Abstract
Breast cancer incidence increases with age, but many older women do not receive appropriate mammography screening. A tool to support provider decision-making holds potential to help providers and patients reach the best-informed decisions possible. We developed and tested a decision aid (DA) for healthcare providers to use in mammography screening recommendations in older women. Literature review, expert opinion, focus groups, and pilot testing of the DA were conducted in a university ambulatory geriatrics practice. Provider evaluations of the DA after piloting were collected and analyzed. Geriatricians reported important factors in decision-making included patient life-expectancy, preferences, cognitive function, and individualization. Geriatricians reported the DA would have helped them make recommendations for mammography screening in 66% of pilot cases. It was less helpful when there was more certainty regarding decision-making.
Keywords: elderly, mammography, screening, decision aid
Introduction
It is estimated that 207,090 women were diagnosed with and 39,840 women died of breast cancer in 2010 (Howlader, Noone et al, 2011). Breast cancer is the most frequently diagnosed cancer in women, and its risk increases with age, with women aged 60-84 experiencing the highest breast cancer incidence (Howlader, Noone et al, 2011). Over two-thirds of breast cancer deaths are in women aged 60 years and older (Jemal, Siegel and Xu, 2010).
There are a number of recommendations regarding breast cancer screening among older women. The American Geriatrics Society recommends screening older women until age 85 in those with an estimated life-expectancy of 5 years or more, and beyond 85 for those with excellent health or functional status (American Geriatrics Society Clinical Practice Committee, 2000). The American Cancer Society recommends mammography screening continue “as long as a woman is in good health,” and the age at which it should be stopped should be individualized (Smith, Saslow et al, 2003). The US Preventive Services Task Force (USPTF), recommends biennial mammography screening for women age 50 to 74 years, stating that current evidence is insufficient to assess the benefits and harms in women 75 and older (US Preventive Services Task Force).
Estimated rates of biennial mammography screening among women age 65 and older in the US appear to be low, with reported rates ranging from 64% to as low as 25% (Breen, Wagner et al, 2001; Randolph, Mahnken, et al, 2002; Kagay, Quale, and Smith-Bindman, 2006; Baggwell, Giordano, 2008). Given that the average life-expectancy for an 80 year old woman is 9.1 years, there may be many women likely to benefit from mammography screening who do not receive it. However, mammography screening in elderly women with more than 3 comorbidities or in women with life expectancy of less than five years is not likely of benefit (Sartiano and Ragland, 1994; Walter, Lewis, and Barton, 2005; Walter and Covinsky, 2001). A population-based study of utilization patterns in women over 80 years of age found that nearly 40% of those unlikely to benefit from mammography screening due to poor health had nonetheless received mammography screening (Schonberg, McCarthy, et al, 2004).
The decision whether to undergo mammography screening among older women is highly influenced by physician recommendation (Schonberg, Ramanan, et al, 2006; Schonberg, McCarthy, et al, 2007; Crane, Kaplan, et al, 1996; Makuc, Breen, et al, 1999). However, decisions to recommend mammography screening for elderly women can be complicated; as such decision-making may be influenced by perceptions of a patient's health status, comorbidities, physical and cognitive functional status, knowledge of the screening recommendations, the risks and benefits of available treatment options, and patient preferences. Given that both underuse and overuse of screening in older patients are influenced by providers' recommendations as well as patient's preferences (often informed and shaped by provider recommendations), and given what can be a complex calculation of whether benefits outweigh risks in older patients, a tool designed to support provider decision-making has the potential to help both providers and patients reach the best-informed decisions possible (Rosen and Weintraub, 2006).
Decision aids may promote informed decision-making for cancer screening (Walter and Lewis, 2007). Although decision aids for mammography screening for use by patients have been examined, none have been developed for use by physicians or other health care providers (Mathieu, Barratt, et al, 2007; Mathiieu, Barratt, et al, 2010). In an effort to inform decision-making for health care providers regarding mammography screening for women aged 65 years and older, we developed and conducted preliminary testing of a decision aid (DA) for use by health care providers in making recommendations for mammography screening among older women.
