–688. doi: 10.1016/S0748-7983(03)00149-5. [DOI] [PubMed] [Google Scholar]
- Sugarbaker PH, Kern K, Lack E. Malignant pseudomyxoma peritonei of colonic origin: natural history and presentation of a curative approach to treatment. Dis Colon Rectum. 1987;30:772–779. doi: 10.1007/BF02554625. [DOI] [PubMed] [Google Scholar]
- Sherer D, Abulafia O, Eliakim R. Pseudomyxoma peritonei: a review of current literature. Gynecol Obstet Invest. 2001;51:73–80. doi: 10.1159/000052897. [DOI] [PubMed] [Google Scholar]
- Higa E, Rosai J, Pizzimbono CA, Wise L. Mucosal hyperplasia, mucinous cystadenoma and mucinous cystadenocarcinoma of the appendix. a re-evaluation of appendiceal 'mucocoele'. Cancer. 1973;33:1525–1541. doi: 10.1002/1097-0142(197312)32:6<1525::aid-cncr2820320632>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]


