Abstract
Despite being the most common entrapment neuropathy and the most common reason for referral to the electromyography (EMG) laboratory, the diagnosis of carpal tunnel syndrome (CTS) continues to be challenging due to a large number of electrodiagnostic (EDX) tests available. We present a flowchart and propose a practical approach to the diagnosis of CTS using the available literature and the American Association of Neuromuscular and Electrodiagnostic Medicine (AANEM) guidelines and the Practice Parameter for Electrodiagnostic Studies in Carpal Tunnel Syndrome.
Keywords: Carpal tunnel syndrome, electrodiagnosis, nerve entrapment
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy caused by compression of the median nerve at the wrist, and the most common reason for referral to the electromyography (EMG) laboratory. Many different electrodiagnostic (EDX) methods have been developed over the years for diagnosis of CTS. Electromyographers are often unclear about the selection of the most appropriate test from a long list of available choices. The objective of this review is to select the most validated electrodiagnostic tests for the diagnosis of CTS and classify them in a stepwise approach. We searched ‘Pubmed’ for all articles relevant to electrodiagnosis of CTS and reviewed American Association of Neuromuscular and Electrodiagnostic Medicine (AANEM) guidelines and Practice Parameter for Electrodiagnostic Studies in Carpal Tunnel Syndrome. Using the available literature, we present a flowchart and propose a practical approach to the diagnosis of CTS.
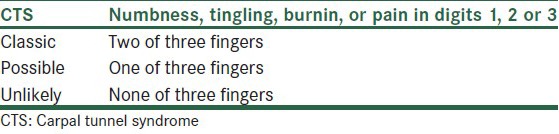
The median nerve, formed by contributions from the lateral (C6–C7 fibers) and medial cords (C8–T1 fibers), enters the wrist, along with nine finger flexor tendons, through the carpal tunnel. The floor and sides of the tunnel are composed of carpal bones, while the transverse carpal ligament forms its roof. CTS is more common in women, is most prevalent after 50 years of age, and usually involves the dominant hand first. The incidence of CTS has increased almost two-fold over the last two decades.[1] CTS remains a clinical syndrome with appropriate symptoms and signs, in the presence of EDX abnormalities. Episodic numbness, tingling, burning or pain in the affected hand, frequent awakening at night, due to hand paresthesias, and relief of symptoms by hand shaking are characteristic symptoms of CTS. Palm pain, wrist pain or radiation proximal to the wrist may occur. The most common site of sensory symptoms is in all digits, followed by median digits only or a glove distribution.[2] Absence of symptoms in the thumb, index, and middle fingers makes the diagnosis of CTS unlikely [Table 1].[3] Likelihood of the carpal tunnel syndrome is the greatest for classic symptoms in combination with positive electrodiagnostic study results. When there are no symptoms in the thumb, index, or middle fingers, the likelihood of carpal tunnel syndrome is judged to be low, regardless of the results of the EDX study.[3] Paresthesia in a median nerve distribution, after percussion of the median nerve at the wrist (Tinel's sign), and particularly, after passive flexion of the hand at the wrist (Phalen's sign)[4] can help in diagnosis, but they are not very sensitive and specific tests.
Table 1.
Classic, possible and unlikely CTS according to clinical symptoms (modified from Rempel, et al.)
Electrodiagnostic (EDX) studies are often necessary for confirmation of CTS diagnosis and exclusion of other possible causes of symptomatology, such as, cervical radiculopathy or peripheral polyneuropathy. In addition, nerve conduction studies could be used to predict the risk of development of CTS symptoms in asymptomatic patients[5] and also to predict the outcome of surgical decompression.[6] Many different EDX tests have been designed for CTS diagnosis and the EDX practitioner is faced with myriad different situations and uncertainties in the proper use of these tests in clinical practice.
