Abstract
Interactive health communication technologies (IHCTs) present a new opportunity and challenge for cancer control researchers who focus on couple and family-based psychosocial interventions. In this article we first present findings from a systematic review of eight studies that utilized IHCTs in psychosocial interventions with cancer patients and their caregivers. Although this research area is still in its infancy, studies suggest that it is feasible to incorporate IHCTs in such interventions, that IHCTs are generally well-accepted by patients and caregivers, and that the choice of technology is largely dependent on intervention target (i.e., patient, caregiver, or both) and outcomes (e.g., decision-making, symptom management, lifestyle behaviors). A major research gap has been the lack of integration of Web 2.0 technologies (e.g., social media), despite the fact that social support and communication are frequently targeted components of interventions that involve cancer patients and their caregivers. Given this, we next present findings from a qualitative study that we conducted to describe the different needs and preferences of 13 cancer survivors and 12 caregivers with regard to social media use. Finally, we discuss some of the opportunities and challenges of using IHCTs in psychosocial interventions for cancer patients and their caregivers and propose directions for future research.
Cancer patients must deal with a number of challenges including the emotional consequences of being diagnosed with a life-threatening illness (Zabora et al., 2001), medical treatments that can have debilitating side effects such as nausea, pain, urinary incontinence, fatigue, bodily disfigurement, sexual dysfunction, dyspnea, and cachexia, (Bonanno & Choi, 2011; DeSimone et al., 2012; Jacobsen & Stein, 1999; Kopp et al., 2013; Pirri et al., 2013; Van den Beuken-van Everdingen et al., 2007; Viola et al., 2008; von Haehling & Anker, 2010) as well as existential and spiritual concerns (Griffiths et al., 2002; Sears, Stanton, & Danoff-Burg, 2003). As a consequence, cancer patients often turn to their close family members for caregiving and support (Manne & Badr, 2008; Schmaling & Sher, 2000). However, the diagnosis of cancer in one family member has significant repercussions for the entire family. Partners in particular cope with challenges such as worry about the potential loss of their life partner and their ability to provide emotional and practical support to the patient (Kalayjian, 1989). In addition, family members are often unprepared and lack the resources for caregiving, (Coleman et al., 2004; Murray et al., 2002) have low self-efficacy for managing patient symptoms at home (Booth, Silvester, & Todd, 2003; Gysels & Higginson, 2009; Porter et al., 2008), and report high rates of distress of their own (Badr & Carmack Taylor, 2008; Dumont et al., 2006; Matthews, 2003). Compounding the problem, cancer often challenges established communication patterns and roles, making it difficult for patients and their family caregivers (i.e., partners or close family members) to coordinate care and support. For example, even though family caregivers are in a prime position to support patients’ lifestyle changes (Cottrell et al., 2005; Kumari, Head, & Marmot, 2004; Wang, Mittleman, & Orth-Gomer, 2005) and adherence (DiMatteo, 2004); they can display unhelpful (e.g., critical) communication (Manne & Schnoll, 2001; Manne et al., 1997) and model unhealthy behaviors that can interfere with patients’ attempts to cope with their illness, adhere to medical recommendations, and make healthy lifestyle changes. Even well-intentioned caregivers may offer assistance in ways that appear controlling or over-protective rather than supportive. (Anderson & Coyne, 1991; Coyne, Wortman, & Lehman, 1988)
Given that cancer patients and their families have substantial unmet needs for help with symptom management, communication, and the coordination of care (Osse et al., 2006; Wingate & Lackey, 1989), it is not surprising that a burgeoning literature involving psychosocial interventions that provide information, skills training, and support to cancer patients and their family caregivers has emerged over the past 2 decades. These dyadic interventions have been shown to enhance social support and communication and to improve multiple aspects of patient and caregiver quality of life (Badr & Krebs, 2013; Northouse et al., 2010). However, study samples are rarely representative and influenced by refusal rates that have varied widely (i.e., from 3–82%; see Badr & Krebs, 2013). Documented barriers to enrollment such as distance from the trial center, fear of randomization, and perceived burden of trial participation are only compounded when recruiting for dyadic interventions because two people must agree to participate (Fredman et al., 2009). Intervention programs are also often delivered via face-to-face methods which can be expensive and difficult to disseminate. Thus, new methods of delivering dyadic interventions are needed that not only address existing challenges but also extend the reach of these programs to improve health in the home environment outside of clinical care systems.
Because cancer patients and their family caregivers experience substantial emotional and practical burden as a result of the disease and its treatment, tools that alleviate this burden may not only have a viable place in cancer care but also help to improve patient and caregiver quality of life (Farnham et al., 2002; Reis, McGinty, & Jones, 2003). IHCTs involve the interaction of an individual with or through an electronic device in order to access, transmit, or receive health information, guidance, or support (Patrick et al., 1999). Most IHCTs are Internet-based applications (Institute of Medicine, 2002); however, the term includes interactive devices, multimedia programs, and mobile platforms. Although cancer patients and caregivers are increasingly engaging with IHCTs (Mayer et al., 2007; van de Poll-Franse & van Eenbergen, 2008), intervention adherence is a challenge because of potentially high rates of rapid attrition (Eysenbach, 2005; Gustafson et al., 2008) and possible suboptimal “dosage” (Cugelman, Thelwall, & Dawes, 2011). As research demonstrates improved outcomes with increased adherence (Evers et al., 2003; Gustafson et al., 2013; Norman et al., 2007), new methods are needed to enhance engagement.
Over the last decade, Internet-based IHCTs have evolved significantly from the “read-only” pages of Web 1.0 that transmitted health information to passive audiences to the user-generated and controlled Web 2.0 (Chou et al., 2012). “Social media” is a term used interchangeably with Web 2.0 to describe applications that allow information sharing and interaction among online communities (Bennett & Glasgow, 2009). There is a high prevalence of Internet (74%) and social media use (39%) among individuals with family members who have/had cancer, suggesting that it is possible to extend the reach of cancer prevention and control interventions to these individuals (Chou et al., 2009). Social media is an appealing tool for dyadic interventions because it has features (e.g., blogs, social bookmarking, public/private messaging, and photo/video content sharing applications) that can provide new opportunities for social engagement with other patients/caregivers (Amichai-Hamburger & Furnham, 2007) and healthcare professionals, as well as facilitate patient-caregiver connection and the coordination of care. It may also increase engagement in cancer prevention and control interventions. A recent study showed that participants with social ties to other participants in an online health promotion program were more likely to engage in the program as demonstrated by opening more e-mails, more frequent visits to the website, and completing more actions that they were prompted to perform (Poirier & Cobb, 2012). Results are consistent with the idea that social influence can affect adherence to behavioral interventions and that networking patients and caregivers or networking patients and caregivers together may increase social influence and engagement.
To our knowledge, there are currently no published studies in cancer that have incorporated social media in dyadic interventions. However, human computer interaction and social computing researchers have been working to understand how best to use IHCTs to support the information and emotional needs of patients and caregivers (Newman et al., 2011; Tixier & Lewkowicz, 2011; Weiss & Lorenzi, 2005; 2006) and several studies involving the use of IHCTs in the delivery of dyadic interventions have recently been published (DuBenske et al., in press; Milne et al., 2012; Silveira et al., 2011; Zulman et al., 2012). In this article, we seek to advance our understanding of the role IHCTs can play in psychosocial interventions for cancer patients and their caregivers. To that end, we first present findings from a systematic review that we conducted to summarize and evaluate the empirical literature on the use of IHCTs in dyadic interventions in cancer. Next, we present data from a small qualitative study that we conducted to explore the social media needs and preferences of cancer survivors and their caregivers. Finally, we discuss some of the opportunities and challenges of using IHCTs in dyadic interventions as well as directions for future research.
Systematic Review of Studies Using IHCTs in Dyadic Interventions
Method
A systematic review was undertaken to explore the extent that IHCTs have been used in dyadic interventions in cancer and to explore whether they facilitate patient-caregiver communication and outcomes. The present review followed the guidelines suggested by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA; Moher et al., 2009).
