Abstract
Care providers' adoption of computer-based health-related documentation (“note capture”) tools has been limited, even though such tools have the potential to facilitate information gathering and to promote efficiency of clinical charting. The authors have developed and deployed a computerized note-capture tool that has been made available to end users through a care provider order entry (CPOE) system already in wide use at Vanderbilt. Overall note-capture tool usage between January 1, 1999, and December 31, 2001, increased substantially, both in the number of users and in their frequency of use. This case report is provided as an example of how an existing care provider order entry environment can facilitate clinical end-user adoption of a computer-assisted documentation tool—a concept that may seem counterintuitive to some.
Patients' charts serve as repositories for documenting the presence or absence of clinical findings, medical reasoning, therapies, and general aspects of care delivery.1,2,3 Third parties impose additional demands on clinical record keeping: courts regard patient charts as evidence in legal proceedings4; payers use the quality and quantity of documentation in charts to justify the level of reimbursement for services5; investigators extract elements of medical records for clinical and health services research2,6,7,8,9,10; and computerized patient care systems use electronic chart data as the substrate for clinical decision support.11,12,13,14,15,16,17 Ideally, computer-based tools can increase the capture of patient chart information by prompting clinicians to be more comprehensive and precise in their documentation of clinical encounters. Such systems can improve the quality of care18,19 through more timely availability of structured patient information. However, due to the time pressures of clinical practice and the inconveniences of system-related workflow diversions, clinicians resist forces (such as cumbersome charting systems) that impede direct patient care activities.12,20,21
A key impediment to adoption of many clinical systems in the United States is the lack of routine computer usage in clinicians' typical workflows.22,23 Busy clinicians conserve time and energy by avoiding unnecessary distractions of all types—including use of isolated, time-consuming computer applications such as documentation and decision support systems—even if such tools may improve care delivery.24 Although numerous research and development efforts over the last half century have demonstrated that computer-assisted documentation tools can improve documentation efficiency,25,26,27,28,29,30,31,32 completeness of records,17,33,34,35,36,37 and the quality of patient care provided,14,15,38,39,40,41,42 little has been published documenting adoption rates. While anecdotal reports suggest that proprietary products, such as those by Epic Systems,36 Logician,43 Physician Micro Systems,44 and the Department of Veterans Affairs,45 have had success being adopted as part of comprehensive medical record systems, the general characteristics of successful adoption related to these products have not been well described in the biomedical literature.
Realizing that synergies among electronic health record (EHR) applications may lead to enhanced system usability and adoption, the authors took a novel approach to the development of a clinical note-capture tool (CNCT) by integrating a generic template-driven, computer-assisted documentation system46 into a successful and widely used institutional inpatient care provider order entry (CPOE) system47 that leveraged a clinical data repository48 at Vanderbilt University Medical Center (VUMC). CPOE generally is regarded as difficult to integrate successfully into clinicians' workflow,21,49,50 yet it enhanced implementation of the authors' CNCT system. When the Vanderbilt CNCT was initially developed, VUMC clinicians were already spending a significant amount of time interacting with computers to write orders and to review data related to patients but continued to document their observations either by handwriting notes in the paper chart (for daily progress notes) or by dictating to a transcriptionist (for history and physical documents, consult notes, procedure notes, and discharge summaries). The CNCT deployment not only took advantage of the proximity of clinicians to computers (for CPOE) to encourage voluntary adoption, but also leveraged key components of CPOE per se to facilitate the process.
