Abstract
Background
AHCT is an established therapy for multiple myeloma (MM) with impact in quality of remissions and survival. We analyzed the role of race-ethnicity, sex and age-disparities in AHCT utilization in US.
Methods
We combined MM incidence derived from SEER-18 with transplant activity reported to the CIBMTR for the period of 2005–2009 to assess the impact of disparities in AHCT. Utilization (number of transplants/new cases) was compared between groups using relative utilization ratio (RUR), defined as [utilization for a given category]/[utilization for the entire population].
Results
Data was obtained from 22,462 actual MM cases and 13,311 AHCT. Age-adjusted RUR was 1.17 (1.15–1.19) among non-Hispanic Whites (NHW), higher than in non-Hispanic Blacks (NHB) [0.69 (0.67–0.72), P<0.0002], Hispanics [0.64 (0.60–0.69), p<0.002] and Asians [0.65 (0.58–0.73), P<0.0002]. There was higher AHCT utilization in men than in women among Hispanics (age-adjusted RUR 0.72 vs. 0.56, P=0.007), but not among NHW, NHB or Asians. Sex disparity prevents 1.3% of potential AHCTs in MM (10.4% among Hispanics). Racial-ethnic disparities prevent 13.8% of AHCTs (44.7% in Hispanic and Asians, 39.9% in NHBs).
Conclusions
Race-ethnicity disparity greatly affects AHCT utilization in MM. Sex disparity plays a lesser role, except among Hispanics. The ongoing decrease in age disparity will continue to drive major increase of AHCT activity. A 2-year and 5-year increase in age of the AHCT population would result in respectively 12% and 32% increase in volume of AHCT.
Keywords: Multiple Myeloma, Healthcare Disparity, Peripheral Blood Stem Cell Transplantation, Autologous Transplantation
Introduction
Autologous hematopoietic cell transplantation (AHCT) is an established modality in the upfront treatment of patients with multiple myeloma (MM). When employed early in the management of MM in younger patients, AHCT prolongs both the depth and duration of response and, in some studies, also overall survival(1, 2). At the population level, the expansion in use of AHCT for management of MM over the last two decades has also been linked to improved survival(3–5).
Recently, the feasibility and low toxicity of AHCT has been demonstrated also in older patients, with toxicity and disease control comparable to younger patients(6, 7). Similarly, Black patients undergoing AHCT for MM have outcomes similar to their White counterparts(8), but are less likely to undergo this treatment(9, 10). Little is known about transplant utilization in Hispanics and Asians in US.
We have recently published on the increasing, but yet low utilization of AHCT among MM patients in the US(11). Here, we combine MM incidence information from Surveillance, Epidemiology and End Results (SEER) database with the profile of patients with MM undergoing AHCT reported to the Center for International Blood and Marrow Transplant Research (CIBMTR) in the same period to understand how race, sex and age can affect utilization of AHCT and how correction of disparities could affect transplant activity.
Methods
Data sources
We estimated the number of new MM cases utilizing the National Cancer Institute Surveillance Epidemiology and End Result Registry (SEER). The SEER-18 includes the Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, Utah, Los Angeles, San Jose-Monterey, Rural Georgia, Alaska Native, Greater California, Kentucky, Louisiana, New Jersey and Greater Georgia tumor registries. It covers 27.8% of the US population and the representation of each racial/ethnic group is known((12)). In order to estimate the number of new MM cases (ICD-O-3 9732/3) diagnosed in the US during the period of study (2005–2009) we inquired the database using the case listing function of SEER*Stat8.1.5. For each case we extracted age, sex, race and ethnicity (Hispanic, non-Hispanic). We excluded cases for which the only source of information was death certificate or autopsy report. By knowing the number of newly diagnosed MM cases for each racial-ethnic category (REC) and the category’s proportional representation in the database, we were able to estimate the approximate number of new MM cases in the entire US population. Cases were grouped in 4 REC, non-Hispanic Whites (NHW), non-Hispanic Blacks (NHB), Hispanics (irrespective of race) and Asians. Cases with unknown race or ethnicity were excluded. A fourth racial group, American Indian/Alaska Native, was not included in the analysis since it accounted for only 0.2% of the MM cases and 0.3% of the AHCT.
