Abstract
Objective
Mental health is an essential component for positive adaptation that enables people to cope with adversity to achieve their full potential and humanity. In this study, using a community based approach, the social determinants of mental health in Iranian women were extracted; and in addition, priority setting for interventional programs according to analytical framework of WHO was implemented.
Method
This study was a community based participatory research (CBPR) in district 22 of Tehran (Iran). The target group was married females with age range of 18-65 years. In this study, mental health priorities were extracted by qualitative methods according to Essential National Health Research model (ENHR) and the analytical framework of WHO. Data analysis was done based on content analysis by the open code 3.6 software.
Results
In the quantitative phase, according to secondary data, 1144 individuals (560 females and 584 males) were selected, of whom 41 percent had impaired mental health based on General Health Questionnaire (GHQ) (P<0.05). According to the qualitative phase, the first mental health priority in socioeconomic level was lack of insurance for unattended families, it was unemployment in differential exposure level and it was lack of knowledge and skills related to dealing with stress in the differential vulnerability level; in differential outcome and consequence levels, the priorities were lack of free counseling centers in the study area and lack of facilities for mental health rehabilitation.
Conclusion
Providing training courses to improve the skills to deal with stress is considered one of the most important interventions for mental health promotion in women.
Keywords: Social Determinant, Mental Health, Priority Setting, Participatory Research, Iran
Mental health is an essential component for positive adaptation that enables people to cope with adversity to achieve their full potential and humanity (1). Mental health is also the key to understanding the impact of inequalities on health (2). The significance of mental health and its role in health outcomes confirms the importance of humans in community, but it does not mean that we should ignore the mental character and power of the individual. Mental disorders are responsible for one third of Years Lived with Disability (YLD) in the world (3). Also, different studies showed that the prevalence of mental disorders in women is more than men (4). In Iran, based on urban HEART study, the prevalence of mental disorder was 38% in Tehran in 2008 (twice in females)(5). Understanding the social determinants of mental health and set their priorities based on community participation are essential to design appropriate interventions for mental health promotion. This process guides the policy makers to design primary prevention plans for mental disorders and provide maximum social welfare (6). In 2007, in the commission on social determinations of health, World Health Organization suggested a five-level priority public health conditions analytical framework that consisted of socioeconomic context and position, differential exposure, vulnerability, health care outcomes and differential consequences to design intervention (7).
The socioeconomic context has a powerful effect on societal distribution of health conditions. In 2004, Bhugra and colleagues investigated the relation between socioeconomic reform and mental disorders and found that rapid changes in the configuration of societies can cause substantial increase in societal burden of mental disorders (8). Differential exposures to risk factors such as stressful life events, social conflict, civil unrest, natural disasters and working environments have strong association with mental health problems (9). In differential vulnerability stage, individual characters such as gender, age, health status, marital status and income affect mental health (10). Chronic physical ill-health, female gender and being a young adult can increase the vulnerability to mental health problems (11).
Lack of mental health literacy and stigma reduce the ability to use health care services (12). Increased financial cost of treatment for mental disorders, loss of job and earning are different consequents of mental health problems (13).
In many studies, different interventions for mental health problems target the five levels of this analytical framework (14, 15). In Iran, there are some interventional programs for the promotion of mental health in different age groups (16, 17), but in the present study, using community participatory research approach, the social determinants of mental disorders were extracted and priority setting for interventional programs according to analytical framework of WHO was implemented.
Material and Methods
This was a community based participatory research(CBPR) conducted for needs assessment and setting priorities for women’s mental health in district 22 in western part of Tehran. This method was selected because the CBPR begins with a research topic of importance to community with the aim of combining knowledge and action for a social change to improve the community’s health and eliminate health disparities. It is a participatory, cooperative and capacity building process that achieves a balance between research and action.
The district 22 of Tehran has an approximate population of 100 thousand, of which, 49% are women; this district has nine zones and has also special characteristics such as easy access to the community, having active humanitarian organizations and hyper active volunteers that led us to select this district as the venue of our study. In this area, more than 41% of the population has impaired mental health (18).
For needs assessment, we used ENHR approach (8) that has four phases: Stakeholder’s analysis, preparatory phase, needs assessment and priority setting. In the third phase, gathering the secondary data was implemented as a quantitative study, and focus group discussion sessions and in-depth interviews were carried out as the qualitative part.
