Abstract
Objective
This study sought to determine congruence between student assessment tasks within the master of chiropractic curriculum at Macquarie University and 2 separate but related domains: (1) disorders commonly presenting to chiropractors and (2) musculoskeletal conditions for which there is published evidence that chiropractic treatment is effective.
Methods
A literature review was undertaken to determine which musculoskeletal disorders commonly present to chiropractors and the conditions for which there is published evidence that chiropractic treatment is effective. These 2 domains were then mapped to the assessment tasks within the curriculum and analyzed. The proportion of time allocated to theory versus skill acquisition was also determined.
Results
Assessment tasks within the curriculum specifically focus on low back pain, neck pain, lower extremity pain, thoracic pain, and adhesive capsulitis. This curriculum mapping demonstrates congruence between the student assessment tasks and published evidence for chiropractic. The assessments also contain an appropriate balance between theory and skills acquisition.
Conclusion
There is congruence between the assessment tasks within the curriculum and the 2 domains against which it was mapped. Thus, completion of the curriculum provides training relevant to conditions that commonly present to chiropractors and musculoskeletal conditions for which chiropractic treatment is effective.
Key Indexing Terms: Chiropractic, Curriculum, Education, Evaluation, Program
INTRODUCTION
According to Harden,1 a curriculum map displays how and when content is taught and which measurement outcomes can be used to determine success. Ultimately, an accurate map will arrange each aspect of the curriculum in a logical and transparent manner, making them equally available to academics and students involved with the program.1
Curriculum mapping has gained widespread popularity with professionals from all areas of education and has been somewhat transformed by modern technology. English first described curriculum mapping in the 1980s as an accurate record of the content taught in a program, the duration of the teaching, and the congruence between what was taught and assessment tasks.2,3 Jacobs4 expanded this concept to include timelines, as well as scheduling of the content taught within the curriculum and a review of both material taught and examination content. Later, electronic collections of these data were used to create curriculum maps.3–5
Curriculum mapping is extremely useful as it assists educators to ensure that course content and assessment tasks accurately reflect the curriculum, while also enabling students to identify the learning outcomes required for success. In the context of our master of chiropractic (MChir) program, this ensures that all graduating students possess the required graduate capabilities to practice safely and effectively.6–10 Although there is significant literature discussing mapping within medicine, there is substantially less literature available for chiropractic curricula.1,11–14 One shared theme between the 2 professions is that the available literature primarily outlines undergraduate programs.11–14 It is important to note that although the program under discussion is for a master degree, it is still fundamentally one that is training primary contact practitioners, not specialists. As such, the literature pertaining to mapping undergraduate programs is still relevant to our study. As primary contact professions, it is important that both medical and chiropractic educators continue to reflect upon the ability of their programs to adequately prepare graduates for entry into clinical life.
When discussing mapping of chiropractic curricula, Vermet focused on “lumbopelvic diagnostic and therapeutic procedures” taught at the Canadian Memorial Chiropractic College. Vermet concluded that while the degree of vertical integration between the undergraduate and clinical program is considerable, it was not entirely complete.7 Several other studies have explored the relationship between graduate perceptions of their chiropractic studies and the degree to which this training was used in a clinical environment. These studies concluded that there were several aspects of the curriculum—namely the basic sciences—that graduates felt they were not using routinely in the clinic.8,15,16
The 2011 Health Workforce Australia Simulated Learning Environment Chiropractic Curriculum Report, compiled by the School of Chiropractic and Health Sciences at Murdoch University in Australia, maps the institution's double-bachelor's curriculum to nonspecific areas including, but not limited to, basic and health sciences, chiropractic skills, and clinical sciences, with a focus on simulated learning. This report provides analysis of the curriculum but does not focus on individual conditions.17 Therefore, we intend that the present article will provide a foundation for more detailed curriculum mapping.
By necessity, accurate mapping is a dynamic, time- and effort-intensive process requiring ongoing feedback and evaluation by both academics and students. It has been widely used within medical education.13,14,18–20 There are a multitude of techniques used to map a curriculum, and traditionally, several stages are involved.1,5,21,22 Prideaux5 discusses the 2 main models of curriculum mapping: prescriptive and descriptive. Prescriptive models are constructed prospectively and indicate what the curriculum should cover, focusing on the end goal of a curriculum rather than the details. Descriptive models are formed retrospectively and focus on the details of what was taught and the context in which it was studied. As all elements within a curriculum are linked, teaching content should be based upon well-formulated statements of intent and should be taught in the context of both internal and external influences.1,5,23
The purposes of this research were to (1) review the literature for commonly presenting complaints to chiropractors and musculoskeletal disorders for which there is published evidence that chiropractic treatment is effective and (2) map the assessment tasks of the MChir curriculum at our university to these conditions.
