Abstract
Objective: Health care providers are beginning to deliver a range of Internet-based services to patients; however, it is not clear which of these e-health services patients need or desire. The authors propose that patients' acceptance of provider-delivered e-health can be modeled in advance of application development by measuring the effects of several key antecedents to e-health use and applying models of acceptance developed in the information technology (IT) field.
Design: This study tested three theoretical models of IT acceptance among patients who had recently registered for access to provider-delivered e-health.
Measurements: An online questionnaire administered items measuring perceptual constructs from the IT acceptance models (intrinsic motivation, perceived ease of use, perceived usefulness/extrinsic motivation, and behavioral intention to use e-health) and five hypothesized antecedents (satisfaction with medical care, health care knowledge, Internet dependence, information-seeking preference, and health care need). Responses were collected and stored in a central database.
Results: All tested IT acceptance models performed well in predicting patients' behavioral intention to use e-health. Antecedent factors of satisfaction with provider, information-seeking preference, and Internet dependence uniquely predicted constructs in the models.
Conclusion: Information technology acceptance models provide a means to understand which aspects of e-health are valued by patients and how this may affect future use. In addition, antecedents to the models can be used to predict e-health acceptance in advance of system development.
Health-related Internet applications delivering a range of content, connectivity, and clinical care are referred to collectively as e-health.1* E-health is promoted as a mechanism to bring growth, cost savings, and process improvement to health care.5,6 Health care providers observed initial developments in e-health mainly from the sidelines due to concerns over risk, liability, and initial expense.5 However, more and more providers are coming to accept the situation that patients want to be involved “as a participant and partner in the flow of information” relating to their own health care.7 A recent survey of 440 health care organizations5 found that more than 80% now deliver some form of e-health to their patients, and more than 50% implement advanced e-health applications, including online formularies, prescription refills, test results, and physician–patient communication. These advanced applications differentiate provider-delivered e-health from sites that supply generalized health content to the mass market, and it is likely that developing and delivering new forms of health care connectivity, clinical care, and personalized content to patients will be an effective business strategy for providers8 and a self-management tool for patients.9
In 2000, health care accounted for 14% of the U.S. gross domestic product ($1.31 trillion), and this figure is projected to increase to 16.2% ($2.6 trillion) by 2010.10 Given the massive size of the industry, decisions by health care organizations to implement e-health are likely to have serious economic consequences5 and social ramifications as patients adapt their lifestyles to interact with providers online rather than via telephone or office visits.4,8 It is clear that patients desire a range of services to be brought online by their own health care provider.11 What is less clear is whether the services offered by health care providers are services that patients desire. Discrepancies between the two positions could obstruct patients' acceptance and use of the technology.12 Indeed, the history of information technology (IT) system development is littered with projects that were rejected by intended users because developers did not attend to key factors underlying acceptance.13 For this reason, it is important that health care providers are able to effectively model patients' acceptance of e-health. Models will be useful in predicting which patients will use e-health and in understanding what factors influence their decisions. Models also can aid in designing and evaluating the ability of specific e-health applications, such as online formularies, to meet the needs of patients in general as well as the needs of specific constituencies, such as diabetic patients.
In this paper, we report a study in which we tested the effectiveness of three models—two well-known models of IT acceptance and a recently introduced approach that integrates the two—in explaining patients' behavioral intention to use provider-delivered e-health. We also tested five conceptually important characteristics of patients to assess whether these are significant antecedents to the models. In the remainder of this paper, we develop hypotheses regarding the models and antecedents, describe the research methods and results, and conclude with a discussion of our findings.
Acceptance Models and Antecedents
IT Acceptance Models
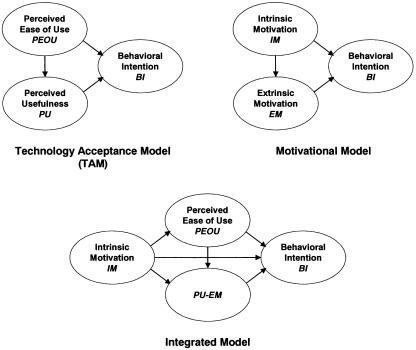
Two prominent models of IT acceptance are the technology acceptance model (TAM)14,15 and the motivational model16 (▶). TAM extends the theory of reasoned action17,18 by proposing that individuals' perceptions of a technology's usefulness (PU) and ease of use (PEOU) are key contributors to behavioral intention (BI) to use the technology. The motivational model proposes that intrinsic motivation (IM) and extrinsic motivation (EM) are key in determining BI. In technology acceptance research, BI is typically used as the dependent variable in place of actual usage. BI is available for measurement at the same time as other constructs in acceptance models and is considered to be an accurate predictor of future usage behavior.14 A meta-analysis of 87 studies finds an average correlation of approximately 0.50 between behavioral intention and actual usage.19
Figure 1.
