Abstract
Aim:
The purpose of this article is to compare the similarity of initial radiological diagnosis and pathological diagnosis between thoracal and lumbar vertebral bodies and the adequacy and the reliability of open and percutaneous biopsies performed via transpedicular approach in the lesions located in vertebral bodies.
Materials and Methods:
Thirty-three patients who had undergone transpedicular biopsy for vertebral body lesions were retrospectively evaluated. Seventeen patients were diagnosed by percutaneous transpedicular biopsy (11 in the lumbar vertebrae, 6 in the thoracal vertebrae). Sixteen patients were diagnosed by open transpedicular biopsy (9 in the lumbar vertebrae, 7 in the thoracal vertebrae).
Results:
The similarity ratio between the initial radiological diagnosis and the final pathological diagnosis was 71.4% in the open biopsy and was 69.2% in the percutaneous biopsy (P > 0.05). The similarity ratio between the initial radiological diagnosis and the final pathological diagnosis was 66.7% in the lumbar region and was 77.8% in the thoracal region (P > 0.05). For percutaneous biopsy group, the similarity ratio was 72.7% in the lumbar region and was 66.7% in the thoracal region (P > 0.05). For open biopsy group, the similarity ratio was 62.5% in the lumbar region and 83.3% in the thoracal region (P > 0.05). No complication was observed.
Conclusion:
Specimen adequacy of open biopsy was higher than percutaneous biopsy. Particularly, the open thoracal biopsy has provided the highest similarity ratio between the initial radiological diagnosis and the final pathological diagnosis.
Keywords: Open biopsy, percutaneous biopsy, transpedicular biopsy, vertebral body
INTRODUCTION
It has long been believed that a needle biopsy of a musculoskeletal neoplasm does not provide adequate tissue for a definitive diagnosis. This belief is based on the agreement among the pathologists that mesenchymal tumors are among the most difficult pathologies to accurately diagnose. Open biopsy has an advantage when the amount of tissue retrieved for histopathology needs to be larger. However, open biopsy has a certain disadvantage of higher morbidity. [1] Percutaneous needle biopsy is safe and recommended in the diagnosis of musculoskeletal masses. [2] Despite increasing knowledge of spinal morphometry and experience with transpedicular fixation, the percutaneous biopsy has not been popularized as a method for percutaneous vertebral biopsy. [3]
The first open transpedicular approach to vertebral corpus was made by Duncan and Ferguson [4] in 1928. Robertson and Ball [5] performed the first percutaneous biopsy of the spine in 1935. Finally, Stringham et al., [6] presented the first percutaneous transpedicular vertebral biopsy in 1994. Pedicle can be used for a minimally invasive access to the vertebral corpus without damaging the adjacent vital structures. Stringham et al., [6] have also emphasized on the importance of maintaining the integrity of the medial and inferior aspects of the pedicle because of the anatomic relationship to the neural elements.
The purpose of this article is to compare the adequacy and the reliability of open and percutaneous biopsies performed via transpedicular approach from spinal lesions located in the vertebral body and also to compare the similarity between initial radiological diagnosis and pathological diagnosis between thoracal and lumbar vertebral bodies.
MATERIALS AND METHODS
Thirty-three patients who had undergone transpedicular biopsy for the lesions located in the vertebral body were retrospectively evaluated. Seventeen patients were diagnosed by percutaneous transpedicular biopsy using an 11G jamshidi trocar (11 in the lumbar vertebrae, 6 in the thoracal vertebrae) [Table 1]. Sixteen patients were diagnosed by open transpedicular biopsy (9 in the lumbar vertebrae, 7 in the thoracal vertebrae) [Table 1]. Percutaneous transpedicular biopsies were performed under sedation and local anesthesia with C-arm fluoroscopy guidance [Figure 1]. Open biopsies were taken under general anesthesia with C-arm fluoroscopy guidance after making a 4-5 cm skin incision in order to introduce a curette through pedicle to the corpus. The initial diagnosis of the lesions was made by an orthopedic surgeon and an expert radiologist before the biopsy procedure. Biopsy specimens were evaluated by an expert pathologist. In the end, the initial diagnoses and the histopathological diagnoses were compared. The obtained data were analyzed and statistically recorded in SPSS version 15.0. Data were evaluated by descriptive statistical methods (rate, mean, standard deviation) as well as quantitative parameters showing normal distribution of data for comparison with the Student t-test; abnormal distribution parameters were evaluated by the Mann-Whitney U test. Chi-square test for the comparison of qualitative data was used. Results were at 95% confidence intervals and P < 0.05 was evaluated.
Table 1.
Demographic data, biopsy level, radiologic and histopathologic diagnoses of patients
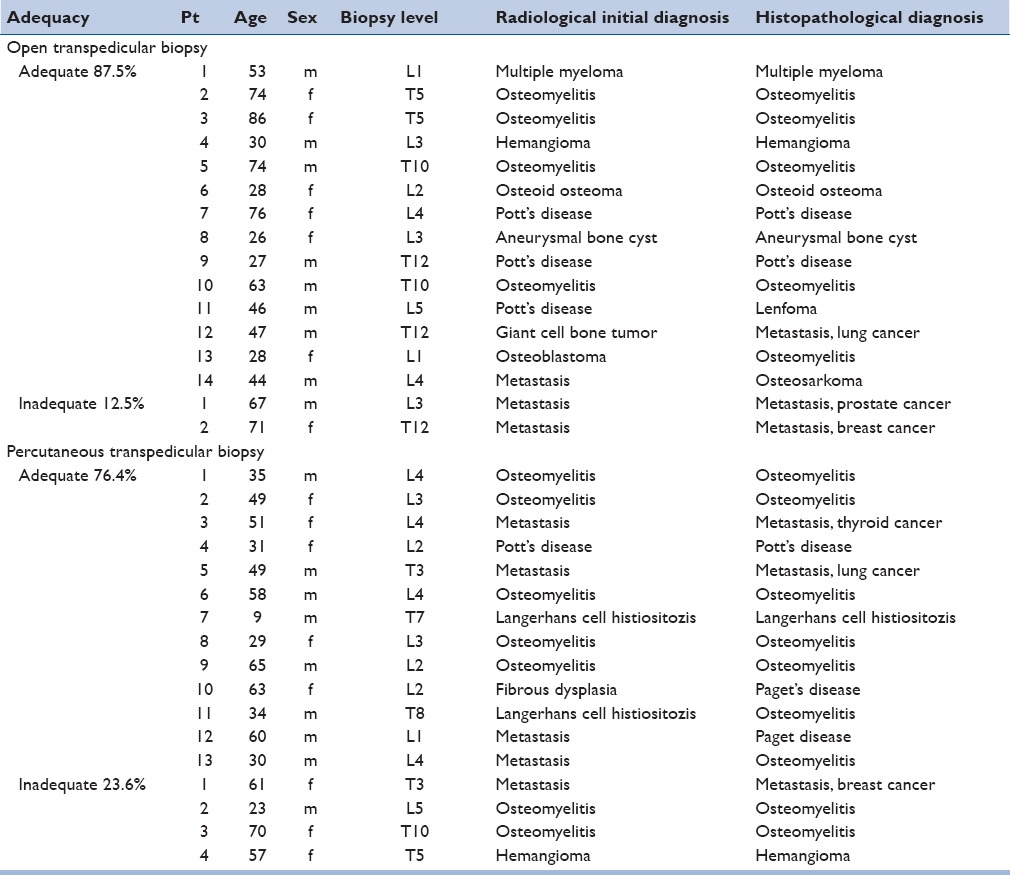
Figure 1.
