Abstract
Spontaneous regression of hepatocellular carcinoma (HCC) is a rare phenomenon. We followed a detailed clinical course of a spontaneous and complete disappearance of HCC during a short interval. A 73-year-old man with hepatitis B virus infection presented with a 15-mm mass in the right anterior superior segment of the liver. The mass was diagnosed as HCC by imaging findings. We found an elevated serum α-fetoprotein (AFP) level of 748 ng/ml. The tumor regressed to 6 mm on imaging examination, and the AFP serum level decreased to 87.8 ng/ml 1 month after the diagnostic hepatic angiography. Therefore, the patient was followed up without any treatment for HCC. The tumor disappeared 5 months later when the AFP serum level was 5.0 ng/ml. The diagnostic hepatic angiography might have had some effect on the spontaneous regression of HCC in the present case.
Key Words: Spontaneous regression, Hepatocellular carcinoma, Imaging course, Complete disappearance, Hepatic angiography, Ischemia
Introduction
Spontaneous regression (SR) of a malignancy has been defined as a partial or complete disappearance of malignancy without receiving any specific treatment [1]. It is a very rare phenomenon, with a frequency of occurrence estimated between 1/60,000 and 1/100,000 malignancy cases [2]. SR has been reported in a variety of malignancies, including renal cell carcinoma, malignant melanoma, neuroblastoma, malignant lymphoma, leukemia, and retinoblastoma.
SR of hepatocellular carcinoma (HCC) is also rare; in particular, complete disappearance is an extraordinarily unusual phenomenon. The previous case reports of SR of HCC did not show a detailed imaging course during a short interval. Several mechanisms of SR of HCC have been discussed; however, the precise cause remains unknown. We report a clinical course of a spontaneous and complete disappearance of HCC and discuss its possible causes.
Case Report
A 73-year-old man with hepatitis B virus (HBV) infection came to our hospital for the workup of his hepatic mass incidentally found by abdominal CT. His mother was also a HBV carrier. He had been drinking regularly, consuming 25 g of alcohol daily for 50 years and had also smoked 10 cigarettes per day for 50 years. He did not consume any drugs.
Laboratory examinations showed a Hb of 14.3 g/dl, platelets of 135,000/mm3 and a WBC count of 6,000/mm3. Blood chemistry tests revealed aspartate aminotransferase of 26 IU/l, alanine aminotransferase of 17 IU/l, γ-glutamyl transpeptidase of 14 IU/l, alkaline phosphatase of 250 IU/l, albumin of 4.3 g/dl, globulin of 3.2 g/dl, total bilirubin of 0.9 mg/dl, prothrombin time of 100.5%, and glucose of 112 mg/dl. Serum HBs antigen was positive, HBs antibody negative, HBe antigen negative, HBe antibody and HBc antibody were positive. The HBV DNA value was 2.7 log copies/ml. The serum hepatitis C virus antibody was negative. The serum level of α-fetoprotein (AFP) was 748 ng/ml (normal <10 ng/ml) and protein induced by vitamin K absence II was 20 mAU/ml (normal <40 mAU/ml). The indocyanine green elimination test showed that the K value was 0.158 (normal 0.168–0.232) and the retention rate at 15 min was 8.4% (normal <10%).