Three models of technology acceptance.
Both TAM and the motivational model have been applied successfully to predict technology acceptance outside health care domains, and TAM has been used successfully to model physicians' acceptance of telemedicine technology.20 We propose Hypotheses 1 and 2 to test these two models in the context of e-health acceptance.
Hypothesis 1: PEOU and PU will have significant positive influence on BI, as predicted by TAM.
Hypothesis 2: IM and EM will have significant positive influence on BI, as predicted by the motivational model.
As development and testing of the two models have progressed, it has become clear that the PU construct of TAM and the EM construct of the motivational model measure the same underlying construct.21 In recognition of this situation, Venkatesh et al.21 developed an integrated model that uses IM, PEOU, and a unitary PU-EM construct to predict BI (▶). Their initial test of this model resulted in better fit statistics than either TAM or the motivational model alone. We replicate these tests in an e-health context with two hypotheses.
Hypothesis 3: The integrated model will be a better fit than TAM.
Hypothesis 4: The integrated model will be a better fit than the motivational model.
Potential Antecedents
In many studies of IT acceptance, antecedent factors relating to the individual, organization, and system have been shown to significantly affect IM, PEOU, PU, and EM.22,23,24,25 Because these factors have temporal precedence to system acceptance and occur independently of the model constructs, they may be applied to predict users' tendencies toward technology acceptance before the technology is actually implemented. Assuming that predictions involving e-health acceptance can be made from antecedent characteristics of patients, it will be important for health care providers to examine these factors prior to making decisions regarding e-health design and deployment. After a careful review of the health care literature, we identified several patient-centered factors that have the potential to affect acceptance of e-health. These are described in the following sections, and hypotheses are developed to test the effects of each factor on IM, PEOU, and PU-EM model constructs. For brevity, a single hypothesis showing the three separate tests is written for each factor.
Satisfaction with medical care
Research shows that the more satisfied that a patient is with medical care, the more likely he or she is to follow the physician's advice.26 Dissatisfaction with medical care can motivate patients to change physicians27 or leave a health plan.28 In addition, satisfaction with a prior hospital experience has been shown to influence evaluations of current experiences.29 These findings suggest that patients who are more satisfied with their current medical care will tend to be more receptive to their provider's additional offerings, including e-health.
Hypothesis 5: Patients who are more satisfied with their medical care will have higher acceptance of e-health, as measured by (a) IM, (b) PEOU, and (c) PU-EM.
Health Care Knowledge
Patients often use e-health sites to gain information about a health condition or disease30 and increase their knowledge about health topics.31 This suggests that patients who feel that they have relatively little knowledge about caring for their own health will tend to accept provider-delivered e-health.
Hypothesis 6: Patients with lower perceived health knowledge will have higher acceptance of e-health, as measured by (a) IM, (b) PEOU, and (c) PU-EM.
Information-seeking Preference
In response to calls for patients to be more involved in their own care, several studies have examined patients' information-seeking preferences. Although most patients do not want to make all the decisions regarding their health care, they do want to be informed.32,33,34 Among patients with chronic conditions, Strull et al.35 report that 41% would prefer to have received additional information from their health care provider. E-health increases the availability of information and may provide a less difficult means of gaining that information compared with finding it in a medical library or asking a physician. This suggests that patients with high information-seeking preference will tend to accept e-health.
Hypothesis 7: Patients who have a higher information-seeking preference will have higher acceptance of e-health, as measured by (a) IM, (b) PEOU, and (c) PU-EM.
Health Care Need
Certain health conditions increase patients' need for health care beyond that of the general patient population. These conditions include chronic diseases, such as diabetes, severe injuries, and lengthy recuperation or rehabilitation periods, all of which can necessitate frequent visits to the primary care physician or specialists. It is anticipated that high need for health care will increase patients' tendencies to accept e-health as a means to receive additional care or reduce the time spent in receiving care.
Hypothesis 8: Patients with higher health care need will have higher acceptance of e-health, as measured by (a) IM, (b) PEOU, and (c) PU-EM.