Observations
VUMC CNCT Implementation History
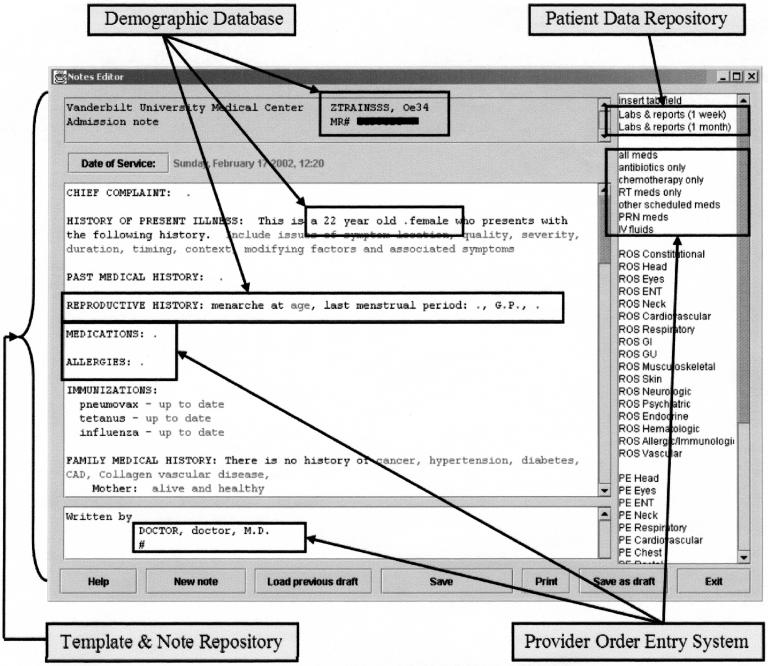
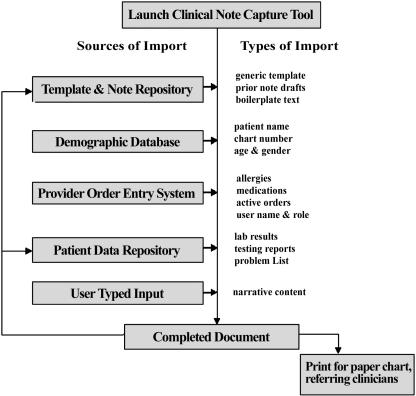
Shortly after the first major deployment of the institutional inpatient CPOE system in 1995, system developers created a primitive CNCT (a simple text editor launched exclusively from within the CPOE system, and containing only one template for progress notes, consisting only of an “S,” an “O,” an “A,” and a “P” on separate lines,51 and one template for history and physical examination documentation) to meet the needs of a clinician who had been instrumental in early CPOE testing. After a year of limited usage, during which time the existence of the CNCT tool was not advertised, an internal medicine resident found a colleague's CNCT-based clinical note in a patient chart and decided to develop additional CNCT capabilities. In a simple user interface (▶), CNCT users could edit and modify semistructured note outlines generated from existing templates by typing or “pasting” text freehand or from categorical lists of predefined text. The resident wrote dozens of templates to assist in his own and his colleagues' progress note generation and worked with the CPOE system developers to adapt CPOE components for general clinical documentation needs. CPOE data elements made available in CNCT, including patient name, gender, age, laboratory results, allergies, and inpatient medications, permitted manual or automated importing into the clinical note at user discretion (▶). Data sources for these elements included both CPOE and linked EHR applications. Imported information could be left unchanged or user-edited to meet the needs of the document being generated (as might occur if the CNCT were to import the list of inpatient medications from CPOE into a history and physical examination note, which generally delineates outpatient medications; in this way the user could document outpatient medications by changing the inpatient list rather than typing the entire outpatient list manually). Users could save drafts of a note to a central server for completion during a subsequent session, or to use as a starting point for subsequent notes on the same patient. This core set of features has remained stable over time.
Figure 1.
The notes editor interface with a template automatically modified into a note outline from four different data sources for a 22-year-old woman.
Figure 2.
The integration of the clinical note-capture tool (CNCT) with other institutional information systems. After launching the CNCT, the user selects either a template or a previous note draft from the template repository. The CNCT then modifies the template into a note outline that includes demographic information and age-/gender-specific content and content from the provider order entry system. The user then can augment the note by typing and by initiating unidirectional queries of the data repository for additional information, such as laboratory results and problem lists. Once completed, the note can be stored in the data repository and printed for inclusion in a paper chart.