Methods
Study Design
We initially developed the DA in 2007, based on a review of the literature and investigators' experience. We then surveyed and conducted focus groups among geriatricians to refine the DA. Finally, we tested the utility of the DA by asking geriatricians to determine whether it would have helped them with decision-making regarding mammography screening when considering clinical data from a sample of their patients.
Participants and Baseline Survey
We recruited 13 geriatricians to participate in the study because of their specialized knowledge and experiences caring for older patients. All geriatricians in this convenience sample practiced in a university-based ambulatory practice and were recruited through department-wide emails and announcements made at in-person meetings. Participants completed a face-to-face survey about academic career track (clinician educator or clinician scientist), years in practice, gender and ethnicity. We also queried them regarding factors influencing their decisions to recommend mammography screening in older patients with no prior history of breast cancer, including life expectancy, comorbidities, physical and cognitive function, quality of life, ability or interest in participating in breast cancer treatment, family history of breast cancer, and ability to obtain transportation for screening. The UCLA Office of Human Research Protection Program approved the study and written informed consent was obtained from all participants.
Developing a draft of the Decision Aid (DA)
We developed a first draft of the DA based on literature review, which identified salient epidemiological, clinical, and ethical factors to consider in making screening decisions in frail elderly women (Rosen and Weintraub, 2006), supplemented by investigators' clinical experience. We utilized the Walter and Covinsky (2001) framework for individualized screening mammogram decision-making, with a particular emphasis on determining quartiles of life expectancy, using life tables based on data from the U.S. National Center on Health Statistics (National Center for Health Statistics, 1997), also informed by Sachs (1994), with considerations of clinical state and prognosis, benefits versus burdens of screening, and whether one would treat a condition if detected. The draft DA had 4 steps and was organized as a flow chart. In Step 1, the healthcare provider was asked to use the life tables to answer the following question: “Does your patient have a life expectancy of more than 5 years?” or “Does your patient have at least one severe chronic medical condition that they are likely to die from in less than 5 years?” If life expectancy was determined to be at least 5 years, then Step 2 asked the healthcare provider the following: “If the patient has an abnormality seen on mammography that looked suspicious for breast cancer, would she want to pursue further treatment?” If the provider thought the patient would want to seek treatment, then in Step 3, the provider was asked: “Will the physical discomfort of a mammogram outweigh any benefit from it? Consider especially those patients with severe physical disability, in whom it will be difficult to be mobilized for mammography.” If the provider answered yes, then in Step 4, they were asked: “Will the patient be able to tolerate breast cancer treatment including chemotherapy, radiation or surgery?” If the provider answered yes, then they were prompted to recommend mammography screening to the patient.
Focus Groups
To enhance our understanding of geriatricians' attitudes and thought processes when making decisions about screening mammography, and to obtain specific feedback on the draft of the DA, we conducted two focus groups each lasting 60 minutes, with 6 geriatricians in the first and 7 geriatricians in the second. An investigator experienced in qualitative research methodology (JL) moderated the focus groups using a standardized, semi-structured question guide. Questions were developed based on a priori knowledge of the literature and clinical experience. The guide used open-ended questions to explore: 1) the factors that geriatricians find most important in assessing appropriateness of mammography screening for their older patients; and 2) reactions to the DA. To supplement the discussion recording, study investigators took notes and documented non-verbal interactions, exchanges of opinions and the general content of the discussion.
Pilot Testing the Revised DA
After the focus groups were completed, we reviewed the findings and revised the DA. We then pilot tested the revised DA to determine its utility to aid geriatricians in making decisions about recommending screening mammograms to their patients. Each participating geriatrician was given the tool to use when seeing a series of up to 10 of their female patients with no history of breast cancer in the office. After seeing each patient, the geriatricians completed a questionnaire asking them the following; “Would the DA help you decide whether or not to recommend mammography screening for this patient?” Response choices were “Yes” or “No”, and comments were encouraged. As the DA was still being tested, we instructed the physicians not to use it in actual decision-making.