Internet Dependence
More than 60% of Americans now have Internet access, and the U.S. population is becoming increasingly dependent on the Internet for information and communication involving health care, government, and other institutions.36 We expect that high levels of Internet dependence will increase patients' tendencies to accept e-health.
Hypothesis 9: Patients with higher Internet dependence will have higher acceptance of e-health, as measured by (a) IM, (b) PEOU, and (c) PU-EM.
Methods
An online questionnaire was administered to subjects who had recently registered for access to e-health delivered by a large health care provider in the midwestern United States. The questionnaire implemented items representing the constructs in TAM, the motivational model, the integrated model, and the five hypothesized antecedent factors.
E-health Application
The provider's e-health application delivers encyclopedic health content with both browse and search access and e-mail-style connectivity with the clinic office that implements standards for patient privacy and security37 and online prescription refill ordering and appointment scheduling. The application was designed to meet standards for accurate health information content38 and for simplified accessibility for users who do not have extensive computer experience as well as elderly patients.39 Access for users is unrestricted, but they must first register online and thereafter log in using a self-assigned ID and password.
Procedure
Patients were informed about the provider's e-health application by a mass mailing featuring a descriptive color brochure. Approximately one month after this mailing, an invitation to participate in the study was sent to the e-mail addresses of the 1,750 individuals who had registered for access. Of these, 163 (9%) responded to the invitation and completed the entire online questionnaire. The health care provider declined to allow the researchers to send additional requests to participate. The subjects' average age was 50 years and 79% were female. Respondents were asked to rate the provider's e-health application and their previous experiences with the provider via an online questionnaire (items used in the questionnaire are presented in Appendix 1). The questionnaire software randomized the administration order of the scaled items for each subject to avoid contamination of responses through item-adjacency effects. Nonscaled items assessing health care need and demographic characteristics were placed at the end of the questionnaire.
Measurements
Items measuring the constructs of TAM, the motivational model, and the integrated model were drawn from validated scales.15,16,21 Items measuring satisfaction with medical care were drawn from Marshall et al.,40 and items measuring information-seeking preference came from Ende et al.32 Items for health care knowledge, Internet dependence, and health care need were developed within the current study. Health care knowledge items were developed to measure the extent of knowledge and understanding of personal health problems. Internet-dependence items were developed to measure usage frequency of and dependence on the Internet and e-mail. Health care need items were developed to measure three facets of need: the frequency of visits to physicians, the number of physicians visited during the previous six months, and the presence of a chronic health condition. Reliability measures for the constructs are reported in Appendix 1.
Results
Data were screened to ensure that responses were entered to all items. Only completed questionnaires were used, so there were no missing data in the analysis of results. In the cases in which subjects spelled out numbers in their textbox entries, these were manually converted to numerical values. All model constructs show reliability in excess of 0.90 (Cronbach's α). All four scaled antecedent factors show reliability in excess of 0.70 except information-seeking preference (α = 0.60), a construct derived from Ende et al.32
Hypothesis testing was conducted using structural equation modeling (SEM). SEM analysis incorporates unique effects of individual measurement items and calculates both direct and indirect effects within a model. This makes SEM useful for assessing models that utilize latent variables (i.e., constructs that are not observed directly but are instead measured indirectly using multiple items) or contain intervening or mediating variables.41 These abilities are especially appropriate for the models that we were testing because their constructs cannot be measured directly and they contain a variety of mediating variables, e.g., PEOU and PU-EM in the integrated model. Application of SEM and model-fit metrics are discussed in the following sections.
Effectiveness of Acceptance Models
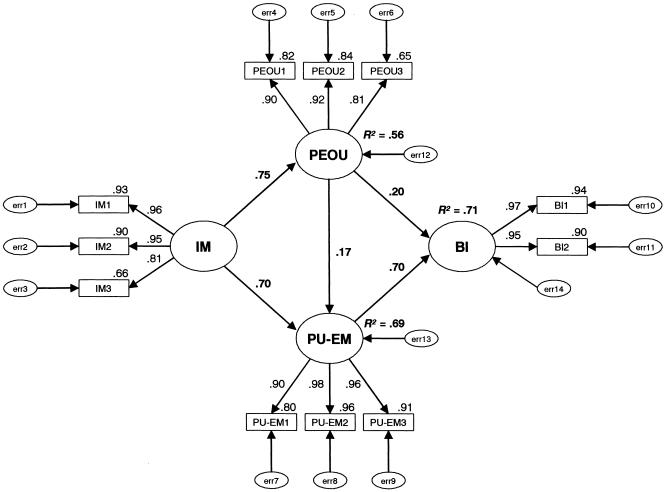
Hypotheses 1–4 address the effectiveness of TAM, the motivational model, and the integrated model in predicting BI of patients to use e-health. To test these hypotheses, SEM was conducted to assess the relationships among each model's constructs using AMOS 4 software.42 The results of these analyses are shown in ▶ and ▶. All predicted relationships were significant except the relationship between IM and BI that is predicted by the integrated model. TAM and the motivational model each accounted for 70% of the measured variance (R2) in BI, and all constructs in each model made significant positive contributions to the predictions. This supports Hypotheses 1 and 2. The integrated model produced fit statistics that are not clearly better than those of its constituent models, failing to support Hypotheses 3 and 4. We found that the PU-EM construct by itself predicts 68% of the measured variance in BI. Because PU-EM is a key construct in each of the tested models, the result is that all models produced similar results in our tests.