Six months after the internal medicine resident adopted the CNCT, an attending obstetrician/gynecologist was attracted by the ease of using the CNCT to generate documents with large amounts of standard text and also began to develop a series of templates that outlined his standard operative narratives. Both clinicians adopted the CNCT for much of their clinical documentation needs and then began to champion its use among colleagues. Use of the CNCT at VUMC remains strictly voluntary; there are no administrative mandates or direct incentives promoting its use among clinicians.
Templates have long been used for clinical data collection52,53,54 and in EHR documentation systems.14,26,28,38,42,45,55,56,57,58,59,60 Similar to the description of “documentation templates” in electronic medical records by Yamazaki et al.,55,61 the VUMC CNCT templates consisted of easily read and edited plain-text files marked up with simple (XML-like) tags for document sections (header, body, footer); prompts for run-time end-user input; and markers for potential sites of insertion, formatting, and conditional logic. The tags allow the template designer to include user and patient attributes, such as patient age and gender. Templates by subspecialty practice type were developed for history and physical examination documents, progress notes, procedural notes, discharge summaries, and consent forms.
Results
CNCT Use at VUMC
From January 1999 through December 2001, a total of 67,632 patients contributed 96,440 admissions and 497,170 patient-days to VUMC without trends in the rates of monthly admissions, patient hospital days, patient gender, or in-hospital deaths. During this period, 1,838 care providers used the CNCT to create 192,141 notes for about 36,150 individual patients. Over the same period, the number of CNCT templates increased from 59 to 87, and the number of distinct CNCT users increased from 923 the first year and 1,003 in the second, to 1,182 in the third. Rates of CNCT use rose from 941 notes written on 193 patients per week at the beginning of the observation period to 1,518 notes written on 268 patients per week by the end. ▶ summarizes the numbers of notes written, categorized by template types and user clinical roles. Among physician users, 811 (79%) were housestaff, and 213 (21%) were attending physicians; 15% of attending physicians were surgeons, anesthesiologists, and gynecologists who carried out procedure-oriented interventions.
Table 1.
Notes Written by Template and User Categories
| CNCT Notes | CNCT Templates | Dictated Notes* | |
|---|---|---|---|
| Template category | |||
| Daily progress | 114,697 (59.6%) | 25 (30%) | NA |
| History and physical | 22,301 (11.6%) | 11 (13%) | 27,666 |
| Consultation | 18,868 (9.8%) | 6 (7%) | 11,644 |
| Procedure narrative | 14,935 (7.7%) | 8 (10%) | 103,951 |
| Discharge summary | 13,224 (6.8%) | 12 (15%) | 78,667 |
| Outpatient | 5,775 (3.0%) | 17 (21%) | NA |
| Contract | 2,341 (1.2%) | 3 (4%) | NA |
| Total |
192,141 |
82 |
221,928* |
| CNCT Notes |
CNCT Users |
CNCT Nonusers† |
|
| User category | |||
| Physician | 156,582 (81.5%) | 1,024 (55.7%) | 1,382 |
| Medical student | 20,080 (10.5%) | 472 (25.7%) | 179 |
| Nurse | 1,694 (0.9%) | 184 (10.0%) | 2,534 |
| Nurse practitioner | 4,876 (2.5%) | 32 (1.7%) | 17 |
| Dietitian | 2,886 (1.5%) | 30 (1.6%) | 56 |
| Case manager | 338 (0.2%) | 25 (1.4%) | 42 |
| Medical receptionist | 36 ( < 0.1%) | 23 (1.3) | 386 |
| Pharmacist | 5,407 (2.8%) | 18 (1.0%) | 79 |
| Other‡ | 242 (0.1%) | 30 (1.6%) | NA |
| Total | 192,141 | 1,838 | 4,675 |
NA = data unavailable.