METHODS
The literature review investigating curriculum mapping was conducted within the Education Resources Information Center (ERIC) and A+ education databases using the Macquarie University Library web portal (last accessed October 5, 2013). Search terms included the following: chiro*, educat*, curric*, map*, design, undergrad*, postgrad*, medical, learning outcomes, grad* capabilit*. The literature review for the top 9 presenting complaints and musculoskeletal disorders for which chiropractic treatment has been shown to be effective used articles retrieved from the Macquarie University Library website (last accessed October 5, 2013). Databases used included Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, ScienceDirect, Scopus, and the Cochrane Collaboration Collection. Search terms used were as follows: common, present*, complaint*, chiro*, clinic*, musculoskelet*, manage*, patient*, descript*, demographic*, Australia*, epidemiolog*, evidence-base*. The authors also conducted a hand search of the reference lists of key articles. Inclusion criteria for both literature reviews included full-text articles, English language, systematic reviews and meta-analyses, and articles published from January 1, 2003, to October 5, 2013. Exclusion criteria were abstract-only, non–English language, and case report articles. There were no exclusion criteria for the hand search.
Following this review, outlines from each of the sixteen 2012–2013 MChir units were accessed using the Macquarie University Department of Chiropractic website: https://units.mq.edu.au/2013/departments/chiropractic/show (last accessed April 7, 2013). These unit outlines were both printed as a hard copy and saved to Dropbox. Qualitative mapping of the assessment tasks delivered within these units was then completed via vertical and horizontal integration against the results from the literature review. Inclusion criteria for the unit outlines included the final draft of all units studied within the 2012–2013 MChir program. Criteria for exclusion were units not studied within the 2012–2013 MChir program. Ethics approval for this study was granted by the Macquarie University Ethics Committee, reference number 5201300397.
To achieve a quick overview of the coverage of the disorders within the MChir curriculum, a summary map was created. If the topic was sufficiently covered in a unit, this was marked with an X, and if the topic was not sufficiently covered, the box was left blank. Significant depth of coverage of a topic within a unit was considered to have occurred if it was the main theme of a 1-h lecture or tutorial. If the MChir curriculum achieved an average of 3 X's per topic per semester across each of the 4 semesters, it was deemed to adequately address that topic.
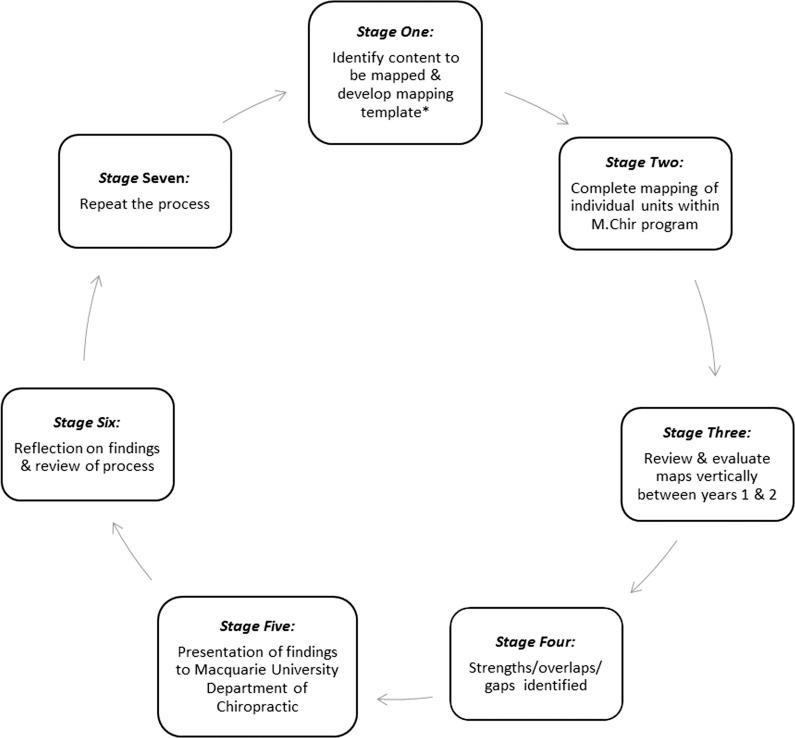
Following this, the unit outlines were hand searched for the purpose of mapping the weighting of content versus skills acquisition for each of the assessment tasks (Fig. 1). Content represents theory taught, whereas skills acquisition includes behaviors such as history taking, clinical decision making, or manual therapy skills. Specifically, it was decided to map to assessment tasks as it was assumed that important topics within each unit would have appropriate representation. Further analysis of skills acquisition is beyond the scope of this article. Following this, each final examination was hand searched, and the corresponding spread of marks allocated to each of the disorders was subsequently mapped against individual units. The data obtained in this way were entered into a Microsoft Excel (Microsoft Corp, Redmond, WA) spreadsheet. Descriptive analysis was completed using tables and histograms enabling accurate and clearly defined mapping of the assessment tasks delivered within each of the MChir units to each disorder.