Table 1.
Model Results
| χ2 | df | χ2/df | GFI | AGFI | CFI | NFI | TLI | RMSEA | |
|---|---|---|---|---|---|---|---|---|---|
| Model | |||||||||
| TAM | 52.97 | 17 | 3.115 | 0.923 | 0.837 | 0.976 | 0.966 | 0.961 | 0.114 |
| Motivational model | 57.08 | 17 | 3.358 | 0.919 | 0.828 | 0.961 | 0.967 | 0.961 | 0.121 |
| Integrated model | 94.00 | 39 | 2.410 | 0.905 | 0.839 | 0.975 | 0.958 | 0.964 | 0.093 |
| Model including antecedents | |||||||||
| Motivational model | 153.65 | 84 | 1.829 | 0.889 | 0.842 | 0.970 | 0.937 | 0.963 | 0.053 |
| TAM | 249.07 | 144 | 1.730 | 0.864 | 0.821 | 0.954 | 0.898 | 0.945 | 0.067 |
| Integrated model | 343.04 | 200 | 1.715 | 0.843 | 0.801 | 0.952 | 0.892 | 0.944 | 0.066 |
TAM = technology acceptance model; GFI = goodness of fit; AGFI = adjusted goodness of fit; CFI = comparative fit index; NFI = normed fit index; TLI = Tucker-Lewis index; RMSEA = root mean square error of approximation.
Figure 2.
Integrated model showing standardized estimates. Measured items are illustrated in rectangles (e.g., IM1). Latent variables are illustrated in ovals (e.g., IM); smaller ovals illustrate error of measurement (e.g., err1). Associations are illustrated by arrows that indicate the direction of prediction. Factor loadings are noted at the top right of item rectangles. Coefficients are noted for each association (i.e., directional arrow). Variance (R2) is noted for each latent variable within the model that has an association directed toward it.
Model fit is typically assessed using a set of metrics that captures various perspectives of fit.42 We report the following fit metrics:
χ2/df: This ratio of the minimum sample discrepancy (χ2) to the degrees of freedom in a sample is interpreted as the distance from perfect fit, a ratio of 1:1; ratios up to approximately 3:1 are considered to indicate acceptable fit.43
GFI/AGFI: Goodness of fit index (GFI) and adjusted goodness of fit index (AGFI) values fall between 0 and 1; GFI values >0.90 and AGFI values >0.80 are considered to indicate reasonable fit.
CFI/NFI/TLI: Comparative fit index (CFI), normed fit index (NFI), and Tucker-Lewis index (TLI) compare model fit to a badly fitting baseline model42; in each case, values close to 1 indicate good fit.
RMSEA: The root mean square error of approximation (RMSEA) compensates for effects in which complex models are disadvantaged by simple fit metrics; values of ≤0.08 indicate reasonable fit.44
All models show good fit on some metrics (e.g., NFI >0.90) but are outside target limits on other metrics (e.g., RMSEA >0.08). In general, the fit results are numerically close to those reported by Venkatesh et al.21 These results suggest that the structures of the current models are reasonably accurate and reliable across studies. However, because model fit is somewhat less than ideal, it may be possible to improve on the models in future research.
Importance of Antecedent Factors
Assessing the importance of the five hypothesized antecedent factors in predicting acceptance proceeded in three stages. First, correlations were produced between the factors and model constructs (▶), providing a test of simple association. Four factors showed a significant association with at least one of the model constructs. Health care need was implemented through three items that measure the number of physicians seen, the number of visits during the past six months, and the existence of chronic disease. None of these measures showed significant associations with model constructs, failing to support any part of Hypothesis 8.