Excludes daily progress notes, outpatient notes, consultation follow-up notes, and contracts, which are not dictated at our institution. Not all Vanderbilt University Medical Center admissions require discharge summaries or typed history and physical examination documents.
Clinicians who accessed the CPOE and EHR systems but did not use the CNCT during the observation period.
Includes respiratory, physical and occupational therapists, and patient care technicians.
Use of the CNCT was not evenly distributed across all clinicians; 4.7% (88) of users in the top percentile for note writing during at least one of the three study years generated 30.2% (58,147) of all notes written. Among the top users, 91% (80) were physicians, with others including nurse practitioners, dietitians, and pharmacists. Six users (0.3% of all users), all physicians consistently in the 99th percentile of note writing, wrote 6.2% of all notes; they included three pediatric oncologists and one general pediatrician who used the CNCT primarily for progress notes, one obstetrician/gynecologist who used the CNCT primarily for operative notes, and one internal medicine resident who had completed training and moved at the time of this evaluation.
A survey of the four remaining highest-volume CNCT users (of the top five historically) asked, “… why you have used this notewriter, how it has impacted your practice, and what needs to be changed better to suit your needs?” All respondents cited as beneficial the form-like template structure, including “the ability to pick and choose my templates which most closely match the admission or the operation provides even more time savings, and another safety net for information retrieval and presentation.” Three respondents appreciated the ability of CNCT to reuse notes and note components, including “calling up prior day's progress note draft allows one to revise without major changes,” and “it was very nice to have already a note with PMHx, FHx.” Two respondents liked the ability of the note-capture tool to import data easily from other information systems: “contains more useful information, e.g., meds, … labs, cultures.” Additionally, three respondents stated that a computer-generated note enhances the legibility of their documentation, while two stated that the process of navigating into the note-capture tool was too complex. Respondents recommended changes to the note-capture tool to make it more closely fit workflow, including improving the efficiency of the template selection, increasing the number of computer terminals available for documentation, integrating a spell checker, and deploying flat screen and touch screen monitors.
Discussion
Lessons Learned
A CNCT was integrated into a workflow that included a successful CPOE system at VUMC. Incorporating note capture into order entry allowed busy health care providers to write clinical notes while simultaneously entering patient orders; there was no need to sign on to separate systems or use different computer terminals. For example, using the integrated systems, a clinician could write admission orders and an admitting history and physical examination summary at the same time and from the same computer program. Merged systems also permitted patient-specific clinical content to be shared between applications so that orders and patient demographic data entered into CPOE were available for automatic insertion into CNCT-assisted clinical notes. Assembling both processes into a single computer system and workflow decreased the effort required for clinicians to access the CNCT and the time required to generate notes. Clinicians used the note-capture tool voluntarily for a variety of documentation needs, including inpatient progress notes, admission history and physical examination records, and operative narratives. The authors believe that specific features of concurrent CPOE usage enhanced CNCT adoption: the ability to prefill highly customizable task-oriented templates with patient- and user-specific information such as provider name and clinical role, current medications list, current laboratory test results, patient demographic information, allergy lists, and other data drawn from existing electronic resources. Users could easily modify prefilled templates through simple typed entry, facile insertion of additional boilerplate text, or importation of additional patient data from other systems. The tool also permitted notes generated during one encounter to be reused on subsequent encounters, further simplifying the process of documentation for situations in which the patient's case remains stable over time. Adoption, as measured by the rates of notes written, number of users of the system, and number of templates, increased substantially over time.
Template-based CNCT systems would be expected to be useful for procedural narratives, where the procedure and its documentation vary little from case to case. Our results show that less than 10% of available templates and written notes documented procedures. Only 15% of the attending physician users had a procedural (e.g., surgery or anesthesia) subspecialty focus, although one of the top users, an obstetrician/gynecologist, used the CNCT primarily to document his operative notes. Furthermore, the CNCT was used as an alternative to dictation for procedure notes less than for history and physical examination notes, consultation notes, or discharge summaries. It is unclear from the data whether the limited adoption of the CNCT among proceduralists resulted from inadequate templates, a high degree of variability in operative techniques (which would make them less amenable to templated documentation), or relatively lower penetration of computerized systems in their clinical workflow.