Data Analysis
All focus group audiotapes were transcribed verbatim by an experienced transcriptionist. We used standard qualitative techniques to identify focus group content and major thematic categories (Ryan and Bernard, 2003). First, one investigator (JL) who was present at all focus groups reviewed the transcripts and session notes and summarized the results from each group. Two investigators, one who was present at all focus groups (SR) and one who was not (DT), reviewed session transcripts and developed categories that described transcript content, and identified themes concerning the two key domains addressed in the focus groups: 1) factors influencing decision-making and 2) critiques of the DA. A third investigator who was present for all groups (AM), reviewed results to ensure validity. Discrepancies among team members were discussed and resolved through an iterative consensus process.
Results
Participant Characteristics
The 13 focus group participants included 6 clinician scientists and 7 clinician educators who had been in practice between 3 and 30 years. There were 4 females and 9 males; 8 were non-Hispanic White, 4 were Asian American, and 1 was Hispanic. The criteria that geriatricians reported influenced decision-making about mammography screening included life expectancy (all 13 geriatricians endorsed this response), cognitive (n=13) and physical (n=11) function, comorbidities (n=11), quality of life (n=11), patient interest in screening (n=11) and treatment (n=8), and family history of breast cancer (n=8).
Focus Group Results: Factors Influencing Decision-Making Regarding Screening Mammography Recommendations
The themes identified during discussion of factors influencing decision-making included patient life-expectancy, patient preferences, comorbidities, cognitive function, and the need for individualized decision-making.
Life Expectancy
Several participants expressed the belief that mammography screening should only be recommended if patients had a life expectancy of greater than 10 years. They reported a need for better evidence and methodologies to support the estimation of life expectancy in their older patients. Many expressed concern regarding their own abilities to estimate life expectancy.
Patient preferences
Responses about the role of patient preferences for screening reflected two general approaches: 1) making recommendations for routine mammography screening only for patients who are already perceived to have a preference for screening and treatment, or 2) making such recommendations to all patients regardless of perceived preferences, because preferences are mutable and may change over time. One physician remarked, “I bring it up regardless of preference. I will often persist, saying, ‘You know, last year you didn't want a mammogram, so let's talk.’ Because sometimes you get high functioning 75-year olds, and they change their mind, so I look at it as an ongoing dialogue.”
Participants also discussed whether to consider patient preferences before or after making a recommendation. Some physicians felt that patient preference would not affect their initial recommendation of mammography screening, although they would take preferences into account when discussing mammography and reaching an informed decision together. Others expressed that they would not even raise the issue of mammography screening for patients who had limited life expectancy or were more likely to die from another comorbidity, and did not feel shared decision-making in these cases was as important unless the patient raised the issue on her own.
The group discussion included considerations of quality of life, not only length of life. One physician gave an example of a frail 86 year-old patient with cardiac disease who chose to undergo mammography screening and was diagnosed with breast cancer. “She became so anxious and stressed out. Radiation really negatively impacted her quality of life. She completed treatment and was still very anxious about her breast cancer. Six months later, she died of cardiac arrest. I've always kind of thought I ruined the last years of this lady's life.”
Competing comorbidities
Some commented that patient clinical pictures also change over time, and that comorbidities requiring immediate management play a large role in influencing the priority given to recommendations for mammography screening. “If they suddenly have some acute issues that have developed over the last year -- they've developed colon cancer, they've been undergoing treatment -- slowly breast cancer screening falls to the bottom of the task list. Their colon cancer treatment is on top probably, their hypertension, their diabetes, and whatever else they have going on. Then mammography screening may make its way back up when things stabilize.”
Cognitive function
Cognitive function and its impact on life expectancy, determining capacity to make an informed decision, and determining whether to recommend mammography screening were discussed. One physician shared that he would not recommend mammography screening for advanced dementia patients, stating “demented patients would find screening mammogram painful and scary.” Another physician shared an example of a woman with dementia, but otherwise good quality of life, who was diagnosed with breast cancer. She received surgery and radiation, and was now continuing to live a good quality of life more than 5 years later. “Its kind of hard,” the physician commented, “but if you're having a discussion about treatment, options and benefits, and I were discussing with that proxy decision-maker, I'd say ‘well, potentially it could lead to a good quality of life.’” This physician added that although this breast lump was initially detected with clinical breast exam, s/he “would always lump a clinical breast exam together with a screening mammogram,” when deciding whether to screen.