We obtained the approximate number of AHCT for MM and basic patient demographics utilizing data from the CIBMTR. The CIBMTR is the research affiliation of the International Bone Marrow Transplant Registry and the National Marrow Donor Program (NMDP). Established in 2004, it receives data from > 500 transplantation centers worldwide on allogeneic and autologous HPC transplantation. Data are submitted to the Statistical Center at the Medical College of Wisconsin in Milwaukee and the NMDP Coordinating Center in Minneapolis, where computerized checks for discrepancies, physicians’ review of submitted data, and on-site audits of participating centers ensure data quality. In this analysis we utilized data on recipients of first AHCT for MM in the US between 2005 and 2009. The information required consisted of age, sex, race and ethnicity and was obtained from pre Transplant Essential Data (pre-TED) form. The CIBMTR does not capture the totality, but a known proportion of autologous transplantation events in the US, (methodology described elsewhere(13)). Therefore, by multiplying the number of registered transplants by a correction factor, one can arrive at the approximate number of transplants for the group of interest. For the purpose of the present work, it was assumed that there was no age, sex, race or ethnicity bias in reporting AHCT procedures.
For residents in the US, the pre-TED form allows selection of ethnicity (Hispanic of Latino, not Hispanic or Unknown) and race (White, Black or African American, Asian, American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander). Contrary to SEER, individuals can be identified by more than one race. Patients were placed in RECs as described above for SEER. There were 3.2% of AHCT cases identified as “Others”, reflecting mostly situations were more than one race or no race was selected. These cases were distributed into the main RECs in proportionality to the number of registered cases for a given age. To ensure that this reassignment did not produce false findings, we performed sensitivity analysis with two other scenarios: exclusion of all AHCPT with “others” identified as REC and distribution of the “others” into the 4 main categories proportional to the number of cases for a given age doubling the weight of the Hispanic and Asian categories. None of these scenarios altered the findings of this analysis.
Utilization
We assessed utilization as the ratio between first AHCT for MM and number of newly diagnosed cases in the period of interest. Since the scope of the present work is disparity, more than underutilization itself, and to avoid possible errors intrinsic to the correction factor, we chose to work with the concept of relative utilization ratio (RUR). We arrived at RUR for each category of interest by dividing the apparent rate of utilization for a given category by the utilization rate for the entire population. RUR was calculated for each sex, REC and age. The population of women is slightly older than the populations of men with MM. RECs also have a diverse age structure(12). Therefore we also compared RUR between RECs and between sexes within a given category by adjusting the age structure of MM cases in each category to match the one of the most numerous categories (NHW men).
Statistics
We described continuous numerical variables by median and interquartile range. Comparisons between proportions were performed using Chi square test. All statistical analysis was performed utilizing SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY). In all inference analyses, two-sided P values of less than 0.05 were considered to indicate statistical significance.
Results
We utilized data from 22,462 actual MM cases reported to SEER (excluding 178 cases with unknown race), and 13,311 actual AHCT reported to CIBMTR. Table 1 displays the distribution of MM cases and AHCT cases by sex and REC after calculation of the total US numbers, along with the median age for each subcategory. Median age at diagnosis of MM was higher in NHW than in any of the other RECs (P=0.0002). In all RECs the age at diagnosis was higher in women than in men.
Table 1.
Age distribution of the MM and AHCT cases according to race/ethnicity.
| NHW | NHB | Hispanic | Asian | ||
|---|---|---|---|---|---|
| MM cases | 72.0% | 18.7% | 6.7% | 2.6% | |
| Male | 55.6% | 70 (61–78)* | 65 (57–74)* | 65 (55–74)* | 69 (60–77)* |
| Female | 44.4% | 72 (62–81)* | 67 (57–76)* | 66 (56–76)* | 70 (59–78)* |
| AHCT | 77.4% | 15.8% | 5.2% | 1.6% | |
| Male | 58.5% | 60 (53–65)* | 58 (51–64)* | 56 (49–62)* | 57 (52–62)* |
| Female | 41.5% | 59 (53–65)* | 57 (50–62)* | 57 (48–62)* | 58 (50–65)* |
Age expressed in median (interquartile range)
Disparity
Both the unadjusted and the age-adjusted RURs are displayed in Table 2 for each sex and REC. There was higher utilization of AHCT in men detected among Hispanics, but not among NHB or Asians. Among NHW, the apparently higher RUR in men becomes non significant when RUR is adjusted for age structure. Such finding suggests that the higher AHCT utilization in NHW men than in NHW women is a function more of younger age at diagnosis than sex.
Table 2.