The authors believe that during clinical practice, health care providers will be best served by a spectrum, rather than a monolithic type, of electronic note-capture mechanisms. The mechanisms can be categorized according to the machine readability of their content, including handwritten notes scanned into computers and made available as images; free-text notes typed or transcribed into a computer-readable format; semistructured template-based notes of the type described in this report; and fully structured, more meticulously captured coded notes such as those already provided by many vendor systems (e.g., Logician by General Electric, EpicCare by Epic Systems, and elements of Practice Partner software from Physician Micro Systems). Relevant strengths and weaknesses of each note-capture mechanism vary. Fully structured coded notes, for example, facilitate data collection for research and real-time decision support but can be cumbersome to use during patient encounters and may lack the flexibility and expressivity required for general medical practices. Handwritten notes, by contrast, are extremely flexible and permit a high degree of expressivity but may be limited in their legibility and accessibility for data processing and analysis. Transcribed notes permit facile documentation into a format possibly useful for machine-based natural language processing for content extraction and summarization but are expensive to produce and require a time delay for the transcription process to occur. It is likely that each note-capture mechanism will find a clinical niche, with different clinicians and different sites each using the type that best fits the practice situation of the moment and that will vary during the course of a day.
Inpatient Setting of Study
The primarily inpatient focus of the CNCT warrants explanation. At the time of the initial development and observation periods, most CPOE and EHR systems at VUMC were deployed in the inpatient environment. Creating a CNCT as an extension of CPOE logically focused on inpatient documentation. As a result, the bulk of outpatient CNCT use consisted of documentation of admitting history and physical examinations (recording the transition from outpatient to inpatient settings). Relevant outpatient information, such as lists of problems, past procedures, and outpatient medications, was not available for import into the CNCT during the observation period, and inpatient information imported into notes that generally record outpatient histories required manual user editing. It is possible that increasing the ability of the CNCT to import more outpatient information from the EHR and the existence of an outpatient CPOE system would make the CNCT more useful for outpatient documentation.
Limitations of the Study
This report has limitations that merit discussion. First, the authors did not perform a separate analysis correlating either CPOE usage or computer literacy with CNCT usage. It is possible that adopters were drawn to the CNCT by its templates, by its availability on widely available computers throughout the hospital, or by their own preferences for using computerized tools, rather than by its integration into an existing workflow that included CPOE. Second, development and evaluation of the Vanderbilt CNCT have historically targeted inpatient documentation, and only a small proportion of notes were written using outpatient-specific templates. User adoption of outpatient documentation tools may have different requirements than adoption of inpatient documentation tools. Third, this report describes the deployment of a single CNCT into a CPOE system at a single academic medical center. Because CPOE is neither ubiquitously used nor uniformly installed in all health care settings, it is possible that attempts to integrate note capture into order entry at different institutions would not be successful.
The authors recommend that other developers consider the benefits of cross-system synergy when implementing clinical note-capture tools.
Presented as a poster at the American Medical Informatics Association Annual Symposium, San Antonio, TX, November 2002: Rosenbloom ST, Grande J. Integrating medical documentation into provider order entry. Proc. AMIA Symp. 2002:1143.
The authors are indebted to Dr. Kevin B. Johnson for his assistance and advice in preparing the manuscript.
References
- 1.Engle RL, Jr. The evolution, uses, and present problems of the patient's medical record as exemplified by the records of the New York Hospital from 1793 to the present. Trans Am Clin Climatol Assoc. 1990;102:182–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Weed LL. Quality control and the medical record. Arch Intern Med. 1971;127:101–5. [PubMed] [Google Scholar]
- 3.DeGowin EL, DeGowin RL. Bedside diagnostic examination. New York: Macmillan, 1969, pp xii, 923
- 4.Holder AR. The importance of medical records. JAMA. 1974;228:118–9. [DOI] [PubMed] [Google Scholar]
- 5.1995 Documentation Guidelines for Evaluation & Management Services. Washington, DC: Centers for Medicare & Medicaid Services, 1995.
