ABSTRACT
Gastric duplication cyst is a rare anomaly, and most cases are recognized during childhood. Recently, several pediatric cases with small gastric duplication cysts treated by laparoscopic resection have been reported. Here, we describe an infant in whom we successfully performed laparoscopic partial gastrectomy for the treatment of a huge gastric duplication cyst. To the best of our knowledge, this is the largest gastric duplication cyst treated by laparoscopic surgery among infants. We introduce our procedure and some tips.
Key Words: Duplication cyst, Gastric, Laparoscopic surgery, Partial gastrectomy, Pediatric
INTRODUCTION
Gastric duplication cyst is a rare anomaly that accounts for 2–7% of all gastrointestinal duplications.1) Most cases are recognized during childhood with nonspecific symptoms, such as nausea, vomiting, weight loss, or an epigastric mass. Gastric duplication cyst is typically treated surgically because of the symptoms and risk of malignant changes.1, 2) Recently, several pediatric cases with small gastric duplication cysts treated by laparoscopic resection have been reported (Table 1).3-7) Here, we describe an infant in whom we successfully performed laparoscopic partial gastrectomy for the treatment of a huge gastric duplication cyst.
Table 1.
Laparoscopic surgery for pediatric patient with gastric duplication cyst
| Age | Sex | Size (cm) | Location | Surgery | Author / Year |
|---|---|---|---|---|---|
| 14 y | F | 4 | Posterior wall of cardia | Cystectomy | Sasaki T et al. 2003 3) |
| 2 m | M | 2.2 | Posterior wall of body | Cystectomy | Ford WD et al. 2004 4) |
| 3 y | M | 3 | Greater curvature of antrum | Cystectomy | Take H et al. 2008 5) |
| 17 m | Unknown | Unknown | Unknown | Cystectomy | Laje P et al. 2010 6) |
| 11 d | F | Unknown | Pylorus | Convert to open, Enucleation |
Chin AC et al. 2011 7) |
| 2 m | M | 8 × 3 × 3 | Greater curvature of body | Partial gastrectomy | Present study |
CASE PRESENTATION
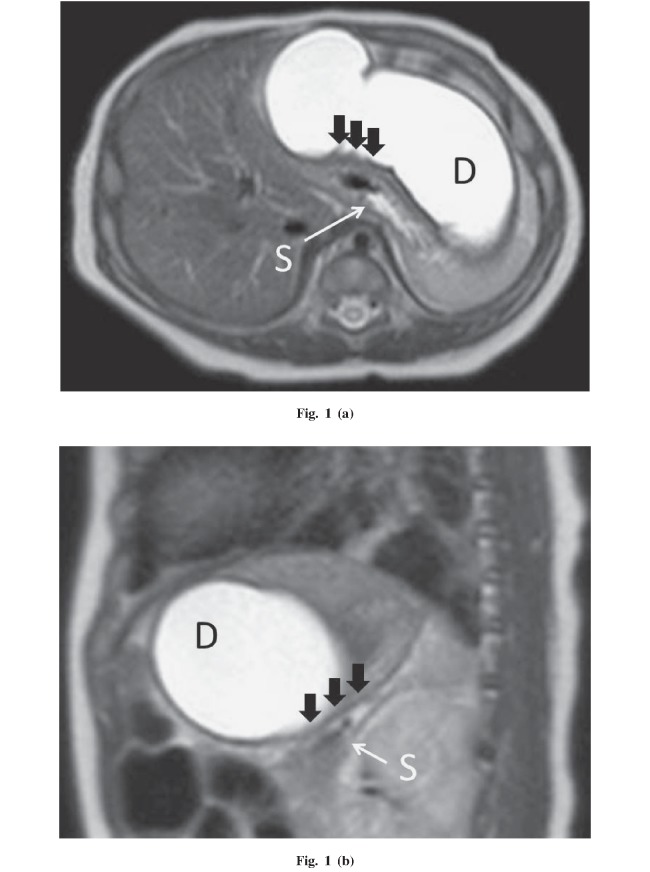
A 2-month-old male patient was referred to our hospital with non-bilious projectile vomiting. His elder brother had hypertrophic pyloric stenosis that had been treated by laparoscopic pyloromyotomy in our hospital, and we suspected that this patient had the same disease. However, ultrasonography revealed an intact pylorus and a huge cyst compressing the greater curvature of the stomach. Magnetic resonance imaging (MRI) showed an 8 × 3 × 3-cm cyst in the left upper peritoneal cavity (Figures 1a, 1b). Because the muscular layer was shared by the cyst and stomach on MRI, we diagnosed a gastric duplication cyst. A barium meal showed a compressed stomach and no communication between the stomach and cyst.