Table 2.
Correlations between Hypothesized Antecedents and Model Constructs
| Hypothesized Antecedent | IM | PEOU | PU-EM |
|---|---|---|---|
| Satisfaction with medical care | 0.335‡ | 0.229† | 0.275‡ |
| Health care knowledge | 0.105 | 0.213† | 0.081 |
| Internet dependence | 0.248† | 0.221† | 0.327‡ |
| Information-seeking preference | 0.175* | 0.270† | 0.209† |
| Number of physicians seen during the past 6 months | −0.011 | −0.065 | 0.000 |
| Number of visits to physician during the past 6 months | 0.044 | −0.116 | −0.011 |
| Chronic disease that requires special medical attention | −0.059 | −0.047 | 0.031 |
IM = intrinsic motivation; PEOU = perceptions of ease of use; PU-EM = perceptions of usefulness–extrinsic motivation.
Significant at the 0.05 level.
Significant at the 0.01 level.
Significant at the 0.001 level.
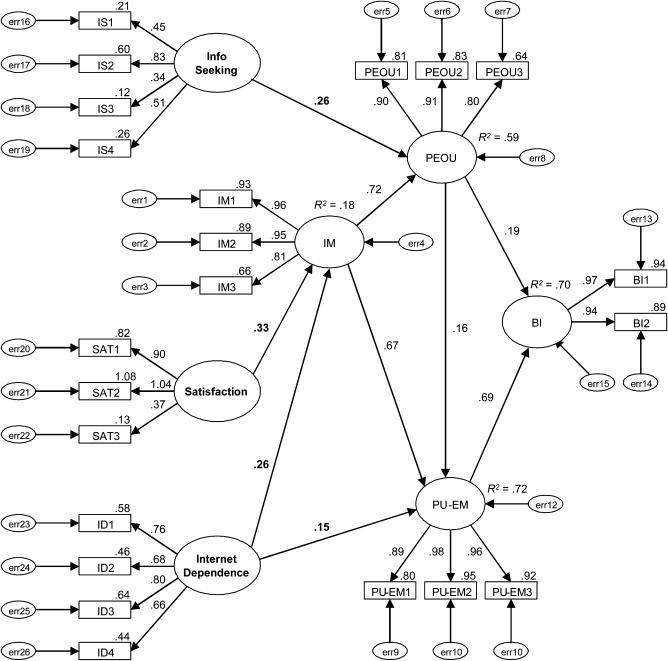
Second, to test the remainder of the hypotheses, SEM was run to associate the four correlated antecedent factors with the IM, PEOU, and PU-EM factors from the integrated model (▶). As shown in ▶, fit of the model including antecedents improved on metrics that adjust more for model complexity (e.g., χ2/df and RMSEA) and tended to decline on metrics that do not adjust or adjust less (e.g., GFI, AGFI, CFI, NFI, and TLI). Overall, the metrics suggest that inclusion of the antecedents does not diminish model fit and may actually improve fit somewhat. The results indicate that three of the four antecedents are important unique predictors of e-health acceptance; however, none of these provided overall predictions of IM, PEOU, and PU-EM. Satisfaction with medical care predicts IM, supporting Hypothesis 5a, and information-seeking preference predicts PEOU, supporting Hypothesis 7b. Internet dependence predicts both IM and PU, supporting Hypotheses 9a and 9c. Health care knowledge did not provide any significant unique predictions.
Figure 3.
Integrated model with antecedents showing standardized estimates.
Finally, stepwise regressions were run to test the cumulative strength of relationships between the antecedent factors identified in SEM and the individual model constructions. The combined antecedent factors accounted for 20% of variance (adjusted R2) in IM, 13% in PEOU, and 20% in PU-EM. These figures suggest that the antecedents will have good predictive power across the three acceptance models.
Discussion
All the acceptance models performed reasonably well in our tests. Although we anticipated that these models would be applicable to e-health acceptance based on substantial research in other domains, it is reassuring to find that they are robust in the previously untested context of e-health and among a subject group primarily composed of middle-aged to elderly female medical patients, a population that has not previously been studied by technology acceptance researchers.
All models showed adequate fit on most metrics. Yet, as was discussed previously, it may be possible to improve on these models. Future researchers should consider several methods that have been recommended for developing better models,41 including refinement of measures, use of multiple measurement methods, and incorporating different constructs and associations. Where new constructs and associations are to be used, however, it is strongly recommended that these changes be theoretically driven because this will allow findings to be related to other research and generalized among situations. In particular, it will be important to consider evaluating related models, e.g., the theory of reasoned action,17,18 because these may prove to be more applicable than the models that we chose to study.