- 6.Solomon DH, Schaffer JL, Katz JN, et al. Can history and physical examination be used as markers of quality? An analysis of the initial visit note in musculoskeletal care. Med Care. 2000;38:383–91. [DOI] [PubMed] [Google Scholar]
- 7.Hershberg PI, Goldfinger SE, Lemon FR, Fessel WJ. Medical record as index of quality of care. N Engl J Med. 1972;286:725–6. [DOI] [PubMed] [Google Scholar]
- 8.Fessel WJ, Van Brunt EE. Assessing quality of care from the medical record. N Engl J Med. 1972;286:134–8. [DOI] [PubMed] [Google Scholar]
- 9.Murphy JG, Jacobson S. Assessing the quality of emergency care: the medical record versus patient outcome. Ann Emerg Med. 1984;13:158–65. [DOI] [PubMed] [Google Scholar]
- 10.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–45. [DOI] [PubMed] [Google Scholar]
- 11.Wagner MM, Bankowitz RA, McNeil M, Challinor SM, Jankosky JE, Miller RA. The diagnostic importance of the history and physical examination as determined by the use of a medical decision support system. Symp Comput Appl Med Care. 1989:139–44.
- 12.Davis LS, Collen MF, Rubin L, Van Brunt EE. Computer-stored medical record. Comput Biomed Res. 1968;1:452–69. [DOI] [PubMed] [Google Scholar]
- 13.Hammond WE, Stead WW, Straube MJ, Jelovsek FR. Functional characteristics of a computerized medical record. Methods Inf Med. 1980;19:157–62. [PubMed] [Google Scholar]
- 14.Schriger DL, Baraff LJ, Rogers WH, Cretin S. Implementation of clinical guidelines using a computer charting system. Effect on the initial care of health care workers exposed to body fluids. JAMA. 1997;278:1585–90. [PubMed] [Google Scholar]
- 15.Schriger DL, Baraff LJ, Buller K, et al. Implementation of clinical guidelines via a computer charting system: effect on the care of febrile children less than three years of age. J Am Med Inform Assoc. 2000;7:186–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown SH, Lincoln M, Hardenbrook S, et al. Derivation and evaluation of a document-naming nomenclature. J Am Med Inform Assoc. 2001;8:379–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kent DL, Shortliffe EH, Carlson RW, Bischoff MB, Jacobs CD. Improvements in data collection through physician use of a computer-based chemotherapy treatment consultant. J Clin Oncol. 1985;3:1409–17. [DOI] [PubMed] [Google Scholar]
- 18.Committee on Improving the Patient Record The Computer-Based Patient Record: An Essential Technology for Health Care, 2 ed.. Washington, DC: Institute of Medicine, 1991.