Figure 1.
Process for mapping the 2-year master of chiropractic curriculum. *Template refers to the mapping instrument presented in Table 1.
RESULTS
A comprehensive search of the literature for systematic reviews on the effectiveness of chiropractic care for musculoskeletal disorders revealed an article published by Bronfort et al.24 In a paper regarding the effectiveness of manual therapies in the United Kingdom, the authors systematically discuss the evidence available for a comprehensive number of musculoskeletal complaints that commonly present to manual therapists.24 The quality of the evidence is categorized into levels, namely inconclusive, moderate, or high. This article provided the basis to ascertain the musculoskeletal disorders for which there is published evidence that chiropractic treatment is effective.
Another systematic review (the Warwick Review, accessible on the website of Health Sciences Research Institute at the University of Warwick for the College of Chiropractors)25 supports chiropractic treatment for the 9 musculoskeletal conditions for which the Bronfort study noted as having favorable evidence. In excess of 1000 articles were identified and evaluated for the Warwick Review, and of these studies, approximately 1 in 6 had been published since the Bronfort study. The Warwick Review also examined cost-effectiveness, which was not considered by Bronfort, and as such, some studies compared chiropractic care with general practitioner (GP) care. The Warwick Review concluded that “For patients with neck, shoulder or low back pain, manual therapies appear to be more cost-effective than usual GP care (alone or with exercise), spinal stabilization, GP advice, advice to remain active and brief pain management.”25 Both the Bronfort and colleagues study24 and the Warwick Review25 include an extensive number of musculoskeletal complaints; however, the Warwick Review discusses more comprehensively the cost-effectiveness of treatment and the depth and quality of literature available. The Warwick Review was used to corroborate the results presented by the Bronfort study.
As shown in Table 1, there is adequate coverage of the relevant disorders throughout both the first and second years of the MChir. Of note are the classes CHIR921 and CHIR922 (Topics in Chiropractic 1 and 2), which do not directly cover specific musculoskeletal disorders; rather, they teach subjects such as research methodology, nutrition, occupational health and safety, and pharmacology. These subjects are integral to the curriculum because they fall within the scope of primary contact health care.26 CHIR896 and CHIR897 (Clinical Internship 1 and 2) comprise students' year-long internship. As such, it is expected that students will be exposed to a varied case mix and gain experience in all disorders listed. However, because of the unique nature of each student's internship experience, this cannot be guaranteed. For example, interns are assigned to 1 of 3 student clinics that serve varying demographics depending upon their locale within Sydney.
Table 1.