The findings suggest that health care providers have flexibility in choosing which model to apply to e-health acceptance. The choice of models in a priori situations, i.e., predicting patients' e-health acceptance prior to application use, should be driven by the antecedent factors that are available for measurement. We recommend applying the integrated model in situations in which measurements of satisfaction with medical care, information-seeking preference, and Internet dependence are available.
Health care providers can use this information in several ways. First, findings from the current study identify several characteristics of patients who tend to accept e-health, which may be useful both in guiding the overall decision of whether to deploy e-health and in clarifying the prospects for e-health within specific patient populations. Patients who are satisfied with their current medical care, those who prefer to seek information about their health care, and those who are already dependent on the Internet tend to accept e-health. Thus, it is likely that patients will use e-health to expand and augment interactions with their health care provider rather than replace interactions that they dislike. One implication of the findings is that e-health will not be instrumental in mitigating problems that may already exist in the relationship between the health care provider and the patient, at least not during initial use.
Second, the findings demonstrate a mechanism for investigating acceptance of specific aspects of e-health. The studied e-health application implemented a range of components related to content, connectivity, and care that the application designers intended to be useful and attractive to patients. However, research has shown that some of the e-health components that designers have the highest hopes for and expend the most funds to produce are used only infrequently by patients.45 Simple survey techniques can reveal patients' BI to use e-health components based primarily on model constructs, such as PU, and secondarily on antecedent factors, which offer the added benefit to e-health designers of clearly delineating key characteristics of potential users.
Limitations
This research is necessarily limited by the geographic location of the health care provider and its patients, the configuration of the e-health application that the provider implemented, our choice of antecedent and measurement factors, and the means by which we recruited subjects. Therefore, we suggest caution in generalizing the findings to substantially different locations or to specialized e-health applications, and we recommend that future researchers explore other potential antecedents. Some interesting examples include measures of patients' health care involvement, normative influences, and socioeconomic status. Although BI is frequently used as the dependent variable in technology acceptance studies and has been shown to be a good predictor of use, future research should extend our design to examine subsequent use of e-health. It is possible that there may be systematic differences between patients who responded to our questionnaire and those who did not respond, and this could have biased our findings. Finally, we surveyed only patients who registered to use e-health technology. Future research should investigate which factors are important in acceptance of e-health by patients in general.
Conclusion
The current research represents a first step in understanding acceptance of e-health technology. For this reason, we chose to apply well-known acceptance models and test their associations with logically related patient characteristics. From these beginnings, it will be important to expand the research in two directions. First, it is key to understand which aspects of e-health are valued by different types of patients and in different situations. Because of the wide range of health care offerings and patient needs that exists, it is difficult to envision a single “best of breed” e-health application that would be able to cover all uses without overloading users. For this reason, there is likely to be greater demand for applicable theories, models, and guidelines for configuring e-health applications than is the case with most custom software. Second, although we have argued that modeling e-health acceptance is useful to health care providers, it is important to extend research to understand why patients continue to use these applications. Research in the area of continuance is likely to provide deeper insights into the process of improving e-health so it can meet ongoing patient needs and become an increasingly valued part of health care services.
Appendix 1
The following items were administered to subjects in the study. Scale items accept responses on a seven-position scale where 1 = strongly disagree and 7 = strongly agree. Presentation order of the scale items was randomized prior to each new administration of the online questionnaire. Reliability scores (Cronbach's α) for items in each construct are shown in parentheses.
Satisfaction with Medical Care Scale (α = 0.78)
SAT1: I am very satisfied with the medical care that I receive.
SAT2: All things considered, the medical care that I receive is excellent.
SAT3: There are things about the medical system from which I receive my care that need to be improved. (Reversed)
Health Knowledge Scale (α = 0.73)
HK1: I am very knowledgeable regarding care for my health problems.
HK2: I understand my health problems and how to care for them.
Internet Dependence Scale (α = 0.82)
ID1: Having access to the Internet is important to me.
ID2: I spend a lot of time using the Internet.
ID3: The ability to send and receive e-mail is important to me.
ID4: I send and receive numerous e-mail messages.
Information-seeking Preference Scale (α = 0.60)
IS1: I believe that as a person becomes sicker that person should be told more and more about his or her illness.
IS2: I believe that doctors should explain the purpose of laboratory tests.