- 19.Committee on Quality of Health Care in America Using Information Technology. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Institute of Medicine, 2001, pp 175–92
- 20.Garrett LE, JrHammond WE, Stead WW. The effects of computerized medical records on provider efficiency and quality of care. Methods Inf Med. 1986;25:151–7. [PubMed] [Google Scholar]
- 21.Bates DW, Boyle DL, Teich JM. Impact of computerized physician order entry on physician time. Proc Annu Symp Comput Appl Med Care. 996;1994:. [PMC free article] [PubMed] [Google Scholar]
- 22.Rotich JK, Hannan TJ, Smith FE, et al. Installing and implementing a computer-based patient record system in sub-Saharan Africa: the Mosoriot Medical Record System. J Am Med Inform Assoc. 2003;10:295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shortliffe EH. The adolescence of AI in medicine: will the field come of age in the '90s?. Artif Intell Med. 1993;5:93–106. [DOI] [PubMed] [Google Scholar]
- 24.Miller RA, Masarie FE, Jr The demise of the “Greek Oracle” model for medical diagnostic systems. Methods Inf Med. 1990;29:1–2. [PubMed] [Google Scholar]
- 25.Ledley RS. Computer aids to medical diagnosis. JAMA. 1966;196:933–43. [PubMed] [Google Scholar]
- 26.Slack WV, Hicks GP, Reed CE, Van Cura LJ. A computer-based medical-history system. N Engl J Med. 1966;274:194–8. [DOI] [PubMed] [Google Scholar]
- 27.Slack WV, Peckham BM, Van Cura LJ, Carr WF. A computer-based physical examination system. JAMA. 1967;200:224–8. [PubMed] [Google Scholar]
- 28.Stead WW, Heyman A, Thompson HK, Hammond WE. Computer-assisted interview of patients with functional headache. Arch Intern Med. 1972;129:950–5. [PubMed] [Google Scholar]
- 29.Ash SR, Mertz SL, Ulrich DK. The Computerized Notation System (CNS). A microcomputer system for rapid entry of notes by physicians and nurses. J Med Syst. 1983;7:193–203. [DOI] [PubMed] [Google Scholar]
- 30.Ash SR, Mertz SL, Ulrich DK. The computerized notation system: a portable, self-contained system for entry of physicians' and nurses' notes. J Clin Eng. 1983;8:147–55. [DOI] [PubMed] [Google Scholar]
- 31.Andrews RD, Gardner RM, Metcalf SM, Simmons D. Computer charting: an evaluation of a respiratory care computer system. Respir Care. 1985;30:695–707. [PubMed] [Google Scholar]
- 32.Karliczek GF, de Geus AF, Wiersma G, Oosterhaven S, Jenkins I. Carola, a computer system for automatic documentation in anesthesia. Int J Clin Monit Comput. 1987;4:211–21. [DOI] [PubMed] [Google Scholar]
- 33.Lloyd SC. Computer-generated progress notes in an automated POMR. J Med Syst. 1984;8:35–42. [DOI] [PubMed] [Google Scholar]
- 34.Stratmann WC, Goldberg AS, Haugh LD. The utility for audit of manual and computerized problem-oriented medical record systems. Health Serv Res. 1982;17:5–26. [PMC free article] [PubMed] [Google Scholar]
- 35.Tang PC, LaRosa MP, Gorden SM. Use of computer-based records, completeness of documentation, and appropriateness of documented clinical decisions. J Am Med Inform Assoc. 1999;6:245–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Epic Systems Corporation. Available at: <http://www.epicsys.com/>. Accessed February 2004.
- 37.Humphreys T, Shofer FS, Jacobson S, Coutifaris C, Stemhagen A. Preformatted charts improve documentation in the emergency department. Ann Emerg Med. 1992;21:534–40. [DOI] [PubMed] [Google Scholar]
- 38.Barnett GO. COSTAR, a computer-based medical information system for ambulatory care. Proc IEEE. 1979;67:1226–37. [Google Scholar]
- 39.Wirtschafter DD, Scalise M, Henke C, Gams RA. Do information systems improve the quality of clinical research? Results of a randomized trial in a cooperative multi-institutional cancer group. Comput Biomed Res. 1981;14:78–90. [DOI] [PubMed] [Google Scholar]
- 40.Shortliffe EH. Update on ONCOCIN: a chemotherapy advisor for clinical oncology. Med Inform (Lond). 1986;11:19–21. [DOI] [PubMed] [Google Scholar]
- 41.Smith SA, Murphy ME, Huschka TR, et al. Impact of a diabetes electronic management system on the care of patients seen in a subspecialty diabetes clinic. Diabetes Care. 1998;21:972–6. [DOI] [PubMed] [Google Scholar]
- 42.Musen MA, Carlson RW, Fagan LM, Deresinski SC, Shortliffe EH. T-HELPER: automated support for community-based clinical research. Proc Annu Symp Comput Appl Med Care. 1992:719–23. [PMC free article] [PubMed]
- 43.Logician Ambulatory. Available at: <http://www.gemedicalsystems.com/it_solutions/clinical/logician.html>. Accessed February 2004.
- 44.Physician Micro Systems, Incorporated: Practice Partner Patient Records. Available at: <http://www.pmsi.com/pr/patientrecordsfeatures.htm>. Accessed February 2004.
- 45.Brown SH, Hardenbrook S, Herrick L, St Onge J, Bailey K, Elkin PL. Usability evaluation of the progress note construction set. Proc AMIA Symp. 2001:76–80. [PMC free article] [PubMed]
- 46.Rosenbloom ST, Grande J. Integrating medical documentation into provider order entry. Proc AMIA Annu Fall Symp. 1143;2002:. [Google Scholar]
- 47.Geissbuhler A, Miller RA. A new approach to the implementation of direct care-provider order entry. Proc AMIA Annu Fall Symp. 1996:689–93. [PMC free article] [PubMed]
- 48.Giuse DA, Mickish A. Increasing the availability of the computerized patient record. Proc AMIA Annu Fall Symp. 1996:633–7. [PMC free article] [PubMed]
- 49.Ash JS, Lyman J, Carpenter J, Fournier L, A diffusion of innovations model of physician order entry. Proc AMIA Symp. 2001:22–6. [PMC free article] [PubMed]
- 50.Ash JS, Gorman PN, Lavelle M, et al. A cross-site qualitative study of physician order entry. J Am Med Inform Assoc. 2003;10:188–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weed LJ. The problem oriented record as a basic tool in medical education, patient care and clinical research. Ann Clin Res. 1971;3:131–4. [PubMed] [Google Scholar]
- 52.Marill KA, Gauharou ES, Nelson BK, Peterson MA, Curtis RL, Gonzalez MR. Prospective, randomized trial of template-assisted versus undirected written recording of physician records in the emergency department. Ann Emerg Med. 1999;33:500–9. [DOI] [PubMed] [Google Scholar]
- 53.Weed L. The problem-oriented record—its organizing principles and its structure. League Exch. 1975;103:3–6. [PubMed] [Google Scholar]
- 54.Palmer IP, Baskett PJ, McCabe SE. A new chart to assist with advanced trauma life support. J R Army Med Corps. 1992;138:118–25. [DOI] [PubMed] [Google Scholar]
- 55.Yamazaki S, Satomura Y. Standard method for describing an electronic patient record template: application of XML to share domain knowledge. Methods Inf Med. 2000;39:50–5. [PubMed] [Google Scholar]
- 56.Poon AD, Fagan LM, Shortliffe EH. The PEN-Ivory project: exploring user-interface design for the selection of items from large controlled vocabularies of medicine. J Am Med Inform Assoc. 1996;3:168–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maultsby MC, JrSlack WV. A computer-based psychiatry history system. Arch Gen Psychiatry. 1971;25:570–2. [DOI] [PubMed] [Google Scholar]
- 58.Johnson KB, Cowan J. Clictate: a computer-based documentation tool for guideline-based care. J Med Syst. 2002;26:47–60. [DOI] [PubMed] [Google Scholar]
- 59.Gordon BL. Regularization and stylization of medical records. JAMA. 1970;212:1502–7. [PubMed] [Google Scholar]
- 60.Chin HL, Krall M. Implementation of a comprehensive computer-based patient record system in Kaiser Permanente's Northwest Region. MD Comput. 1997;14:41–5. [PubMed] [Google Scholar]
- 61.Yamazaki S, Satomura Y, Suzuki T, Arai K, Honda M, Takabayashi K. The concept of “template” assisted electronic medical record. Medinfo. 1995;8(pt 1):249–52. [PubMed] [Google Scholar]