A- Stakeholders analysis
This part has three steps consisting of identifying stakeholders and prioritizing them based on some criteria such as influence, power, interest and finally considering key stakeholders. To implement these steps, the following actions were taken:
At first, we coordinated with regional stakeholders and key persons and explained them the aim of the study. Volunteers were chosen according to some criteria such as being married, having at least high school diploma and motivation to participate in activities, and finally ten candidates were selected. The volunteers had to do the necessary arrangements in order to carry out the different steps of the study which were as follows:
To encourage the community to participate in the needs assessment process
To carry out the focus group discussion sessions with married women and conducting in- depth interviews with key persons.
Knowing different disciplines in the area and forming the intersectional and multidisciplinary working groups.
Providing a check list of stakeholders. This check list consisted of all stakeholders’ names which were prioritized based on some criteria.
B-Preparatory phase
Doing preparatory work which consisted of awareness raising and capacity building, reaching agreement with the stakeholders and planning for needs assessment and priority setting. One of the most important parts of this process is capacity building of the individuals. One training workshop was conducted for the volunteers.
C-Needs assessment
C1- Quantitative study
Gathering secondary data such as demographic characteristics, executive programs and extracting the results of the 28-item version of the General Health Questionnaire (GHQ) from Urban Health Equity Assessment and Response Tool (Urban HEART). In Tehran, an improved model incorporates the six domains of infrastructure, social and humanity development, economics, governance, health and nutrition.
GHQ
In 1999, this questionnaire was translated to the official language of Iran (Farsi), and its validity and reliability were approved in an independent study by Noorbala (19). The best cutoff point was 6; and those participants who scored 6 and above were designated as possible cases of mental disorder. The sensitivity, specificity and overall misclassification rate for the GHQ 28 cut-off score of 6 were 84.7%, 93.8% and 8.2%, respectively (19).
C2- Qualitative study
A qualitative study was done to extract the mental health needs and their social determinants in women. Four focus group discussions (FGD) with married women and five in- depth interviews with key stakeholders were conducted to reach data saturation. The guide questionnaires consisted of three general questions related to mental health needs, mental health priorities and appropriate interventions followed by some probes such as when, who, how, where and so on. Each interview lasted for almost one hour, and informed consent was obtained from all the participants. After each session, the taken notes were completed with recorded tapes.
The analysis of health situation consisted of health status and health system in the study area.
Different techniques such as brainstorming and nominal group (20) with stakeholders were used to assign the scoring system.
D-Priority setting
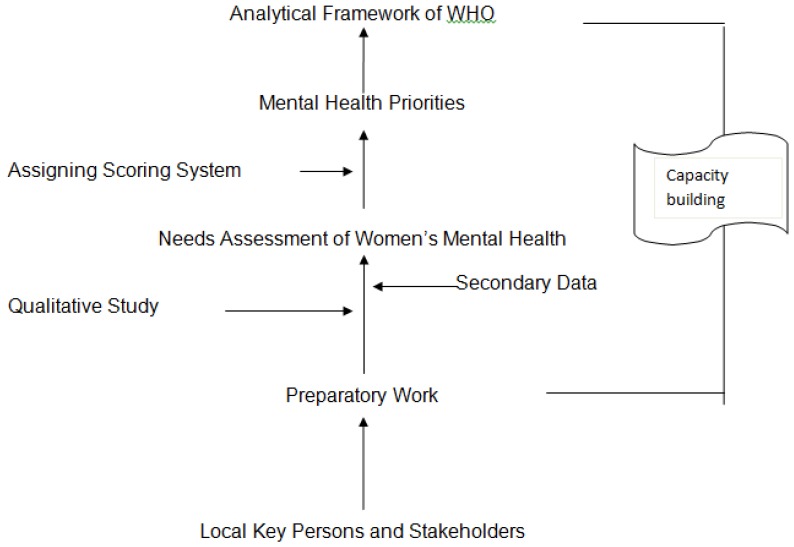
Using the bottom up approach or ENHR model (6), the mental health priorities were extracted by stakeholders’ participation; and then based on the public health analytical framework of WHO, five levels of social determinants, priorities and interventional programs were determined. (Figure 1)
Figure 1. The Process of Determining Women’s Mental Health Priorities.
Data analysis
Data analysis in the qualitative study was done based on conventional content analysis. In this method of analysis, coding categories are derived directly from the text data (21). In order to increase the reliably of the data, all codes and classes were cross-checked by the research team. To address conformability, we shared the summarized interview findings with the key persons at the end of the interview (respondent validation) to get find the participants’ recognition of the finding (22). To assess dependability, peer checking was done by an experienced colleague to re-analyze some of the data was performed. Team consistency checks between colleagues were also performed throughout the coding process (23).
Ethical Considerations
In this study, ethical issues were considered. Informed consent was obtained from all the participants. They were assured that the data would be managed in line with regulations in the law of confidentiality and anonymity. The Local Ethics Committee of Welfare and Social Science University approved the study design.
Results
Based on the ENHR model, four steps were implemented. In this part, we presented the result of the three steps. The preparatory work consisted of some actions which were explained in the method’s section.
A- StakeholdersAnalysis
Based on the stakeholder’s analysis, the five categories are as follows:
Team researchers
Decision makers on provincial and district levels
Health service providers at the district level
Charitable actions
The most important category is community.
B-Needs Assessment
This phase has two sections. In the quantitative phase, the status of mental health was extracted by GHQ via Urban HEART developed by the WHO office (5) (Table 1).
Table 1.
The Status of Different Domains of Mental Health Based on GHQ
| Indicator | District 22 (%) | Tehran (%) |
|---|---|---|
| Anxiety | 38.6 | 38 |
| somatization | 36.6 | 37 |
| Impaired social function | 22.7 | 26 |
| depression | 35.2 | 36 |
| Impaired mental health | 41.01 | 41 |
In the qualitative study, four FGD and five in-depth interviews were implemented. The characteristics of the participants in the FGD are as follows:
The participants in the individual interviews consisted of the representatives from the municipality, health centers, two of volunteers and one member from of the NGO related to women’s health in the district.
Based on data saturation, and according to the analytical framework of WHO in mental health condition, five categories and twenty sub categories related to social determinants of mental disorders are extracted as follows:
- Socioeconomic and position: this category was presented by key persons. It seems that these needs were related to the national level. There are four sub- categories in this level consist of: including instability on policy and planning, social gradient, lack of insurance for unattended family families and income inequality.
Member of NGO said: “Instability on of policy can cause mental health problems, because you cannot have any plans for your life. Today you are wealthy, but tomorrow you will may be poor.”
- Differential Exposure: Based on the views of the majority of participants’ view, there are some exposures leading to impaired mental health such as unemployment, income insecurity and increased living costs that can lead cause to a decrease in social welfare.
Married women in FGD said: “when you are poor and cannot pay the rent, you will be depressed”.
Representative A representative from municipality: commented, “Income insecurity as much as unemployment can create mental disorders”.
Globalization, internet access and changing changes in the cultural norms, despite some benefits, can make cause complex problems especially particularly for the youth. In addition, in the opinions of the majority of the participants tobacco use and addiction could in opinion’s majority of participants destroy the capacities of the community.
- Differential vulnerability: in this regard, two important needs were expressed by most of the women, : at first lack of mental health literacy and then lack of knowledge and skills related to dealing with stress.
Most of married women in the FGD: said,” we don’t know how to manage the techniques of our stress management and or how to dealing deal with daily stress pressure”.
-
- Differential health outcome: In this category, three important sub- categories were presented as follows:
- lack of free counseling centers in the study area
- stigma and delay in help seeking
- lack of access to mental health services
Representative from a health center said:“To promote mental health, having access to mental health services and free counseling centers in the district are needed to mental health promotion ”.
The above mentioned categories are related to the prevention of mental disorders, but the following themes are related to harm reduction.
- Differential Consequences: the most important need in this part is Lacking of facilities for mental health rehabilitation is an important issue needing attention, and. Failure to response to satisfy this need may be create social exclusion and reduce the ability to work.
C-Priority Setting
During the nominal group and brain storming sessions with participation of the key persons and research team, some criteria (Table 3) for setting the priorities were extracted. These criteria consisted of three main categories and seven sub-categories. Based on the participants’ view, for each subcategory, scores 0-3 was considered.
Table 3.
Mental Health Priority Setting Criteria
| Main Category | Sub- category |
|---|---|
| Appropriateness |
|
| Relevancy |
|
| Chance of Success |
|
After a score was given to each of the social determinants of mental disorders in each level, the first important priority was determined (Table 4).
Table 4.
The Most Important Priority of Women’s Mental Health
| Level of Conceptual Framework | First Priority in Each Level | Authorities for Intervention |
|---|---|---|
| Socioeconomic Status and Position | lack of Insurance for Unattended Families | Policy Makers in National Level /Legislation |
| Differential Exposures | Unemployment | GOs and NGOs in the District such as Municipality |
| Differential Vulnerability | Lack of Knowledge and Skills to Deal with Stress | Training Positive Coping Mechanisms by Projects |
| Differential Health Outcome | Lack of Free Counseling Center in the Study Area | Ministry of Health and Medical Education |
| Differential Consequences | Lack of Facilities for Mental Health Rehabilitation | Social Welfare Organization |
Discussion
In this study, three main approaches have been used simultaneously (CBPR, ENHR and Analytical framework of WHO) to design the interventions of public health condition. In the CBPR approach, community participation can improve the positive health behaviors, human resource mobilization, community empowerment and finally mental health promotion (24). ENHR model is a bottom up approach that set the priorities based on stakeholders’ opinion (6), and then determines the stage of the intervention based on the analytical framework of WHO.
In our study, stakeholders’ analysis was essential to start the project. In this analysis, the role and function of each stakeholder is important, and not the personal identity (25). In our society, with rapid changes in the political positions, the sustainability of the stakeholders was not enough and this was one of the limitations of our project.
Interventions that address the socioeconomic context are at the national level. Providing insurance coverage for unattended families is one of the policies in this level. According to the result of this project, secure employment is important in differential exposure level, but at the vulnerability level, training the positive coping mechanism has been considered. In 2009, the result of the study of the regional office for the Eastern Mediterranean of WHO showed that in this region, the interventions related to the above levels, consist of reducing risk behaviors such as tobacco use, unsafe sex, improving access to basic health care and reducing social problems such as school drop-outs and domestic violence(26). It seems that the first priorities in our study are not completely compatible with this study. In Iran, during the recent years, access to basic health care has been facilitated, but the development of free counseling centers and providing coping mechanisms trainings are necessary. Considering the differential consequences, the majority of the interventions cannot evaluate these consequences, because they are frequently distal to the intervention. Furthermore, given the multiple, interacting nature of the social determinants, it may be difficult to identify which aspect of the intervention “caused” the mental health outcome (26). Also, it is necessary to recognize that mental health as a determinant can help explain outcomes for individuals and communities (1), and as an outcome it has multi-factorial etiologies consisting of genetic, biological, psychological and social determinants, with social determinants having particular salience (27). For sustainability of all the interventions targeting social determinants, existing political will, strong community partnerships, availability of financial and human resources are broad requirements (28).
Conclusions
Improving the coping skills to deal with stress is one of the most important interventions for mental health promotion in women.
Figure 2. Public Health Conditions Analytical Framework of WHO.
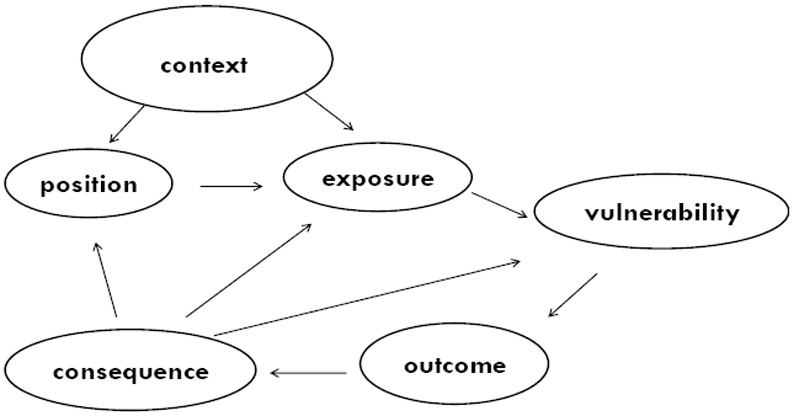
Table 2.
The Demographic Characteristics of the Participants in FGD
| Demographic Characteristic | Status | |||
|---|---|---|---|---|
| Age | Max :59 | Min:23 | Mean:24.6 | SD:10.5 |
| Education | Non Academic Education :30% | Academic Education :70% | ||
| Employment status | Employed :30% | Unemployed:70% | ||
| Number of Children | Max:5 | Min: 0 | ||
| Number of Participants | 30 | |||
Acknowledgments
The authors wish to thank all the volunteers in district 22 of Tehran for assistance in data collection and cooperation.
This project was extracted from a PhD thesis supported by National Health Research Institute.
References
- 1.Friedli L. Mental health, resilience and inequalities. Denmark: WHO Regional Office for Europe Copenhagen; 2009. [Google Scholar]
- 2.Zaveleta R. Working Paper 3. Oxford: University of Oxford; 2007. The ability to go about without shame: a proposal for internationally comparable indicators of shame and humiliation. ( http://www.ophi.org.uk/pubs/Zavaleta_Shame_Humiliation_Final.pdf) [Google Scholar]
- 3.Hughes JR. Nicotine dependence and WHO mental health surveys. JAMA. 2004;292:1021–1022. doi: 10.1001/jama.292.9.1021-c. author reply 1022. [DOI] [PubMed] [Google Scholar]
- 4.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 1998;33:587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 5.Asadi Lari M, Vaez-Mahdavi M. Overviews on Urban-Heart Tehran experience. World Health Organization; 2008. [Google Scholar]
- 6.Owlia P, Baradaran Eftekhari M, Setareh Forouzan A, Bahreini F, Farahani M, Ghanei M. Health research priority setting in Iran: Introduction to a bottom up approach. J Res Med Sci. 2011;16:691–698. [PMC free article] [PubMed] [Google Scholar]
- 7.Solar O, Irwin A. A conceptual framework for action on the social determinants of health. World Health Organization; 2007. [Google Scholar]
- 8.Bhugra D, Mastrogianni A. Globalisation and mental disorders. Overview with relation to depression. Br J Psychiatry. 2004;184:10–20. doi: 10.1192/bjp.184.1.10. [DOI] [PubMed] [Google Scholar]
- 9.Patel V, Kirkwood BR, Pednekar S, Pereira B, Barros P, Fernandes J, et al. Gender disadvantage and reproductive health risk factors for common mental disorders in women: a community survey in India. Arch Gen Psychiatry. 2006;63:404–413. doi: 10.1001/archpsyc.63.4.404. [DOI] [PubMed] [Google Scholar]
- 10.Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166:182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- 11.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 12.Patel V, Swartz L, Cohen A. The evidence for mental health promotion in developing countries. Promoting Mental Health. World Health Organization; 2005. [Google Scholar]
- 13.Hu TW. Perspectives: an international review of the national cost estimates of mental illness, 1990-2003. J Ment Health Policy Econ. 2006;9:3–13. [PubMed] [Google Scholar]
- 14.Saraceno B. The WHO World Health Report 2001 on mental health. Epidemiol Psichiatr Soc. 2002;11:83–87. doi: 10.1017/s1121189x00005546. [DOI] [PubMed] [Google Scholar]
- 15.Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, et al. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370:991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- 16.Djalalinia S, Tehrani FR, Afzali HM, Peykari N, Eftekhari MB. Community mobilization for youth health promotion: a lesson learned from iran. Iran J Public Health. 2012;41:55–62. [PMC free article] [PubMed] [Google Scholar]
- 17.Moshki M, Atarodi BA, Moslem A, Taheri M. Applying an Educational-participatory Program based on the PRECEDE Model for Promoting Self-esteem and Mental Health of Students in Iran. Int J Prev Med. 2012;3:241–248. [PMC free article] [PubMed] [Google Scholar]
- 18.Richardson EA, Moon G, Pearce J, Shortt NK, Mitchell R. Oral Presentations - Wednesday 10 September 2014 - Poster Session A: PP21 Mortality change over time in European cities: a population-based longitudinal study of 80 million people. J Epidemiol Community Health. 2014;68(Suppl 1):A55. doi: 10.1136/jech-2014-204726.117. [DOI] [Google Scholar]
- 19.Noorbala AA, Mohammad K, Bagheri Yazdi SA. The Validation of General Health Questionnaire- 28 as a Psychiatric Screening Tool (Persian) Hakim Magazine. 1999;5:101–110. [Google Scholar]
- 20.Delbecq AL, Van de Ven AH. A group process model for problem identification and program planning. The Journal of Applied Behavioral Science. 1971;7:466–492. [Google Scholar]
- 21.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 22.Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322:1115–1117. doi: 10.1136/bmj.322.7294.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rolfe G. Validity, trustworthiness and rigour: quality and the idea of qualitative research. J Adv Nurs. 2006;53:304–310. doi: 10.1111/j.1365-2648.2006.03727.x. [DOI] [PubMed] [Google Scholar]
- 24.Jacobs B, Price N. Community participation in externally funded health projects: lessons from Cambodia. Health Policy Plan. 2003;18:399–410. doi: 10.1093/heapol/czg048. [DOI] [PubMed] [Google Scholar]
- 25.Mulyaningrum M, Kartodihardjo H, Jaya INS, Nugroho B. Stakeholders Analysis of Policy-Making Process: The Case of Timber Legality Policy on Private Forest. Jurnal Manajemen Hutan Tropika (Journal of Tropical Forest Management) 2013;19:156–162. [Google Scholar]
- 26.Sheikh MR, Ali SZ, Hussain A, Shehzadi R, Afzal MM. Measurement of social capital as an indicator of community-based initiatives (CBI) in the Islamic Republic of Iran. J Health Organ Manag. 2009;23:429–441. doi: 10.1108/14777260910979317. [DOI] [PubMed] [Google Scholar]
- 27.Blas E, Kurup AS. Equity, social determinants and public health programmes. World Health Organization; 2010. [Google Scholar]
- 28.Friedli L. Mental health, resilience and inequalities. Copenhagen, Denmark: WHO Regional Office for Europe; 2009. [Google Scholar]