IS3: I believe that people should know all the side effects of their medications.
IS4: When there is more than one method to treat a problem, I should be told about each one.
Health Care Need (measured as three separate aspects of need, each as a single item)
HN1: Number of face-to-face visits [to your physician during the past six months]. (Textbox response)
HN2: How many different physicians have you seen at your health care provider during the past six months? (Textbox response)
HN3: Do you have a chronic disease (such as diabetes or asthma) that requires special medical attention? (Binary response)
IM: Intrinsic Motivation Scale (α = 0.93)
IM1: I will find [e-health] to be enjoyable.
IM2: The actual process of using [e-health] will be pleasant.
IM3: I will have fun using [e-health].
PEOU: Perceived Ease of Use Scale (α = 0.91)
PEOU1: My interaction with [e-health] will be clear and understandable.
PEOU2: [E-health] will be easy to use.
PEOU3: I will find it easy to get [e-health] to do what I want it to do.
PU-EM: Perceived Usefulness: Extrinsic Motivation Scale (α = 0.96)
PU-EM1: Using [e-health] will support critical aspects of my health care.
PU-EM2: Using [e-health] will enhance my effectiveness in managing my health care.
PU-EM3: Overall, [e-health] will be useful in managing my health care.
BI: Behavioral Intention to Use E-health Scale (α = 0.96)
BI1: I intend to use [e-health].
BI2: I predict I will use [e-health].
A preliminary version of this paper was presented at the 2003 Americas Conference on Information Systems (AMCIS), Tampa, FL, August 6–9, 2003.
References
- 1.Maheu MM, Whitten P, Allen A. E-health, Telehealth, and Telemedicine. San Francisco, CA: Jossey-Bass, 2001.
- 2.Kaplan B, Brennan PF. Consumer informatics supporting patients as co-producers of quality. J Am Med Inform Assoc. 2001;8:309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinciroli F. A manifesto on telehealth and telemedicine. J Am Med Inform Assoc. 2001;8:349–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson EV. Asynchronous health care communication. Commun ACM. 2003;46:79–84. [Google Scholar]
- 5.Lazarus IR. Separating myth from reality in e-health initiatives. Managed Healthc Exec. 2001;Jun:33–6. [Google Scholar]
- 6.Malcolm CL. Five e-business strategies you can take to the bank. Healthc Financ Manage. 2001;Sep:72–5. [PubMed] [Google Scholar]
- 7.Masys D, Baker D, Butros A, Cowles KE. Giving patients access to their medical records via the Internet: the PCASSO experience. J Am Med Inform Assoc. 2002;2:181–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson EV, Lankton NK. Strategic implications of asynchronous healthcare communication. Int J Healthc Technol Manage. 2003;5:213–31. [Google Scholar]
- 9.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care?. JAMA. 2003;290:259–64. [DOI] [PubMed] [Google Scholar]
- 10.Plunkett. Health Care Industry Trends and Market Analysis. Plunkett Research, Ltd. Available at: http://www.plunkettresearch.com/health/health_trends.htm. Accessed Feb 7, 2004.
- 11.Homan Q. Healthcare satisfaction study final report. Harris Interactive/ARiA Marketing Report. Available at: http://www.harrisinteractive.com/news/downloads/harrisariahcsatrpt.pdf. Accessed Feb 7, 2004.
- 12.Brooks FP. The Mythical Man-Month. Reading, MA: Addison-Wesley, 1995.
- 13.Davis FD. User acceptance of information technology: system characteristics, user perceptions, and behavioral impacts. Int J Man Machine Stud. 1993;38:475–8. [Google Scholar]
- 14.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989;13:319–29. [Google Scholar]
- 15.Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: a comparison of two theoretical models. Manage Sci. 1989;35:982–1002. [Google Scholar]
- 16.Davis FD, Bagozzi RP, Warshaw PR. Extrinsic and intrinsic motivation to use computers in the workplace. J Appl Soc Psychol. 1992;22:1111–32. [Google Scholar]
- 17.Fishbein M, Belief Ajzen I. Attitude, Intention, and Behavior. Reading, MA: Addison-Wesley, 1975.
- 18.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall, 1980.