Fig. 1.
The horizontal (a) and sagittal (b) views on magnetic resonance imaging. The muscular layer is shared by the cyst and stomach (black arrows). S: stomach. D: duplication cyst.
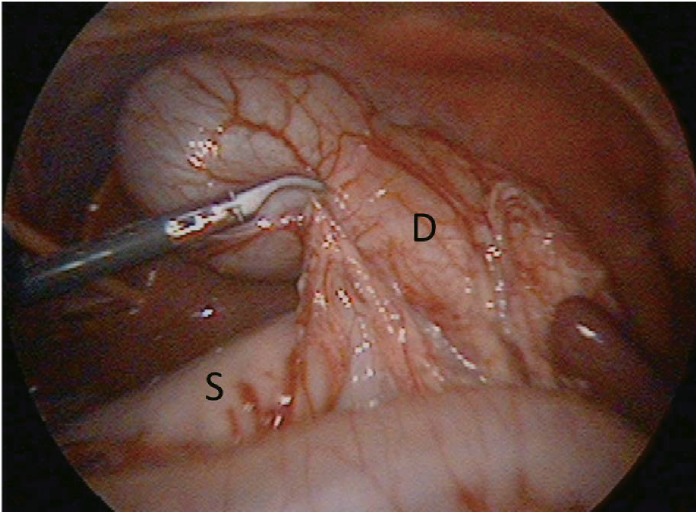
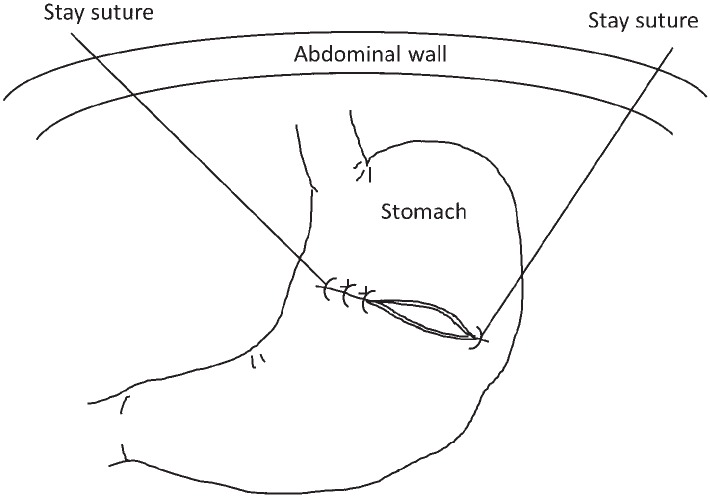
Laparoscopic resection of the gastric duplication cyst was performed using a 5-mm, 30-degree camera and 4 ports, including a 12-mm port in the umbilicus and three 5-mm ports. The cyst arose from the greater curvature of the stomach (Figure 2), and the shared muscular layer was detected by intraoperative ultrasonography. At the beginning of the operation, fluid in the duplication cyst was aspirated by a SAND balloon catheter (Hakko Medical, Nagano, Japan) introduced through an umbilical port. The tumor was separated from the gastrocolic ligament using an ultrasonic coagulating dissector. Because of the wide lesion shearing the muscular layer and inflammation-related adhesion between the gastric mucosa and sheared muscular layer, we resected the duplication cyst through the full thickness of the gastric wall. The specimen was placed in a bag (Endo Catch Gold, Covidien, Mansfield, MA, USA) and removed via an umbilicus incision. The stomach was closed with an Albert-Lembert suture parallel to the short axis using 3-0 PDSII. The threads of the first two stitches on both sides were drawn outside to lift the suture line (Figure 3). The peritoneal cavity was lavaged with normal saline. The wounds were closed in a typical fashion, and no drain was placed. The total operative time was 262 min, with minimal blood loss. Pathology of the specimen revealed gastric duplication cyst with gastric mucosa (Figure 4). The patient started oral intake on postoperative day 3 and was discharged on postoperative day 9 without any complications.