Curriculum Mapped to the Literature Review Results for Common Presenting Conditions and to Conditions for Which Chiropractic Is Considered Effective
| MChir Year 1 (2012) |
MChir Year 2 (2013) |
|||||||||||||||
| Semester 1 |
Semester 2 |
Semester 1 |
Semester 2 |
|||||||||||||
| Mapping to: | 873 | 891 | 916 | 918 | 874 | 892 | 917 | 919 | 931 | 903 | 921 | 896 | 932 | 904 | 922 | 897 |
| (1) Literature review results | ||||||||||||||||
| LBP | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Neck pain | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Shoulder pain | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Headache | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |
| Lower-extremity pain | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Upper-extremity pain | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Thoracic pain | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Scoliosis | X | X | X | X | X | X | X | |||||||||
| TMJ pain | X | X | X | X | X | X | X | |||||||||
| (2) Effectiveness article conclusionsa | ||||||||||||||||
| Acute LBP | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Chronic LBP | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Acute/subacute neck pain | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Chronic neck pain | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Shoulder girdle pain/dysfunction | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Adhesive capsulitis | X | X | X | X | X | X | X | X | X | |||||||
| Hip osteoarthritis | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Migraine | X | X | X | X | X | X | X | X | X | X | X | X | ||||
| Cervicogenic headache | X | X | X | X | X | X | X | X | X | X | X | X | X | |||
MChir indicates master of chiropractic; LBP, low back pain; TMJ, temporomandibular joint
Class numbers indicate the following: 873/874 = Neuromusculoskeletal Diagnosis 1 and 2; 891/892 = Clinical Chiropractic 1 and 2; 916/917 = Diagnostic Imaging 1 and 2; 918/919 = Physical/Functional Assessment and Clinical Management; 931/932 = Diagnosis and Management 1 and 2; 903/904 = Clinical Chiropractic 3 and 4; 921/922 – Topics in Chiropractic 1 and 2; 896/897 = Clinic Internship 1 and 2.
The referenced effectiveness article is Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopathy. 2010;18(1):3.
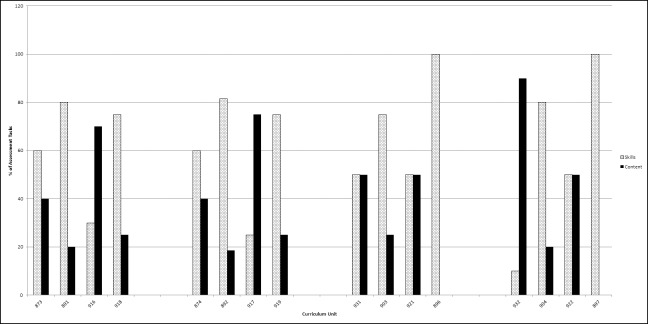
The analysis of the content vs skills acquisition data is presented in Figure 2 and shows a distinct bias toward skills acquisition in the majority of subjects. The exceptions to this are the diagnostic imaging subjects (CHIR916 and 917), the diagnosis and management subjects (CHIR931and 932), and the topics in chiropractic subjects (CHIR921 and 922). These subjects rely heavily on mastery of theory, which is then applied to the relevant scenario. Practical subjects such as chiropractic skills (CHIR891 and 892, CHIR903 and 904), clinic internship (CHIR896 and 897), and neuromusculoskeletal diagnosis (CHIR873 and 874) focus heavily on skills acquisition and clinical decisions.
Figure 2.
Percentage of skills vs. content tested in both assessment tasks and final examinations. Numbers along the X-axis refer to the curriculum units (873 and 874 = Neuromusculoskeletal Diagnosis 1 and 2; 891 and 892 = Clinical Chiropractic 1 and 2; 916 and 917 = Diagnostic Imaging 1 and 2; 918 and 919 = Physical/Functional Assessment and Clinical Management ; 931 and 932 = Diagnosis and Management 1 and 2; 903 and 904 = Clinical Chiropractic 3 and 4; 921 and 922 = Topics in Chiropractic 1 and 2; 896 and 897 = Clinic Internship 1 and 2.
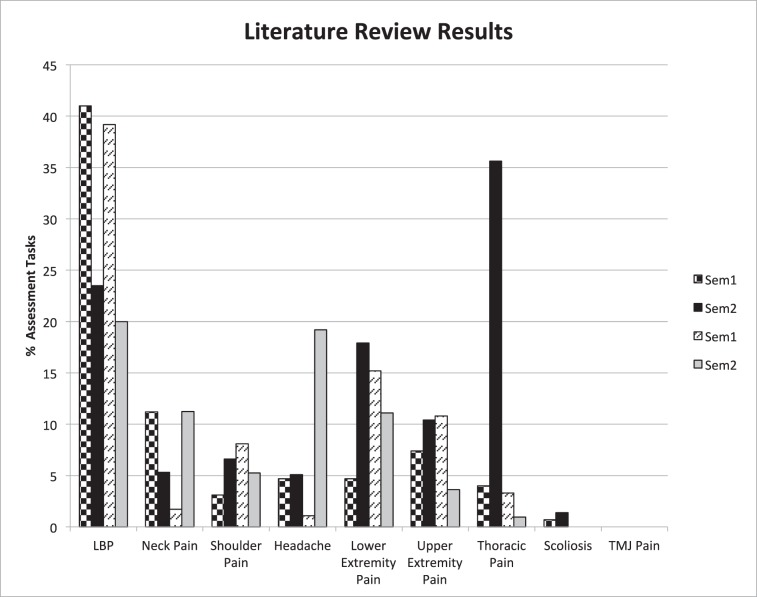
Congruency between the MChir curriculum and the top 9 presenting complaints is depicted in Figure 3. Low back pain, the most frequently presenting complaint to chiropractors, is most comprehensively covered. Neck pain and headache are often taught concurrently, which may partially explain why they both appear to be covered less than would be expected. It is suggested that the lower limb was used to assess student's knowledge of theory and skills during theory assessment tasks and examinations, thus resulting in a high rate of coverage of lower extremity pain. Temporomandibular joint disorders are not represented within the assessment tasks, but are covered adequately within the course work.