- 19.Sheppard BH, Hartwick J, Warshaw PR. The theory of reasoned action: a meta-analysis of past research with recommendations for modifications and future research. J Consumer Res. 1988;15:325–43. [Google Scholar]
- 20.Hu PJ, Chau PYK, Sheng ORL, Tam KY. Examining technology acceptance model using physician acceptance of telemedicine technology. J Manage Inf Syst. 1999;16:91–112. [Google Scholar]
- 21.Venkatesh V, Speier C, Morris MG. User acceptance enablers in individual decision making about technology: toward an integrated model. Decis Sci. 2002;22:297–316. [Google Scholar]
- 22.Gefen D, Straub DW. Gender differences in the perception and use of e-mail: an extension to the technology acceptance model. MIS Q. 1997;21:389–400. [Google Scholar]
- 23.Venkatesh V, Davis FD. A model of the antecedents of perceived ease of use: development and test. Decis Sci. 1996;27:451–81. [Google Scholar]
- 24.Jackson CM, Chow S, Leitch RA. Toward an understanding of the behavioral intention to use an information system. Decis Sci. 1997;28:357–89. [Google Scholar]
- 25.Hong W, Thong JYL, Wong W, Tam K. Determinants of user acceptance of digital libraries: an empirical examination of individual differences and system characteristics. J Manage Inf Syst. 2001;19:97–124. [Google Scholar]
- 26.Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz RL. Antecedents of adherence to medical recommendations: results from the medical outcomes study. J Behav Med. 1992;15:447–68. [DOI] [PubMed] [Google Scholar]
- 27.Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE. Patients' ratings of outpatient visits in different practice settings. JAMA. 1993;270:835–40. [PubMed] [Google Scholar]
- 28.Kerr EA, Hays RD, Lee ML, Siu AL. Does dissatisfaction with access to specialists affect the desire to leave a managed care plan?. Med Care Res Rev. 1998;55:59–77. [DOI] [PubMed] [Google Scholar]
- 29.John J. Patient satisfaction: the impact of past experience. J Health Care Marketing. 1992;12:56–64. [PubMed] [Google Scholar]
- 30.Ferguson T. Online patient-helpers and physicians working together: a new partnership for high quality health care. BMJ. 2000;321:1129–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fulton ML. A healthy flow of information. Searcher. 2002;10:10–2. [Google Scholar]
- 32.Ende J, Lewis K, Ash A, Moskowitz MA. Measuring patients' desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med. 1989;4:23–30. [DOI] [PubMed] [Google Scholar]
- 33.Nease RF, Brooks WB. Patient desire for information and decision making in health care decisions: the Autonomy Preference Index and the Health Opinion Survey. J Gen Intern Med. 1995;10:593–600. [DOI] [PubMed] [Google Scholar]
- 34.Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making?. Arch Intern Med. 1996;156:1414–20. [PubMed] [Google Scholar]
- 35.Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making?. JAMA. 1984;252:2990–4. [PubMed] [Google Scholar]
- 36.Horrigan JB, Rainie L. Counting on the Internet. Pew Internet & American Life. Available at: http://www.pewinternet.org/reports/pdfs/PIP_Expectations.pdf. Accessed Feb 7, 2004.
- 37.Prady SL, Norris D, Lester JE, Hoch DB. Expanding the guidelines for electronic communication with patients. J Am Med Inform Assoc. 2001;8:344–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fallis D, Frické M. Indicators of accuracy of consumer health information on the Internet: a study of indicators relating to information for managing fever in children in the home. J Am Med Inform Assoc. 2002;9:73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Demiris G, Finkelstein SM, Speedie SM. Considerations for the design of a Web-based clinical monitoring and educational system for elderly patients. J Am Med Inform Assoc. 2001;8:468–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marshall GN, Hays RD, Sherbourne CD, Wells KB. The structure of patient satisfaction with outpatient medical care. Psychol Assess. 1993;5:477–83. [Google Scholar]
- 41.Maruyama GM. Basics of Structural Equation Modeling. Thousand Oaks, CA: Sage, 1998.
- 42.Arbuckle J, Wothke W. AMOS 4.0 User's Guide. Chicago, IL: Smallwaters Corporation, 1999.
- 43.Carmines EG, McIver JP. Analyzing models with unobserved variables. In Bohrnstedt GW, Borgatta EF (eds). Social Measurement: Current Issues. Beverly Hills, CA: Sage, 1981, pp 65–115.
- 44.Browne MW, Cudeck R. Alternative ways of assessing model fit. In Bollen KA, Long JS (eds). Testing Structural Equation Models. Newbury Park, CA: Sage, 1993, pp 136–62.
- 45.Payton FC, Brennan PF. How a community health information network is really used. Commun ACM. 1999;42:85–9. [Google Scholar]