Search, Selection, and Review Strategies
The electronic databases MEDLINE, PsycInfo, CINAHL, EMBASE, the Cochrane library, and gray literature (e.g., conference proceedings) were searched using search terms specific to each database and keywords for terms indicating presence of cancer (e.g. neoplasms, cancer), and use of IHCTs (e.g., internet, multimedia, cellular phone, social media). These criteria were combined with psychosocial interventions (e.g. psychotherapy, couples therapy) and inclusion of a spouse/partner or caregiver (e.g., spouses, caregivers). Because this is an emerging research area, all publication types (e.g., randomized controlled trial, evaluation studies, pilot studies) were included. The searches were inclusive of studies published in English from the earliest publication date available in each database, and updated through July, 2013.
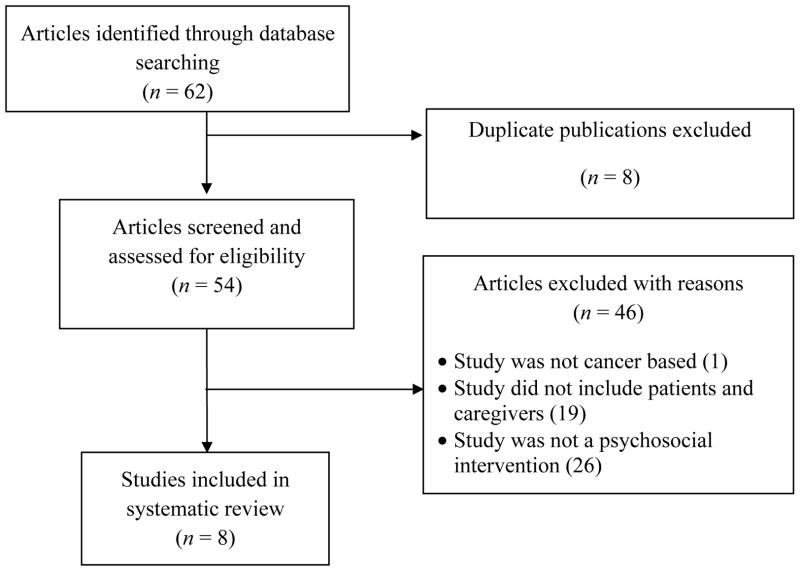
Figure 1 depicts the process used to identify and select relevant studies. Two raters reviewed the abstracts independently and produced a list of studies for full-text examination. Studies had to: 1) include patients with a diagnosis of cancer and their caregivers (spouses/partners, family members, or other caregivers); and, 2) employ a psychosocial IHCT-based intervention. We defined psychosocial intervention as any intervention that included: cognitive-behavioral techniques, stress management, relaxation training, or psycho-education. Studies that employed education only (e.g., instruction on how to search for cancer-related information on the internet) without a psychological or communication skills training component were not included. Discrepancies between raters were systematically resolved by consensus.
Fig. 1.
Flow diagram depicting the systematic review process.
Once the list of studies for full-text review was identified, the two raters independently reviewed the studies and abstracted data on study design, sample size, outcome measures, type of intervention (i.e. format, duration), and key findings. When full text could not be located or when published articles did not present sufficient data, we contacted authors to request the required information. Discrepancies were systematically resolved by consensus, and final data were entered for each study. Methodological quality of the studies included in the review was not assessed because the majority were pilot studies or descriptions of studies that are currently in progress (i.e., no data from the trial were provided in the article).
Results
Participant and design characteristics of the 8 studies included in the systematic review are described in detail in Table 1. Half of the studies focused on prostate cancer (Diefenbach & Butz, 2004; Reis, McGinty, & Jones, 2003; Schover et al., 2012; Zulman et al., 2012) and half focused exclusively on survivors who were post-treatment (Carmack et al., 2013; Diefenbach & Butz, 2004; Schover et al., 2012; Zulman et al., 2012). Only one study focused exclusively on patients with advanced disease (Gustafson et al., 2013). Type of study varied widely from randomized controlled trials (Carmack et al., 2013; Gustafson et al., 2013; Schover et al., 2012), to feasibility and acceptability studies (e.g., focus group evaluations, usability testing) (Diefenbach & Butz, 2004; Milne et al., 2012; Zulman et al., 2012), to trial or intervention descriptions (Reis, McGinty, & Jones, 2003; Silveira et al., 2011).
Table 1.
Systematic Review of Dyadic Studies that Utilized IHCTs (N = 8 studies)
| Study Target and Demographics | Refusal rate, Follow-up, and Attrition | Theoretical Model and Study Design | Intervention and Control/Comparison Group Descriptions* | Main Findings* | |
|---|---|---|---|---|---|
| Carmack, 2013 |
Target: breast, prostate, and colorectal cancer survivors (post-treatment) and their spouses N: 22 patient-spouse dyads Mean age: 63.1 (10.4) for survivors and 63.6 (7.1) for spouses |
Refusal rate: N/A Follow-up: 14 weeks, 6 month Attrition:4.5% for survivors and 9.1% for spouse |
Theory: Social Cognitive Theory Study Design:
|
Couples-Based (CB) Intervention: Survivors and spouses each received a workbook tailored to their current health behavior practices and individual goals. In addition to intrapersonal (individual) cognitive-behavioral strategies oriented towards one’s own behavior change (e.g., problem-solving, relapse prevention, goal-setting, cognitive restructuring, and time management), participants learned interpersonal cognitive-behavioral skills including communal coping, joint problem-solving, and adaptive communication strategies during 9 counseling sessions delivered via web-camera over 6 months Survivor Only (SO) Comparison Group: Survivors participate in the counseling sessions alone and no intervention materials are provided to spouses. Same intrapersonal skills are taught as the CB arm. No interpersonal skills were taught. |
Survivors in both study conditions experienced changes in health behaviors and weight loss. Spouses in the CB group evidenced changes in health behaviors and weight loss; whereas, those in the SO condition had no significant changes in any outcomes. |
| Diefenbach, 2004 |
Target: Prostate cancer survivors and their spouses N: 5 focus groups (FGs) with 18 prostate cancer survivors (3 FGs) and 15 spouses (2 FGs) Mean age: patients = 67 years; spouses = 60 years |
Refusal rate: NS Follow-up: N/A Attrition: N/A |
Theory: Self-regulation theory Study Design: Focus groups evaluated a CD-ROM-based multimedia Prostate Interactive Educational System (PIES) to enhance treatment decision making. PIES virtually mirrors a health center to provide information about prostate cancer and its treatment through an intuitive interface, using videos, animations, graphics, and texts. |
N/A | Patients and spouses were very interested in PIES and rated it as very useful; 83% stated a clear preference for the PIES software over printed materials. Patients and spouses rated the virtual library highly and patients showed greatest interest in watching video clips of other prostate cancer patients sharing their experience. Spouses wanted information specific to their own needs. Topics of interest to spouses were: nutrition, emotional support, caregiving after treatment, & communication and coping with sexual issues. |
| Gustafson, 2013 |
Target: The informal caregivers of patients with non-small cell lung cancer N: 285 patient-caregiver dyads Mean age: 52 |
Refusal rate: 32% Follow-up: Patients and caregivers completed bi-monthly assessments during the study Attrition: 41% |
Theory: Self-Determination Theory Study Design:
|
Intervention: CHESS-LC integrates 14 services to provide tailored cancer information (e.g., Ask an Expert feature, recent news, resource guide), support (e.g., limited access, facilitated bulletin boards, written and video accounts of how other lung cancer patients and families coped), and interactive tools (e.g., decision making support, action planning, skills building for easing distress and healthy relating, and journaling). Clinicians also receive a report that summarizes caregiver and patient ratings of the patient’s health status and lists their questions for the next clinic visit. Control: Patients and caregivers received training on using the Internet and a list of Internet sites about lung cancer. |
Caregivers in the intervention arm consistently reported lower patient physical symptom distress than caregivers in the control arm. Significant differences were observed at 4 months and at 6 months |
| Milne, 2012 |
Target: cancer patients undergoing chemotherapy, their caregivers, and healthcare providers N: 9 patients with 4 different types of cancer and receiving chemotherapy Mean age: 56 |
Refusal rate: N/A – patients self-selected to take part in the study Follow-up: structured online surveys were completed 6–8 weeks after commencing use of the CanCare website and again at the end of study (5 months). Semi-structured interviews were also conducted at the end of study. Attrition: NS |
|
Intervention: Patients could use the website to invite family, friends, and healthcare providers to help them develop and implement a shared care-plan for managing symptoms. They could also record symptoms, keep an appointment calendar, and create medication lists. | Patients saw the potential of the website but found it too complex to use and were frustrated by the lack of integration with existing hospital systems. The cancer-specific information tab rated highly and used extensively. Due to the lack of caregiver and provider engagement, it was not possible to test whether the CanCare intervention enhanced communication. |
| Reis, 2003 |
Target: Prostate cancer patients undergoing active treatment and their family members N: N/A |
Refusal rate: NS Follow-up: N/A Attrition: N/A |
Theory: Social-cognitive theory Study Design: Description is provided of a multimedia caregiving training program for prostate cancer patients and family members that provides assistance in prioritizing caregiving needs and expanding self-efficacy with caregiving tasks. Delivery: The program was designed for hybrid delivery utilizing both web-based resources (e.g., hyperlinks to internal and external resources) and a CD-ROM that stores and recalls media such as digital audio, video, high resolution graphics, and animations. |