Figure 3.
Mapping to assessment tasks the commonly presenting complaints to chiropractic practice, per the literature review. LBP indicates low back pain; TMJ, temporomandibular joint.
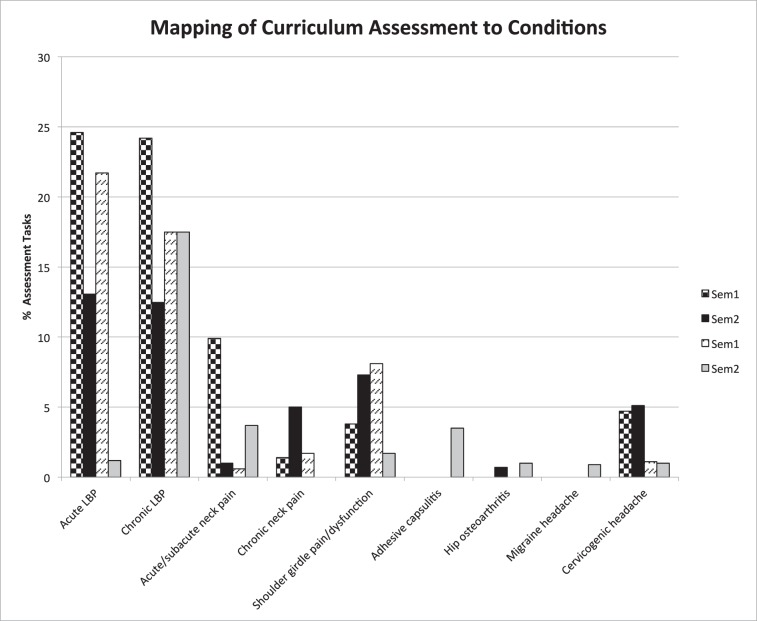
Figure 4 demonstrates a mixed congruence between the conclusions formed by Bronfort24 and the MChir curriculum. Both acute and chronic low back pain are covered extensively within the MChir curriculum, whereas migraine and adhesive capsulitis appear to be neglected. However, this apparent exclusion of adhesive capsulitis may have occurred as other shoulder girdle dysfunction disorders have taken precedence within assessment tasks.
Figure 4.
Mapping to assessment tasks musculoskeletal conditions for which chiropractic treatment was deemed effective in Bronfort et al.24 LBP indicates low back pain.
DISCUSSION
The results demonstrate that assessment tasks within the MChir curriculum are congruent with both the musculoskeletal conditions commonly treated by chiropractors in private practice and those disorders highlighted by Bronfort et al24 for which chiropractic treatment is effective and displays high-quality evidence. Originally, it was proposed that the mapping would use learning outcomes and graduate capabilities. However, it was decided that mapping of the assessment tasks would be more informative, enabling a more comprehensive and detailed analysis of the curriculum. Ideally, to achieve the most accurate and meaningful results, the entire curriculum content should be used rather than the assessment tasks in isolation. This would involve retrospectively listening to all lecture recordings from the past 2 years and cross-referencing this content to the printed lecture notes. This task would be both extremely difficult and time intensive. Consequently, there is some subjectivity in the data presented in Table 1 regarding whether a disorder is covered adequately within the unit to justify its inclusion in the analysis.