Prolongation of the median motor distal latency (MDL) was first described in 1956 by Simpson[7] and later confirmed by Thomas[8] and Lambert.[9] At the same time, measurement of median sensory nerve conduction was introduced by Dawson, and median sensory slowing across the carpal tunnel was demonstrated in patients with CTS, by Gilliatt and Sears.[10] Prolongation of median palm-to-wrist sensory nerve latency was first described by Eklund,[11] and with slight modification, remains the preferred method for diagnosis of CTS in many laboratories.[12] The inching method, described by Kimura, consists of antidromic serial 1-cm stimulation of the median nerve across the carpal tunnel recording, from the index or middle fingers.[13,14] Comparison of the latencies of the median and ulnar nerves from the ring finger with antidromic[15,16] or orthodromic[17,18] stimulation is another sensitive method of diagnosis. Similarly comparison of the latencies of radial and median nerves from the thumb could be used in the diagnosis of CTS.[19] Finally, the median MDL recording from the second lumbrical is compared with the ulnar MDL recording from the second interossei.[20] Comparison of the orthodromic or antidromic sensory nerve conduction velocity (SNCV) in the median nerve between the third digit and palm and between the palm and wrist is another proposed method.[21] Other less confirmed methods include: The second lumbrical–interossei premotor potential,[22] the cutaneous silent period,[23] modified sensory ‘inching’ method,[24] comparison of sensory nerve conductions in the palmar cutaneous branch and digit I nerves,[25] combined sensory index,[26] terminal latency index,[27] median motor nerve conduction amplitude comparisons with stimulation above and below the carpal ligament,[28,29,30] measurement of the refractory period of the median nerve,[31,32] median motor residual latency measurement,[33,34] terminal latency ratio,[35] median F-wave abnormalities,[36] sensory amplitude measurements,[37] and measurement of the median sensory and motor nerve conduction across the wrist before and after prolonged wrist flexion.[38,39]
In an extensive literature review by the American Association of Neuromuscular And Electrodiagnostic Medicine (AANEM) Quality Assurance Committee, Jablecki et al. found that median MDL, median sensory NCS (between the wrist and digit, between the wrist and palm, inching method), comparison of median and ulnar mixed nerve sensory conduction between the wrist and palm, comparison of median sensory nerve conduction to the ulnar or radial sensory nerve conduction in the same limb, and EMG of the abductor pollicis brevis (APB) were the best documented EDX tests in the electrodiagnosis of CTS.[40] They found that absent or delayed peak sensory distal latencies (SDL) occur in 49 to 66% of the CTS patients, with 97.5 to 100% specificity and delayed motor distal latencies (MDL) occurring in 60 to 74% of the CTS patients with 95 to 99% specificity. The latter tests are the most popular EDX studies in the evaluation of CTS.
The AANEM Guidelines recommend median sensory or mixed nerve conduction study, median motor conduction study, needle examination of APB, ulnar or/and radial motor and sensory NCSs (in order to exclude a peripheral neuropathy), and needle electromyography of the limb muscles innervated by the C5toT1 roots (in order to exclude a cervical radiculopathy, brachial plexopathy, and a proximal median neuropathy) be performed, as part of the examination of patients suspected of CTS.[41]
The American Association of Neuromuscular and Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation report a practice parameter for electrodiagnostic studies in carpal tunnel syndrome that was published in two journals, Muscle, Nerve, and Neurology, simultaneously.[42,43]
This report recommends performing a median sensory NCS across the wrist, a motor NCS of the median nerve recording from the thenar muscle, and of one other nerve in the symptomatic limb, to include measurement of distal latency, and needle electromyography (EMG) of a sample of muscles innervated by the C5 to T1 spinal roots, including a thenar muscle innervated by the median nerve of the symptomatic limb. If the result of the median sensory and motor distal latencies are abnormal in comparison to the result of the sensory and motor distal latencies of one another adjacent nerve in the symptomatic limb, the diagnosis of CTS is confirmed, However, if the initial median sensory and motor distal latenciesacross the wrist are normal or equivocal, one of the following additional studies is recommended: Comparison of a median sensory or mixed nerve conduction across the wrist over a short (7 cm to 8 cm) conduction distance, with ulnar sensory nerve conduction across the wrist over the same short (7 cm to 8 cm) conduction distance, comparison of the median sensory conduction across the wrist with radial or ulnar sensory conduction across the wrist in the same limb, or comparison of the median sensory or mixed nerve conduction through the carpal tunnel to the sensory or mixed NCSs of the proximal (forearm) or distal (digit) segments of the median nerve in the same limb.