Intervention: The caregiving program separately assesses patient and family member perceived caretaking needs and caregiving skills related to treatment outcomes. The program then provides targeted instruction in caregiving techniques and skills based on patient and caregiver need and areas of disagreement. |
Outcome measures will include pre–post changes in self-efficacy for specific caregiving functions, and pre–post changes in expectations of outcomes in performing these caregiving functions. |
| Schover, 2012 |
Target: patients treated for localized prostate cancer with surgery or radiotherapy and their partners N: 186 patient-partner dyads Mean age: 61 |
Refusal rate: NS Follow-up: post-treatment, and 6 and 12 month follow-ups Attrition:34% |
Theory: No explicit theory Study Design:
|
Web Intervention: Education, training to improve sexual communication and expression of feelings, cognitive-behavioral techniques to address negative beliefs about cancer and sexuality. Homework exercises had standardized report forms completed online and were submitted by each partner. Therapists e-mailed feedback to the couple. Face to Face Intervention: included the same content and cognitive-behavioral homework as the web intervention. Therapists discussed homework with couples in the session. Control: 3 month wait-list control |
Women made significantly fewer visits to and completed significantly less of the website than men. In the web group, International Index of Erectile Functioning (IIEF) scores improved significantly more in men who completed >75% of the program. Sexual function/satisfaction did not improve significantly for women within any treatment group. Neither marital happiness nor overall distress changed significantly across time for men in any subgroup or in the total sample. |
| Silveira, 2011 |
Target: The informal caregivers of patients with solid tumors undergoing chemotherapy N: 300 patient-caregiver dyads are expected to be enrolled Mean age: N/A |
Refusal rate: N/A – trial is ongoing Follow-up: post-intervention and 1 month Attrition: N/A – trial is ongoing |
Theory: Stress and coping theory Study Design: The article provides a description of an ongoing trial.
|
Intervention: Patients receive a Symptom Management Toolkit and weekly automated telephone assessment calls. Their caregiver receives weekly emails prompting them to log into the Cancer CarePartners website when their patient reports any core symptom severity of four or higher. The website informs caregivers of their patients’ symptom assessment scores and provides them with advice for how to help. Control: Patients receive a Symptom Management Toolkit followed by weekly automated telephone assessment calls. Caregivers receive an email with a PDF copy of “What you need to know about cancer” from the National Cancer Institute |
The goal is to determine if, when compared to a comparison group receiving automated telephone assessment alone, patients who receive automated telephone assessment and whose caregivers receive access to the Cancer CarePartners website will report significantly less total symptom severity. Secondary outcomes for patients include: physical functioning, adherence to chemotherapy, and more appropriate utilization of health services. The study also will determine whether caregivers provide more social support and report less caregiver burden and distress. |
| Zulman, 2012 |
Target: prostate cancer patients post-treatment and their caregivers N: 4 FGs with 2–3 patient-caregiver pairs per group (N=22 total participants) and 2 iterations of usability testing with 4 patient-caregiver pairs per session (N = 16 total participants) Mean age: 52.6 years |
Refusal rate: NS Follow-up: N/A Attrition: N/A |
Framework: No explicit theory Study Design:
|
Intervention: The article describes the process of developing a web-based version of the family involvement module of an in-person intervention for prostate cancer couples called FOCUS (Family involvement, Optimistic attitude, Coping effectiveness, Uncertainty reduction, and Symptom management). The family involvement module provides relational content that addresses communication, support, and teamwork. | In general, participants were comfortable completing the program on the web and working together as a dyad. Response to the program’s structure, design, and content was favorable, even among users who were older or had limited computer and Internet experience. The program received high ratings for ease of use and overall usability. |
Note. FGs = focus groups; NS = Not specified; N/A = Not applicable; CBT = Cognitive-behavioral therapy; CBMT = Cognitive Behavioral Marital Therapy; BMT = Behavioral Marital Therapy.
If applicable.
Participant Characteristics
Most studies did not specify the racial/ethnic breakdown of their samples. Those that did (N=4) included predominately white participants (75%). Their mean reported age of participants across studies was 58 years (range of mean age= 52 to 67). The total number of dyads enrolled in the randomized trials ranged from 22 to 285. One study cited a recruitment goal of 300 dyads, but is still recruiting participants (Silveira et al., 2011). Only two studies (Carmack et al., 2013; Gustafson et al., 2013) provided information on refusal rates (32% and 68%). Three studies provided attrition statistics (Carmack et al., 2013; Gustafson et al., 2013; Schover et al., 2012); rates ranged from 0 to 41%.
Design Characteristics
Most studies (N=6) specified a theoretical model that grounded their approach but did not specify how theory was used in the development of intervention materials. Individual stress and coping models, which grounded one study (Silveira et al., 2011), view social support as a form of coping assistance and posit that person-, social-, and illness-related factors influence how people appraise and cope with an illness (Thoits, 1986). Self-regulation theory (Baumeister, Heatherton, & Tice, 1994; Cameron & Leventhal, 2012) grounded two studies (Diefenbach & Butz, 2004; Milne et al., 2012). Resource theories (e.g., social cognitive theory (Lepore & Revenson, 2007), which grounded or had elements in two studies (Carmack et al., 2013; Reis, McGinty, & Jones, 2003), view the partner and relationship as resources patients can draw upon for assistance during difficult life events. Finally, self-determination theory (Deci & Ryan, 1985), which is a motivational theory, grounded one study (Gustafson et al., 2013). It is concerned with supporting our natural or intrinsic tendencies to behave in effective and healthy ways and posits that conditions supporting an individual’s experience of autonomy, competence, and relatedness foster the most volitional and high quality forms of motivation and engagement for health-related activities, including enhanced performance and persistence. In addition self-determination theory proposes that the degree to which any of these three psychological needs is unsupported or thwarted within a social context will have a detrimental impact on health and well-being.
Study Descriptions
Due to the limited number and diversity of the studies published in this area, we chose to be inclusive and to describe all eight articles where IHCTs were used in psychosocial interventions for cancer patients and their caregivers. We organize our descriptions below based on the study’s primary focus. Specifically, one study used IHCTs as part of a comprehensive interactive health system (Gustafson et al., 2013). One study had a primary focus on enhancing decision-making (Diefenbach & Butz, 2004). In five studies, the goal was to use IHCTs to improve patient-caregiver communication (Milne et al., 2012; Reis, McGinty, & Jones, 2003; Schover et al., 2012; Silveira et al., 2011; Zulman et al., 2012). Finally, one study used IHCTs to help promote healthy lifestyle behaviors in couples (Carmack et al., 2013).
IHCTs in Comprehensive Interactive Health Systems
The Comprehensive Health Enhancement Support System (CHESS), the most extensively studied IHCT, has three main components – information, support, and coaching to collectively facilitate decision-making and communication (DuBenske et al., 2008; Gustafson et al., 1999; Gustafson, McTavish, & Hawkins, 1999; McTavish et al., 2000; Shaw et al., 2006). For example, the Supportive Services feature comprises an asynchronous Discussion Group (limited access, facilitated bulletin board), as well as Personal Stories (written accounts of how other cancer patients and families coped) and a Personal Webpage which allows users to connect with their own support network to request help and share updates. CHESS also has a decision aid to help patients and caregivers think through difficult decisions by “learning about options, clarifying values, and understanding consequences.” Further, the “Ask an Expert” feature allows patients and caregivers to pose confidential questions directly to an expert (DuBenske et al., 2010).
