Abstract
Objectives
To investigate the underlying causes of intravenous medication administration errors (MAEs) in National Health Service (NHS) hospitals.
Setting
Two NHS teaching hospitals in the North West of England.
Participants
Twenty nurses working in a range of inpatient clinical environments were identified and recruited using purposive sampling at each study site.
Primary outcome measures
Semistructured interviews were conducted with nurse participants using the critical incident technique, where they were asked to discuss perceived causes of intravenous MAEs that they had been directly involved with. Transcribed interviews were analysed using the Framework approach and emerging themes were categorised according to Reason's model of accident causation.
Results
In total, 21 intravenous MAEs were discussed containing 23 individual active failures which included slips and lapses (n=11), mistakes (n=8) and deliberate violations of policy (n=4). Each active failure was associated with a range of error and violation provoking conditions. The working environment was implicated when nurses lacked healthcare team support and/or were exposed to a perceived increased workload during ward rounds, shift changes or emergencies. Nurses frequently reported that the quality of intravenous dose-checking activities was compromised due to high perceived workload and working relationships. Nurses described using approaches such as subconscious functioning and prioritising to manage their duties, which at times contributed to errors.
Conclusions
Complex interactions between active and latent failures can lead to intravenous MAEs in hospitals. Future interventions may need to be multimodal in design in order to mitigate these risks and reduce the burden of intravenous MAEs.
Keywords: QUALITATIVE RESEARCH
Strengths and limitations of this study.
This is the first study to use qualitative interviewing with the critical incident technique to explore the underlying causes of intravenous medication administration errors (MAEs) in UK hospitals.
Using human error theory, different active failures were found to be associated with their own combination of errors and violations provoking conditions concerning the patient, tasks, healthcare team, individual nurse, related equipment and working environment.
A unique insight into everyday practice was revealed when nurses, in particular, reported that problems with dose-checking activities, the work mentality they adopted to meet the demands of their role, and lack of support or high workload at important time periods contributed to their work errors.
Theory-based recommendations for interventions designed to minimise intravenous MAEs in hospitals have been suggested.
While the sample size may limit representativeness of findings to other healthcare settings, we included a range of nurses working in different environments and data saturation was achieved.
Introduction
Median estimates show that between 5.1–12.8% of hospital admissions1 and 1.8% of hospitalised patients2 are affected by preventable adverse drug events (ADEs). Medication errors (MEs) are a key contributor to ADEs, and commonly affect the prescribing and administration stages.3 Medication administration errors (MAEs) can be defined as ‘a deviation from the prescriber's medication order as written on the patient's chart, manufacturers’ preparation/administration instructions, or relevant institutional policies’, and affect a median of 19.1% of total opportunities for error (TOE) in hospitals,4 with error rates varying according to study methods, definitions and settings.4 5 Those responsible for drug administration may also inherit MEs arising from earlier medication use stages (eg, prescribing).3 6
MAEs affecting the intravenous route of administration appear much more frequent than for non-intravenous routes. A recent systematic review found that MAEs affected a median 85.9% (IQR 81.8–89.9%) of intravenous TOE in healthcare settings.4 It has been estimated that the probability of making at least one MAE in intravenous doses is 73%7 and that intravenous doses are five times more likely to be associated with a MAE than non-intravenous doses.5 Patient harm associated with intravenous MEs is known to be much greater than for other errors.8
Understanding the underlying causes of MAEs is important for the design and implementation of successful remedial interventions9 especially given the limited impact of those tested so far.10 Despite the high prevalence of MAEs in hospitals, few have concentrated on studying their causes,9 11–14 with only two focusing solely on intravenous MAEs.11 12 Both of these studies used direct observation of medicines administration and brief conversations with individuals as their data collection method, which when compared with in-depth interviews limits detailed investigation of underlying intent or mental processes.9 11 Studies reporting available data on intravenous MAE causes cite contributory factors, including high workload/rushing,11–13 poor supervision,11 knowledge and training deficiencies, distractions and interruptions, inadequate communication and policies/procedures, sharing bad practices, lack of intravenous access for individual patients and deficiencies in the design of related equipment.11 12
This study aimed to use the critical incident technique (CIT) within semistructured interviews to investigate the underlying causes of intravenous MAEs in two National Health Service (NHS) hospitals.
Methods
Setting and recruitment
Nurses were recruited between June 2012 and August 2013 and worked in two NHS teaching hospitals in the North West of England. Eligible nurses could work in ward-based or theatre-based environments provided they were willing to discuss the causes of at least one intravenous MAE that they had been directly involved with.
Study contacts at each participating hospital distributed information about the study to nursing staff working on wards where intravenous medicines were administered frequently. Each interested nurse was given a study pack containing a letter of invitation, participant information leaflet and preinterview questionnaire, and interviews were arranged once they returned the questionnaire to RNK. Participants were reassured that all outputs would be anonymised before providing written informed consent at each interview.
Data collection
Face-to-face semistructured interviews were conducted by RNK, with each nurse participant in hospitals using the CIT.15 A summary of the interview guide can be found in box 1. The CIT has been used to collect empirical data on the causes of MEs16 17 and explores problems by focusing on the intentions, behaviours and actions of those involved in specific situations, as opposed to estimations or generalisations.15 These characteristics made the CIT a more useful data collection tool when compared with in-depth interviewing, as it enabled high-quality relevant data to be gathered from the busy nursing staff.
Box 1. Summary of interview guide.
Part one: background
Training background (including intravenous medication administration)
Years qualified as a nurse
Area of practice
Part two: the intravenous medication administration error
Error details (medication involved, error type, how was error discovered, did the error reach the patient)
Circumstances at time of error (eg, day of week, time of day, who else involved, location, physical/mental health, general workload, level of supervision, patient factors)
Reasons for the error
Part three: reflecting on the error
Changes to personal practice following the error
Prevention of incident (what might have been put in place)
An interview guide was constructed based on the principles of the CIT and previous work investigating prescribing errors,16 with only minor typographical changes being made after piloting at one study site. Background demographic information was collected before participants were asked to recall MAE(s) in detail (including nature and circumstances surrounding the MAE and perceived underlying causes). Nurses were invited to discuss both MAEs that reached the patient, and errors that were caught and rectified before administration.
Categorisation of MAEs was based on established definitions,4 9 11 18 with labelling errors considered as ‘wrong preparation errors’. Interviews lasted for 26–60 min and were conducted in private rooms at each hospital. Interviews were audio recorded and transcribed verbatim.
Data analysis
Interview transcripts were coded and analysed using the NVivo computer software programme (V.10) according to the Framework analysis approach.19 Framework analysis has been used in applied social research since the 1980's to understand human behaviour and has recently found favour in healthcare research due to its rigorous, transparent and systematic approach to qualitative data management and analysis.19 20
Reason's21 22 model of accident causation was used to inform the generation of themes within the Framework approach based on a priori knowledge9 and emerging data from the interviews, and is summarised in box 2 and figure 1. This model has been used elsewhere to study causes of MEs.9 16 17 23 24 Data were coded as active failures and latent failures, including error and violation provoking conditions and high-level organisational decisions. The coding accuracy of each active failure was checked by a second author (SDW, JC and DMA), and the reliability of the coding framework was confirmed using two authors (SDW and JC), who independently extracted and analysed data for 10 interviews.
Box 2. Reason's21 22 model of accident causation.
In this model accidents such as intravenous medication administration errors (MAEs) arise when defensive barriers which protect medication administration processes from subversion are compromised. This can result from the actions or omissions of those on the front lines (eg, nurses), which are called active failures, as well as latent failures affecting the wider system in which they work. Latent failures arise primarily from decisions at a higher organisational level (eg, hospital managers) which may be flawed, influenced by wider goals or limited by regulatory or financial constraints. These decisions can weaken defences while also influencing the working conditions of healthcare staff such as nurses to make them more hazardous, thereby creating error and violation provoking conditions (see figure 1). Latent failures do not immediately lead to accidents; instead they lie dormant for long periods of time and may only be revealed when they combine with active failures in particular circumstances to cause accidents.
Active failures can be categorised at the operator level:
- Execution failures (plan is adequate to achieve outcome, but failure in execution):
- Slips (observable actions and often associated with attention failures),
- Lapses (internal events, often involving memory failure).
- Mistakes (plan is inadequate to achieve intended outcome, failures in problem solving):
- Knowledge based (cannot use prior experience to solve a novel problem),
- Rule based (misapply/omit a good rule or successfully apply a bad rule to solve a trained for problem).
- Violations (intentional deviations from recommended practice (eg, clinical procedures)):
- Routine (eg, cutting corners as habitual behaviour),
- Optimising (furthering personal rather task-orientated goals),
- Necessary (violation essential to perform task appropriately).
Although active failures may occur frequently their effects on defences are immediate and short lived; however the presence of any latent failures increases their frequency and the likelihood that their effects cause an accident such as an intravenous MAE to occur.
Figure 1.
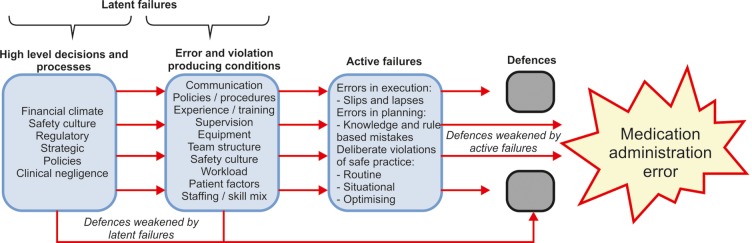
Reason's model of accident causation as applied to medication administration error research.
Results
Twenty nurses were interviewed and 21 individual intravenous MAEs were discussed (see table 1). The MAEs contained descriptions of 23 active failures, of which 8 were mistakes (5 knowledge based and 3 rule based), 7 were slips, 4 were lapses and 4 were deliberate violations of policy. Six different error and violation provoking conditions were identified: problems with the patient; the individual nurse; the task of drug administration; the healthcare team; the working environment and relevant equipment. Latent conditions were discussed as wider organisational decisions.
Table 1.
Summary of study participants and reported intravenous MAEs
| Participant code | Gender | Years since qualification* | Environment at time of MAE | Type of MAE | Did the error reach the patient | Medication class | Active failure(s) |
|---|---|---|---|---|---|---|---|
| N01 | F | 0–4 | Ward | Wrong rate | Yes | Respiratory | Slip |
| N02 | F | 5–9 | Ward | Wrong dose | Yes | Cardiovascular | KBM |
| N03 | M | 0–4 | Ward | Wrong drug†‡ | Yes | Antimicrobial | Violation |
| N04 | F | 0–4 | Ward | Wrong dose | Yes | Endocrine | Slip |
| N05 | F | 10+ | Ward | Wrong rate | Yes | Electrolyte | Slip |
| N06 | F | 0–4 | Ward | Wrong rate | Yes | Cardiovascular | KBM |
| N07 | F | 5–9 | Ward | Wrong rate | Yes | Antimicrobial | KBM |
| 0–4 | Ward | Wrong administration technique | Yes | Cardiovascular | Lapse | ||
| N08 | F | 0–4 | Ward | Wrong drug‡ | Yes | Antimicrobial | Lapse |
| N09 | F | 0–4 | Ward | Wrong rate | Yes | Respiratory | Slip |
| N10 | F | 0–4 | Ward | Wrong dose† | No | Cardiovascular | KBM |
| N11 | M | 5–9 | Ward | Wrong drug†‡ | Yes | Antimicrobial | Violation |
| N12 | F | 0–4 | Theatre | Wrong preparation§¶ | Yes | CNS | Violation (×2) |
| N13 | M | 10+ | Ward | Wrong preparation | Yes | Antimicrobial | KBM |
| N14 | F | 10+ | Ward | Unordered drugठ| Yes | Endocrine | Slip |
| N15 | F | 10+ | Ward | Extra dose†‡§ | Yes | CNS | RBM |
| N16 | F | 0–4 | Ward | Wrong rate | Yes | Antimicrobial | Slip |
| N17 | F | 10+ | Ward | Wrong preparation¶ | Yes | Cardiovascular | Lapse |
| N18 | F | 5–9 | Ward | Wrong rate | Yes | Cardiovascular | RBM |
| N19 | F | 10+ | Theatre | Wrong preparation§¶ | Yes | CNS | Slip, RBM |
| N20 | F | 10+ | Theatre | Wrong dose | Yes | Cardiovascular | Lapse |
*Number of years after qualified/licensed as a nurse that intravenous MAE occurred.
†Indicates occasions where nurses prepared and/or administered prescribing errors (eg, poorly written prescription).
‡Wrong drug, wrong patient, unordered drug and extra dose errors are considered ‘unauthorised drug errors’.
§Indicates occasions where a complex chain of events involving different professional groups was involved.
¶Indicates wrong label errors within wrong preparation group.
CNS, central nervous system; F, female; KBM, knowledge-based mistake; M, male; MAE, medication administration error; RBM, rule-based mistake.
Active failures
Casual attitudes towards dose checking were often discussed in relation to slips, whereas both types of execution failure shared common causal elements in equipment design (eg, look-a-like medicines), distractions and familiarity with patients. One nurse reported how distractions adversely affected her when checking a pump infusion rate:
“[…] ward rounds going on […] the patients are buzzing and everyone's asking you for handover and they're wanting patients out the ward and all this to do and I think to be honest there was too much going on, and the fact that someone was standing talking to me just kind of like, took my attention away at the time.” (N16, female, 0–4 years (qualified as a nurse when IV MAE occurred))
Knowledge-based mistakes (KBMs) occurred when participants encountered novel or infrequent challenges and lacked sufficient knowledge, as one nurse described:
“[…] I didn't know that vancomycin given too quickly could cause that reaction [red man syndrome] at all. So you just…that's something else maybe my knowledge of that wasn't, kind of, good enough.” (N07, female, 5–9 years)
When faced with knowledge gaps, nurses either lacked or chose not to access support resources due to a variety of reasons which included challenging professional relationships, high perceived workload and application of incorrect actions which were based on prior experiences.
Rule-based mistakes occurred when nurses misapplied normally good rules regarding dosage adjustments for continuous infusions or for prescription checking activities. Infusion pump design, application of past experience, high perceived workload and local working practices were also implicated as contributory factors.
Most violations of procedures hinged on a decision not to challenge or question another member of the healthcare team when uncertain about either the legibility of a prescription or whether to administer a drug without it being checked. One nurse described how their knowledge of the condition being treated and their relationships with other staff members influenced the decision not to clarify an illegible prescription:
“[…] because of the clinical context I was like […] I know meningitis, I know ceftriaxone, […] and showing [the drug to] my peer and […] I trust that person implicitly. […] because I should've just said well, to the prescriber who wasn't there, […] would you re-prescribe this please, it's illegible. And you'd have to take grief off them […] And that is policy, that's what one should do. The problem with policy is that it doesn't take into the individuals accounts that the patient needs the antibiotic promptly. […] And it's a real balance, especially in the moment, in the clinical mind set what will take precedent.” (N11, male, 5–9 years)
Error and violation provoking conditions
The patient
The increase in workload and associated distractions which accompanied dealing with clinically deteriorating patients or their relatives either individually or collectively during busy shifts commonly contributed to slips and lapses. In some cases, workload pressures added to nurses’ concerns for other patients to adversely affect concentration on the task at hand, leading to lapses and slips:
“[…] so I was probably rushing as well due to the stress of getting everything done on time, and with me having quite a poorly patient I really wanted to be focusing on him […] Because this patient, the lady, she was stable apart from the high potassium […] She was absolutely fine otherwise. So he was my priority, really.” (N04, female, 0–4 years)
The individual nurse
Participants described making KBMs or execution failures when they were not familiar with infrequently used medicines. Conversely, overconfidence when ascertaining the identity of prescriptions or checking infusion pump inputs or prescriptions also led to MAEs and arose due to familiarity with patients’ treatment regimens, their physiological response to drug treatment or in using infusion pump devices, as one nurse recalled, when checking a prescription:
“[…] I didn't concentrate enough on the prescription […] I've known her for years she's been coming to the ward for years. I know exactly why she's coming in […] I had given her the drug myself [in the past] […] So somehow[…] I've allowed myself to see that [not concentrating] as acceptable.” (N14, female, 10+ years)
Some newly qualified nurses described their lack of confidence and willingness to challenge others’ decisions as factors which contributed to intravenous MAEs. Perceptions of team hierarchy contributed to these decisions when nurses thought that doctors did not make mistakes or that they would inform them of important information personally (meaning they would not need to check the patient's medical notes). Others reported how they wanted to be perceived as managing their role but that in reality they struggled with workload, with two nurses mentioning that fear of looking incompetent explained this behaviour. These opinions tended to change as the nurse grew in experience and felt confident to challenge others. Junior nurses, in particular, described how they had learnt bad practices experientially from more senior colleagues on the ward over time.
When dealing with multiple competing priorities and high workloads, nurses described reverting to a subconscious level of functioning which relied on experiential pattern recognition, often referred to as ‘autopilot’ (N09, female, 0–4 years). Violations and execution errors resulted while in this state as decisions were made instantaneously and with little conscious thought of the circumstances at the time. Nurses also reported a task-focused approach where intravenous administrations were rushed, particularly before lunch breaks, shift changes or between ward rounds, in order to focus attention on other tasks (eg, very sick patients, other ward round duties) or reduce workload for others (eg, on the next shift).
The healthcare team
Illegible prescription and medical note documentation, prescribing using incorrect sections of the prescription chart and failure to record medication administration contributed to slips, mistakes and violations when nurses decided against or omitted looking at these or misinterpreted their meaning. Illegible documentation at times led some nurses to give higher importance to verbal communication with medical staff for patient care. However, verbal miscommunication also contributed to mistakes and lapses, particularly in noisy theatre environments.
Participants recognised that they did not check intravenous doses thoroughly if the prescription was written by a respected physician or the task was carried out with a trusted nursing colleague. The superior knowledge and confidence perceived to be held by more experienced nursing colleagues also contributed to junior staff accepting their decisions and not second checking thoroughly, at times despite doubting the prescriptions’ safety.
Nurses described how poor relationships with medical staff deterred them from clarifying ambiguous or possibly incorrect prescriptions; these perceptions were influenced by previous negative experiences of being pressured to administer, treated discourteously and not being understood. Perceptions of being beneath medical staff in the professional hierarchy were linked closely with these experiences. The positive patient safety contribution of pharmacists was often dependent on them being present on the ward when nurses needed them. Experiences of limited accessibility to pharmacists and/or doctors contributed to two violations, two mistakes and one lapse when nurses either could not contact them or decided against doing so based on prior experience.
Risky practice norms contributed to MAEs. Examples included the dividing of checking roles such that the medication was never checked by two people, the preparing and administering of multiple intravenous medications simultaneously and administering of all evening intravenous doses before shift change. A nurse described how the latter example pressurised her and promoted a task-based approach to intravenous administration that eventually lead to a lapse:
“So being new myself it was drummed into me that we got the IV medications out before the night shift came on. So to me come eight o'clock, the night shift was starting […] So I felt pressure that I had to get them [IV doses] all out before they came out of the staff room [after shift hand over].” (N08, female, 0–4 years)
The working environment
Noisy, chaotic and busy working environment pressurised and distracted nurses, leading them to rush through tasks and fail to check prescriptions or dose preparation adequately. In one account, end of shift pressures combined with the ward layout and a temporary staff shortage encouraged a nurse to use time-saving techniques when administering intravenous medicines on her own:
“[…] it was hand over period. One nurse went in to hand over and the other nurse was dealing with another patient in the bay and I was left to make up the IVs […] That's why I took them [medication trays] both together [for second checking] because it was the furthest away bay, so I thought to save time […] it was easier to get her to check them both […] Obviously not checking the things properly resulted in the error.” (N08, female, 0–4 years)
Perceived high workload also contributed to mistakes and violations; and was increased due to temporary staff shortages, busy shifts, being responsible for more sick patients and inadequate staff-skill mix. One nurse considered workload and other contextual factors when deciding whether to challenge an illegible prescription:
“[…] you'd be thinking, I need to get these medicines finished, because in an hour and a half's time, I've got my lunch time drugs to get out. So, that would have been a factor [in not clarifying an illegible prescription].” (N03, male, 0–4 years)
Interruptions and distractions contributed to a total of 11 intravenous MAEs, all but 1 (KBM) of which were execution failures. Participants described dividing their attention while conversing with patients, their relatives and other healthcare professionals. Distractions also originated from all other error and violation producing conditions.
Related equipment
Ambiguous or obstructed dosage adjustment/checking interfaces on infusion pumps facilitated administration rate and dose errors via slips, mistakes and violations. In two cases, medicines required dose calculations which led to KBMs; in one case the medication vial was formulated for adults and the dose had to be converted for paediatric use. Look-a-like and sound-a-like medicines featured when nurses applied rules based on pattern recognition and consensus between colleagues or picked up the wrong product while being distracted, as described below:
“[The medicines looked] absolutely similar, except for the writing [on the label] […] They were both in the same syringes.” (N05, female, 10+ years)
The drug administration task
The majority (n=17) of respondents described a failure in either their individual intravenous dose-checking processes or the approach used when double checking with a nurse colleague as important contributors to intravenous MAEs. Weaknesses manifested as failures to read prescriptions properly, seek support, challenge prescribers and question the decisions of nursing colleagues, often despite personal doubts. A variety of other problems exposed the frailties of current intravenous dose-checking practices which included individual overconfidence and distraction, patient illness severity, high workload and interruptions, intraprofessional or interprofessional relationships, and inappropriate local working practices. One nurse described how some of these error and violation provoking conditions influenced her when double checking intravenous doses for senior colleagues:
“[…] with the nature of the ward and it being so busy, I think it's becoming just a bit of a habit to people to just check the expiry date, check it's the right drug and then yeah, it's fine […] up until this incident I'd still say that if a sister asked me to check something, I would check it by the look of it […] she'll have done it right.” (N04, female, 0–4 years)
Wider organisational decisions
Latent conditions were reported as a lack of availability of supportive resources for safe intravenous dosing, such as drug reconstitution guidelines as well as insufficient access to medicines and other healthcare professionals during evenings and weekends. Logistical issues concerning the balance between new patient admissions and discharges, and the timing of medication rounds also featured due to their negative effects on workload. Junior nurses mentioned that controlled access to intravenous administration as an undergraduate would have given them greater experience and confidence, thus preparing them more adequately for the demands of practice.
Discussion
This study has found that hospital nurses’ intravenous MAEs occur largely due to the error and violation provoking environment in which they work. Key strengths of this study are that it is the first to focus on investigating the causes of intravenous MAEs in UK hospitals using interview-based CIT to generate detailed error accounts; we achieved data saturation in the main emerging themes and the data analysis was carried out using human error theory which facilitated identification of a range of system failures. For each active failure a nurse made, different combinations of error and violation provoking conditions were responsible; however, considerable overlap existed as latent failures were closely linked.
Implications of findings
Active failures and error and violation provoking conditions
Execution failures most often occurred when nurses were working in familiar surroundings on routine tasks, but were either distracted or experienced changes in their immediate environment (eg, emergencies),22 which is consistent with the MAE literature which has studied these failures.9 11 12 17 Unlike prescribing errors,24 execution failures causing intravenous MAEs described by participants were often not identified and corrected before administration to patients.
KBMs had roots in lack of knowledge and experience of using medicines9 11 12 16 17 but were also dependent on the quality of the checking processes and whether nurses were able or chose to access supportive resources. A recent review of interventions designed to reduce MAEs in hospitals reported that education, training and increased access to supportive resources generally showed positive results.10
Accounts of violations revealed insights into intraprofessional and interprofessional relationships, and how nurses made clinical judgements in practice. Others have also identified the risks posed by violations that lead to MAEs9 25 and this active failure appeared frequently in intravenous MAEs.11 12 17
The collective accounts of nurse participants reveal that a number of healthcare team and working environment related conditions contributed to multiple active failure types. Nurses were the inheritors of prescribing errors made by other team members leading to MAEs (mistakes and violations), findings which have also been acknowledged by others investigating the origins of related ADEs.3 There is growing interest in the effect of interruptions and distractions on patient safety, and this study builds on previous work in associating them with MAEs.9 Previous efforts to reduce the impact of interruptions while administering medication show little evidence for improvements in error rates26 and nurses in this study also voiced mixed opinions towards these strategies. Attention now appears to be shifting towards understanding the origins and management of interruptions.27 28 Future research could build on the principle that some interruptions contribute positively towards patient care, and instead focus on empowering and training nurses in interruption management.26–28
Timing of medicines administration
Timing-dependent contextual influences were shaped by local working norms and the nurses’ desire to improve patient care, and were crucial contributory factors to intravenous MAEs. There were times when nurses rushed tasks, cut corners and worked subconsciously as they felt under pressure to administer intravenous doses. This pressure emerged from the need to attend concurrent ward rounds, to clear outstanding tasks for the next shift, to cover others’ workload while they were in shift handover, to meet the demands of medical staff or to respond to emergency situations. While efforts to improve shift handover have shown positive results for medical errors,29 no such interventions have yet been tested robustly for their effects on MAEs.10
Interestingly, workload was not mentioned as a contributory factor for the KBM and violations that occurred on weekends, and instead a lack of access or decision not to utilise supportive resources (medical and pharmacy staff) normally present during weekdays featured as a factor. Few have sought to determine whether MAE or related outcomes are more prevalent on weekends.30
Checking processes
Although inadequate checking processes have been reported previously as a contributory factor to error,31–34 these factors do not feature strongly in previous investigations of intravenous MAE causes9 11 12 or as a part of robust interventions designed to reduce MAEs.10 Checking exercises failed when nurses assumed overcompetence and had trust in each other or medical staff, were distracted by other duties, approached the administration task overconfidently without checking, or could not access or decided against accessing additional support. Earlier research in nursing33 34 and medicine16 have acknowledged similar issues regarding over-reliance on colleagues.
Current UK nursing standards for medicines management state that all intravenous dose calculations should be independently checked and that where possible, intravenous administrations should be checked by a second registrant (without specifying exactly when this checking should take place).35 In England, 85% of NHS hospitals have a double checking policy for intravenous doses.36 The majority of nurses in this study were unsure or gave conflicting accounts as to what they perceived to be correct checking policy, perhaps indicating a lack of understanding of this process.33 As the majority of dose calculation second checks in one UK paediatric hospital were not independent32 and the effect of double checking on MAE rates in unclear,31 a fundamental principle guiding remedial approaches should perhaps be to stress the importance of equal responsibility between the two practitioners involved and the nurses of any grade should be empowered to challenge others, given the fallibility of human nature.34
Task management
Nurses described how the working environment often resulted in management of tasks at a subconscious level, as they perceived that they had little time to complete all their work and therefore, could not stop to think about what they were doing. Mental workload has received little attention in previous MAE research.9 11 12 17 This led to some participants considering drug administration as a task of less importance when compared with other duties or overall shift goals, causing them to rush medication administration so that they could move onto other duties. Others were rendered susceptible to inappropriate application of pattern recognition or missing important checking steps in maintaining safety while distracted.
Nurse decision-making during intravenous medication administration has been studied37 as have the underlying theoretical principles behind such behaviours.38 The findings of this study reflects the work of other researchers; it suggests that we manage and process information using type 1 (predominant approach, using intuitive subconscious responses based on instinct and repetitive experiences) and type 2 thinking modes (conscious, analytic responses which are slower), both of which are prone to cognitive biases that can lead to error.39 Nurse respondents shared beliefs with those from earlier work regarding how patient advocacy, a sense of time pressure and familiarity with their patients contributed to their decision-making during medication administration.37 However, as these decision-making investigations predominantly tried to understand how nurses maintain safety during medication administration, further work could focus on understanding which cognitive biases negatively affect medication safety for nurses, and how practitioners can recognise and minimise them in their own practice.
Limitations
Data collection relied on nurses self-reporting and recounting past intravenous MAE events which increases the risk of recall and hindsight bias.40 Social desirability bias41 was minimised by using CIT as nurses were encouraged to explore their actual behaviours and describe circumstances at the time in detail. Nurses openly accepted blame for their errors and at times required prompting to reveal latent failures which could have reduced attributional bias.42 Recruitment of participants from two NHS hospitals may have limited the representativeness of the findings to other healthcare settings.
Conclusion
This qualitative critical incident study has revealed the complex interactions between active and latent failures that underpin the emergence of intravenous MAEs in UK hospitals. Depending on the active failures made by front-line staff, there are a number of error and violation provoking conditions that are often present. Three of these conditions were found to contribute to most of the identified MAEs: these were the dose-checking activities carried out by nursing staff, the mental workload of nurses in order to manage the demands of their role, and the timing of ward-based activities, such as shift changes as well as the shift patterns of healthcare staff during weekends. This evidence suggests that a number of complex and multifaceted novel interventions may be required in order to reduce the burden of intravenous MAEs in hospitals.
Acknowledgments
The authors would like to thank all the nurses who agreed to take part in this study, as well as healthcare staff at each participating site for acting as contacts to facilitate the participant recruitment process.
Footnotes
Contributors: All the authors contributed in the conception and design of the study. RNK and SDW conducted participant recruitment. RNK contributed to the collection and analysis of the data, and to the preparation of the manuscript. RNK and an authorised external transcribing company performed the data transcription. RNK, SDW and JC participated in the data extraction. All the authors reviewed and gave approval of the manuscript.
Funding: This work was supported as part of RNK’s Doctor of Philosophy (PhD) studentship, which is funded by the University of Manchester and University Hospital of South Manchester NHS Foundation Trust.
Competing interests: This work has not been posted or published elsewhere in its entirety with the exception of RNK's Doctor of Philosophy (PhD) thesis. An abstract summarising the study was presented at the European Drug Utilisation Research Group (EuroDURG) Annual Scientific Meeting (August 2014, Groningen, The Netherlands).
Ethics approval: The study was approved by the University of Manchester Research Ethics Committee (1028) and by the Research and Development departments of each participating NHS hospital trust.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Taché SV, Sönnichsen A, Ashcroft DM. Prevalence of adverse drug events in ambulatory care: a systematic review. Ann Pharmacother 2011;45:977–89. 10.1345/aph.1P627 [DOI] [PubMed] [Google Scholar]
- 2.Kanjanarat P, Winterstein AG, Johns TE et al. . Nature of preventable adverse drug events in hospitals: a literature review. Am J Health Syst Pharm 2003;60:1750–9. [DOI] [PubMed] [Google Scholar]
- 3.Carayon P, Wetterneck TB, Cartmill R et al. . Characterising the complexity of medication safety using a human factors approach: an observational study in two intensive care units. BMJ Qual Saf 2014;23:56–65. 10.1136/bmjqs-2013-001828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keers RN, Williams SD, Cooke J et al. . Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother 2013;47:237–56. 10.1345/aph.1R147 [DOI] [PubMed] [Google Scholar]
- 5.McLeod MC, Barber N, Franklin BD. Methodological variations and their effects on reported medication administration error rates. BMJ Qual Saf 2013;22:278–89. 10.1136/bmjqs-2012-001330 [DOI] [PubMed] [Google Scholar]
- 6.Rogers AE, Dean GE, Hwang WT et al. . Role of registered nurses in error prevention, discovery and correction. Qual Saf Health Care 2008;17:117–21. 10.1136/qshc.2007.022699 [DOI] [PubMed] [Google Scholar]
- 7.McDowell SE, Mt-Isa S, Ashby D et al. . Republished paper: where errors occur in the preparation and administration of intravenous medicines: a systematic review and Bayesian analysis. Postgrad Med J 2010;86:734–8. 10.1136/qshc.2008.029785rep [DOI] [PubMed] [Google Scholar]
- 8.National Patient Safety Agency. Safety in doses: improving the use of medicines in the NHS. http://www.nrls.npsa.nhs.uk/EasySiteWeb/getresource.axd?AssetID=61626&type=full&servicetype=... (Last accessed 11 Apr 2014).
- 9.Keers RN, Williams SD, Cooke J et al. . Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf 2013;36:1045–67. 10.1007/s40264-013-0090-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keers RN, Williams SD, Cooke J et al. . Impact of interventions designed to reduce medication administration errors in hospitals: a systematic review. Drug Saf 2014;37:317–32. 10.1007/s40264-014-0152-0 [DOI] [PubMed] [Google Scholar]
- 11.Taxis K, Barber N. Causes of intravenous medication errors: an ethnographic study. Qual Saf Health Care 2003;12:343–7. 10.1136/qhc.12.5.343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taxis K, Barber N. Causes of intravenous medication errors—observation of nurses in a German hospital. J Public Health 2004;12:132–8. 10.1007/s10389-004-0019-4 [DOI] [Google Scholar]
- 13.Treiber LA, Jones JH. Devastatingly human: an analysis of registered nurses’ medication error accounts. Qual Health Res 2010;20:1327–42. 10.1177/1049732310372228 [DOI] [PubMed] [Google Scholar]
- 14.Reid-Searl K, Moxham L, Happell B. Enhancing patient safety: the importance of direct supervision for avoiding medication errors and near misses by undergraduate nursing students. Int J Nurs Pract 2010;16:225–32. 10.1111/j.1440-172X.2010.01820.x [DOI] [PubMed] [Google Scholar]
- 15.Flanagan JC. The critical incident technique. Psychol Bull 1954;51:327–58. 10.1037/h0061470 [DOI] [PubMed] [Google Scholar]
- 16.Lewis PJ, Ashcroft DM, Dornan T et al. . Exploring the causes of junior doctors’ prescribing mistakes: a qualitative study. Br J Clin Pharmacol 2014;78:310–19. 10.1111/bcp.12332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ozkan S, Kocaman G, Ozturk C et al. . Frequency of pediatric medication administration errors and contributing factors. J Nurs Care Qual 2011;26:136–43. 10.1097/NCQ.0b013e3182031006 [DOI] [PubMed] [Google Scholar]
- 18.Anon ASHP Standard definition of a medication error. Am J Hosp Pharm 1982;39:321. [PubMed] [Google Scholar]
- 19.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG eds. Analysing qualitative data. London, UK: Routledge, 1994:172–94. [Google Scholar]
- 20.Gale NK, Heath G, Cameron E et al. . Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:117 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reason J. Human error. Cambridge, UK: Cambridge University Press, 1990. [Google Scholar]
- 22.Reason J. Managing the risks of organizational accidents. Aldershot, UK: Ashgate Publishing Limited, 1997. [Google Scholar]
- 23.Ross S, Ryan C, Duncan EM et al. . Perceived causes of prescribing errors by junior doctors in hospital inpatients: a study from the PROTECT programme. BMJ Qual Saf 2013;22:97–102. 10.1136/bmjqs-2012-001175 [DOI] [PubMed] [Google Scholar]
- 24.Dornan T, Ashcroft D, Heathfield H et al. . An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education. EQUIP study, 2009. http://www.gmc-uk.org/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf (Last accessed 10 Mar 2014). [Google Scholar]
- 25.Alper SJ, Holden RJ, Scanlon MC et al. . Self-reported violations during medication administration in two paediatric hospitals. BMJ Qual Saf 2012;21:408–15. 10.1136/bmjqs-2011-000007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raban MZ, Westbrook JI. Are interventions to reduce interruptions and errors during medication administration effective? A systematic review. BMJ Qual Saf 2014;23:414–21. 10.1136/bmjqs-2013-002118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colligan L, Bass EJ. Interruption handling strategies during paediatric medication administration. BMJ Qual Saf 2012;21:912–17. 10.1136/bmjqs-2011-000292 [DOI] [PubMed] [Google Scholar]
- 28.Walter SR, Li L, Dunsmuir WT et al. . Managing competing demands through task-switching and multi-tasking: a multi-setting observational study of 200 clinicians over 1000 hours. BMJ Qual Saf 2014;23:231–41. 10.1136/bmjqs-2013-002097 [DOI] [PubMed] [Google Scholar]
- 29.Starmer AJ, Sectish TC, Simon DW et al. . Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA 2013;310:2262–70. 10.1001/jama.2013.281961 [DOI] [PubMed] [Google Scholar]
- 30.Ho CYW, Dean BS, Barber ND. When do medication administration errors happen to hospital inpatients? Int J Pharm Pract 1997;5:91–6. 10.1111/j.2042-7174.1997.tb00891.x [DOI] [Google Scholar]
- 31.Alsulami Z, Conroy S, Choonara I. Double checking the administration of medicines: what is the evidence? A systematic review. Arch Dis Child 2012;97:833–7. 10.1136/archdischild-2011-301093 [DOI] [PubMed] [Google Scholar]
- 32.Alsulami Z, Choonara I, Conroy S. Paediatric nurses’ adherence to double-checking process during medication administration in a children's hospital: an observational study. J Adv Nurs 2014;70:1404–13. 10.1111/jan.12303 [DOI] [PubMed] [Google Scholar]
- 33.Dickinson A, McCall E, Twomey B et al. . Paediatric nurses’ understanding of the process and procedure of double-checking medications. J Clin Nurs 2010;19:728–35. 10.1111/j.1365-2702.2009.03130.x [DOI] [PubMed] [Google Scholar]
- 34.Armitage G. Double checking medicines: defence against error or contributory factor? J Eval Clin Pract 2008;14:513–19. 10.1111/j.1365-2753.2007.00907.x [DOI] [PubMed] [Google Scholar]
- 35.Nursing and Midwifery Council. Standards for medicines management 2010. http://www.nmc-uk.org/Documents/NMC-Publications/NMC-Standards-for-medicines-management.pdf (Last accessed 14 Apr 2014). [Google Scholar]
- 36.McLeod M, Ahmed Z, Barber N et al. . A national survey of inpatient medication systems in English NHS hospitals. BMC Health Serv Res 2014;14:93 10.1186/1472-6963-14-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dougherty L, Sque M, Crouch R. Decision-making processes used by nurses during intravenous drug preparation and administration. J Adv Nurs 2012;68:1302–11. 10.1111/j.1365-2648.2011.05838.x [DOI] [PubMed] [Google Scholar]
- 38.Banning M. A review of clinical decision making: models and current research. J Clin Nurs 2008;17:187–95. [DOI] [PubMed] [Google Scholar]
- 39.Croskerry P. From mindless to mindful practice—cognitive bias and clinical decision making. N Engl J Med 2013;368:2445–8. 10.1056/NEJMp1303712 [DOI] [PubMed] [Google Scholar]
- 40.Henriksen K, Kaplan H. Hindsight bias, outcome knowledge and adaptive learning. Qual Saf Health Care 2003;12(Suppl 2):ii46–50. 10.1136/qhc.12.suppl_2.ii46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grimm P. Social desirability bias. In: Sheth JN, Malhotra NK, eds. Wiley international encyclopedia of marketing. John Wiley and Sons Ltd, 2010. http://onlinelibrary.wiley.com/doi/10.1002/9781444316568.wiem02057/abstract [Google Scholar]
- 42.Mezulis AH, Abramson LY, Hyde JS et al. . Is there a universal positivity bias in attributions? A meta-analytic review of individual, developmental, and cultural differences in the self-serving attributional bias. Psychol Bull 2004;130:711–47. 10.1037/0033-2909.130.5.711 [DOI] [PubMed] [Google Scholar]