Heterogeneity of geriatrics patients
One geriatrician in each focus group made the point that, although the risk-benefit calculations and practice styles of geriatricians may be more conservative than in other specialties, particularly with respect to screening, this approach may not always be appropriate given the heterogeneity of the geriatric patient population. One stated, “The problem comes with the downstream effects of your decision-making. I think one of the things that distinguish geriatricians from general internists is that we are very wary of the adverse consequences of our actions. Because you tend to behave according to the average patient, and most of my patients are in their 80s or 90s, I think I tend to have a very conservative style, which is why the decision aid might be helpful to remind me that there are these people… for whom it (mammography screening) might be appropriate.” Another commented, “It is a hard task…when we know we take care of older adults, and there is so much variability, that chronology has little to do with life expectancy.”
Individualized care
These discussions included a strong theme of the need for individualization of care. One physician stated, “In cases where I've been their doctor for a while, I may continue to recommend screening because I know their personality. I think I have to take it based on each individual patient.”
Focus Group Results: Critique of the Draft DA
Participants reviewed the draft DA and shared their reactions. Participants liked the life tables presented in DA Step I, life expectancy determination, but some wanted more help to classify patients into percentiles of functional status. Some appreciated the degree of subjectivity, allowing for flexibility and physician judgment. Others felt unable to classify patients without more information, and requested more specific guidance about known predictors of life expectancy.
The majority of participants commented that Step 2: “patient preferences for treatment if the mammogram looked suspicious for cancer” must be discussed with patients in order to adequately assess preferences. As one participant explained, “Clinicians…a lot of times they're wrong about what they think their patients want. Most of the time, I need to ask. I don't assume I know their decisions. As physicians, I really think it is our job to help them go through that decision process.” A minority of physicians responded that, in some cases involving longstanding physician-patient relationships, prior knowledge of a patient's or her proxy's preferences might influence the physician not to initiate the discussion.
In Step 3, physicians were asked to consider whether the physical discomfort of getting a mammogram, especially in someone with severe disability would outweigh benefit. Some questioned whether this item overlapped with the first item regarding life-expectancy. One physician said, “A lot of times the ones with severe physical disabilities also have a life-limiting condition.’” Others questioned the ethics of not offering mammograms to patients with disabilities for any reason. Some strongly encouraged the addition of emotional discomfort or psychological distress as an issue that could alter the risk-benefit calculation. Others conceptualized the issue essentially as a dimension of patient preferences, and while the prospect of discomfort might influence patient preferences, it should not alter the physician's decision to recommend mammography screening.
In Step 4, physicians were asked to consider whether the patient would be able to physically tolerate treatment if screening detected breast cancer. Some respondents pointed out that this was not a simple question, since some patients might not be able to tolerate surgery, while others might be able to tolerate surgery alone or with radiation but not chemotherapy. Another participant stated, “the modern treatments for breast cancer are more tolerable than previous treatments have been. I think some of this has to do with the patient's baseline mental health and how they're going to react to information that might be negative. So part of it comes down to the physician's assessment of what the patient can handle.” Other respondents questioned whether this consideration should be part of the decision of whether to recommend mammography screening. One physician pointed out that many elderly patients might like to know whether they have cancer, apart from the questions of whether they were willing or able to undergo treatment, and that the physician recommendation for a screening mammogram could provide the starting place for the discussion of these issues.
Revised DA (Figure 1)
Figure 1. Decision Aid for Mammography Screening in Older Women.