One of the newest CHESS modules, CHESS-LC (lung cancer), provides a comprehensive package targeted to caregivers of advanced lung cancer patients. In addition to the standard CHESS features, CHESS-LC includes a Clinician Report which sends an e-mail alert when patients exceed a threshold on the symptom distress scale; it also sends an e-mail to the clinical team 2 days before a clinic appointment alerting them to look at the patient’s CHESS-LC report. In a recent trial, 285 caregiver-patient dyads were randomized to receive standard care plus either the Internet or CHESS-LC. Caregivers in the CHESS-LC arm reported lower patient physical symptom distress at 4 and 6 month follow-up (Gustafson et al., 2013) and lower caregiver burden and negative mood at 6-month follow-up compared to caregivers in the Internet-only arm (DuBenske et al., in press). Although findings suggest that interventions that incorporate IHCTs can improve outcomes for both patients and caregivers, further research is needed to elucidate mechanisms of effect.
IHCTs to Facilitate Treatment Decision-Making
Diefenbach and Butz (2004) conducted focus groups to evaluate a multimedia prostate cancer interactive education system (PIES) and decision tool for patients and their family members. PIES uses the metaphor of a virtual health center to organize and store information. Users can visit rooms such as a library, a conference room with videos by survivors who discuss their treatment experiences, and physician offices with videos discussing different treatment modalities. Five focus groups (3 with patients and 2 with spouses) were conducted to evaluate the PIES prototype. Overall, spouses felt PIES was intuitive to use, but did not have information tailored to their specific needs as spouses and caregivers. Specifically, they wanted information about how to cope with their own feelings of distress and information about post-treatment care and side-effects -- particularly sexual and urinary dysfunction. When asked how to best convey this information to others, spouses/partners felt that a video format was preferable to reading information. The result was a 30-minute video of three spouses talking about their experiences that was thematically edited and made available in the family room. Although evaluation data specifically related to the PIES family room has not been published, this study suggests that providing information that addresses the unique needs of both patients and caregivers is critical for the engagement of both and that caregivers may prefer receiving information in the form of personal stories and video as opposed to static text. Recently, Diefenbach and colleagues (2012) published preliminary patient data on the efficacy of a web-based version of the PIES software; however, spouse/partner data have not been reported in that study.
IHCTs to Enhance Patient-Caregiver Communication
Studies have used IHCTs in an effort to enhance patient-caregiver communication about cancer-related symptoms; however, existing studies appear to be quite small and/or just beginning. The only full-scale randomized controlled trial that has been completed was conducted by Schover (2012) and targeted prostate cancer survivors and their partners. Couples were randomized to a 3-month wait list control group, an intervention group called CAREss (Counseling About Regaining Erections and Sexual Satisfaction) that received 3 face-to-face sessions over 12 weeks, and an intervention group that used an internet format of CAREss and communicated with a therapist via e-mail. CAREss involved exercises to increase expression of affection, improve sexual communication, increase comfort in initiating sexual activity, and facilitate resuming sex without performance anxiety (using a sensate focus framework). Suggestions were provided to treat postmenopausal vaginal atrophy or cope with male urinary incontinence. Gender-specific exercises helped participants identify negative beliefs about sexuality and use cognitive reframing. Treatments for erectile dysfunction (ED) after prostate cancer were described, with suggestions on their efficacy and using them optimally. Results showed that traditional face-to-face sexual counseling and the internet-based format of the CAREss program that depended on e-mail for contact with the therapist produced equally significant gains in men’s sexual function and satisfaction. In addition, neither marital happiness nor overall distress changed significantly across time for men in any subgroup or in the total sample. Sexual function/satisfaction did not improve significantly for women within any treatment group.
Milne (2012) reported on a small trial (n=9) of a website called CanCare to promote self-management; the primary target was the patient. Patients could use the website to invite family, friends, and healthcare providers to help them develop and implement a shared care-plan for managing symptoms. They could also record symptoms, keep an appointment calendar, and create medication lists. Overall, patients found CanCare cumbersome and difficult to use and the lack of integration with existing hospital systems resulted in a lack of provider participation. Only one patient asked her caregiver to participate and patients said they were reluctant to approach their caregivers because they thought participating would be burdensome for them. Due to the lack of caregiver and provider engagement, it was not possible to test whether CanCare enhanced communication. Thus, this study highlights the need to develop an intuitive, user-friendly interface, the importance of integrating IHCTs with existing clinical systems when the goal is to involve providers, and the need to actively enroll caregivers instead of relying exclusively on the patient.
Silveira (2011) is currently conducting a 10-week randomized trial targeting family caregivers of a program that includes weekly automated telephone assessments and self-management support calls to cancer patients and web-based alerts for caregivers. The alerts help caregivers identify problems and provide symptom management advice. Zulman and colleagues (2012) are also currently conducting a pilot trial of a tailored interactive web-based communication program that targets prostate cancer patients and their spouses/partners. Their article describes the process of developing a web-based version of the family involvement module of an in-person intervention for prostate cancer couples called FOCUS (Family involvement, Optimistic attitude, Coping effectiveness, Uncertainty reduction, and Symptom management). The web-based program offers self-care strategies for symptom-management and tips for communication and working together as a team. Couples log on to the website together. Communication and processing is facilitated through a unique dyadic interface that directs questions to patients, caregivers, and the pair, and then provides tailored feedback based on users’ responses. Finally, Reis presented data from 45 prostate cancer patients and family members on needs for caregiving and described an interactive multimedia program that assesses patient and family member’s level of preparedness for specific caregiving functions for prostate cancer and provide tailored skill building vignettes on caregiving techniques based on caregiver need and areas of disagreement with the patient. According to the article, the program was designed for hybrid delivery utilizing both web-based resources (e.g., hyperlinks to internal and external resources) and a CD-ROM that stores and recalls media such as digital audio, video, high resolution graphics, and animations. No further data regarding the prototype was presented in the article.
Taken together, these interventions showcase different ways IHCTs have been used to enhance patient-caregiver communication. Even though Milne (2012) used IHCTs to enhance communication through the sharing of self-care plans, Silveira (2011) used alerts to keep caregivers informed about symptoms, and Reis used the discrepancy between patient and caregiver assessments as a springboard for providing tailored educational information so that caregivers could provide better support, these studies took a passive, technology-mediated approach to sharing health-related information within the dyad. Schover (2012) provided communication skills training; however, patients and partners logged on to the website and communicated with the therapist separately. In contrast, the web-based version of the FOCUS intervention described by Zulman (2012) appears to take a more interactive couple-based approach because it requires couples to discuss an issue in front of the computer before answering questions. More research is needed to determine which of these approaches is most effective in improving patient and caregiver outcomes.
IHCTs to Promote Lifestyle Behavior Change
Carmack and colleagues recently concluded a pilot study entitled Healthy Moves to examine the feasibility and efficacy of a couples-based multi-behavior change web-based counseling intervention (diet and physical activity) compared to the same intervention delivered to the patient alone (Carmack et al., 2013). Video-based counseling delivered over the internet was chosen over other distance-based approaches (e.g., telephone counseling), because it provides counselors with the ability to see their clients in real-time and monitor their non-verbal cues during the session. This is highly important for couples’ interventions since communication skills training is key for addressing issues related to social support and social control (Bodenmann & Shantinath, 2004; Markman et al., 1993; Neff & Karney, 2005).
Twenty-two couples facing breast, prostate or colorectal cancer were enrolled, vrandomized, and completed assessments at baseline, 14 weeks, and 6 months; 95% of survivors and 91% of spouses completed the 6 month follow-up. Attendance to the 9 counseling sessions was high in both conditions (91–97%). Problems were encountered with logging on to the system and navigating the toolbars once logged in. Other problems included not receiving counseling session notices which were submitted through e-mail and having to frequently upgrade JAVA.