RUR for AHCT in MM according to sex and race/ethnicity
| Unadjusted RUR | Adjusted RUR | |||||
|---|---|---|---|---|---|---|
| Men | Women | P | Men | Women | P | |
| NHW | 1.13 (1.11–1.15) | 1.02 (0.99–1.04) | 0.02 | 1.18 (1.16–1.20) | 1.16 (1.13–1.18) | 0.23 |
| NHB | 0.87 (0.83–0.92) | 0.82 (0.78–0.87) | 0.11 | 0.70 (0.66–0.74) | 0.69 (0.65–0.73) | 0.89 |
| Hispanic | 0.90 (0.83–0.97) | 0.67 (0.60–0.74) | <0.0002 | 0.72 (0.66–0.79) | 0.56 (0.50–0.63) | 0.007 |
| Asian | 0.67 (0.57–0.77) | 0.60 (0.49–0.69) | 0.35 | 0.66 (0.56–0.77) | 0.64 (0.54–0.76) | 0.81 |
| All | 1.05 (1.03–.07) | 0.93 (0.91–0.95) | <0.0002 | 1.02 (1.01–1.04) | 0.97 (0.98–0.99) | P<0.0002 |
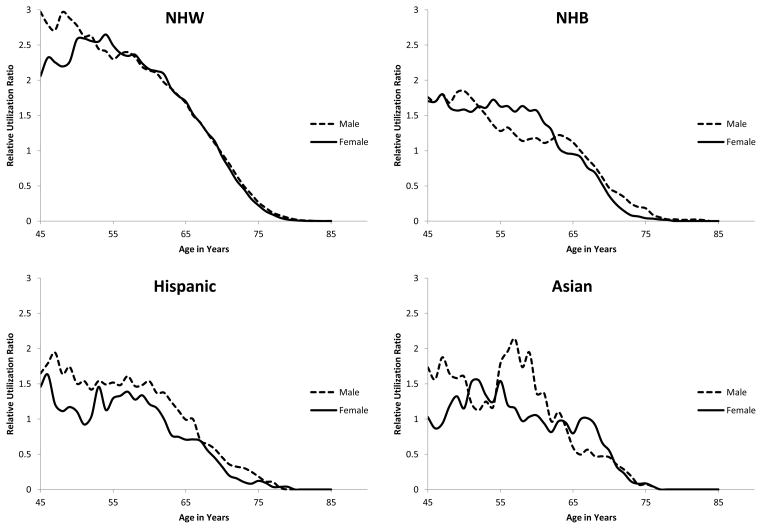
We subsequently aggregated data from both sexes in order to compare AHCT utilization among the RECs. Adjusted RUR was 1.17 (95% C.I. 1.15–1.19) among NHW, higher than in NHB [0.69 (95% C.I. 0.67–0.72), P<0.0002], Hispanics [0.64 (95% C.I. 0.60–0.69), p<0.002] and Asians [0.65 (95% C.I. 0.58–0.73), P<0.0002]. In fact, Figure 1 displays RUR as a function of age and sex for all RECs making clear the highest AHCT utilization among NHW. It is also obvious that AHCT declines with age in all RECs for both men and women, with the decline becoming very pronounced after the age of 55 years.
Figure 1.
Relative utilization ratio for AHCT in MM according to sex and age in the different race-ethnicity categories.
Even though the reasons for racial-ethnic disparity in transplant access are unknown, we performed an exploratory analysis in an attempt to recognize possible links between health care insurance and REC. Insurance information is available in SEER for the year of 2007 onward. We found that only 3.1% of the NHW patients with MM younger than 65 were identified as uninsured vs. 8.1% of NHB, 11.9% of Hispanics and 3.2% of Asians (P<0.0001). Along the same lines, Medicaid was the primary insurance for 7.1% of NHW, vs. 17.8% of NHB, 28% of Hispanics and 13.5% of Asians (P<0.001).
Effect of disparities in AHCT activity
We subsequently aimed at understanding the impact of disparities in the overall AHCT utilization and transplant volumes for MM. This was obtained by simulating AHCT numbers for the subcategory of interest when the utilization rates of a reference subcategory are applied to its MM population. Therefore, for estimation of underutilization due to sex disparity, utilization in men was used as reference. For estimation of underutilization due to race, NHW was the reference group.