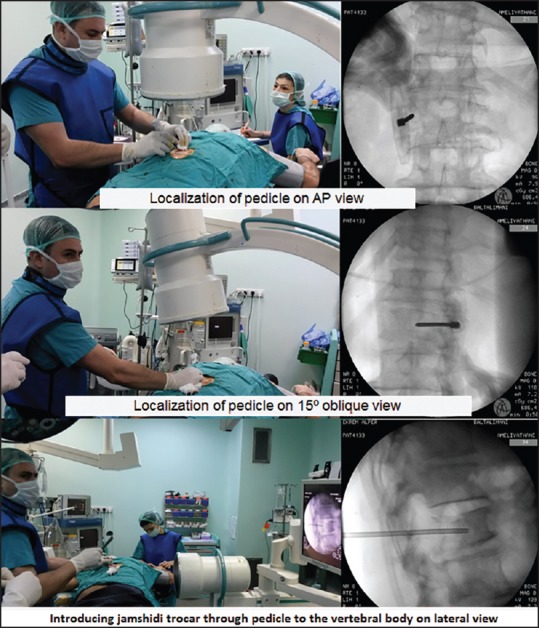
C-arm fluoroscopy-assisted percutaneous technique
RESULTS
After histopathological evaluation, 13 of the 17 percutaneous biopsies’ (76.5%) and 14 of the 16 open biopsies’ (87.5%) specimens were adequate for diagnosis (P > 0.05). Six patients had undergone second open biopsy because of inadequate specimen biopsies. Three of the 13 adequate percutaneous biopsy specimens were taken from the thoracal spine and 10 from the lumbar spine. Six of the 14 adequate open biopsy specimens were taken from the thoracal spine and 8 from the lumbar spine. The histopathological diagnosis and the initial diagnosis of the percutaneous biopsy patients were the same for 66.7% in the thoracal spine and 72.7% in the lumbar spine (P > 0.05). The histopathological diagnosis and the initial diagnosis of the open biopsy patients were the same for 83.3% in the thoracal spine and 62.5% in the lumbar spine (P > 0.05). No complication was observed in both groups.
DISCUSSION
The accuracy of percutaneous spine biopsy is reported to range between 16% and 92%, and the complication rates are reported to range between 0% and 10%. [3] The accuracy of percutaneous spine biopsy performed under fluoroscopy guidance was reported as 93.8% by Kamei et al., [7] in a series of 128 cases. In this report, the accuracy for primer neoplasms was reported as 78.6% and 97% for metastatic neoplasms.
The adequacy of percutaneous spine biopsy performed under fluoroscopy guidance was reported as 88.7% by Dave et al., [8] and as 87% under CT guidance by Kornblum et al., [9] Kornblum et al., [9] also reported that lumbar percutaneous biopsies were more accurate than thoracic percutaneous biopsies. The meta-analysis of Nourbakhsh et al., [10] showed that there is no difference in terms of accuracy or adequacy between the percutaneous transpedicular biopsies performed under CT or fluoroscopy guidance.
The reports of CT-guided vertebral body biopsies have indicated that its reliability is 94% for osteolytic lesions and 75% for sclerotic lesions. [11] For sclerotic lesions, Ghelman et al., [12] recommended the use of trocar instruments rather than spinal needles. The disparity between the accuracy, the adequacy and the complication results could be attributed to the differences in diameter size of the biopsy needles used. Thus, in a cadaver study Fyfe et al., [13] showed that an increase of the diameter of the biopsy needle by 2 mm increased the diagnostic value of the specimen from 59% to 90%. But the complication rate increases as the diameter of the biopsy needle increases. In our study, the adequacy of percutaneous transpendicular biopsy was found to be 76.4% and was found to be 87.5% for open transpedicular biopsy (P > 0.05).
Percutaneous transpedicular biopsy has the disadvantage of having complications like bleeding, pneumothorax, nerve injury, and very rarely transient paresis, transient spinal analgesia, radiculopathy, paraplegia, meningitis and death. [14,15] No complication was observed in both groups but this may be due to the small number of patients in our study. Comparative prospective studies with more cases are needed to determine more definitive complication rates.
In contrast to the studies in the literature, Fidler and Niers [16] stated that an open transpedicular approach has certain advantages over a percutaneous procedure in enabling the surgeon to perform block resection, and avoiding any damage to the pedicle wall, thus minimizing the possibility of contaminating the epidural space or paravertebral structures.
The accuracy of percutaneous biopsy has increased with the development of new techniques and imaging modalities. In appropriate cases, percutaneous transpedicular biopsy can be applied easily and quickly with local anesthesia and sedation. Open thoracal biopsy specimens have yielded the highest similarity ratio between the radiological initial diagnosis and the final pathological diagnosis and have been followed by percutaneous lumbar biopsy.
In our study, the adequacy of the specimen for determining a final diagnosis was higher in open biopsy than in percutaneous transpedicular biopsy (P > 0.05). Also the adequacy was higher in the lumbar spine than in the thoracal spine in percutaneous transpedicular biopsy (P > 0.05). The limited number of patients is the most important limitation of our study. Comparative prospective studies with more cases are needed to determine the reliability and the adequacy of open and percutaneous transpedicular biopsy in the thoracolumbar spine.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am. 1996;78:656–63. doi: 10.2106/00004623-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Welker JA, Henshaw RM, Jelinek J, Shmookler BM, Malawer MM. The percutaneous needle biopsy is safe and recommended in the diagnosis of musculoskeletal masses. Cancer. 2000;89:2677–86. doi: 10.1002/1097-0142(20001215)89:12<2677::aid-cncr22>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 3.Metzger CS, Johnson DW, Donaldson WF., 3rd Percutaneous biopsy in the anterior thoracic spine. Spine (Phila Pa 1976) 1993;18:374–8. doi: 10.1097/00007632-199303000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Duncan GA, Ferguson AB. Benign giant cell tumor of the fourth lumbar vertebra: A case report. J Bone Joint Surg Am. 1936;3:769–72. [Google Scholar]
- 5.Robertson RC, Ball RP. Destructive spinal lesions: Diagnosis by needle biopsy. J Bone Joint Surg. 1935;17:749–58. [Google Scholar]
- 6.Stringham DR, Hadjipavlou A, Dzioba RB, Lander P. Percutaneous transpedicular biopsy of the spine. Spine (Phila Pa 1976) 1994;19:1985–91. doi: 10.1097/00007632-199409000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Kamei Y, Nishida J, Mimata Y, Shiraishi H, Ehara S, Satoh T, et al. Core needle percutaneous transpedicular vertebral body biopsy: A study of 128 cases. J Spinal Disord Tech. 2013 doi: 10.1097/BSD.0b013e31829c077a. [DOI] [PubMed] [Google Scholar]
- 8.Dave BR, Nanda A, Anandjiwala JV. Transpedicular percutaneous biopsy of the vertebral lesions: A series of 71 cases. Spinal Cord. 2009;47:384–9. doi: 10.1038/sc.2008.108. [DOI] [PubMed] [Google Scholar]
- 9.Kornblum MB, Wesolowski DP, Fischgrund JS, Herkowitz HN. Computed tomography-guided biopsy of the spine. A review of 103 patients. Spine (Phila Pa 1976) 1998;23:81–5. doi: 10.1097/00007632-199801010-00018. [DOI] [PubMed] [Google Scholar]
- 10.Nourbakhsh A, Grady JJ, Garges KJ. Percutaneous spine biopsy: A meta-analysis. J Bone Joint Surg Am. 2008;90:1722–5. doi: 10.2106/JBJS.G.00646. [DOI] [PubMed] [Google Scholar]
- 11.Brugieres P, Revel MP, Dumas JL, Heran F, Voisin MC, Gaston A. CT-guided vertebral biopsy: A report of 89 cases. J Neuroradiol. 1991;18:351–9. [PubMed] [Google Scholar]
- 12.Ghelman B, Lospinuso MF, Levine DB, O’Leary PF, Burke SW. Percutaneous computed-tomography-guided biopsy of the thoracic and lumbar spine. Spine (Phila Pa 1976) 1991;16:736–9. doi: 10.1097/00007632-199107000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Fyfe IS, Henry AP, Mulholland RC. Closed vertebral biopsy. J Bone Joint Surg Br. 1983;65:140–3. doi: 10.1302/0301-620X.65B2.6826616. [DOI] [PubMed] [Google Scholar]
- 14.Kattapuram SV, Khurana JS, Rosenthal DI. Percutaneous needle biopsy of the spine. Spine (Phila Pa 1976) 1992;17:561–4. doi: 10.1097/00007632-199205000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Murphy WA, Destouet JD, Gilula LA. Percutaneous skeletal biopsy 1981: A procedure for radiologists — results, review, and recommendations. Radiology. 1981;139:545–9. doi: 10.1148/radiology.139.3.7232719. [DOI] [PubMed] [Google Scholar]
- 16.Fidler MW, Niers BB. Open transpedicular biopsy of the vertebral body. J Bone Joint Surg Br. 1990;72:884–5. doi: 10.1302/0301-620X.72B5.2211776. [DOI] [PubMed] [Google Scholar]