There are several limitations for using assessment tasks as representative of the entire curriculum. It is postulated that many of the final theory examinations within the MChir seek to assess an understanding of concepts using specific examples (e.g., the lower limb) rather than simple recall and comprehension. The final practical examinations include, but are not limited to, chiropractic skills, neurological examination, and rehabilitation tracks, in addition to radiographic positioning and analysis. As such, it is important to note that these assessment tasks are testing simultaneously both mastery of skills and integration of theory. The MChir is not simply a content-based degree, and future studies investigating skills acquisition and mastery within the degree should be conducted to provide a more complete analysis of the degree. A clear example of this is found within the clinic internship subjects (CHIR896 and 897), where students learn to integrate theory learned and skills required. It is expected that students will be exposed to a variety of common disorders. However, the limitation to this assumption is the actual case-mix presentation and demographic spectrum to which an intern is exposed.
Although the Bronfort article represents a single paper, it is a systematic literature review and thus holds an elevated standing in the hierarchy of evidence. This suggests that the conclusions offered carry far greater significance than those given by a single paper. In addition to this, the results of the Warwick Review corroborate those of the Bronfort article. It may be noted that Bronfort acknowledges that the evidence surrounding the most common presenting conditions to chiropractors displays significant heterogeneity. This heterogeneity within the literature made it difficult to establish the most common presenting complaints. Initially, there was a 10th category, “other”; however, it was decided to omit this category as it did not add anything further to the study. This topic requires further investigation and research if chiropractors are to be fully accepted within the sphere of medical and health sciences. This being said, the current literature supports the claim that chiropractic is both effective and widely used in the treatment of low back pain, which is reflected by the emphasis placed upon low back pain within the MChir curriculum.24,27–32
CONCLUSION
There is congruence between the assessment tasks within the MChir curriculum and the 2 domains against which it was mapped. Thus, completion of the MChir curriculum provides training relevant to conditions that commonly present to chiropractors and musculoskeletal conditions for which chiropractic treatment is effective. It also highlights that there is a balance between skills acquisition and content-driven learning befitting any primary contact health care practitioner training program. It is hoped this study will provide a foundation for which elements of the chiropractic curriculum can be mapped against each other in addition to the needs of clinicians, their patients, and the profession.
CONFLICTS OF INTEREST
Robyn Beirman and Subramanyam Vemulpad are members of the Macquarie University Department of Chiropractic, and Lindsay Gorrell was a student within this department at the time of the study.
REFERENCES
- 1.Harden R. AMEE Guide No. 21: Curriculum mapping: a tool for transparent and authentic teaching and learning. Med Teach. 2001;23(2):123–137. doi: 10.1080/01421590120036547. [DOI] [PubMed] [Google Scholar]
- 2.English F. Curriculum mapping. Educ Leadership. 1980;37:558–559. [Google Scholar]
- 3.Hege I, Nowak D, Kolb S, Fischer M, Radon K. Developing and analysing a curriculum map in Occupational- and Environmental Medicine. BMC Med Educ. 2010;10(1):60. doi: 10.1186/1472-6920-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobs H. Mapping the Big Picture. Alexandria, VA: Association for Supervision and Curriculum Development; 1997. [Google Scholar]
- 5.Prideaux D. ABC of learning and teaching in medicine. Curriculum design. BMJ. 2003;326:268–270. doi: 10.1136/bmj.326.7383.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haas M, Leo M, Peterson D, LeFebvre R, Vavrek D. Evaluation of the effects of an evidence-based practice curriculum on knowledge, attitudes, and self-assessed skills and behaviors in chiropractic students. J Manipulative Physiol Ther. 2012;35:701–709. doi: 10.1016/j.jmpt.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vermet S, McGinnis K, Boodham M, Gleberzon BJ. Degree of vertical integration between the undergraduate program and clinical internship with respect to lumbopelvic diagnostic and therapeutic procedures taught at the Canadian Memorial Chiropractic College. J Chiropr Educ. 2010;24:46–56. doi: 10.7899/1042-5055-24.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saranchuk RWT. Analysis of the relationship between program design and professional practice in CMCC's undergraduate chiropractic program. J Can Chiropr Assoc. 2000;44:230–244. [Google Scholar]