Fig. 2.
Operative findings. The duplication cyst arises from the greater curvature of the stomach and receives feeding vessels from the gastrocolic ligament. S: stomach. D: duplication cyst.
Fig. 3.
Schema of the operation. The stomach was closed with an Albert-Lembert suture parallel to the short axis. The threads of the first two stitches on both sides were kept as stay sutures and drawn outside to lift the suture line.
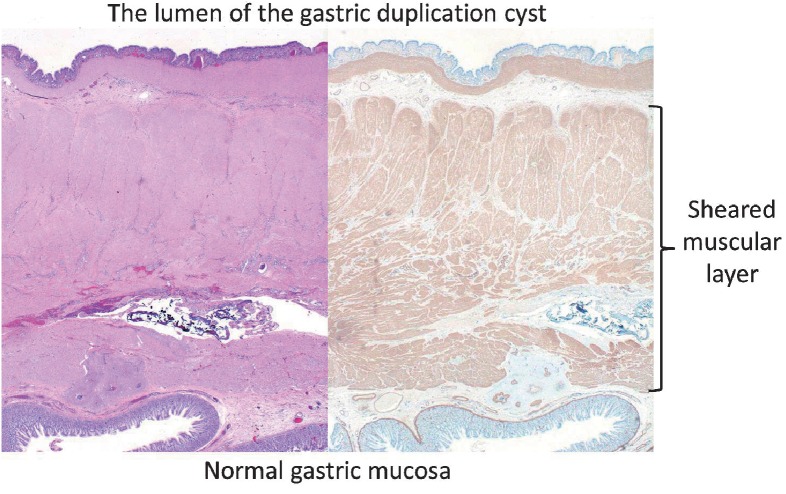
Fig. 4.
Pathology of the specimen revealing gastric duplication cyst with gastric mucosa. Left side: hematoxylin and eosin stain; Right side: immunohistochemistry of smooth muscle actin.
DISCUSSION
Depending on the location and size, the presentation of gastric duplication cyst varies from gastric outlet obstruction to asymptomatic occurrence. This case presented with non-bilious projectile vomiting such as that with hypertrophic pyloric stenosis. Previous reports include a 10-month-old female infant, who had presented with non-bilious vomiting, with an 8 × 6-cm cyst arising from the greater curvature of the stomach treated by open surgery.8) Ford et al.4) reported a 2-month-old female baby with an asymptomatic 2.2-cm antenatal cyst detected at the back wall of the stomach treated by elective laparoscopic surgery. Broad consensus indicates surgical treatment of asymptomatic gastric duplication cyst because of the risk of malignant changes.1, 2) Minimally invasive resection of gastric duplication cyst for pediatric patients is acceptable; Liu et al. reported that carcinomas arising from gastric duplication cysts generally occur in middle-aged adults (median age, 56 years; range, 25–71 years).9)
To our knowledge, this is the largest gastric duplication cyst treated by laparoscopic surgery among infants. We suggest the following tips for the laparoscopic treatment of a large gastric duplication cyst. (1) A nasogastric tube should be placed before the operation to achieve sufficient decompression. (2) At the beginning of the operation, fluid in the duplication cyst should be aspirated using a needle. We usually use a SAND balloon catheter with a double balloon that is designed to minimize the risk of spillage.10) In adult patients, this procedure should be performed with caution. Malignant changes in the duplication cyst must be ruled out. (3) When the stomach requires suturing, the threads of the first two stitches at both sides should be drawn outside to lift the suture line (Figure 3). This technique enables suturing and minimizes the risk of irregularity in the distance between the stitches. In addition, we recommend that the suture line should be parallel to the short axis of the stomach to prevent stenosis. (4) When adequate working space is not obtained by aspiration or complete resection of the duplication cyst is not achieved, the surgeon should not hesitate to convert to open surgery. Intraoperative complications, such as bleeding, are also sufficient to justify conversion.