In supplementary NCS, as recommended by the report, a comparison of the median motor nerve distal latency (second lumbrical) to the ulnar motor nerve distal latency (second interossei), inching method, median motor terminal latency index, and median motor nerve conduction between the wrist and palm are the most sensitive and specific tests.
Considering the above data and literature, we have designed a flowchart and stepwise approach to the diagnosis of CTS [Figure 1]. To begin with, we must remember that CTS is a clinical diagnosis and performing EDX in patients with clinically unlikely manifestations of CTS is fruitless[Table 1].[3] There is strong evidence in favor of performing SDL and MDL as the first step in EDX of CTS (see above). If the results of both tests are abnormal, CTS is probable, but peripheral polyneuropathy could also be present with abnormal median SDL and MDL. Concomitant abnormality of the ulnar SDL and MDL is in favor of polyneuropathy. In this situation, the median-ulnar second lumbrical–interossei comparison study is the preferred method that could demonstrate the presence of CTS in polyneuropathy patients[20,44] [Figure 1].
Figure 1.
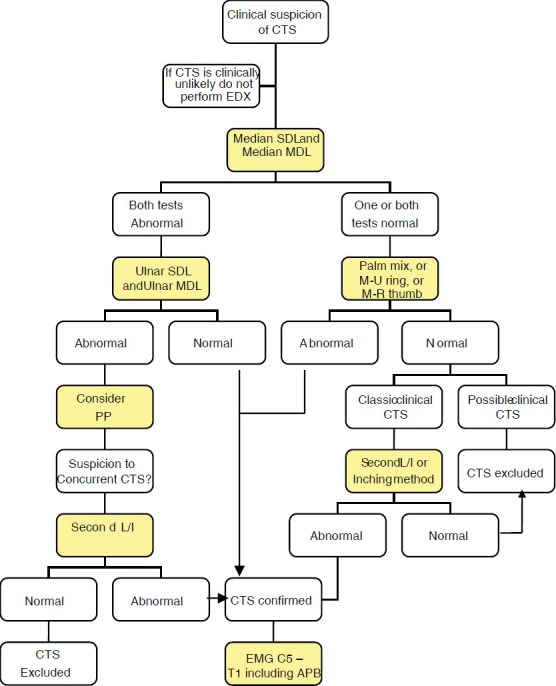
Practical approach to diagnosis of carpal tunnel syndrome (CTS) SDL = Sensory peak distal latency, MDL = Motor distal latency, PP = Peripheral polyneuropathy, Palm mix = Median-ulnar palmar mixed study, Second L/I = Median-ulnar Second -lumbrical/interossei study, M-U ring = Median-ulnar ring finger study, M-R thumb = Median-radial thumb study
If the results of median SDL and MDL are normal or equivocal despite clinical symptoms of CTS, one or more comparison study of median NCS with neighboring nerves in the same limb is logical.
The recommended tests are the median-ulnar palmar mixed comparison study, the median-ulnar ring finger sensory study, the median-radial thumb sensory study, or the median-ulnar second lumbrical-interossei study (see above). The diagnosis of CTS is confirmed if one, and preferably two, of these tests are abnormal. If the results of these tests are normal, CTS is almost excluded [Figure 1]. Finally, needle EMG of APB muscle for evaluation of CTS severity and C5-T1 innervated muscles for evaluation of radiculopathy must be performed.
Median motor study
The median nerve is stimulated at the wrist (between tendons to the flexor carpi radialis and palmar longus) and at the antecubital fossa (over the brachial artery pulse). The recording electrode is over the abductor pollicis brevis (APB) muscle keeping the distance between the cathode of the stimulator and the active recording electrode btween 4 and 6 cm. Distal Motor Latency (DML) longer than 4.2 ms and Nerve Conduction Velocity (NCV) less than 49 m/s is considered abnormal.
Median sensory study
The median nerve is stimulated in the middle of the wrist between the tendons to the flexor carpi radialis and palmars longus at a distance of 13 cm from the recording electrode (ring electrode), which is placed over the index finger. An SDL (peak latency) longer than 3.5 ms is considered abnormal. Several studies proposed that recording SDL from the index finger has a lower sensitivity than the other median innervated fingers and suggested recording SDL from the thumb, middle or ring fingers.[45,46,47]
Median-ulnar palmar mixed comparison study
The median and ulnar nerves are stimulated in the mid-palm between the second and third metacarpals, and between the fourth and fifth metacarpals, respectively. The recording electrode is at the wrist over the median and ulnar nerves 8 cm proximal to the mid-palm cathode.[48] The compound nerve action potential (CNAP) is recorded from the median and ulnar stimulation and a difference of > 0.4 msec in latency is considered as significant. Palmar mixed studies are abnormal in 66% of the hands symptomatic with CTS.[40] Kimura reported prolonged palm-to-wrist latency in 21% of the hands in which conventional DML and PSL were normal.[13]
Median-ulnar second lumbrical–interossei comparison study
In this study the motor distal latency (MDL) of the median nerve recording the second lumbrical muscle is compared to the ulnar motor latency recording the second intersossei. The recording surface electrode is placed just lateral to the midpoint of a line over the third metacarpal bone that connects the base of the middle finger to the middle of the distal wrist crease.[49] The reference electrode is placed over the second proximal interphalangeal joint. With stimulation of the median and ulnar nerves at the wrist, the compound muscle action potentials (CMAPs) are recorded from the second lumbrical and interosseous muscles, respectively. If a standard and equal distance of 8–10 cm is used for both nerves, a median–ulnar distal latency difference of >0.5 msec is consistent with CTS. This technique has a reported sensitivity of 97.5%.[50] Motor fibers to the lumbrical muscles have a more central position in the median nerve than motor fibers to the thenar muscles and sensory fibers to the digits. In severe CTS, resulting in absent median CMAP and sensory nerve action potentials (SNAPs), second a lumbrical/interossei study localizes the lesion to the wrist in over 90% of the cases.[51] Similarly, this study can still be easily performed in patients with CTS and advanced polyneuropathy associated with absent sensory responses in the hands.[20] In this situation, a median–ulnar distal latency difference of >0.8 msec has the highest sensitivity and specificity.[44]
Median–ulnar ring finger sensory study
Median and ulnar nerves are stimulated at the wrist and antidromic SDLs recording the ring finger at an 11 to 13 cm distance are compared. An orthodromic study is also described. The difference in peak latencies of >0.4 msec is considered as abnormal. This test is abnormal in 82% of the patients with CTS.[40] Some authorities proposed that this test may be more sensitive than other comparative studies.[40,52]
Median–radial thumb sensory study
The median and radial nerves are stimulated at the wrist and SDLs of the median and radial nerves are recorded from the thumb.[53] At an 8–10 cm distance, a difference of >0.4 msec of peak latencies is considered abnormal. This study is abnormal in about 60–69% of the hands with CTS.[40]
Segmental nerve conduction study (‘Inching’ study)
The median nerve is stimulated serially in 1-cm increments from the mid-palm to the distal forearm, and the sensory nerve action potential (SNAP) is recorded antidromically from the index or middle finger.[13] There usually is a latency change of 0.16 to 0.21 msec/cm between the stimulation sites. An abrupt latency increase of >0.4 to 0.5 msec across one or two adjoining segments (usually 2 to 4 cm distal to the distal wrist crease) is consistent with the diagnosis of CTS. Despite the fact that this study is time consuming and subject to measurement error and volume conduction, it could precisely localize the lesion in a large number of symptomatic hands.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gelfman R, Melton LJ third, Yawn BP, Wollan PC, Amadio PC, Stevens JC. Long-term trends in carpal tunnel syndrome. Neurology. 2009;72:33–41. doi: 10.1212/01.wnl.0000338533.88960.b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stevens JC, Smith BE, Weaver AL, Bosch EP, Deen HG, Jr, Wilkens JA. Symptoms of 100 patients with electromyographically verified carpal tunnel syndrome. Muscle Nerve. 1999;22:1448–56. doi: 10.1002/(sici)1097-4598(199910)22:10<1448::aid-mus17>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 3.Rempel D, Evanoff B, Amadio PC, de Krom M, Franklin G, Franzblau A, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88:1447–51. doi: 10.2105/ajph.88.10.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phalen GS. The carpal tunnel syndrome: Seventeen years’ experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48:211–28. [PubMed] [Google Scholar]
- 5.Nathan PA, Keniston RC, