Abstract
Objective
The goal of this article is to review the published literature on laparo-endoscopic single-site surgery (LESS) in gynecology and to present current advances in instruments for LESS surgery.
Methods
A review of the current literature on the use of laparo-endoscopic single-site surgery in gynecology was performed. In addition, a review of currently available techniques for peritoneal access and specialized instruments was done.
Results
As LESS surgery is relatively novel, the current literature on use of this technique in gynecology is somewhat limited. A total of 16 publications were available for the review of literature (10 case series, 2 comparative studies, 3 case reports and 1 surgical technique demonstration). In recent years, however, improvement in traditional laparoscopic techniques and availability of more advanced instruments has made single-incision laparoscopy more feasible and safer for the patient. There is increasing interest in the LESS surgery both as an alternative to traditional laparoscopy and as an adjunct to robotic surgery when performing complicated procedures through a single incision.
Conclusion
LESS surgery provides another option in the arena of minimally invasive gynecologic surgery. The ultimate role of this approach in gynecologic surgery remains to be determined.
Introduction
With the success of laparoscopic surgery in the last decade in gynecology, most gynecologic surgeons would agree that minimally invasive surgery for appropriately chosen patients provides a clear advantage in terms of both patient outcomes and cost [1, 2]. One of the more recent advances in the field of minimally invasive gynecology is the increasing utilization of single-port laparoscopic surgery. This minimally invasive approach to surgery requires only 1 entry point, typically in the umbilical region.
Single-port laparoscopic surgery has been described in the literature using a number of other terms, including single-port access surgery (SPA), single-incision laparoscopic surgery (SILS), embryonic natural-orifice trans-umbilical endoscopic surgery (E-NOTES), and trans-umbilical endoscopic surgery (TUES). A recently convened consortium at the Cleveland Clinic agreed to use the term laparo-endoscopic single-site surgery (LESS surgery) to describe techniques in which a single incision is used to accomplish laparoscopic surgery [3].
LESS surgery is another attempt at improving cosmetic results, decreasing hospital stay, and facilitating faster recovery. Reduction in the number of ports would also mean reduction in the port-associated complications like hernias, vascular as well as soft tissue traumatic injuries during trocar insertion and nerve injuries. So far the comparative peri-operative outcomes and short-term measures have established the safety of LESS surgery both in gynecologic surgery [4] and other surgical specialties [5–8]. The goal of this article is to review the published literature on LESS surgery in gynecology, discuss the current advances in instrumentation for LESS surgery and discuss potential future roles of LESS surgery.
Development of LESS Surgery in Gynecology
The concept of single-port minimally invasive surgery in gynecology dates back to 1969, when Wheeless [9] reported single-incision laparoscopy for female sterilization. In the 1970s, several gynecologists conducted laparoscopic tubal ligations through a single umbilical incision [10].
The ability to perform complex procedures through a single incision has only recently been realized. Among the former limitations included limited instrumentation, lighting, and access ports. In recent years, however, improvement in traditional laparoscopic techniques and availability of more advanced instruments has made single-incision laparoscopy more feasible and safer for the patient. To date, LESS surgery has been described for cholecystectomy [11–15], appendectomy [16–24], nephrectomy [5, 6, 25–27], colectomy [28–30], adrenalectomy [31–33] and bariatric surgery [34]. LESS surgery has also been described in gynecology; although experience with this approach is limited and the accompanying literature is sparse (Table 1).
Table 1.
LESS procedure in gynecology
| Year, Authors, Reference |
Publication Type |
Type of Surgery | No. of Patients |
Incision Size |
Access Port Used |
Median Operating Time (Range) |
Complications (Including Conversion to Open Procedure) |
|---|---|---|---|---|---|---|---|
| Yim et al [7] | Comparative study |
Single-port TLH vs. Conventional TLH |
SP-TLH (52) and TLH (105) |
1.2 –1.5 cm |
Wound retractor and surgical glove |
SP-TLH 117 min (54–195) and TLH 110 (45–253) |
2/52 SP-TLH ( 1 1 wound infection); 10/105 TLH |
| Song et al [54] |
Case Series | LAVH (uterus >500 gm) |
15 | 2 cm | Wound retractor and surgical glove |
125 min (80–236) |
2 patients – additional port needed. |
| Mereu et al [53] |
Case series | Removal of various benign adnexal masses |
16 | 2 – 2.5 cm |
S-Portal X-Cone, curved instruments |
42 min (20–72) |
1 patient with wound infection |
| 2010, Escobar et al [52] |
Case Series | Removal of various benign adnexal masses |
9 | 1.5 – 2 cm |
SILS port (Covidien |
N.A. | 1 patient with stage endometriosis required additional trocars. |
| 2010, Kim et al [4] |
Comparative study |
Single port LAVH vs conventional LAVH |
43 in each group |
1.5 – 2 cm |
Wound retractor and surgical glove |
SPA - 119 min (87–151); Conventional 124 mins (61–187) |
Laparotomy SPA=Conventional=2; Need for additional trocars SPA=3 |
| 2010, Yoon et al [51] |
Case Series | Supracervical hysterectomy with trans-cerivcal uterine morcellation |
7 | 2 cm | Wound retractor and surgical glove |
157 min (140–233) |
None |
| 2009, Fader et al [38] |
Case Serie | Malignancies (Endometrial cancer staging (n = 1), ovarian cancer staging (n = 1), retroperitoneal pelvic lymph node dissection (n = 1), risk-reducing extrafascial hysterectomy and BSO (n = 2), risk-reducing BSO alone (n = 5), ovarian cystectomy (n = 1) and BSO for complex adnexal masses (n = 2) |
13 | 2–3 cm | SILS port (Covidien) for laparoscopy and GelPort (Applied Medical) for robotic surgery |
65 min (35–178) |
None |
| 2009, Escobar et al [36] |
Case Report/Descri ption of Surgical Technique |
1 | 3 cm | GelPort multichannel trocar (Applied Medical) and Da Vinci robo |
168 min | None | |
| 2009, Lee et al [49] |
Case Series | Laparoscopic- assisted vaginal hysterectomy |
24 | Wound retractor, surgical glove, 5-mm laparoscope, flexible instruments (Cambridge Endosurgery) |
|||
| 2009, Fagotti et al [48] |
Case Series | Ovarian cyst enucleation |
3 | 2 cm | TriPort (Advanced Surgical Concepts) and EndoEYE deflectable- tip video laparoscope (Olympus America) |
79.6 min (79–100) |
None |
| 2009, Langebrekke A and Qvigstad E [47] |
Case Report | Hysterectomy | 1 | 1.5 cm | TriPort (Advanced Surgical Concepts) and EndoEYE deflectabletip video laparoscope (Olympus America) |
60 min | None |
| 2009, Kim et al [46] |
Case series | Adnexal surgery (BSO (n = 2), USO (n = 11) and ovarian cystectomy (n = 11) |
24 | 2 cm | Wound retractor, surgical glove, 5-mm laparoscope, flexible instruments (Cambridge) |
70 min (40– 120 min) |
Additional trocar needed (1 case). Conversion to staging laparotomy (1 case). |
| 2009, Lim et al [44] |
Case Series | Adnexal surgery (BSO (n = 6), paratubal cystectomy (n = 3), USO (n = 2), ovarian cystectomy (n = 2), myomectomy (n = 1), inguinal lipoma excision (n = 1), and intramural cornual resection (n = 1 |
12 | 2 cm | Wound retractor and surgical glove |
73 min (25– 110) |
None |
| 2005, Ghezzi et al [43] |
Case Report | Salpingectomy for treatment of tubal pregnancy |
10 | 1 cm | Operative Laparoscope and percutaneous suture |
27 min (15– 37) |
None |
| 2001, Kosumi et al [42] |
Case Report | Ovarian Cystectomy |
1 | 1 cm | Operative Laparoscope |
N/A | None |
| 1992 Pelosi et al [41] |
Case Series | Laparoscopic supracervial hysterectomy |
4 | 1 cm | Operative Laparoscope |
N/A | None |
- LAVH – Laparoscopically-assisted vaginal hysterectomy
- BSO - Bilateral Salpingo-ophorectomy
- USO – Unilateral Salpingo-ophorectomy
Instruments for LESS Surgery
Abdominal Access
There are 3 approaches to completing laparoscopic surgery via a single incision. The first is to employ an operative laparoscope; this approach has been widely used by gynecologists to perform tubal ligations. An operative scope, which has a channel along the scope shaft allows for the entry of bipolar cautery to carry out the coagulation of fallopian tubes. Second is to make a single incision in the skin and multiple incisions in the fascia with small bridges cut between the fascial incisions to allow for organ retrieval [8, 35]. With this approach, multiple 5- to 10-mm trocars are inserted next to each other to access the abdominal cavity. Third, and a more recent option, is to use specialized access ports with multiple channels for access to the abdominal cavity. These commercially available specialized access ports are discussed in the following paragraphs and are summarized in Table 2.
Table 2.
Comparison of various ports
| Category | Device/ Method |
Advantages | Disadvantages |
|---|---|---|---|
| Access Port | Multiple fascial incisions with low profile conventional ports |
|
|
| Wound retractor and surgical glove |
|
|
|
| SILS port |
|
|
|
| Gelpoint/Gelport |
|
|
|
| Airseal |
|
|
AirSeal
AirSeal ports (SurgiQuest, Orange, CA) (Fig. 1) use air pressure to create pneumoperitoneum. The flow of air around the port at a pressure much higher than pneumoperitoneum creates the “AirSeal.” The biggest advantage of this system is that it eliminates smoke because of the constant circulation of air. The new AirSeal port’s oval design is advantageous for single-port laparoscopy because it allows better access to multiple instruments. The major disadvantages of the AirSeal system are the noise associated with the AirSeal device and the absence of a fulcrum point since the device is open at the instrument entry site.
Fig. 1.
Access Ports: (A) AirSeal port (SurgiQuest, Orange, CA) (B) SILS port (Covidien, Mansfield, MA) (C) TriPort multichannel access port (Advanced Surgical Concepts, Ireland) (D) GelPort laparoscopic system (Applied Medical, Rancho Santa Margarita, CA)
Ethicon Endo-Surgery SSL Access System
Ethicon (Ethicon Endo-Surgery, Cincinnati, OH) recently introduced its single port access system. The SSL Access System consists of two 5mm seals and a larger 15mm seal in a low profile design that allows surgeons to use a wide variety of instrumentation across several different procedures. The device consists of a retractor and a seal cap. The two sizes of the retractors allow proper placement depending on the depth of abdominal wall, the smaller 2 cm retractor for walls up to 4 cm and larger 4 cm retractor for abdominal wall up to 7 cm. A single incision between 1.5 – 3.5 cm is required for insertion of this port. Unique to the device is the 360-degree rotation of the seal cap, which enables quick re-orientation of instruments during procedures and reduces the need for instrument exchanges.
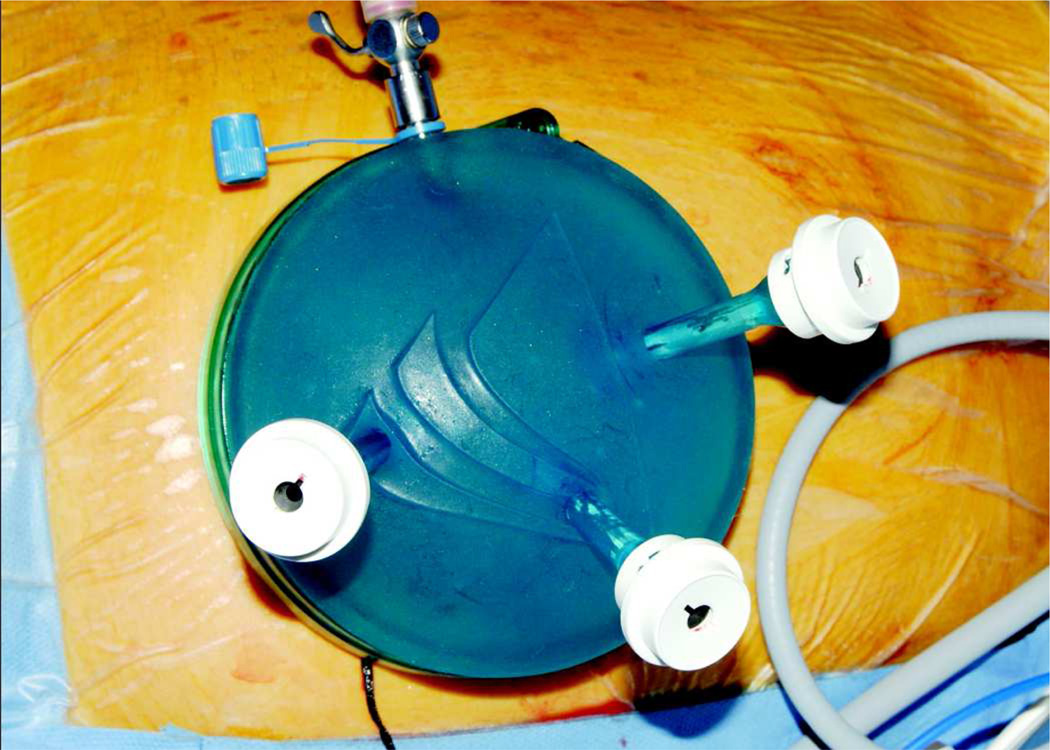
GelPort and GelPOINT Systems
The GelPort laparoscopic system (Applied Medical, Rancho Santa Margarita, CA) (Fig. 1) consists of a wound retractor with a flexible inner ring connected to an outer ring with a clear sheath. The inner ring is inserted with an open technique; the retractor can be used in incisions from 1.5 to 7 cm. The outer ring has a diameter of about 10 cm. A GelSeal cap fits over the outer ring. The GelPort system has previously been used for hand-assisted laparoscopy. Passing multiple trocars of varying lengths through the gel interface easily modifies the GelPort for single-port laparoscopy. The advantages of the GelPort system for LESS surgery include the versatility of the GelSeal cap, which allows placement of instruments of different shapes and sizes, and the 10-cm diameter of the outer ring, which reduces instrument crowding. Fader and Escobar used the GelPort system for robotically assisted LESS surgery in gynecology [36]. They reported that the larger outside dimension of the GelSeal cap reduces the crowding of the robotic arms (Fig 3). A recent retrospective review of the GelPort system in pelvic surgery concluded that this system is favorable to single-port surgery as the device provides a circumferential access and retraction [37].
Fig. 3.
Olympus deflectable-tip EndoEYE video laparoscope (Olympus America, Center Valley, PA).
The GelPOINT platform is a dedicated modification of the GelPort system available for single-port laparoscopy in which along with the GelSeal cap 4 small cannulas are provided by the manufacturer for easier insertion of laparoscopic instruments through the gel interface. One of the disadvantages of the GelPort system is the large slit in the GelSeal which can leak gas at times. The addition of GelSeal cap in the GelPOINT platform has alleviated this problem.
SILS Port
Covidien (Mansfield, MA) offers 2 products for LESS surgery—the SILS port (Fig. 1) and the SILS kit. The SILS port is a flexible laparoscopic port, which necessitates a fascial incision of 1.8 – 3 cms and can accommodate up to 3 instruments through a single incision. The SILS kit includes the SILS port and Roticulator instruments. The port is made of elastic polymer and fits fascial incisions of about 2 cm. The advantages of the SILS port include the availability of the dedicated SILS kit with multiple compatible instruments and open Hassan entry into the peritoneal cavity. Another advantage of the SILS port is that individual ports use a traditional laparoscopic seal, which helps minimize gas leak.
In the only series reported to date on LESS surgery in gynecologic oncology, Fader and Escobar used the SILS port for most of their laparoscopic cases [38].
TriPort and QuadPort
TriPort and QuadPort (Advanced Surgical Concepts, Co Wicklow, Ireland) are multichannel access ports.
TriPort (Fig. 1) has two 5 mm ports and one 12 mm port and can be used with fascial incisions ranging from 12 to 25 mm. The port has an outer, proximal ring to which the 3 ports and an insufflation line are attached. A retracting sleeve runs through the outer ring both upwards and downwards. The lower end of the sleeve is attached to a distal ring.
For insertion, a skin incision is made, and the distal ring is loaded into an introducer. The introducer is used to bluntly pierce the abdominal wall and push the distal ring into the abdominal cavity. Then the introducer is removed, the retracting sleeve is grasped at the proximal end and the outer ring is passed downwards over it to create a tight seal with the abdominal wall. The excess sleeve is then cut away.
This system has several advantages. First, multiple instruments can be placed and removed without loss of pneumo-peritoneum. Second, the system fits a wide range of depths of abdominal wall. Third, the angle of the different ports helps reduce instrument crowding.
The major disadvantages are the maximum depth of 10 cm, which limits use of the system in obese patients, and the possibility of sleeve damage resulting in loss of pneumo-peritoneum.
QuadPort is similar to TriPort but provides 4 ports—one 5-mm port, one 15-mm port, and two 10-mm ports. The device can be used with fascial incisions ranging from 25 to 65 mm. The QuadPort has an advantage over the TriPort when organ retrieval would necessitate a fascial incision between 25 and 65 mm.
In our experience, both TriPort and QuadPort have fragile valves at each access site and damage leads to potential of slow loss of pneumoperitoneum, especially in longer cases. Lubrication of instruments is necessary to prevent the valve damage.
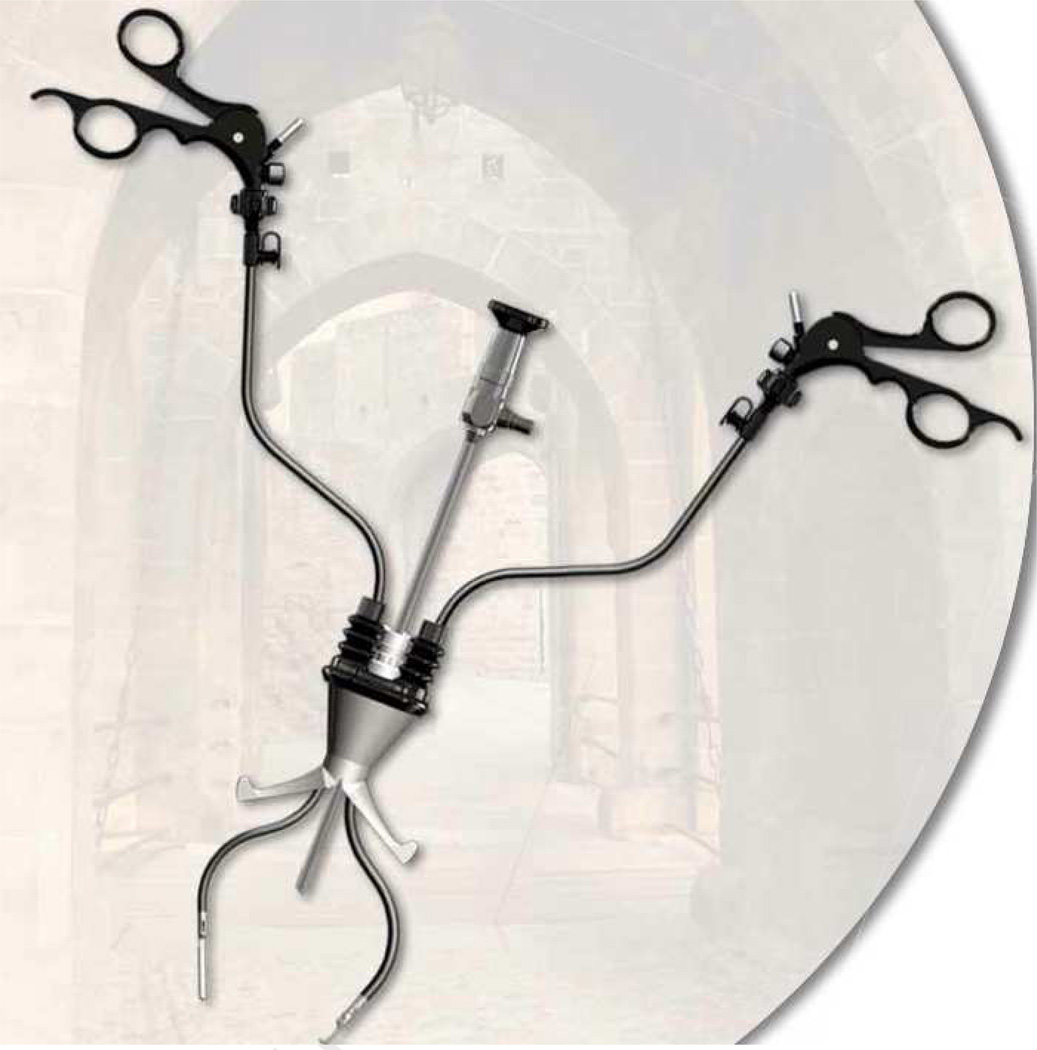
X-Cone and Endocone
X-Cone and Endocone (Karl Storz, Tuttlingen, Germany) are the reusable single port access devices, which are 2–2.5 and 3.5 cm in diameter respectively. The devices when used in tandem with specially designed curved instruments are developed to enhance the triangulation in single port surgery (Fig 5). These devices are not yet FDA approved for use in United States.
Fig. 5.
X-Cone access port and S-Portal curved instruments (Karl Storz, Tuttlingen, Germany), the first generation of curved coaxial instruments with double bending.
Operating Instruments
Traditional laparoscopy is constrained by the combination of long, rigid instruments and fixed trocar sites with only 4 degrees of freedom, which limits surgeon dexterity. The newer surgical instruments provide 7 degrees of freedom and may play an important role in adoption of single-port surgery. The following are the most common specialized instruments currently available in the market for facilitating LESS surgery.
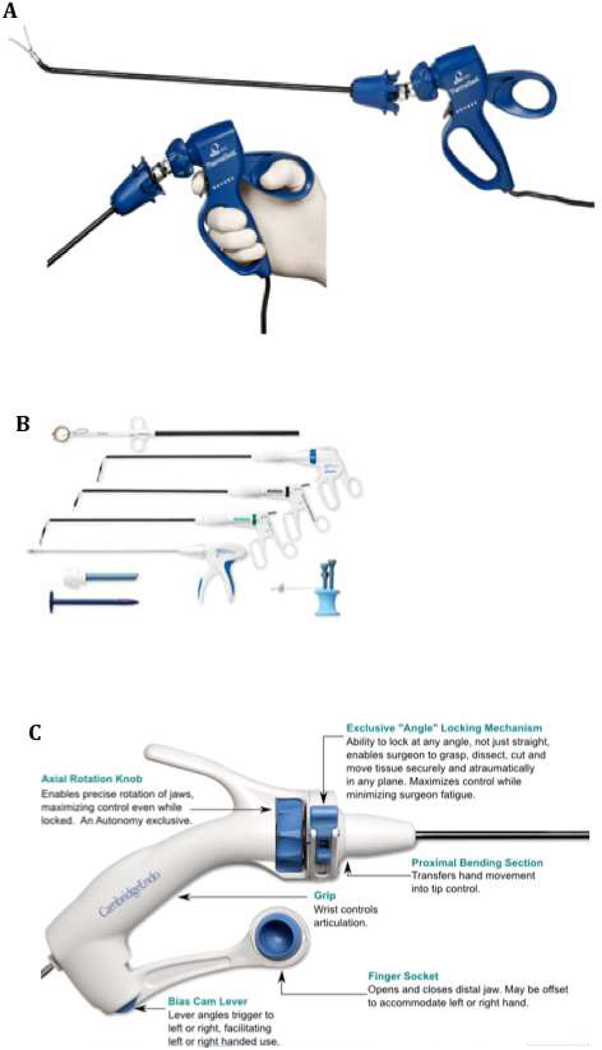
RealHand Instruments
RealHand high-dexterity instruments (Novare Surgical, Cupertino, CA) are 5-mm instruments in which the handle is connected to the tip by several cables, which allow for 360-degree articulation that mimics the movement of the surgeon’s hand and therefore provide 7 degrees of freedom of movement. The initial experience in using these instruments in gynecology was reported by Rettenmaier et al. in the setting of traditional 3-point laparoscopy [39]. One of the major potential advantages of these instruments is the dexterity that they allow the surgeon. This allows the surgeon to overcome limited triangulation. Currently, 11 different instrument tips are available under the RealHand brand, including the ThermaSeal tip, which utilizes thermal energy to denature protein structures and create high-integrity seals and clean divisions. Other tips available are standard graspers, scissors, and needle holders with added range of movement (Fig. 2). The potential disadvantages of these instruments include a steep learning curve and a relatively high cost.
Fig. 2.
Instruments for LESS Surgery (A) RealHand high-dexterity instruments (Novare Surgical, Cupertino, CA) (B) SILS kit for LESS surgery with Roticulator instruments (Covidien, Mansfield, MA) (C) Autonomy Laparo-Angle instruments (Cambridge Endoscopic Devices, Framingham, MA)
Autonomy Laparo-Angle Instruments
Like the RealHand instruments, Autonomy Laparo-Angle instruments (Cambridge Endoscopic Devices, Framingham, MA) provide a 360-degree articulating head, which mimics the surgeon’s movements. Unlike the RealHand instruments, the Autonomy Laparo-Angle instruments include a mechanism to rotate the instrument head after locking at any angle and a finger socket to open and close the distal jaws (Fig. 2). There is a proximal bending section, which translates the movements of the surgeon’s wrist to the tip of the instrument. There is also an “angle” locking mechanism to lock the distal tip in any angle to facilitate a better working angle on the outside. The current line of Autonomy instruments includes a needle holder, Metzenbaum scissors, dissecting hook, Maryland dissector, and graspers.
SILS Kit with Roticulator Instruments
The SILS kit for LESS surgery (Covidien, Mansfield, MA) is made to accompany the SILS port, which was described above. The SILS kit includes Roticulator instruments. These instruments have distal ends with limited range of movement: 0–80 degrees. As the distal end is pushed out from its outer sheath, the extended bent portion’s angle increases. The handle also allows the surgeon to rotate the distal instrument 360 degrees, similar to what is possible with traditional laparoscopic instruments (Fig. 2). The instrument tips include dissectors, scissors, and graspers. Several of the roticulator instruments have monopolar cautery attachments. The major advantages of these instruments include their availability as a SILS kit, which minimizes compatibility issues, and the fact that these instruments are cheaper than RealHand or Laparo-Angle instruments. The disadvantages include the limited movement of the instrument tip, which does not allow translation of the surgeons’ hand movements, as is possible with RealHand or Laparo-Angle instruments.
Cameras
Traditional 5-mm and 10-mm cameras can be used for LESS surgery. However, the use of traditional laparoscopy cameras increases the instrument crowding. There are three ways to reduce the crowding and hence providing a stable image during the procedure. First and one of the cheaper alternatives is to use the bariatric length, rigid 5-mm scopes to off-set the instrument length during the surgery and hence reduce the crowding. Second, is to use laparoscopic camera–scope combination with an in-line light cord and a low-profile camera head to reduce the tangling of light source coming in at a 90 degree angle in a traditional laparoscopic camera. Third, is to use the specialized laparoscopic camera for single port surgery with a deflectable tip. The Olympus deflectable-tip EndoEYE video laparoscope (Olympus America, Center Valley, PA) (Fig. 3) was approved by the Food and Drug Administration in 2005 and has been commercially available since then, long before single-port surgery became mainstream. This laparoscope has an outer diameter of 5-mm for standard video resolution camera and 10 mm for the high definition video resolution camera. The distal tip is flexible and hosts the camera allowing enhanced angulation range. The major advantage of use of the deflectable-tip EndoEYE in single-port surgery is that less movement is necessary at the port site to move the camera, which reduces collision with other instruments in the limited space. The major disadvantages of this scope are incompatibility with other video platforms necessitating an entire new setup and hence relatively high cost.
Stryker (Stryker Corporation, Kalamazoo, MI) also markets the “IDEAL EYES HD” articulating laparoscope with an inline design providing about 100 degrees of flexion in all directions.
LESS Surgery in Gynecology
As LESS surgery is relatively novel, the current literature on use of this technique in gynecology is somewhat limited (Table 1). Wheeless, after reporting the first single-incision laparoscopic tubal ligation in 1969 [9], later published, together with Thompson, a series of 3600 women who underwent sterilization with this technique [40]. In 1992, Pelosi et al. [41] reported the first successful supra-cervical hysterectomy performed through a single incision. Four patients underwent the procedure.
In 2001, Kosumi et al [42] used an operative laparoscope to perform ovarian cystectomy through a single incision. In 2005, Ghezzi et al. [43] reported a novel single-port technique for the treatment of tubal pregnancy. Using an operative laparoscope and a percutaneous midline suture inserted with a straight needle, the surgeon pulled the affected fallopian tube towards the midline. Bipolar cautery was then used in combination with laparoscopic scissors to dissect the tube. Using a laparoscopic retrieval bag, the tube was then removed through the umbilical incision. A total of 10 ectopic pregnancies, with a median gestational age of 7 weeks and 2 days (range, 5.6–10.2 days), were treated with this technique. The median time reported for the procedure was 27 minutes (range, 15–37 minutes), and no failures or complications were reported.
In 2009, Lim et al. [44] reported a series of 12 patients who underwent single-port laparoscopic surgery for benign adnexal masses. In these patients, the single-port access was created using an innovative method of combining a wound retractor with a surgical glove, a slight modification of a technique previously described for finger-assisted laparoscopic surgery [45]. The median size of the adnexal masses was 4 cm (range, 3–9 cm). These were all performed through a 2-cm fascial incision. The mean operative time was 73 minutes (range, 25–110 minutes), and no complications were reported. The median hospital stay after surgery was 2 days (range, 2–3 days).
Also in 2009, Kim et al. [46] published a series of 24 patients who underwent adnexal surgery performed through a single port. The authors successfully completed the adnexal surgery in 22 patients; 1 patient required placement of an additional trocar for adhesiolysis and another patient required staging laparotomy for a borderline malignancy after successful completion of single port adnexal surgery. The access port used was a combination of a wound retractor and a surgical glove as described by Lim et al.[44]. The median size of the adnexal mass was 5 cm (range, 3–12 cm). The median operative time was 70 minutes (range, 40–128 min). Median time for preparation for single-port access was 6 minutes (range, 5–15 minutes). Estimated blood loss was 10 mL (range, 10–100 mL). There were no intraoperative complications. The median postoperative hospital stay was 1 day (range, 1–3 days).
Langebrekke et al [47] in 2009 reported the first total laparoscopic hysterectomy through a single incision. TriPort access device with EndoEye camera were used for the procedure. Fagotti et al [48] reported the used a similar setup for ovarian cyst enucleation in 3 patients. Lee et al. [49] recently reported a series of 24 patients who underwent laparoscopic-assisted vaginal hysterectomy. The combination of wound retractor and a surgical glove was used for abdominal access. Distal articulating instruments were used for performing the surgery. The authors also did a sub-analysis to compare the first 10 cases with the last 14 cases and found a trend towards decreasing operative time and significantly less blood loss and shorter hospital stay with increasing surgeon experience. There were 3 conversions to open laparotomy because of adhesions.
The use of trans-cervical morcellation was recently reported in the setting of conventional laparoscopic supra-cervical hysterectomy by Rosenblatt et al [50]. Yoon et al [51] have recently described the use of this novel method of morcellation using a single-port access in 7 patients. Mean operating time was 157 minutes (range, 140–233 minutes). After transecting the uterine corpus, cervical os was dilated to number 15 hegars dilator and morcellator was introduced. The mean morcellation time reported was 35 minutes (range, 140–233 minutes). Mean EBL reported was 200 ml (range, 100–300 ml) and no intra-operative or post-operative complications were noted.
Kim et al [4] recently published a comparative study comparing LESS with conventional laparoscopy in cases of laparoscopic assist vaginal hysterectomy. The VAS-based pain scores at 24 h (LESS, 2.5 ± 0.7; conventional, 3.5 ± 0.8; p=0.01) and 36 h after surgery (LESS, 1.7 ± 1.2; conventional, 2.9 ± 1.1; p=0.01) were lower in the LESS group. Other intra-operative and peri-operative outcomes were similar in two groups. Also in 2010, Escobar et al [52] successfully reported removal of benign adnexal masses in 9 patients using SILS port.
Mereu et al [53] reported their experience of single-port access surgeries in 16 patients undergoing procedures for benign adnexal pathologies. 9 salpingo-ophorectomies, 5 ovarian cyst enucleation and 2 salpingectomies were performed. This group used specialized curved instruments in combinations with X-cone S-portal (Karl Storz, Tuttlingen, Germany) and reported a much lower mean operating time of 42 min (range, 20–72 min) in their cohort.
Yim et al [7] reported a comparative study of single-port access total hysterectomy (SPA-TLH) versus conventional total hysterectomy (TLH). The single-port access used was the combination of a wound retractor and surgical glove. The SPA-TLH group had less intra-operative blood loss, shorter hospital stay and earlier diet intake. No difference in peri-operative complications was noted. The authors successfully repaired the vaginal cuff laparoscopically in 38 of 52 cases in the SPA-TLH group.
Song et al [54] reported their technique of laparoscopic-assisted vaginal hysterectomy for large uterus weighing more than 500 grams. 13 of the 15 patients enrolled successfully underwent the single-port procedure. 2 patients required additional ports. The median operation time, weight of the uterus, and estimated blood loss were 125 minutes (80 to 236 minutes), 690 g (503 to 1260 g), and 500 mL (150 to 1000 mL), respectively. No peri-operative complications were reported.
Fader and Escobar [38] were the first to publish on single-port surgery in patients with gynecologic malignancies. Thirteen patients underwent single-port surgery; 9 cases were done laparoscopically and 4 cases were done using the Da Vinci robotic system through a single incision. The median patient age was 47 years (range, 34–60 years), and the median body mass index was 28 (range, 20–37). All the procedures were performed successfully without the need for conversion to laparotomy and there were no reported post-operative complications. The median operating time was 65 minutes (range, 35–178 minutes). The mean hospital stay was 0.7 days (standard deviation, 0.5 days). Eleven of the 13 patients reported a pain score of 0–1 in the immediate postoperative period and follow-up, 8 (62%) patients received ketorolac only after surgery, and no narcotics were used in the outpatient setting. Two (15%) patients reported pain scores of 3–4 in the postoperative period and required intravenous narcotics and oral narcotics after discharge from the hospital.
Technical Challenges of LESS Surgery
Despite the development of novel instruments and access ports, there remain several technical challenges in operating through a single port. The following are some of the most common technical challenges that may be encountered in single-port surgery.
Instrument Crowding
Crowding of the instruments inserted through a single port is a major problem in LESS surgery. Range of movement is limited because of the close proximity of the instruments. There are several ways of overcoming this problem. First, surgeons can cross the instruments. However, this may lead to counterintuitive movements as the surgeon controls the instrument on the opposite side of the field. The second option is to use the Da Vinci robot with swapping of the laterality of the arms. However, this might not be a viable solution to simple cases as it adds to both operating time and cost. Another option is to use the GelPOINT access device with a larger outer cap to increase the instrument distance.
Loss of Triangulation
Triangulation is a necessity in traditional laparoscopy. With rigid instruments and ports that provide minimal flexibility, the safest and easiest way to perform laparoscopy is through triangulation of instruments. But with single incision accommodating both the camera and the instruments there is a loss of triangulation. With currently available instruments, which include both rigid instruments and the instruments with a articulating tip, there is minimal room for triangulation. The development of proximally deviating curved coaxial instruments with double bending will give the surgeon the impression of using triangulation without crossing hands while ensuring minimal interference at the instrument introduction site. The first generation of curved instruments is the X-Cone access port and S-Portal curved instruments (Karl Storz, Tuttlingen, Germany) (Fig. 5). These instruments, however, are not yet available in the US. Pre-bent instruments (Olympus, Hamburg, Germany) have also been shown to out perform the flexible/articulating instruments in the laboratory setting [55] and may reduce instrument crowding in addition to providing enhanced triangulation.
Learning Curve
The learning curve for laparoscopic gynecologic procedures [56–59] and robotic gynecologic procedures [60] has already been described. The move from laparoscopic to robotic surgery had several advantages. There is evidence that novice surgeons acquire robotic surgery skills faster than traditional laparoscopy skills [61]. Better visualization and the enhanced dexterity of the robotic arms made the adoption of robotic surgery easier for surgeons but still involved a steep learning curve. Single port surgery, on the other hand, might not be as easy to learn given the high level of skill and technical ability required to overcome many of the aforementioned obstacles. This may lead to a difficult and long learning curve, and it is imperative that surgeons who attempt this novel surgical approach be at least highly proficient in traditional laparoscopy.
Need for Long-term Follow-up and Prospective Data on LESS Surgery
No prospective data are available on long-term complications with LESS surgery. Currently, there are no studies of patient preference comparing a single 2- to 3-cm scar from a single trocar to multiple small 5-mm scars from traditional laparoscopy or robotic surgery. Finally, data on the safety of single-port laparoscopic procedures in gynecologic cancer patients is also very limited.
Conclusion
According to the results of a recent Cochrane review, the laparoscopic approach for hysterectomy has been shown to be superior to laparotomy in terms of speedier return to normal activities, lower intra-operative blood loss, a smaller drop in hemoglobin level, a shorter hospital stay, and fewer wound or abdominal wall infections [2]. In addition, laparoscopic surgery for hysterectomy has been found to be cost-effective as the shorter hospital stay and lower morbidity offset the initial cost of the procedure [62]. LESS surgery—with the entire surgery performed through a 2-cm incision hidden in the umbilicus—has clear cosmetic benefits, but the advantages over traditional 3-port laparoscopy will have to be investigated with larger sample sizes. The available comparative studies between LESS and traditional laparoscopic assisted vaginal hysterectomies by Kim et al [4] and Yim et al [7] does provide evidence suggesting reduced post operative pain in LESS group and comparable outcomes to traditional laparoscopy. The recently reported study by Song et al [54] in successfully completing laparoscopically assisted vaginal hysterectomies in large uteri (>500 grams) certainly challenges the boundaries of single-port laparoscopic surgery. Unfortunately, the data available at this time on single-port laparoscopy are too limited to permit drawing any conclusions about long-term outcomes and benefits.
Future of LESS surgery
There are several key areas in LESS surgery that require further investigation. One of the most exciting areas is the use of the Da Vinci robot to perform surgery through a single incision. An initial report by Fader et al [38] shows a promising new approach in which the limitations of single-port access might be overcome by the enhanced instrumental dexterity of the robot. There is also potential for development of smaller robotic arms, specifically geared towards entry through dedicated 2- to 3-cm ports, to improve range of motion.
Another potential area of development is the trans-abdominal magnetic anchoring system (MAGS), which controls intra-abdominal laparoscopic camera and working instruments first described by Park et al [63]. The system uses magnetic anchors outside of abdominal wall to provide unrestricted intra-abdominal movements of the instruments and providing better working angles, which are comparable to traditional laparoscopy. The system has been evaluated in porcine models with two successful nephrectomies and trans-vaginal cholecystectomies [64, 65]. Although under development there are a few case reports using MAGS camera system in LESS surgery in humans, the largest series by Dominguez et al [66] describes the use of neodymium magnetic forceps in 40 patients undergoing single port cholecystectomy.
Another area of interest as LESS surgery gains popularity is resident and fellow training [49]. Minimally invasive cases are now divided among 3 different modalities—traditional laparoscopy, robotic surgery, and now LESS surgery. Teaching surgeons-in-training 3 different ways of performing the same surgical procedure within the same training period may present a challenge. A more structured curriculum will be needed for implementation of more advanced minimally invasive surgical techniques during resident and fellowship training.
Fig. 4.
Single-port access created using Gelpoint device.
Acknowledgement
The authors would like to thank Ms. Stephanie P. Deming for her editorial assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
Shitanshu Uppal, MD, has no conflict of interest to declare.
Michael Frumovitz, MD, is a speaker for Covidien (Boulder, CO) and Ethicon Endosurgery (Cincinnati, OH).
Pedro Escobar, MD, is a speaker for Covidien (Boulder, CO), Ethicon EndoSurgery (Cincinnati, OH)., and Olympus (Center Valley, PA).
Pedro T. Ramirez, MD, is a speaker for Covidien (Boulder, CO) and Intuitive Surgery (Sunnyvale, CA).
References
- 1.Frumovitz M, Ramirez PT, Greer M, Gregurich MA, Wolf J, Bodurka DC, et al. Laparoscopic training and practice in gynecologic oncology among Society of Gynecologic Oncologists members and fellows-in-training. Gynecol Oncol. 2004 Sep;94(3):746–753. doi: 10.1016/j.ygyno.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 2.Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;(3):CD003677. [Google Scholar]
- 3.Gill IS, Advincula AP, Aron M, Caddedu J, Canes D, Curcillo PG, 2nd, et al. Consensus statement of the consortium for laparoendoscopic single-site surgery. Surg Endosc. 2010 Apr;24(4):762–768. doi: 10.1007/s00464-009-0688-8. [DOI] [PubMed] [Google Scholar]
- 4.Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, et al. Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc. 2010 Feb 23; doi: 10.1007/s00464-010-0944-y. [DOI] [PubMed] [Google Scholar]
- 5.Raybourn JH, 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010 Jan;75(1):100–103. doi: 10.1016/j.urology.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009 May;55(5):1198–1204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 7.Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010 Jul;203(1):26, e1–e6. doi: 10.1016/j.ajog.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 8.Podolsky ER, Curcillo PG., 2nd Single port access (SPA) surgery--a 24-month experience. J Gastrointest Surg. 2010 May;14(5):759–767. doi: 10.1007/s11605-009-1081-6. [DOI] [PubMed] [Google Scholar]
- 9.Wheeless C. A rapid, inexpensive, and effective method of surgical sterilization by laparoscopy. J Reprod Med. 1969;5:255. [Google Scholar]
- 10.Quinones GR, Alvarado DA, Ley Ch E. [Tubal ligation using Yoon's ring] Ginecol Obstet Mex. 1976 Aug;40(238):127–136. [PubMed] [Google Scholar]
- 11.Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009 May;23(5):1138–1141. doi: 10.1007/s00464-009-0389-3. [DOI] [PubMed] [Google Scholar]
- 12.Chow A, Purkayastha S, Aziz O, Paraskeva P. Single-incision laparoscopic surgery for cholecystectomy: an evolving technique. Surg Endosc. 2010 Mar;24(3):709–714. doi: 10.1007/s00464-009-0655-4. [DOI] [PubMed] [Google Scholar]
- 13.Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg. 2009 Aug;75(8):681–685. discussion 5–6. [PubMed] [Google Scholar]
- 14.Hirano Y, Watanabe T, Uchida T, Yoshida S, Tawaraya K, Kato H, et al. Single-incision laparoscopic cholecystectomy: single institution experience and literature review. World J Gastroenterol. 2010 Jan 14;16(2):270–274. doi: 10.3748/wjg.v16.i2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon's initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010 Mar 1;14(3):506–510. doi: 10.1007/s11605-009-1116-z. [DOI] [PubMed] [Google Scholar]
- 16.Sesia SB, Frech M, Hacker FM, Mayr J. Laparoscopic "Single-Port" Appendectomy in Children. Zentralbl Chir. 2010 Jul 1; doi: 10.1055/s-0030-1247390. [DOI] [PubMed] [Google Scholar]
- 17.Ate O, Hakguder G, Olguner M, Akgur F. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007 Jun 1;42(6):1071–1074. doi: 10.1016/j.jpedsurg.2007.01.065. [DOI] [PubMed] [Google Scholar]
- 18.Chouillard E, Dache A, Torcivia A, Helmy N, Ruseykin I, Gumbs A. Single-incision laparoscopic appendectomy for acute appendicitis: a preliminary experience. Surg Endosc. 2010 Aug 1;24(8):1861–1865. doi: 10.1007/s00464-009-0860-1. [DOI] [PubMed] [Google Scholar]
- 19.Chow A, Purkayastha S, Paraskeva P. Appendicectomy and cholecystectomy using single-incision laparoscopic surgery (SILS): the first UK experience. Surg Innov. 2009 Sep;16(3):211–217. doi: 10.1177/1553350609344413. [DOI] [PubMed] [Google Scholar]
- 20.Inoue H, Takeshita K, Endo M. Single-port laparoscopy assisted appendectomy under local pneumoperitoneum condition. Surg Endosc. 1994 Jun 1;8(6):714–716. doi: 10.1007/BF00678574. [DOI] [PubMed] [Google Scholar]
- 21.MacDonald E, Ahmed I. Single-port laparoscopic appendicectomy. Ann R Coll Surg Engl. 2009 Sep 1;91(6):519–520. doi: 10.1308/003588409X464612h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen N, Reavis K, Hinojosa M, Smith B, Stamos M. A single-port technique for laparoscopic extended stapled appendectomy. Surg Innov. 2009 Mar 1;16(1):78–81. doi: 10.1177/1553350608330528. [DOI] [PubMed] [Google Scholar]
- 23.Rao M, Rao R. Two-port and single port laparoscopic appendicectomy. J Indian Med Assoc. 2004;102(7):360. [PubMed] [Google Scholar]
- 24.Roberts K. True single-port appendectomy: first experience with the "puppeteer technique". Surg Endosc. 2009 Aug 1;23(8):1825–1830. doi: 10.1007/s00464-008-0270-9. [DOI] [PubMed] [Google Scholar]
- 25.Stolzenburg JU, Hellawell G, Kallidonis P, Do M, Haefner T, Dietel A, et al. Laparoendoscopic single-site surgery: early experience with tumor nephrectomy. J Endourol. 2009 Aug;23(8):1287–1292. doi: 10.1089/end.2009.0120. [DOI] [PubMed] [Google Scholar]
- 26.Canes D, Berger A, Aron M, Brandina R, Goldfarb D, Shoskes D, et al. Laparo-endoscopic single site (LESS) versus standard laparoscopic left donor nephrectomy: matched-pair comparison. Eur Urol. 2010 Jan 1;57(1):95–101. doi: 10.1016/j.eururo.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 27.Desai M. Single-port surgery for donor nephrectomy: a new era in laparoscopic surgery? Nat Clin Pract Urol. 2009 Jan 1;6(1):1. doi: 10.1038/ncpuro1278. [DOI] [PubMed] [Google Scholar]
- 28.Choi S, Lee K, Park S, Lee S-H. Single port laparoscopic right hemicolectomy with D3 dissection for advanced colon cancer. World J Gastroenterol. 2010 Jan 14;16(2):275–278. doi: 10.3748/wjg.v16.i2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bucher P, Pugin F, Morel P. Single-port access laparoscopic radical left colectomy in humans. Dis Colon Rectum. 2009 Oct 1;52(10):1797–1801. doi: 10.1007/DCR.0b013e3181b551ce. [DOI] [PubMed] [Google Scholar]
- 30.Bucher P, Pugin F, Morel P. Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis. 2008 Oct 1;23(10):1013–1016. doi: 10.1007/s00384-008-0519-8. [DOI] [PubMed] [Google Scholar]
- 31.Walz MK, Groeben H, Alesina PF. Single-access retroperitoneoscopic adrenalectomy (SARA) versus conventional retroperitoneoscopic adrenalectomy (CORA): a case-control study. World J Surg. 2010 Jun;34(6):1386–1390. doi: 10.1007/s00268-010-0494-4. [DOI] [PubMed] [Google Scholar]
- 32.Walz MK, Alesina PF. Single access retroperitoneoscopic adrenalectomy (SARA)--one step beyond in endocrine surgery. Langenbecks Arch Surg. 2009 May;394(3):447–450. doi: 10.1007/s00423-008-0418-z. [DOI] [PubMed] [Google Scholar]
- 33.Castellucci SA, Curcillo PG, Ginsberg PC, Saba SC, Jaffe JS, Harmon JD. Single port access adrenalectomy. J Endourol. 2008 Aug;22(8):1573–1576. doi: 10.1089/end.2008.0100. [DOI] [PubMed] [Google Scholar]
- 34.Tacchino RM, Greco F, Matera D, Diflumeri G. Single-Incision Laparoscopic Gastric Bypass for Morbid Obesity. Obes Surg. 2010 Apr 17; doi: 10.1007/s11695-010-0153-8. [DOI] [PubMed] [Google Scholar]
- 35.Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009 Apr;23(4):896–899. doi: 10.1007/s00464-008-0147-y. [DOI] [PubMed] [Google Scholar]
- 36.Escobar PF, Fader AN, Paraiso MF, Kaouk JH, Falcone T. Robotic-assisted laparoendoscopic single-site surgery in gynecology: initial report and technique. J Minim Invasive Gynecol. 2009 Sep-Oct;16(5):589–591. doi: 10.1016/j.jmig.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Rettenmaier M, Abaid L, Erwin M, John C, Micha J, Brown J, et al. A retrospective review of the GelPort system in single-port access pelvic surgery. J Minim Invasive Gynecol. 2009 Nov 1;16(6):743–747. doi: 10.1016/j.jmig.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 38.Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol. 2009 Aug;114(2):157–161. doi: 10.1016/j.ygyno.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 39.Rettenmaier MA, Lopez K, Graham CL, Brown JV, John CR, Micha JP, et al. Realhand high dexterity instruments for the treatment of stage I uterine malignancy. JSLS. 2009 Jan-Mar;13(1):27–31. [PMC free article] [PubMed] [Google Scholar]
- 40.Wheeless CR, Jr, Thompson BH. Laparoscopic sterilization. Review of 3600 cases. Obstet Gynecol. 1973 Nov;42(5):751–758. [PubMed] [Google Scholar]