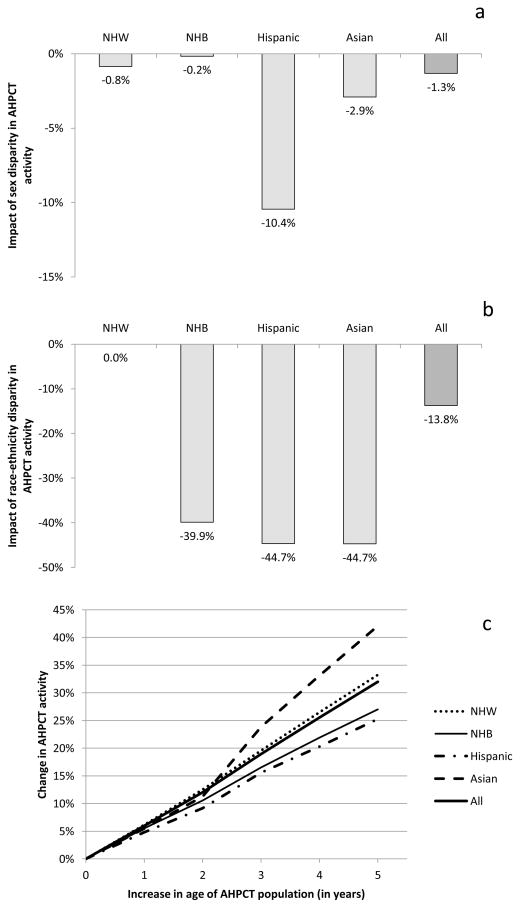
We found that 1.3% of potential AHCT procedures are unrealized due to sex disparity. This reaches 10.4% among Hispanics, and is lower among Asians and NHB (Figure 2a).
Figure 2.
Estimated impact of sex (panel a) and race-ethnicity disparities (panel b) in AHCT activity. Potential impact in volume of AHCT for MM resulting from the increase in the age of patients undergoing transplantation (panel c).
A much bigger impact can be attributed to race/ethnicity disparity that prevents 13.8% of AHCT procedures with a much greater impact seen in NHB, Hispanics and Asians (Figure 2b).
The impact of age disparity is more complex. Comorbidities impeding AHCT tend to become more common with age and there are very limited data supporting AHCT for the treatment of MM in individuals older than 75. Therefore, some decline in AHCT utilization with age is to be expected. It is known that the median age of MM patients pursuing AHCT continues to increase (11). We estimated the potential future impact of this increase by calculating transplant volumes when the current utilization rate for a given age is replaced by the one of a younger age. For example, to calculate the impact of 2 year increase in age at AHCT, we projected transplant volume by applying to a population of a certain age (e.g. 70 years) the current utilization rate of age −2 (in this example, 68 years). The impact of age disparity in AHCT utilization can be seen in Figure 2c. A 2-year increase in age of the AHCT population would lead to 12% increase, while 5 year would lead to 32% in the volume of AHCT for MM. Since RECs have diverse age structures, they are affected differently by the aging of the AHCT population. A larger effect would be seen among NHW and Asians while a smaller effect would be seen among NHB and Hispanics.
Discussion
Age and sex disparities in access to AHCT for treatment of MM have been described before (9, 10). A prior publication from the CIBMTR covering autologous transplant activity in the US from 1997 to 2002 found that Whites were more likely than Blacks (OR= 1.72) while males were more likely than females (OR=1.1) to undergo AHCT for MM(9). Importantly, by performing sensitivity analysis, that study found that selective under reporting of transplants performed in ethnic minorities, in addition to being unlikely, is not expected to affect the main conclusion. Similar disparities were seen in transplant utilization for other hematologic disorders. That study however did not address transplant utilization in Hispanic and Asians or sex disparities in access within each specific race.
More recently, Al-Hamadani et al(10) used data from the National Cancer Data Base (NCDB) to identify socio-geo-demographic factors associated with the utilization of AHCT for upfront treatment of MM. This study identified Black and Asian races, Hispanic ethnicity, older age, low neighborhood income or education, residence in a metro area, no or unknown medical insurance as factors associated with lower likelihood of use of AHCT upfront. Of interest, sex was not an independent factor associated with use of AHCT.
The present study explores in detail AHCT utilization in all main RECs, addresses the differential impact of sex in transplant utilization among the different RECs and provides detailed information on the effect of age in AHCT within each REC. Moreover, we estimated the impact of each recognized disparity in the overall volume of AHCT for MM. Unfortunately, since information linking transplant and patient place of residence is missing from the CIBMTR database, it was not possible to confirm the recently found underutilization of AHCT for MM in the Northeast(10).