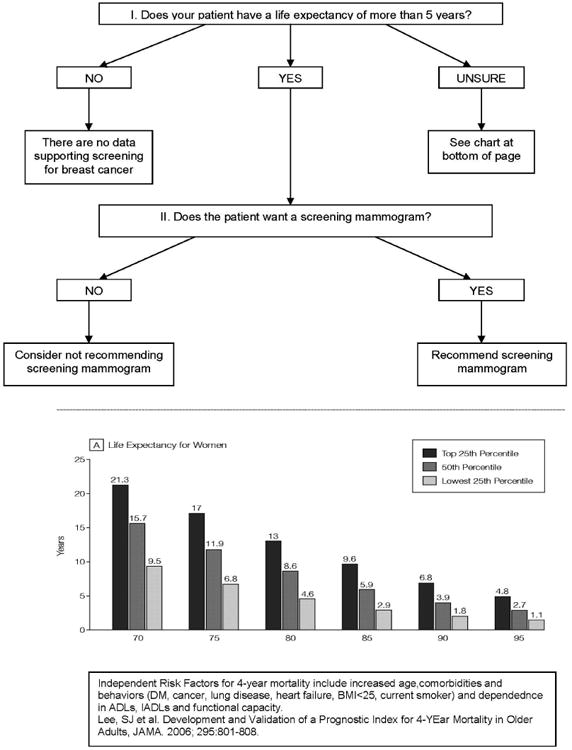
The data from the focus groups was used to revise the DA. The original four steps were condensed to two steps. Because geriatricians felt physical discomfort and life-expectancy were comingled, and would thus be captured by estimated life-expectancy, we eliminated Question 3 from the revised DA. In addition, rather than specifically asking whether the patient would want to pursue treatment if cancer were detected, geriatricians suggested that the DA could be simplified to ask whether the otherwise eligible patient would want a screening mammogram.
The first step in the revised DA includes the question “Does your patient have a life expectancy of more than 5 years?” If the answer is no, a text box indicates that there are no data to support mammography screening. If unsure, one is directed to the accompanying Life Tables of the United States to help determine the patient's life expectancy. In response to feedback that physicians felt uncertainty regarding estimation of life expectancy, in the revised DA we listed the independent risk factors for 4-year mortality derived by Lee et al, which include increased age, key comorbidities (Diabetes, cancer, lung disease, heart failure, BMI<25, current smoker) and functional status (Lee et al, 2006). If a patient is thought to have a life expectancy greater than 5 years, one is directed to the second step, “Does the patient want a screening mammogram?” If the answer is “No”, the accompanying text box reads “Consider not recommending a screening mammogram”. If the answer is “Yes”, then the accompanying text box reads, “Recommend a screening mammogram”.
Pilot Test of DA Utility
The revised DA was pilot tested by 12 of the 13 geriatrician focus group participants using clinical data from 88 of their patients (mean number of patients per physician=7, range 2-11). One of the 13 focus group participants was unable to participate in the pilot test due to a clinic scheduling conflict. For 58 of the 88 patients (66%), geriatricians felt that the DA would help them to decide whether or not to recommend a screening mammogram. Physicians reported they liked being prompted to consider mammography screening, as well as the life expectancy table and the information on predictors of mortality. Physicians did not think the DA was useful for patients who could be classified at the extremes of either very ill or very healthy, since they felt, in these patients, there was less uncertainty regarding whether or not to recommend a screening mammogram.
Discussion
Evidence suggests that physician recommendation is a key determinant of whether older women receive mammography screening (Schonberg, Ramanan, et al, 2006; Schonberg, McCarthy, et al, 2007; Crane, Kaplan, et al, 1996; Makuc, Breen, et al, 1999). Major guidelines for mammography screening recommend screening in older women be individualized, considering health status and patient preferences. However, there has been a relative lack of guidance for physicians regarding how to synthesize considerations of functional status, comorbidity, life expectancy as well as patient preferences, and incorporate these topics into the process of decision-making. To begin to address this deficit, we developed the DA for use by physicians that incorporates consideration of life expectancy given risk factors for mortality such as age, comorbidities, smoking, and functional status as well as patient preferences. To develop this measure, we relied upon the existing literature, opinions and expertise of practicing geriatricians, and geriatrician assessments of its utility among a sample of their eligible patients.
In the focus groups, geriatricians identified several issues and concerns. First, there was concern over the paucity of clinical trial-based evidence regarding mammography screening in elderly women, and many were unfamiliar with current practice guideline recommendations. Second, many of the participants expressed concern over how to estimate life expectancy most accurately, and the relationships among life expectancy and physical and cognitive functioning in the elderly. Third, there was variation in approaches to discussions assessing patient preferences and incorporating them into the decision-making process. Focus group participants thought the DA was very helpful in raising their awareness of guidelines for mammography screening and clarifying the decision-making process. In testing the revised version of the DA, participating physicians thought the DA would help them to make screening mammograms decisions for patients who were neither very healthy nor very ill.
The recent USPSTF recommendation regarding routine mammography screening in women under the age of 50 has raised much attention (US Preventive Services Task Force), but issues around screening older women are still largely ignored. There are demonstrated variations in patterns of mammography screening among older women, including both underuse in women likely to benefit and overuse in women unlikely to benefit (Breen, Wagner, et al, 2001; Randolph, Mahnken, et al, 2002; Kagay, Quale, and Smith-Bindman, 2006; Schonberg, McCarthy, et al, 2004). As noted by Walter et al, given the heterogeneity of health status in the elderly, there is no single age cutoff at which potential harms suddenly outweigh potential benefits of mammography screening (Walter, Lewis, et al, 2005). Informed decision-making for preventive and screening services is increasingly promoted, consistent with Institute of Medicine Committee on Quality of Health Care in America recommendations for patient-centered quality healthcare (2001). Mammography screening for older women is a prime example of a service that could be better targeted with improved informed decision-making..
Given that screening in older patients is influenced by provider recommendations, and that calculating the likelihood of benefit outweighing risks can be challenging, we believe that a provider decision aid has the potential to help providers and patients reach the best-informed decisions possible. There have been efforts to develop decision aids for patients. Mathieu developed and tested two decision aids to assist patients in understanding the advantages and disadvantages of mammography screening, and in decision-making consistent with their values (Mathieu, Barratt, et al, 2007; Mathieu, Barratt, et al, 2010), but none have been developed for decision support among providers. One was targeted to 70 year-old women, and accounted for declining life expectancy but not health status (Mathieu, Barratt, et al, 2007). The decision aid increased knowledge and helped women to make an informed choice but did not alter their intention to undergo mammography screening. While we are unaware of prior studies of decision aids for providers addressing mammography screening, other work has sought to guide providers' discussions regarding the initiation of mammography screening with patients under the age of 50 (Nekhlyudov and Braddock, 2009).
This study has several limitations. First, focus groups included only geriatricians at an academic medical center, not other healthcare providers who practice in the community and who provide the vast majority of care to older women. We chose to gather data from geriatricians at an academic medical center, due to their specific training and experience in addressing health care needs, and considerations of risk-benefit tradeoffs for a range of older patients. Additional work may be necessary to adapt the DA for use among other specialists such as primary care providers. Second, since the DA was under development, physicians testing it were instructed not to use it in their actual clinical decision-making. Therefore, our findings are based on the physicians' assessment of how the tool might have affected their decision-making about offering mammography screening to older patients, and not on actual clinical care. Third, because most of the physicians who tested the DA also had input on its development, they may have had more favorable opinions about it than physicians who did not participate in its development. The pilot test was based on implicit physician judgment regarding whether the DA would have been helpful in decision-making; no gold standard test evaluated whether screening should have been recommended for pilot patients. Lastly, the DA as pilot-tested has certain limitations. It does not explicitly direct physicians to consider the risks of screening, (e.g., false positives and their consequences such as anxiety, further testing) but assumes the physician will be aware of these risks and discuss them with the patient when making a recommendation. It is important to note that the prognostic index used in the DA is based on large population-based science and is not intended as an individual prediction tool. Although several of the geriatricians voiced a preference for electronic decision aids, the DA was pilot tested in paper format.
A sample of geriatricians who helped to develop and test a mammography screening decision aid it found it to be useful for decision-making about mammography screening for the majority of the patients they were asked to consider. They found this decision aid helpful because of its brevity and incorporation of factors important to physicians in making decisions about mammography screening in older adults. Further, the presence of a decision aid that is readily available when seeing patients helped remind physicians to consider screening mammograms for their patients, and begin the process of informed decision-making.
Next, we hope to adapt and test this tool further, ideally in an electronic format for use on a tablet, among a larger and more diverse group of healthcare providers including providers specializing in primary care implementing the DA among a group of their patients to evaluate whether the DA influences rates of overuse and underuse of mammography screening among older women. With further testing, we hope that the DA will be useful to healthcare providers to initiate conversations about mammography screening, and for making informed recommendations to patients regarding mammography screening.
Acknowledgments
We thank the physicians in the Division of Geriatrics, David Geffen School of Medicine for their assistance with the research, Diana H. Liao, MS for her assistance with statistical analyses and Paul Camarena, BA for his assistance with manuscript preparation.
Funding Sources: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grant #040952095 from the Donald W. Reynolds Foundation as part of the Donald W. Reynolds Consortium to Strengthen Faculty Expertise in Geriatrics in US Academic Health Centers. Dr. Tisnado received support from P30-AG021684 and P30-AG128784 from the National Institute on Aging. Dr. Moore received support from P30-AG021684 from the National Institute on Aging, and from K24-AA15957 from the National Institute on Alcohol Abuse and Alcoholism.
Sponsor's Role: The organizations funding this study had no role in the design or conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review or approval of the manuscript.
Biographies
Diana M. Tisnado, PhD, is a health services researcher and Adjunct Associate Professor in the Division of General Internal Medicine and Health Services Research at the David Geffen School of Medicine at UCLA. Her research focuses on understanding and improving access to and quality of cancer care.
Alison A. Moore, MD, MPH, is a Professor of Medicine and Psychiatry at the David Geffen School of Medicine at UCLA. She is a geriatrician and health services Researcher, whose research primarily focuses on substance use in older adults.
Jennifer R. Levin, PhD, is a health educator with expertise in program planning and implementation. Dr. Levin specializes in stress management, addressing sleep disorders, nutrition and exercise, and substance use.
Sonja Rosen, MD, is an Associate Clinical Professor at UCLA David Geffen School of Medicine, Department of Medicine, Division of Geriatrics. She is a clinician educator and also the Medical Director of the inpatient service at SM-UCLA Hospital. Her research interests include preventive care, delirium and teaching geriatrics.
Footnotes
IRB Protocol Number: UCLA South Campus Institutional Review Board Approval #10-001755.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: Study concept and design: Rosen, Moore. Acquisition of data: Levin, Moore, Rosen. Analysis and Interpretation of data: Tisnado, Moore, Levin, Rosen. Preparation of manuscript: Tisnado, Moore, Levin, Rosen.
References
- American Geriatrics Society Clinical Practice Committee. Breast cancer screening in older women. Journal of the American Geriatrics Society. 2000;48:842–844. [PubMed] [Google Scholar]
- Badgwell BD, Giordano SH, Duan ZZ, et al. Mammography before diagnosis among women age 80 years and older with breast cancer. Journal of Clinical Oncology. 2008;26(15):2482–8. doi: 10.1200/JCO.2007.12.8058. [DOI] [PubMed] [Google Scholar]
- Breen N, Wagner DK, Brown ML, et al. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. Journal of the National Cancer Institute. 2001;93(22):1704–13. doi: 10.1093/jnci/93.22.1704. [DOI] [PubMed] [Google Scholar]
- Crane LA, Kaplan CP, Bastani R, et al. Determinants of adherence among health department patients referred for a mammogram. Women Health. 1996;24(2):43–64. doi: 10.1300/J013v24n02_03. [DOI] [PubMed] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA, Edwards BK, editors. SEER Cancer Statistics Review. National Cancer Institute; Bethesda, MD: 2011. pp. 1975–2008. http://seer.cancer.gov/csr/1975_2008/, based on November 2010 SEER data submission, posted to the SEER web site, 2011. [Google Scholar]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing The Quality Chasm: A New Health System For The 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer Journal for Clinicians. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- Kagay CR, Quale C, Smith-Bindman R. Screening mammography in the American elderly. American Journal of Preventive Medicine. 2006;31(2):142–149. doi: 10.1016/j.amepre.2006.03.029. [DOI] [PubMed] [Google Scholar]
- Lee SJ, et al. Development and Validation of a Prognostic Index for 4-Year Mortality in Older Adults. JAMA. 2006;295(7):801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- Makuc DM, Breen N, Fried V. Low income, race, and use of mammography. Health Services Research. 1999;34(1, Part 2):229–239. [PMC free article] [PubMed] [Google Scholar]
- Mathieu E, Barratt A, Davey HM, et al. Informed choice in mammography screening: a randomized trial of a decision aid for 70-year old women. Archives of Internal Medicine. 2007;167(19):2039–2046. doi: 10.1001/archinte.167.19.2039. [DOI] [PubMed] [Google Scholar]
- Mathieu E, Barratt A, Davey HM, et al. Helping women make choices about mammography screening: an online randomized trial of a decision aid for 40-year old women. Patient Education and Counseling. 2010;81(1):63–72. doi: 10.1016/j.pec.2010.01.001. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Life Tables of the United States. 1997 [Google Scholar]
- Nekhlyudov L, Braddock CH. An approach to communication about screening mammography in primary care. Journal of Women's Health. 2009;18(9):1403–1412. doi: 10.1089/jwh.2008.1184. [DOI] [PubMed] [Google Scholar]
- Randolph WM, Mahnken JD, Goodwin JS, et al. Using Medicare data to estimate the prevalence of breast cancer screening in older women: comparison of different methods to identify screening mammograms. Health Services Research. 2002;37(6):1643–57. doi: 10.1111/1475-6773.10912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen S, Weintraub N. The efficacy of performing screening mammography in the frail elderly population. Journal of the American Medical Directors Association. 2006;7(4):230–233. doi: 10.1016/j.jamda.2006.01.026. [DOI] [PubMed] [Google Scholar]
- Ryan GW, Bernard HR. Techniques to Identify Themes. Field Methods. 2003;15:85–109. [Google Scholar]
- Sachs GA. Flu shots, mammograms, and Alzheimer's disease: ethics of preventive medicine and dementia. Alzheimer Dis Assoc Disord. 1994 Spring;8(1):8–14. doi: 10.1097/00002093-199408010-00003. [DOI] [PubMed] [Google Scholar]
- Sartiano WA, Ragland DR. The effect of comorbidity on 3-year survival of women with primary breast cancer. Annals of Internal Medicine. 1994;120(2):104–110. doi: 10.7326/0003-4819-120-2-199401150-00002. [DOI] [PubMed] [Google Scholar]
- Schonberg MA, McCarthy EP, Davis RB, et al. Breast cancer screening in women aged 80 and older: results from a national survey. Journal of the American Geriatrics Society. 2004;52(10):1688–1695. doi: 10.1111/j.1532-5415.2004.52462.x. [DOI] [PubMed] [Google Scholar]
- Schonberg MA, Ramanan RA, McCarthy EP, et al. Decision making and counseling around mammography screening for women aged 80 or older. Journal of General Internal Medicine. 2006;21(9):979–985. doi: 10.1111/j.1525-1497.2006.00487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonberg MA, McCarthy EP, York M, et al. Factors influencing elderly women's mammography screening decisions: Implications for counseling. BMC Geriatrics. 2007;7:26. doi: 10.1186/1471-2318-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RA, Saslow D, Sawyer KA, et al. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer Journal for Clinicians. 2003;53(3):141–169. doi: 10.3322/canjclin.53.3.141. [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force. Screening for breast cancer. 2009 Retrieved from http://www.uspreventiveservicestaskforce.org/uspstf09/breastcancer.htm.
- Walter LC, Covinsky KE. Cancer screening in elderly patients – A framework for individualized decision making. JAMA. 2001;285(21):2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- Walter LC, Lewis CL, Barton MB. Screening for colorectal, breast, and cervical cancer in the elderly: A review of the evidence. American Journal of Medicine. 2005;118(10):1078–1086. doi: 10.1016/j.amjmed.2005.01.063. [DOI] [PubMed] [Google Scholar]
- Walter LC, Lewis CL. Maximizing informed cancer screening decisions. Archives of Internal Medicine. 2007;167(19):2027–2028. doi: 10.1001/archinte.167.19.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]