- 41.Pelosi MA, Pelosi MA. Laparoscopic supracervical hysterectomy using a single-umbilical puncture (mini-laparoscopy) J Reprod Med. 1992 Sep 1;37(9):777–784. [PubMed] [Google Scholar]
- 42.Kosumi T, Kubota A, Usui N, Yamauchi K, Yamasaki M, Oyanagi H. Laparoscopic ovarian cystectomy using a single umbilical puncture method. Surg Laparosc Endosc Percutan Tech. 2001 Feb;11(1):63–65. [PubMed] [Google Scholar]
- 43.Ghezzi F, Cromi A, Fasola M, Bolis P. One-trocar salpingectomy for the treatment of tubal pregnancy: a 'marionette-like' technique. BJOG. 2005 Oct 1;112(10):1417–1419. doi: 10.1111/j.1471-0528.2005.00665.x. [DOI] [PubMed] [Google Scholar]
- 44.Lim MC, Kim TJ, Kang S, Bae DS, Park SY, Seo SS. Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for adnexal tumors. Surg Endosc. 2009 Nov;23(11):2445–2449. doi: 10.1007/s00464-009-0408-4. [DOI] [PubMed] [Google Scholar]
- 45.Ichihara T, Takada M, Fukumoto S, Yasuda T, Kuroda Y. A novel technique of finger-assisted laparoscopic surgery. Am J Surg. 2004 Feb;187(2):285–287. doi: 10.1016/j.amjsurg.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Kim TJ, Lee YY, Kim MJ, Kim CJ, Kang H, Choi CH, et al. Single port access laparoscopic adnexal surgery. J Minim Invasive Gynecol. 2009 Sep-Oct;16(5):612–615. doi: 10.1016/j.jmig.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 47.Langebrekke A, Qvigstad E. Total laparoscopic hysterectomy with single-port access without vaginal surgery. J Minim Invasive Gynecol. 2009 Sep-Oct;16(5):609–611. doi: 10.1016/j.jmig.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 48.Fagotti A, Fanfani F, Marocco F, Rossitto C, Gallotta V, Scambia G. Laparoendoscopic single-site surgery (LESS) for ovarian cyst enucleation: report of first 3 cases. Fertil Steril. 2009 Sep;92(3):1168, e13–e16. doi: 10.1016/j.fertnstert.2009.05.060. [DOI] [PubMed] [Google Scholar]
- 49.Lee YY, Kim TJ, Kim CJ, Kang H, Choi CH, Lee JW, et al. Single-port access laparoscopic-assisted vaginal hysterectomy: a novel method with a wound retractor and a glove. J Minim Invasive Gynecol. 2009 Jul-Aug;16(4):450–453. doi: 10.1016/j.jmig.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 50.Rosenblatt P, Makai G, DiSciullo A. Laparoscopic supracervical hysterectomy with transcervical morcellation: initial experience. J Minim Invasive Gynecol. 2010 May-Jun;17(3):331–336. doi: 10.1016/j.jmig.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 51.Yoon G, Kim TJ, Lee YY, Kim CJ, Choi CH, Lee JW, et al. Single-port access subtotal hysterectomy with transcervical morcellation: a pilot study. J Minim Invasive Gynecol. 2010 Jan-Feb;17(1):78–81. doi: 10.1016/j.jmig.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 52.Escobar PF, Bedaiwy MA, Fader AN, Falcone T. Laparoendoscopic single-site (LESS) surgery in patients with benign adnexal disease. Fertil Steril. 2010 Apr;93(6):2074, e7–e10. doi: 10.1016/j.fertnstert.2009.11.034. [DOI] [PubMed] [Google Scholar]
- 53.Mereu L, Angioni S, Melis GB, Mencaglia L. Single access laparoscopy for adnexal pathologies using a novel reusable port and curved instruments. Int J Gynaecol Obstet. 2010 Apr;109(1):78–80. doi: 10.1016/j.ijgo.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 54.Song T, Kim TJ, Kim MK, Park H, Kim JS, Lee YY, et al. Single Port Access Laparoscopic-Assisted Vaginal Hysterectomy for Large Uterus Weighing Exceeding 500 Grams: Technique and Initial Report. J Minim Invasive Gynecol. 2010 Jul;17(4):456–460. doi: 10.1016/j.jmig.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 55.Stolzenburg J-U, Kallidonis P, Oh M, Ghulam N, Do M, Haefner T, et al. Comparative assessment of laparoscopic single-site surgery instruments to conventional laparoscopic in laboratory setting. J Endourol. 2010 Feb 1;24(2):239–245. doi: 10.1089/end.2009.0296. [DOI] [PubMed] [Google Scholar]
- 56.Melendez TD, Childers JM, Nour M, Harrigill K, Surwit EA. Laparoscopic staging of endometrial cancer: the learning experience. JSLS. 1997 Jan-Mar;1(1):45–49. [PMC free article] [PubMed] [Google Scholar]
- 57.Holub Z, Jabor A, Bartos P, Hendl J, Urbanek S. Laparoscopic surgery in women with endometrial cancer: the learning curve. Eur J Obstet Gynecol Reprod Biol. 2003 Apr 25;107(2):195–200. doi: 10.1016/s0301-2115(02)00373-1. [DOI] [PubMed] [Google Scholar]
- 58.Lecuru F, Taurelle R. Transperitoneal laparoscopic pelvic lymphadenectomy for gynecologic malignancies (II). Indications. Surg Endosc. 1998 Feb;12(2):97–100. doi: 10.1007/s004649900606. [DOI] [PubMed] [Google Scholar]
- 59.Lecuru F, Taurelle R. Transperitoneal laparoscopic pelvic lymphadenectomy for gynecologic malignancies (I). Technique and results. Surg Endosc. 1998 Jan;12(1):1–6. doi: 10.1007/s004649900582. [DOI] [PubMed] [Google Scholar]
- 60.Seamon LG, Fowler JM, Richardson DL, Carlson MJ, Valmadre S, Phillips GS, et al. A detailed analysis of the learning curve: robotic hysterectomy and pelvic-aortic lymphadenectomy for endometrial cancer. Gynecol Oncol. 2009 Aug;114(2):162–167. doi: 10.1016/j.ygyno.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 61.Sarle R, Tewari A, Shrivastava A, Peabody J, Menon M. Surgical robotics and laparoscopic training drills. J Endourol. 2004 Feb;18(1):63–66. doi: 10.1089/089277904322836703. discussion 6–7. [DOI] [PubMed] [Google Scholar]
- 62.Bijen CB, Vermeulen KM, Mourits MJ, de Bock GH. Costs and effects of abdominal versus laparoscopic hysterectomy: systematic review of controlled trials. PLoS One. 2009;4(10):e7340. doi: 10.1371/journal.pone.0007340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Park S, Bergs RA, Eberhart R, Baker L, Fernandez R, Cadeddu JA. Trocar-less instrumentation for laparoscopy: magnetic positioning of intra-abdominal camera and retractor. Ann Surg. 2007 Mar;245(3):379–384. doi: 10.1097/01.sla.0000232518.01447.c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Scott DJ, Tang SJ, Fernandez R, Bergs R, Goova MT, Zeltser I, et al. Completely transvaginal NOTES cholecystectomy using magnetically anchored instruments. Surg Endosc. 2007 Dec;21(12):2308–2316. doi: 10.1007/s00464-007-9498-z. [DOI] [PubMed] [Google Scholar]
- 65.Zeltser IS, Bergs R, Fernandez R, Baker L, Eberhart R, Cadeddu JA. Single trocar laparoscopic nephrectomy using magnetic anchoring and guidance system in the porcine model. J Urol. 2007 Jul;178(1):288–291. doi: 10.1016/j.juro.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 66.Dominguez G, Durand L, De Rosa J, Danguise E, Arozamena C, Ferraina PA. Retraction and triangulation with neodymium magnetic forceps for single-port laparoscopic cholecystectomy. Surg Endosc. 2009 Jul;23(7):1660–1666. doi: 10.1007/s00464-009-0504-5. [DOI] [PubMed] [Google Scholar]