Our study confirms the prior demonstration of profound underutilization of AHCT among Black patients with MM. However, underutilization almost to the same magnitude can be seen among Hispanics and Asians. Unfortunately, the databases used for the study do not provide an explanation for the strong link between REC and AHCT utilization. Recent work using data from the NCDB demonstrated that racial disparity in access to AHCT persists even when adjusted for income and education(10). It is possible that patient and physician bias play a role into the decision to pursue transplantation. Another possibility is that income and educational differences within a given geographic area may be linked to both race and transplant utilization, not being captured when those variables are analyzed collectively, instead of at the individual patient level. Our data also suggest that lack of health care insurance or coverage under Medicaid may be linked to the lower AHCT utilization among NHB and Hispanics as two studies have shown lower utilization of AHCT among Medicaid beneficiaries(10, 14). However, it is unlikely that insurance plays a major role among Asians as the pattern of insurance coverage was very similar to the one seen in NHW.
Prior studies addressing disparity in access to AHCT have not explored the interaction between sex and REC or have not found one(9, 10). We found however that the underutilization of AHCT among women with MM is only significant among Hispanics for reasons that are unknown.
Lastly, we estimated the impact of access disparities in AHCT volumes. Racial disparity itself prevents approximately 1 in 7 potential AHCT for MM. Among NHB, Hispanics and Asians almost half the potential transplants do not occur due to disparity in access. In addition to the possible detrimental effect on outcome from the lack of transplant therapy, it is also possible that transplantation serves as a surrogate for more advanced tertiary level care. Barriers preventing minority patients from accessing transplantation may be the same as preventing them from accessing advanced supportive care, novel agents, clinical trials and expert consultation with potential further impairment of outcomes.
As the field evolves, age is no longer considered an absolute barrier to transplantation in general(15), although only one positive randomized trial comparing transplant and non-transplant therapy in MM has included patients older than 65(16) and one study with patients 65–75 years old failed to show advantage of “reduced intensity” AHCT over conventional therapy(17). Age disparity is however the main contributor to AHCT underutilization in MM. As demonstrated in Figure 2, the evolving inclusion of AHCT as a viable therapy for older patients will sharply increase transplant volumes at a rate of approximately 6% for each one year of increase in the median age of AHCT patients. Even though this is a positive trend, it will present a further challenge due to the anticipated workforce shortage in blood and marrow transplantation (18).
In summary, race-ethnicity disparity greatly affects AHCT utilization for management of MM in US. Sex disparity plays a much lesser role, except among Hispanics. The profound age disparity is decreasing over time and will likely continue to drive major increase of AHCT activity.
Acknowledgments
The CIBMTR is supported by Public Health Service Grant/Cooperative Agreement U24-CA76518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI), and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 5U01HL069294 from NHLBI and NCI; a contract HHSH234200637015C with Health Resources and Services Administration (HRSA/DHHS); two grants, N00014-06-1-0704 and N00014-08-1-0058, from the Office of Naval Research; and grants from Allos, Inc.; Amgen, Inc.; Angioblast; Anonymous donation to the Medical College of Wisconsin; Ariad; Be the Match Foundation; Blue Cross and Blue Shield Association; Buchanan Family Foundation; CaridianBCT; Celgene Corporation; CellGenix, GmbH; Children’s Leukemia Research Association; Fresenius-Biotech North America, Inc.; Gamida Cell Teva Joint Venture Ltd.; Genentech, Inc.; Genzyme Corporation; GlaxoSmithKline; HistoGenetics, Inc.; Kiadis Pharma; The Leukemia & Lymphoma Society; The Medical College of Wisconsin; Merck & Co, Inc.; Millennium: The Takeda Oncology Co.; Milliman USA, Inc.; Miltenyi Biotec, Inc.; National Marrow Donor Program; Optum Healthcare Solutions, Inc.; Osiris Therapeutics, Inc.; Otsuka America Pharmaceutical, Inc.; RemedyMD; Sanofi; Seattle Genetics; Sigma-Tau Pharmaceuticals; Soligenix, Inc.; StemCyte, A Global Cord Blood Therapeutics Co.; Stemsoft Software, Inc.; Swedish Orphan Biovitrum; Tarix Pharmaceuticals; Teva Neuroscience, Inc.; THERAKOS, Inc.; and Wellpoint, Inc.