Upon study completion, participants rated the difficulty of using the web-camera for counseling on a scale of 1 (extremely difficult) to 5 (not at all difficult). In the couples condition, average ratings for survivors and spouses were 3.7 (SD=1.6) and 3.33 (SD=1.9) respectively, and the average rating in the survivor-only condition was 2.3 (SD=1.5). One possibility is that couples may have rated it less difficult because they had each other to problem-solve difficulties. Additionally, participants rated on a scale of 1 (did not like at all) to 5 (liked it a lot) how much they liked using the web-camera from home for counseling. In the couples condition, average ratings for survivors and spouses were 3.8 (SD=1.8) and 3.5 (SD=1.5) respectively; the average rating in the survivor-only condition was 3.9 (SD=1.6). Despite some technical difficulties, survivors and spouses both liked the convenience of participating in sessions from their homes. Thus, targeting the couple is not only feasible but also may help to facilitate engagement with lifestyle interventions and help overcome some of the technical problems that can happen.
Summary
Although this research area is still in its infancy, studies suggest that it is feasible to incorporate IHCTs in dyadic interventions, that IHCTs are generally well-accepted by patients and caregivers, and that the choice of technology is largely dependent on intervention target (i.e., patient, caregiver, or both) and outcomes (e.g., decision-making, symptom management, lifestyle behaviors). A major research gap has been the lack of integration of Web 2.0 despite the fact that social support and communication are frequently targeted components of dyadic interventions (Manne & Badr, 2008). Indeed, online social networking is recognized for its potential to provide new opportunities for social engagement and connection (Amichai-Hamburger & Furnham, 2007; Campbell, Cumming, & Hughes, 2006) and studies have demonstrated the benefits of social networking sites for mental health and well-being (Ellison, Steinfield, & Lampe, 2007; Liu & LaRose, 2008). Social media represents a challenge for dyadic interventions because the focus is on improving social support and communication between patients and caregivers (Manne & Badr, 2008), and social media platforms largely enhance the ability to connect with others outside the family unit. Complicating things further, for cancer patients, receiving social network support does not compensate for a problematic relationship or a lack of partner support (Pistrang & Barker, 1995). Thus, one challenge for dyadic interventions will be to leverage social media to network patients and caregivers together.
Social Media Needs and Preferences of Cancer Survivors and Their Caregivers
Badr and colleagues are developing a multi-behavioral web-based intervention to improve adherence to oral health regimens and quality of life in oral cancer survivors and their family caregivers (R34 DE022273). To this end, semi-structured interviews were conducted with oral cancer survivors and caregivers to identify social media features that would enhance patient and caregiver engagement with the site and facilitate patient-caregiver communication.
Method
Procedures
Oral cancer survivors who had completed treatment, spoke English, and who could identify a spouse/partner who served as their primary caregiver were eligible to participate. Twenty consecutive survivors were approached to participate during the survivor’s routine clinic visits. If they were accompanied by their caregiver, the caregiver was also approached to participate. If not, study staff asked the survivor for permission to approach their caregiver by phone. Thirteen (out of 20) patients agreed to participate (65%) and 12 out of 16 caregivers (75%) agreed to participate. Reasons for refusal included: the patient was fatigued or was unable to vocalize well enough to complete the interview (N=5), the caregiver was too busy (2), the patient was not interested (2), and the caregiver was not interested (2). Sixty-minute semi-structured interviews were scheduled with patients and caregivers separately to better understand their use and interest in using social media to obtain cancer-related information and support. They received $25 gift cards upon completion of their interviews. The audio of the interviews was recorded and transcribed. Transcript analysis consisted of inductive coding performed by two independent raters followed by discussion to iteratively generate and refine themes. This process continued until saturation was achieved.
Results
Survivors were mostly male (77%) and caregivers were mostly female (92%). The majority of caregivers were spouses (67%), with the remainder being adult children of the survivor. Key themes from the qualitative interviews are presented in Table 2.
Table 2.
Social Media Needs and Preferences of Oral Cancer Survivors and their Family Caregivers (N=25)
| Survivors (N=13) | Caregivers (N=12) | |
|---|---|---|
| Reasons for seeking out other survivors and caregivers via social networks | “Family members tell you what you want to hear, but other survivors tell it like it is.” “Communication between the newies [newly diagnosed] and the oldies [long-term survivors] would help a lot.” “People need to commiserate with other people going through the same or similar situations.” “You never know what the tomorrow is, so if those who have been through it could relate their experiences to those who are just starting to deal [with the effects of treatment]…It would act as a sort of timeline [for recovery] and provide hope.” |
“When the patient is really sick and going through a hard time, it is really scary and that would be a good time to talk to someone who has been through it. It’s about the sharing…the frustration, the struggles, and your fears like you are not doing the right thing. You know other wives are going through the same and that they will understand.” “When you ask the medical people, they keep it more about health, but when you talk with other caregivers on the Internet, it’s more anecdotal. What you get is how to have a comfortable life while you are going through hell.” |
| What social networks provide that talking with the patient/caregiver does not | “You can get a lot out of strangers, strangely enough. You kind of hook up with people that are going through the same things [and] you don’t have that emotional pile…They’re not judging you or have ulterior motives. Unlike your family or friends, with strangers, you get – it’s not support, but it’s not criticism either – it’s just listening.” | “Sometimes I need to get cancer off my chest but I don’t want to burden [my husband] because he has already gone through so much.” “I want to hear how other wives survived it…I wonder how they handled it and how they are doing.” “Its a lot of communication…and I see people on there [the Internet] praying. Even if they don’t know my mom, they know me [through message boards], and they are praying to make sure that she is doing better.” |
| Ways that social media can be used to facilitate patient-caregiver communication | “I write a private blog and invited my family and close friends to read it. It gets tiring to tell the whole story about what is happening over and over to everyone…If they want to know how I am doing or how I am feeling, they can just read it (the blog) and it keeps everyone in the loop.” “When you’re in front of each other, both of you are trying to hold up and be strong, but online you are not seeing each other, so you might be more inclined to be honest because you know your wife is not there with you and isn’t going to respond right then and there. Having that kind of space in the conversation could be really useful.” |
“Part of the problem is him not being able to talk…there are also times when he’s so fatigued that he can’t listen to me when I want to talk about things. I could write it down [online] and then when he is feeling up to it, he could then maybe go and read and respond.” “There were times when I would be frustrated because I thought I should be doing something and he didn’t want to do it and we would argue. I remember there was a period where he kept calling me the drill sergeant. If there was a way you could communicate some of those things and not get into the defensive stuff…Maybe you could write it down online and say you have to have at least five cans (liquid nutrition) a day. If you don’t want to take it now, when are you going to do it? How do you want to do it? If you blow up and express it verbally it makes it bigger, but if you do it in a funny or removed way online - maybe through an emoticon or picture even - you could still express but it wouldn’t be as threatening or anger provoking.” |
Overall, 84% (21/25) of patients and caregivers were interested in using social media, but they differed in the types of information and support they wanted to receive. While many survivors (54%) were interested in using social media to help them reach out to others for emotional support, more (77%) were interested in obtaining practical support and information about how to deal with side effects. Specifically, they wanted applications that would allow them to set their own oral care and rehabilitation goals (46%), monitor and track progress (46%), and set up text or e-mail reminders (23%) that they could share with their caregivers (75%) and healthcare team (62%). They also wanted a realistic picture about what to expect after treatment from other survivors who were farther along in the recovery/rehabilitation process. In contrast, caregivers wanted social support. They wanted to connect to other caregivers to learn how they were coping (50%), obtain tips for providing support and communicating with survivors (50%), and share and receive practical advice for managing responsibilities and taking care of themselves while caring for their loved one (42%).
Both survivors and caregivers were interested in using social media to communicate with family members and each other. Survivors felt social media could help them to efficiently convey information to their families and that it provided an opportunity to be more open and candid about thoughts and feelings. In contrast, caregivers felt social media was a communication tool that could be used when the survivor was experiencing symptoms that might impair his/her ability to talk. They also felt it could be used to help them avoid conflicts and coordinate care with the survivor without nagging or criticizing (see Table 2).
Summary
Findings suggest that social media may be a useful tool for conveying health-related information and support to cancer survivors and their caregivers. While survivors and caregivers may stand to benefit from interacting with similar others through this technology, more work is needed to identify ways that social media can be used to network patient-caregiver dyads and families together.
Discussion
Taken together, the findings from our systematic review and qualitative analysis suggest several opportunities for IHCTs and Web 2.0 to be integrated in dyadic interventions in cancer control. For example, integrating blogs and content sharing applications may help survivors and family members find meaning in their cancer experience by sharing their story with others, foster social relationships and social support, and facilitate decision-making by connecting family members who are geographically dispersed. Technology may also make it easier for patients to reach out for support and express their concerns (Walther & Boyd, 2002). Moreover, sites that connect survivors and caregivers to others dealing with the same cancer may not only enhance overall perceptions of social support but may augment information from the healthcare team by providing practical tips for managing the day-to-day aspects of life after cancer (Eysenbach et al., 2004).
Indeed, there are shortcomings to using IHCTs that offer online support groups in either an asynchronous (facilitated bulletin boards wherein participants post comments and others respond as they are able) or synchronous (groups occurring in “real time”) formats. In synchronous groups, posts can be made so quickly that they may be overlooked by participants or result in multiple conversations occurring simultaneously (Owen, Bantum, & Golant, 2009). In both synchronous and asynchronous formats, it is possible that patients post information to which no one responds, which might leave them feeling ignored. Further, non-verbal cues are missed, a problem for those who want to speak but are not assertive enough to talk over others (Owen, Bantum, & Golant, 2009). Similarly, emotional expression is more difficult for facilitators to detect through written text compared to face-to-face. Positive affect is overestimated and defensive/hostile affect underestimated (Liess et al., 2008). Ultimately, this may affect the facilitator’s ability to assist with emotional expression, thus hindering cognitive processing. Finally, patients may bond less in an online format compared to face-to-face because of reduced expectations for attendance and/or responsibility to the group (Owen, Bantum, & Golant, 2009). At this point, these issues remain unexplored for such interventions targeting dyads.
Clearly, more research is needed to determine whether online communication through social media stimulates in-person communication, whether patients and caregivers use social media as a substitute for working through communication difficulties in person (and if that matters), and whether social media use has discernible effects on both patient and caregiver outcomes relative to other types of IHCTs. Indeed, how an IHCT system is used is likely to reflect user need and may be the most important factor in determining intervention efficacy (Han et al., 2009; Han et al., 2010). More research is also needed to determine whether social media preferences are different for survivors and caregivers who are dealing with a new diagnosis or active treatment, compared to the post-treatment survivors and caregivers we interviewed in our qualitative study presented above. If indeed social media preferences and online information and support needs differ depending on location on the cancer trajectory (e.g., treatment, post-treatment survivorship, end-of-life), then this would suggest the need for more tailored approaches. Finally, our understanding of what types of decisions and problems can be best addressed through IHCTs and social media technologies has yet to be determined. Thus, research is needed to determine if there are certain circumstances where IHCTs need to be supplemented by “human interaction” with a professional. For example, a recent meta-analysis showed that Internet-based cognitive-behavioral interventions that include a therapist are more effective for anxiety and depression than those that do not (Spek et al., 2007); thus dyads facing individual or couple level distress may have differing needs than those not facing any psychosocial distress.
These above issues notwithstanding, IHCTs and social media represent a “brave new world” for dyadic interventions in cancer control because they: 1) provide a convenient on-demand resource with needed flexibility when delivering interventions that target more than one individual; 2) may have greater reach to those who are homebound, have transportation difficulties, or are geographically isolated; 3) incorporate content sharing applications (e.g., video, photos) that can provide a rich and engaging forum to convey information and model skilled behaviors, as well as an opportunity to make that information more personal and potentially more relevant; and 4) make available new opportunities for social networking with “strangers” (i.e., other patients/caregivers outside one’s personal social circle) and family members which may enhance engagement with health promotion materials and facilitate the coordination of care. We hope this article stimulates thinking about ways researchers can incorporate these new communication technologies in dyadic interventions to improve the health and well-being of both cancer patients and their family caregivers.
Acknowledgments
The authors thank Daniella Lipnick and Mariam Sallam who helped to transcribe and code the social media interviews.
Funding
Dr. Badr’s work was supported by grants from the National Institute of Dental and Craniofacial Research (grant number R34 DE022273) and National Cancer Institute (grant number K07CA 124668); Dr. Diefenbach’s work was supported by R01CA118682; R21 CA164807; R21 CA155963; and DAMD PC101223; and Dr. Carmack’s work was supported by MD Anderson Cancer Center’s Multidisciplinary Research Program.
References
- Amichai-Hamburger Y, Furnham A. The positive net. Computers in Human Behavior. 2007;23(2):1033–1045. [Google Scholar]
- Anderson BJ, Coyne JC. “ Miscarried helping” in the families of children and adolescents with chronic diseases. Paper presented at the An adaptation of this paper was presented at the National Institute of Child Health and Human Development Conference on Compliance to Health-Promoting Behavior in Children; Washington, DC. Jul 1989.1991. [Google Scholar]
- Badr H, Carmack Taylor CL. Effects of relational maintenance on psychological distress and dyadic adjustment among couples coping with lung cancer. Health Psychology. 2008;27(5):616–627. doi: 10.1037/0278-6133.27.5.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H, Krebs P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psycho-Oncology. 2013;22:1688–1704. doi: 10.1002/pon.3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF, Heatherton TF, Tice DM. Losing control: How and why people fail at self-regulation. Academic Press; 1994. [Google Scholar]
- Bennett GG, Glasgow RE. The Delivery of Public Health Interventions via the Internet: Actualizing Their Potential. Annual Review of Public Health. 2009;30(1):273–292. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- Bodenmann G, Shantinath SD. The Couples Coping Enhancement Training (CCET): A new approach to prevention of marital distress based upon stress and coping*. Family Relations. 2004;53(5):477–484. [Google Scholar]
- Bonanno A, Choi JY. Ophthalmic Oncology. Springer; 2011. Psychosocial aspects of orbitofacial disfigurement in cancer patients; pp. 311–318. [Google Scholar]
- Booth S, Silvester S, Todd C. Breathlessness in cancer and chronic obstructive pulmonary disease: using a qualitative approach to describe the experience of patients and carers. Palliat Support Care. 2003;1(4):337–344. doi: 10.1017/s1478951503030499. [DOI] [PubMed] [Google Scholar]
- Cameron L, Leventhal H. The self-regulation of health and illness behaviour. Routledge: 2012. [Google Scholar]
- Campbell AJ, Cumming SR, Hughes I. Internet use by the socially fearful: Addiction or therapy? CyberPsychology & Behavior. 2006;9(1):69–81. doi: 10.1089/cpb.2006.9.69. [DOI] [PubMed] [Google Scholar]