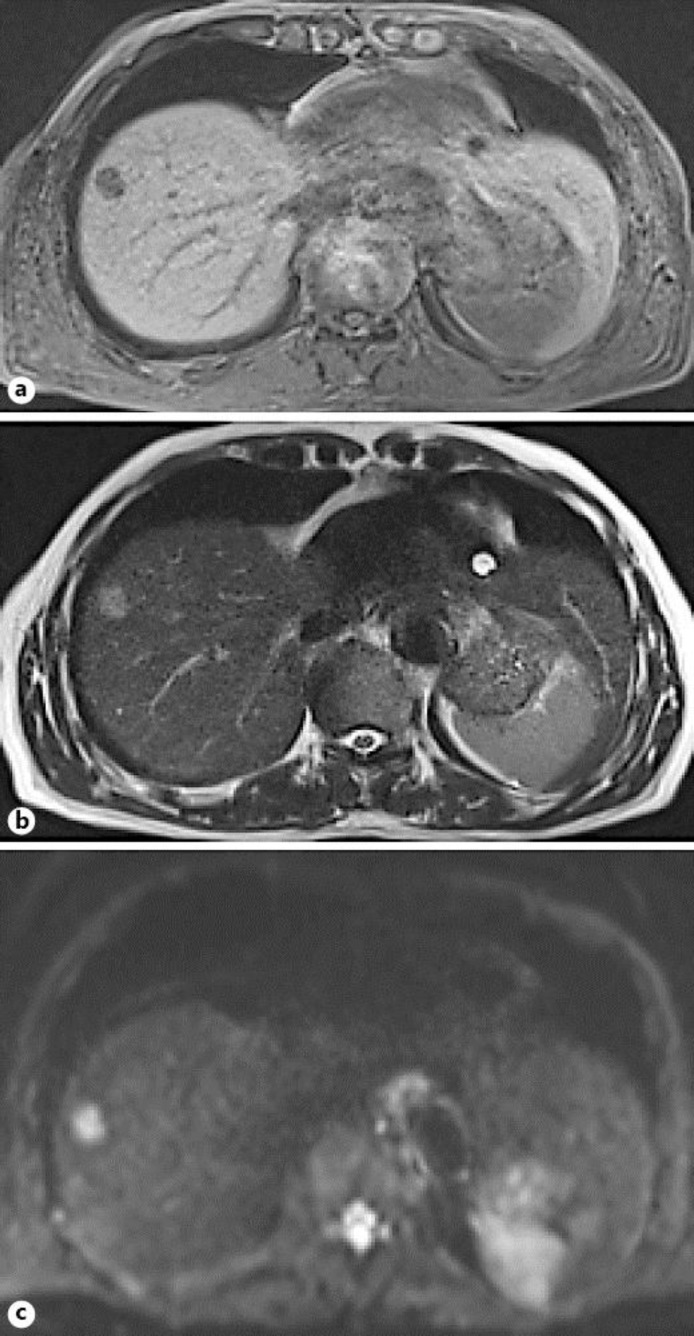
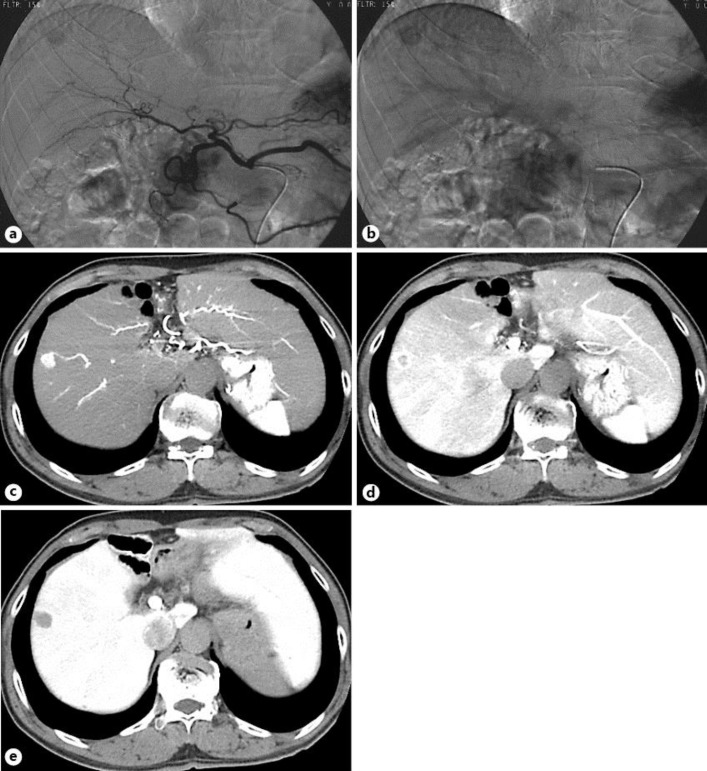
Abdominal ultrasonography demonstrated a hypoechoic mass of 15 mm in diameter in the right anterior superior segment of the liver [Couinaud's segment 8 (S8)]. MRI disclosed a 15-mm low-signal intensity mass in T1-weighted image (fig. 1a), a high-signal intensity mass in T2-weighted image (fig. 1b), and a very high-signal intensity mass in the diffusion-weighted image (fig. 1c) in the liver (S8). Hepatic angiography disclosed a tumor stain in the arterial (fig. 2a) and late phase (fig. 2b) in the same area. The mass in the liver (S8) was described as an enhanced lesion on CT during hepatic arteriography (fig. 2c, d) and as a low-density lesion on CT during arterial portography (fig. 2e). We diagnosed this case as HCC stage I (T1N0M0) according to the TNM classification of the Liver Cancer Study Group of Japan based on the above imaging findings and the high AFP serum value.