- 9.Souza T. Differential Diagnosis and Management for the Chiropractor: Protocols and Algorithms. 3rd ed. Burlington, Massachusetts: Jones & Bartlett Publishers; 2005. ed. [Google Scholar]
- 10.Council on Chiropractic Education Australasia. [homepage on the Internet]. Armadale: Council on Chiropractic Education Australasia, Inc; c 2013[cited 2013 Apr 7]. Available from. http://www.ccea.com.au/ [Google Scholar]
- 11.Redwood-Campbell L, Pakes B, Rouleau K, et al. Developing a curriculum framework for global health in family medicine: emerging principles, competencies, and educational approaches. BMC Med Educ. 2011;11:46. doi: 10.1186/1472-6920-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis MH, Harden RM. Planning and implementing an undergraduate medical curriculum: the lessons learned. Med Teach. 2003;25:596–608. doi: 10.1080/0142159032000144383. [DOI] [PubMed] [Google Scholar]
- 13.Willett TG. Current status of curriculum mapping in Canada and the UK. Med Educ. 2008;42:786–793. doi: 10.1111/j.1365-2923.2008.03093.x. [DOI] [PubMed] [Google Scholar]
- 14.Maxwell S, Walley T. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow's doctors. Br J Clin Pharmacol. 2003;55:496–503. doi: 10.1046/j.1365-2125.2003.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Draper B, Walsh M. A survey of graduate perception of undergraduate chiropractic training. Chiropr J Aust. 2008;38:97–103. [Google Scholar]
- 16.Bruno P, Ongaro A, Fraser I. Long-term retention of material taught and examined in chiropractic curricula: its relevance to education and clinical practice. J Can Chiropr Assoc. 2007;51:14. [PMC free article] [PubMed] [Google Scholar]
- 17.Cooley J, Parkin-Smith G, Maire J, Simpson K, Chap P, Nook B. Simulated Learning Environment Chiropractic Curriculum Report Murdoch University. Perth, Australia: Murdoch University; 2011. [Google Scholar]
- 18.Bath D, Smith C, Stein S, Swann R. Beyond mapping and embedding graduate attributes: bringing together quality assurance and action learning to create a validated and living curriculum. High Educ Res Dev. 2004;23:313–328. [Google Scholar]
- 19.Harden RM, Hart IR. An international virtual medical school (IVIMEDS): the future for medical education? Med Teach. 2002;24:261–267. doi: 10.1080/01421590220141008. [DOI] [PubMed] [Google Scholar]
- 20.Harris L, Driscoll P, Lewis M, Matthews L, Russell C, Cumming S. Implementing curriculum evaluation: case study of a generic undergraduate degree in health sciences. Assess Eval High Educ. 2009;35:477–490. [Google Scholar]
- 21.Uchiyama K, Radin J. Curriculum mapping in higher education: a vehicle for collaboration. Innov High Educ. 2009;33:271–280. [Google Scholar]
- 22.Ervin L, Carter B, Robinson P. Curriculum mapping: not as straightforward as it sounds. J Vocat Educ Train. 2013;65:309–318. [Google Scholar]
- 23.Bligh J, Prideaux D, Parsell G. PRISMS: new educational strategies for medical education. Med Educ. 2001;35:520–521. doi: 10.1046/j.1365-2923.2001.00984.x. [DOI] [PubMed] [Google Scholar]
- 24.Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopathy. 2010;18:3. doi: 10.1186/1746-1340-18-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sutcliffe P, Clar C, Tsertsvadze A, et al. Clinical and Cost-Effectiveness of Manual Therapy for the Management of a Variety of Musculoskeletal and Non-musculoskeletal Conditions: A Systematic Review and Narrative Synthesis. Coventry, UK: Warwick Medical School; 2013. [Google Scholar]
- 26.Battat R, Seidman G, Chadi N, et al. Global health competencies and approaches in medical education: a literature review. BMC Med Educ. 2010;10:94. doi: 10.1186/1472-6920-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Airaksinen O, Brox J, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15((suppl 2)):S192–S300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Assendelft W, Morton S, Yu E, Suttorp M, Shekelle P. Spinal manipulative therapy for low back pain. Cochrane Database Syst Rev. 2004: doi: 10.1002/14651858.CD000447.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Bronfort G, Haas M, Evans R, Bouter L. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4:335–356. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine J. 2008;8:213–225. doi: 10.1016/j.spinee.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 31.Chou R, Qaseem A, Snow V, Casey D, Cross J, Shekelle P. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 32.Deyo RA, Weinstein JN. Low Back pain. N Engl J Med. 2001;344:363–370. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]