Footnotes
Financial disclosure statement
The authors have no financial relationship or conflict of interest to disclose
This work was presented at the 56th ASH Annual Meeting and Exposition on December 8, 2014
References
- 1.Child JA, Morgan GJ, Davies FE, et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med. 2003;348:1875–1883. doi: 10.1056/NEJMoa022340. [DOI] [PubMed] [Google Scholar]
- 2.Attal M, Harousseau JL, Stoppa AM, et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Francais du Myelome. N Engl J Med. 1996;335:91–97. doi: 10.1056/NEJM199607113350204. [DOI] [PubMed] [Google Scholar]
- 3.Kristinsson SY, Landgren O, Dickman PW, Derolf AR, Bjorkholm M. Patterns of survival in multiple myeloma: a population-based study of patients diagnosed in Sweden from 1973 to 2003. J Clin Oncol. 2007;25:1993–1999. doi: 10.1200/JCO.2006.09.0100. [DOI] [PubMed] [Google Scholar]
- 4.Schaapveld M, Visser O, Siesling S, Schaar CG, Zweegman S, Vellenga E. Improved survival among younger but not among older patients with Multiple Myeloma in the Netherlands, a population-based study since 1989. Eur J Cancer. 2010;46:160–169. doi: 10.1016/j.ejca.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Brenner H, Gondos A, Pulte D. Recent major improvement in long-term survival of younger patients with multiple myeloma. Blood. 2008;111:2521–2526. doi: 10.1182/blood-2007-08-104984. [DOI] [PubMed] [Google Scholar]
- 6.Kumar SK, Dingli D, Lacy MQ, et al. Autologous stem cell transplantation in patients of 70 years and older with multiple myeloma: Results from a matched pair analysis. American journal of hematology. 2008;83:614–617. doi: 10.1002/ajh.21191. [DOI] [PubMed] [Google Scholar]
- 7.Sharma M, Zhang MJ, Zhong X, et al. Older Patients with Myeloma Derive Similar Benefit from Autologous Transplantation. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2014 doi: 10.1016/j.bbmt.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hari PN, Majhail NS, Zhang MJ, et al. Race and outcomes of autologous hematopoietic cell transplantation for multiple myeloma. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2010;16:395–402. doi: 10.1016/j.bbmt.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joshua TV, Rizzo JD, Zhang MJ, et al. Access to hematopoietic stem cell transplantation: effect of race and sex. Cancer. 2010;116:3469–3476. doi: 10.1002/cncr.25297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Hamadani M, Hashmi SK, Go RS. Use of autologous hematopoietic cell transplantation as initial therapy in multiple myeloma and the impact of socio-geo-demographic factors in the era of novel agents. American journal of hematology. 2014 doi: 10.1002/ajh.23753. [DOI] [PubMed] [Google Scholar]
- 11.Costa LJ, Zhang MJ, Zhong X, et al. Trends in utilization and outcomes of autologous transplantation as early therapy for multiple myeloma. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2013;19:1615–1624. doi: 10.1016/j.bbmt.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Surveillance Epidemiology and End Results. SEER Data, 1992–2011. Bethesda, MD: Surveillance Research Program, National Cancer Institute; 2012. [Google Scholar]
- 13.Nietfeld JJ, Pasquini MC, Logan BR, Verter F, Horowitz MM. Lifetime probabilities of hematopoietic stem cell transplantation in the U. S. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2008;14:316–322. doi: 10.1016/j.bbmt.2007.12.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warren JL, Harlan LC, Stevens J, Little RF, Abel GA. Multiple myeloma treatment transformed: a population-based study of changes in initial management approaches in the United States. J Clin Oncol. 2013;31:1984–1989. doi: 10.1200/JCO.2012.46.3323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michaelis LC, Hamadani M, Hari PN. Hematopoietic stem cell transplantation in older persons: respecting the heterogeneity of age. Expert review of hematology. 2014;7:321–324. doi: 10.1586/17474086.2014.913978. [DOI] [PubMed] [Google Scholar]
- 16.Palumbo A, Bringhen S, Petrucci MT, et al. Intermediate-dose melphalan improves survival of myeloma patients aged 50 to 70: results of a randomized controlled trial. Blood. 2004;104:3052–3057. doi: 10.1182/blood-2004-02-0408. [DOI] [PubMed] [Google Scholar]
- 17.Facon T, Mary JY, Hulin C, et al. Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99-06): a randomised trial. Lancet. 2007;370:1209–1218. doi: 10.1016/S0140-6736(07)61537-2. [DOI] [PubMed] [Google Scholar]
- 18.Gajewski JL, LeMaistre CF, Silver SM, et al. Impending challenges in the hematopoietic stem cell transplantation physician workforce. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2009;15:1493–1501. doi: 10.1016/j.bbmt.2009.08.022. [DOI] [PubMed] [Google Scholar]