- Carmack C, Basen-Engquist K, Shely L, Baum G, Giordano S, Rodriguez-Bigas M, Pettaway C, Demark-Wahnefried W. Healthy Moves to improve lifestyle behaviors of cancer survivors and their spouses: Feasibility and preliminary results of intervention efficacy. Annals of Behavioral Medicine. 2013;45(S2):s178. doi: 10.3390/nu13124460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou WS, Prestin A, Lyons C, Wen K. Web 2.0 for Health Promotion: Reviewing the Current Evidence. American Journal of Public Health. 2012;103(1):9–18. doi: 10.2105/AJPH.2012.301071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou WYS, Hunt YM, Beckjord EB, Moser RP, Hesse BW. Social media use in the United States: implications for health communication. Journal of Medical Internet Research. 2009;11(4):e48. doi: 10.2196/jmir.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E, Smith J, Frank J, Min S, Parry C, Kramer A. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. Journal of the American Geriatrics Society. 2004;52(11):1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- Cottrell L, Spangler-Murphy E, Minor V, Downes A, Nicholson P, Neal WA. A kindergarten cardiovascular risk surveillance study: CARDIAC-kinder. American Journal of Health Behavior. 2005;29(6):595–606. doi: 10.5555/ajhb.2005.29.6.595. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Wortman CB, Lehman DR. The other side of support: Emotional overinvolvement and miscarried helping. In: Gonlieb BH, editor. Marshaling social support. Newbury Park, CA: Sage; 1988. pp. 305–330. [Google Scholar]
- Cugelman B, Thelwall M, Dawes P. Online interventions for social marketing health behavior change campaigns: a meta-analysis of psychological architectures and adherence factors. Journal of Medical Internet Research. 2011;13(1) doi: 10.2196/jmir.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum; 1985. [Google Scholar]
- DeSimone M, Spriggs E, Gass JS, Carson SA, Krychman ML, Dizon DS. Sexual dysfunction in female cancer survivors. American Journal of Clinical Oncology. 2012 doi: 10.1097/COC.0b013e318248d89d. [DOI] [PubMed] [Google Scholar]
- Diefenbach MA, Butz BP. A multimedia interactive education system for prostate cancer patients: development and preliminary evaluation. Journal of Medical Internet Research. 2004;6(1) doi: 10.2196/jmir.6.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diefenbach MA, Mohamed NE, Butz BP, Bar-Chama N, Stock R, Cesaretti J, et al. A pilot study to examine the feasibility and preliminary outcomes of an interactive, multimedia education and decision program for early-stage prostate cancer patients. Journal of Medical Internet Research. 2012;14(1):e6. doi: 10.2196/jmir.1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- DuBenske L, Gustafson D, Namkoong K, Hawkins R, Atwood A, Brown R, Chih M, McTavish F, Carmack C, Buss M, Govindan R, Cleary J. CHESS improves cancer caregivers’ burden and mood: Results of an eHealth RCT. Health Psychology. doi: 10.1037/a0034216. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuBenske L, Gustafson D, Shaw B, Cleary J. Web-based cancer communication and decision making systems: connecting patients, caregivers, and clinicians for improved health outcomes. Medical Decision Making. 2010;30(6):732–744. doi: 10.1177/0272989X10386382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuBenske LL, Chih MY, Dinauer S, Gustafson DH, Cleary JF. Development and implementation of a clinician reporting system for advanced stage cancer: initial lessons learned. Journal of the American Medical Informatics Association. 2008;15(5):679–686. doi: 10.1197/jamia.M2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont S, Turgeon J, Allard P, Gagnon P, Charbonneau C, Vézina L. Caring for a loved one with advanced cancer: determinants of psychological distress in family caregivers. Journal of Palliative Medicine. 2006;9(4):912–921. doi: 10.1089/jpm.2006.9.912. [DOI] [PubMed] [Google Scholar]
- Ellison NB, Steinfield C, Lampe C. The benefits of Facebook “friends:” Social capital and college students’ use of online social network sites. Journal of Computer-Mediated Communication. 2007;12(4):1143–1168. [Google Scholar]
- Evers KE, Prochaska JM, Prochaska JO, Driskell MM, Cummins CO, Velicer WF. Strengths and weaknesses of health behavior change programs on the Internet. Journal of Health Psychology. 2003;8(1):63–70. doi: 10.1177/1359105303008001435. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. Journal of Medical Internet Research. 2005;7(1) doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. BMJ. 2004;328(7449):1166. doi: 10.1136/bmj.328.7449.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farnham S, Cheng L, Stone L, Zaner-Godsey M, Hibbeln C, Syrjala K, Clark AM, Abrams J. HutchWorld: clinical study of computer-mediated social support for cancer patients and their caregivers. Paper presented at the Proceedings of the SIGCHI Conference on Human Factors in Computing Systems.2002. [Google Scholar]
- Fredman SJ, Baucom DH, Gremore TM, Castellani AM, Kallman TA, Porter LS, Kirby JS, Claire Dees E, Klauber-Demore N, Peppercorn J, Carey LA. Quantifying the recruitment challenges with couple-based interventions for cancer: applications to early-stage breast cancer. Psycho-Oncology. 2009;18(6):667–673. doi: 10.1002/pon.1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths C, Norton L, Wagstaff G, Brunas-Wagstaff J. Existential concerns in late stage cancer. European Journal of Oncology Nursing. 2002;6(4):243–246. doi: 10.1054/ejon.2002.0205. [DOI] [PubMed] [Google Scholar]
- Gustafson D, DuBenske L, Namkoong K, Hawkins R, Chih M, Atwood A, Johnson R, Bhattacharya A, Carmack C, Traynor A, Campbell T, Buss M, Govindan R, Schiller J, JFC An eHealth system supporting palliative care for patients with nonsmall cell lung cancer: A randomized trial. Cancer. 2013;119:1744–1751. doi: 10.1002/cncr.27939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson D, Hawkins R, McTavish F, Pingree S, Chen W, Volrathongchai K, Stengle W, Stewart J, Serlin R. Internet-Based Interactive Support for Cancer Patients: Are Integrated Systems Better? Journal of Communication. 2008;58(2):238–257. doi: 10.1111/j.1460-2466.2008.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, Chan CL. Impact of a patient-centered, computer-based health information/support system. Am J Prev Med. 1999;16(1):1–9. doi: 10.1016/s0749-3797(98)00108-1. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Hawkins RP. Computer-based support systems for women with breast cancer. Journal of the American Medical Association. 1999;281:1268–1269. [Google Scholar]
- Gysels MH, Higginson IJ. Caring for a person in advanced illness and suffering from breathlessness at home: threats and resources. Palliative and Supportive Care. 2009;7(02):153–162. doi: 10.1017/S1478951509000200. [DOI] [PubMed] [Google Scholar]
- Han J, Hawkins R, Shaw B, Pingree S, McTavish F, Gustafson D. Unraveling uses and effects of an interactive health communication system. Journal of Broadcasting & Electronic Media. 2009;53(1):112–133. doi: 10.1080/08838150802643787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, Wise M, Kim E, Pingree R, Hawkins R, Pingree S, McTavish F, Gustafson D. Factors associated with use of interactive cancer communication system: An application of the comprehensive model of information seeking. Journal of Computer-Mediated Communication. 2010;15(3):367–388. doi: 10.1111/j.1083-6101.2010.01508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Speaking of health: Assessing health communication strategies for diverse populations. National Academy Press; 2002. [PubMed] [Google Scholar]
- Jacobsen P, Stein K. Is fatigue a long-term side effect of breast cancer treatment? Cancer Control. 1999;6:256–263. doi: 10.1177/107327489900600304. [DOI] [PubMed] [Google Scholar]
- Kalayjian AS. Coping with cancer: the spouse’s perspective. Archives of Psychiatric Nursing. 1989;3(3):166. [PubMed] [Google Scholar]
- Kopp RP, Marshall LM, Wang PY, Bauer DC, Barrett-Connor E, Parsons JK. The Burden of Urinary Incontinence and Urinary Bother Among Elderly Prostate Cancer Survivors. European Urology. 2013 doi: 10.1016/j.eururo.2013.03.041. epub before print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari M, Head J, Marmot M. Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Archives of Internal Medicine. 2004;164(17):1873–1880. doi: 10.1001/archinte.164.17.1873. [DOI] [PubMed] [Google Scholar]
- Lepore SJ, Revenson TA. Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass. 2007;1(1):313–333. [Google Scholar]
- Liess A, Simon W, Yutsis M, Owen JE, Piemme KA, Golant M, Giese-Davis J. Detecting emotional expression in face-to-face and online breast cancer support groups. Journal of Consulting and Clinical Psychology. 2008;76(3):517–523. doi: 10.1037/0022-006X.76.3.517. [DOI] [PubMed] [Google Scholar]
- Liu X, LaRose R. Does using the Internet make people more satisfied with their lives? The effects of the Internet on college students’ school life satisfaction. CyberPsychology & Behavior. 2008;11(3):310–320. doi: 10.1089/cpb.2007.0040. [DOI] [PubMed] [Google Scholar]
- Manne S, Badr H. Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer. 2008;112(11 Suppl):2541–2555. doi: 10.1002/cncr.23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Schnoll R. Measuring supportive and unsupportive responses during cancer treatment: A factor analytic assessment of the partner responses to cancer inventory. Journal of Behavioral Medicine. 2001;24(4):297–321. doi: 10.1023/a:1010667517519. [DOI] [PubMed] [Google Scholar]
- Manne S, Taylor KL, Dougherty J, Kerneny N. Supportive and negative responses in close relationships: Their association with psychological adjustment among individuals with cancer. Journal of Behavioral Medicine. 1997;20:101–126. doi: 10.1023/a:1025574626454. [DOI] [PubMed] [Google Scholar]
- Markman HJ, Renick MJ, Floyd FJ, Stanley SM, Clements M. Preventing marital distress through communication and conflict management training: a 4-and 5-year follow-up. Journal of Consulting and Clinical Psychology. 1993;61(1):70. doi: 10.1037//0022-006x.61.1.70. [DOI] [PubMed] [Google Scholar]
- Matthews AB. Role and gender differences in cancer-related distress: A comparison of survivor and caregiver self-reports. Paper presented at the Oncology Nursing Forum; 2003. [DOI] [PubMed] [Google Scholar]
- Mayer D, Terrin N, Kreps G, Menon U, McCance K, Parsons S, Mooney K. Cancer survivors information seeking behaviors: a comparison of survivors who do and do not seek information about cancer. Patient Education and Counseling. 2007;65(3):342–350. doi: 10.1016/j.pec.2006.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTavish FM, Hawkins RP, Gustafson DH, Pingree S, Shaw BR. Experiences of women with breast cancer: Exchanging social support over the CHESS computer network. Journal of Health Communication. 2000;5(2):135–159. doi: 10.1080/108107300406866. [DOI] [PubMed] [Google Scholar]
- Milne D, Sheeran L, Holmes M, Tidhar G, Aranda S. Trialling a patient-led cancer care website in an acute cancer care setting. Journal of Research in Nursing. 2012;17(6):538–554. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Murray S, Boyd K, Kendall M, Worth A, Benton T, Clausen H. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. British Medical Journal. 2002;325(7370):929. doi: 10.1136/bmj.325.7370.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff LA, Karney BR. Gender differences in social support: A question of skill or responsiveness? Journal of Personality and Social Psychology. 2005;88(1):79. doi: 10.1037/0022-3514.88.1.79. [DOI] [PubMed] [Google Scholar]
- Newman MW, Lauterbach D, Munson SA, Resnick P, Morris ME. It’s not that I don’t have problems, I’m just not putting them on Facebook: challenges and opportunities in using online social networks for health. Paper presented at the Proceedings of the ACM 2011 conference on Computer supported cooperative work.2011. [Google Scholar]
- Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A Review of eHealth Interventions for Physical Activity and Dietary Behavior Change. American Journal of Preventive Medicine. 2007;33(4):336–345. e316. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with Family Caregivers of Cancer Patients: Meta-Analysis of Randomized Trials. CA: A Cancer Journal for Clinicians. 2010;60(5):317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osse BH, Vernooij-Dassen MJ, Schadé E, Grol RP. Problems experienced by the informal caregivers of cancer patients and their needs for support. Cancer Nursing. 2006;29(5):378–388. doi: 10.1097/00002820-200609000-00005. [DOI] [PubMed] [Google Scholar]
- Owen JE, Bantum EO, Golant M. Benefits and challenges experienced by professional facilitators of online support groups for cancer survivors. Psychooncology. 2009;18(2):144–155. doi: 10.1002/pon.1374. [DOI] [PubMed] [Google Scholar]
- Patrick K, Robinson TN, Alemi F, Eng TR. Policy issues relevant to evaluation of interactive health communication applications. American Journal of Preventive Medicine. 1999;16(1):35–42. [PubMed] [Google Scholar]
- Pirri C, Bayliss E, Trotter J, Olver I, Katris P, Drummond P, Bennett R. Nausea still the poor relation in antiemetic therapy? The impact on cancer patients’ quality of life and psychological adjustment of nausea, vomiting and appetite loss, individually and concurrently as part of a symptom cluster. Supportive Care in Cancer. 2013;21(3):735–748. doi: 10.1007/s00520-012-1574-9. [DOI] [PubMed] [Google Scholar]
- Pistrang N, Barker C. The partner relationship in psychological response to breast cancer. Social Science & Medicine. 1995;40:789–797. doi: 10.1016/0277-9536(94)00136-h. [DOI] [PubMed] [Google Scholar]
- Poirier J, Cobb NK. Social influence as a driver of engagement in a web-based health intervention. Journal of Medical Internet Research. 2012;14(1) doi: 10.2196/jmir.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Garst J, McBride CM, Baucom D. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: Associations with symptoms & distress. Pain. 2008;137(2):306. doi: 10.1016/j.pain.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis J, McGinty B, Jones S. An e-learning caregiving program for prostate cancer patients and family members. Journal of Medical Systems. 2003;27(1):1–12. doi: 10.1023/a:1021040911088. [DOI] [PubMed] [Google Scholar]
- Schmaling KB, Sher TG. The psychology of couples and illness. Washington, DC: American Psychological Association; 2000. [Google Scholar]
- Schover LR, Yuan Y, Sui D, Neese L, Jenkins R, Rhodes MM. A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer. 2012;118(2):500–509. doi: 10.1002/cncr.26308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22(5):487. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- Shaw BR, Hawkins R, McTavish F, Pingree S, Gustafson DH. Effects of insightful disclosure within computer mediated support groups on women with breast cancer. Health Commun. 2006;19(2):133–142. doi: 10.1207/s15327027hc1902_5. [DOI] [PubMed] [Google Scholar]
- Silveira MJ, Given CW, Cease KB, Sikorskii A, Given B, Northouse LL, Piette JD. Cancer CarePartners: Improving patients’ symptom management by engaging informal caregivers. BMC Palliative Care. 2011;10(1):21. doi: 10.1186/1472-684X-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychological Medicine. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Social support as coping assistance. Journal of Consulting and Clinical Psychology. 1986;54:416–423. doi: 10.1037//0022-006x.54.4.416. [DOI] [PubMed] [Google Scholar]
- Tixier M, Lewkowicz M. Online Communities and Social Computing. Springer; 2011. Design and evaluation of an online social support application for family caregivers; pp. 267–276. [Google Scholar]
- van de Poll-Franse L, van Eenbergen M. Internet use by cancer survivors: current use and future wishes. Supportive Care in Cancer. 2008;16(10):1189–1195. doi: 10.1007/s00520-008-0419-z. [DOI] [PubMed] [Google Scholar]
- Van den Beuken-van Everdingen M, De Rijke J, Kessels A, Schouten H, Van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Annals of Oncology. 2007;18(9):1437. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- Viola R, Kiteley C, Lloyd NS, Mackay JA, Wilson J, Wong RK. The management of dyspnea in cancer patients: a systematic review. Supportive Care in Cancer. 2008;16(4):329–337. doi: 10.1007/s00520-007-0389-6. [DOI] [PubMed] [Google Scholar]
- von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. Journal of cachexia, sarcopenia and muscle. 2010;1(1):1–5. doi: 10.1007/s13539-010-0002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walther JB, Boyd S. Attraction to computer-mediated social support. Communication technology and society: Audience adoption and uses, 153188 2002 [Google Scholar]
- Wang HX, Mittleman MA, Orth-Gomer K. Influence of social support on progression of coronary artery disease in women. Social Science and Medicine. 2005;60(3):599–607. doi: 10.1016/j.socscimed.2004.05.021. [DOI] [PubMed] [Google Scholar]
- Weiss JB, Lorenzi NM. Online communication and support for cancer patients: a relationship-centric design framework. Paper presented at the AMIA Annual Symposium Proceedings; 2005. [PMC free article] [PubMed] [Google Scholar]
- Weiss JB, Lorenzi NM. Interface Design for Patient-Caregiver Integrated Network. Paper presented at the AMIA Annual Symposium Proceedings; 2006. [PMC free article] [PubMed] [Google Scholar]
- Wingate AL, Lackey NR. A description of the needs of noninstitutionalized cancer patients and their primary care givers. Cancer Nursing. 1989;12(4):216–225. [PubMed] [Google Scholar]
- Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Zulman DM, Schafenacker A, Barr KLC, Moore IT, Fisher J, McCurdy K, Derry HA, Saunders EW, An LC, Northouse L. Adapting an in-person patient–caregiver communication intervention to a tailored web-based format. Psycho-Oncology. 2012 doi: 10.1002/pon.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]