Fig. 1.
MRI disclosed a 15-mm mass in the liver (S8) with a low-signal intensity in T1-weighted image (inphase) (a), a high-signal intensity in T2-weighted image (b), and a strong high-signal intensity in the diffusion-weighted image (c).
Fig. 2.
Hepatic angiography in the early phase (a) and late phase (b) revealed a tumor stain in the anterior superior arteries. The mass in the liver (S8) was described as an enhanced lesion on CT during hepatic arteriography (c), a corona-like enhanced lesion on CT in the portal-venous phase (d), and a low-density lesion on CT during arterial portography (e).
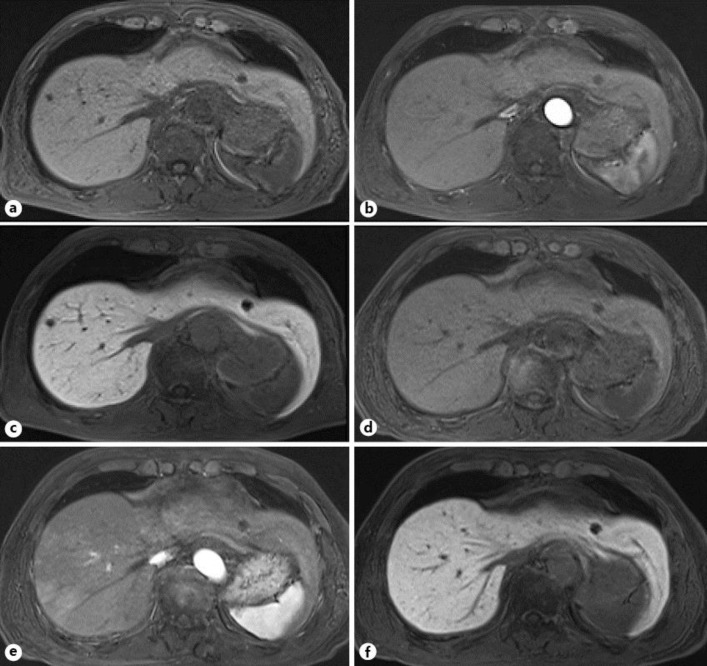
We planned an anterior lobectomy of the liver. However, 1 month after the initial diagnosis, a plain MRI disclosed a regression of the tumor to 6 mm, and the AFP serum level decreased to 87.8 ng/ml. Therefore, we cancelled the surgical treatment and followed up the patient. Two months after the initial diagnosis, follow-up gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced MRI showed a 6-mm low-signal intensity mass in T1-weighted image (fig. 3a), no mass in the arterial phase (fig. 3b), and a low-signal intensity mass in the hepatobiliary phase (fig. 3c). A dynamic CT also showed the same behaviors. The AFP serum level was 71.8 ng/ml at that time. The patient had not taken any herbal medicine nor consumed any drugs. He had stopped alcohol consumption and smoking after the HCC diagnosis.
Fig. 3.
MRI revealed a 6-mm low-signal intensity mass in the liver (S8) in T1-weighted image (a) 2 months after the initial diagnosis. The gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced MRI disclosed no mass in the arterial phase (b) and a 6-mm low-signal intensity mass in the hepatobiliary phase (c). MRI showed no mass in the liver (S8) in the pre-enhanced phase of T1-weighted image (d), arterial phase (e), and hepatobiliary phase (f) 6 months after the initial diagnosis.
He was followed up without any treatment for HCC. Six months after the initial diagnosis, follow-up ethoxybenzyl MRI showed no mass in the liver (S8) (fig. 3d–f), and the AFP serum level decreased to a normal range (5.0 ng/ml). To our regret, the tumor regression was not confirmed histologically. The patient has been followed up at our outpatient clinic without any signs of recurrence for 5 years.
Discussion
Here we report an unusual case of HCC with a clinical course of spontaneous and complete disappearance. The present case is unique because we were able to follow its detailed imaging course during a short interval.
SR of HCC in previous reports has been reported in various patients. The possibility of SR may not be associated with the size of the mass, the number of the mass, the level of tumor markers, background liver disease, and with the presence or absence of distal metastases [3]. The characteristics of HCC in the present case were the smallness (15 mm), singleness, the high serum level of AFP (748 ng/ml), and the association with HBV infection. The tumor size was minimal compared to the previous SR cases.
The exact mechanism leading to SR of HCC remains obscure. Several causes of SR have been suggested in the previous literature [4]. First, ischemia might be a main cause of SR, because malignant tissue is more sensitive to ischemic change than normal tissue. Because of the hypervascular character of HCC, an important factor might be an insufficient blood supply to the tumor, possibly due to injuries of the feeding arteries associated with angiography and arterial thrombosis [5, 6], portal vein tumor thrombus [7], and the deprivation of oxygen due to rapid tumor growth [8] as well as gastrointestinal bleeding [9].
The mechanism of SR in the present case is unclear; however, ischemia may be a main cause because of a clinical course of the imaging examinations, possibly due to a loss of the feeding arterial blood supply (fig. 2, 3b). The present patient had not had the above episodes except for receiving angiography. The procedure of selective catheterization may have had some effects in the present case; however, there was no evidence of subintimal injury (fig. 2a, b) [5]. It is difficult to prove the local effect of blood deficiency (A8) in the present patient.
Second, immunological reactions might cause SR of HCC. Abstinence from alcohol or smoking [10, 11], operation with blood transfusion [12], the use of some herbal medicine [13], withdrawal or reduction of androgen [14] and secondary bacterial infection in the tumor [15] may produce cytokines such as tumor necrosis factors (TNF), and TNF may play an important role in anti-tumor activities. The present patient had not received any medication (including herbal medicine) and had not had the above episodes except for his changes in lifestyle (stoppage of alcohol consumption and smoking) during this period. The change of lifestyle might be one of the causes of SR, but it might not be the main cause.
The limitation of the present case study is that this case was not proven histologically. However, the findings of imaging examinations (fig. 1, fig. 2) and the elevation of serum AFP level supported the diagnosis of HCC. In previous reports of SR of HCC, most tumors were diagnosed by imaging techniques and tumor marker levels, and occasionally by histological examinations.
We presented a rare case of HCC with a clinical course of spontaneous and complete disappearance. After all, although the precise mechanism of SR remains unclear in the present case, the diagnostic hepatic angiography might have played an important role in this phenomenon. The accumulation for this kind of special case will contribute to the understanding of this phenomenon and give us the possibility to improve a future strategy for the treatment of HCC.
Disclosure Statement
The authors declare that there are no conflicts of interest.
References
- 1.Cole WH, Everson TC. Spontaneous regression of cancer: preliminary report. Ann Surg. 1956;144:366–383. doi: 10.1097/00000658-195609000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cole WH. Efforts to explain spontaneous regression of cancer. J Surg Oncol. 1981;17:201–209. doi: 10.1002/jso.2930170302. [DOI] [PubMed] [Google Scholar]
- 3.Oquinena S, Inarrairaegui M, Vila JJ, Alegre F, Zozaya JM, Sangro B. Spontaneous regression of hepatocellular carcinoma: three case reports and a categorized review of the literature. Dig Dis Sci. 2009;54:1147–1153. doi: 10.1007/s10620-008-0447-z. [DOI] [PubMed] [Google Scholar]
- 4.Oquinena S, Guillen-Grima F, Inarrairaegui M, Zozaya JM, Sangro B. Spontaneous regression of hepatocellular carcinoma: a systematic review. Eur J Gastroenterol Hepatol. 2009;21:254–257. doi: 10.1097/MEG.0b013e328324b6a2. [DOI] [PubMed] [Google Scholar]
- 5.Takayasu K, Muramatsu Y, Shima Y, Moriyama N, Yamada T, Yoshida T, et al. Necrosis of hepatocellular carcinoma as a result of subintimal injury incurred by hepatic angiography: report of two cases. Am J Gastroenterol. 1986;81:979–983. [PubMed] [Google Scholar]
- 6.Okano A, Ohana M, Kusumi F, Nabeshima M. Spontaneous regression of hepatocellular carcinoma due to disruption of the feeding artery. Case Rep Oncol. 2013;6:180–185. doi: 10.1159/000350682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uenishi T, Hirohashi K, Tanaka H, Ikebe T, Kinoshita H. Spontaneous regression of a large hepatocellular carcinoma with portal vein tumor thrombi: report of a case. Surg Today. 2000;30:82–85. doi: 10.1007/PL00010054. [DOI] [PubMed] [Google Scholar]
- 8.Iwasaki M, Furuse J, Yoshino M, Moriyama N, Kanemoto H, Okumura H. Spontaneous regression of hepatocellular carcinoma: a case report. Jpn J Clin Oncol. 1997;27:278–281. doi: 10.1093/jjco/27.4.278. [DOI] [PubMed] [Google Scholar]
- 9.Tocci G, Conte A, Guarascio P, Visco G. Spontaneous regression of a hepatocellular carcinoma after massive gastrointestinal hemorrhage. BMJ. 1990;300:641–642. doi: 10.1136/bmj.300.6725.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gottfried EB, Steller R, Paronetto F, Lieber CS. Spontaneous regression of hepatocellular carcinoma. Gastroenterology. 1982;82:770–774. [PubMed] [Google Scholar]
- 11.Grossmann M, Hoermann R, Weiss M, Jauch KW, Oertel H, Staebler A, et al. Spontaneous regression of hepatocellular carcinoma. Am J Gastroenterol. 1995;90:1500–1503. [PubMed] [Google Scholar]
- 12.Sato Y, Fujiwara K, Nakagawa S, Kanishima S, Ohta Y, Oka Y, et al. A case of spontaneous regression of hepatocellular carcinoma with bone metastasis. Cancer. 1985;56:667–671. doi: 10.1002/1097-0142(19850801)56:3<667::aid-cncr2820560339>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 13.Chien RN, Chen TJ, Liaw YF. Spontaneous regression of hepatocellular carcinoma. Am J Gastroenterol. 1992;87:903–905. [PubMed] [Google Scholar]
- 14.Johnson FL, Lerner KG, Siegel M, Feagler JR, Majerus PW, Hartmann JR, et al. Association of androgenic-anabolic steroid therapy with development of hepatocellular carcinoma. Lancet. 1972;ii:1273–1276. doi: 10.1016/s0140-6736(72)92649-9. [DOI] [PubMed] [Google Scholar]
- 15.Watanabe N, Yamauchi N, Maeda M, Neda H, Tsuji Y, Okamoto T, et al. Recombinant human tumor necrosis factor causes regression in patients with advanced malignancies. Oncology. 1994;51:360–365. doi: 10.1159/000227366. [DOI] [PubMed] [Google Scholar]