The layer of resection should be carefully considered. With partial full-thickness gastrectomy, resection of just the cyst in combination with repair of the muscle layer has been suggested as the treatment of choice; however, it is difficult with large cysts that share a considerable portion of the muscular layer, as in the present case. If the shared portion of the muscular layer is larger, the risk of mucosal perforation or residual duplication cyst increases, even with open surgery. Laparoscopic partial gastrectomy for a huge gastric duplication cyst was feasible and provided a good cosmetic result with no complications. Partial full-thickness gastrectomy could be easily performed using laparoscopic linear staplers, if the muscle layer shared with the cyst is not large.11)
In conclusion, in the present case, a 2-month-old infant with a huge gastric duplication cyst was treated successfully by laparoscopic partial gastrectomy, which was feasible and provided a good cosmetic result with no complications.
Conflict of Interest
None
REFERENCES
- 1).Coit DG, Mies C. Adenocarcinoma arising within a gastric duplication cyst. J Surg Oncol, 1992; 50: 274–277. [DOI] [PubMed]
- 2).Zheng J, Jing H. Adenocarcinoma arising from a gastric duplication cyst. Surg Oncol, 2012; 21: e97–101. [DOI] [PubMed]
- 3).Sasaki T, Shimura H, Ryu S, Matsuo K, Ikeda S. Laparoscopic treatment of a gastric duplication cyst: report of a case. Int Surg, 2003; 88: 68–71. [PubMed]
- 4).Ford WD, Guelfand M, López PJ, Furness ME. Laparoscopic excision of a gastric duplication cyst detected on antenatal ultrasound scan. J Pediatr Surg, 2004; 39: e8–10. [DOI] [PubMed]
- 5).Take H, Ohhama Y, Shinkai M, Kitagawa N, Kudou H, Mochizuki K, Hatata T. Laparoscopic resection of a gastric duplication cyst: case report. Jpn J Pediatr Surg, 2008; 40: 1086–1090.
- 6).Laje P, Flake AW, Adzick NS. Prenatal diagnosis and postnatal resection of intraabdominal enteric duplications. J Pediatr Surg, 2010; 45: 1554–1558. [DOI] [PubMed]
- 7).Chin AC, Radhakrishnan RS, Lloyd J, Reynolds M. Pyloric duplication with communication to the pancreas in a neonate simulating hypertrophic pyloric stenosis. J Pediatr Surg, 2011; 46: 1442–1444. [DOI] [PubMed]
- 8).G KK. Gastric duplication cyst in an infant presenting with non-bilious vomiting. Malays J Med Sci, 2012; 19: 76–78. [PMC free article] [PubMed]
- 9).Liu K, Lin X, Wu J, Liu H, Meng M, Su H, Tai W, Chang H. Peritoneal metastatic adenocarcinoma possibly due to a gastric duplication cyst: a case report and literature review. BMC Gastroenterol, 2014; 14: 48. [DOI] [PMC free article] [PubMed]
- 10).Yamada T, Okamoto Y, Kasamatsu H. Use of the SAND balloon catheter for the laparoscopic surgery of benign ovarian cysts. Gynecol Endosc, 2000; 9: 51–54.
- 11).Wakabayashi H, Okano K, Yamamoto N, Suzuki Y, Inoue H, Kadota K, Haba R. Laparoscopically resected foregut duplication cyst (bronchogenic) of the stomach. Dig Dis Sci, 2007; 52: 1767–1770. [DOI] [PubMed]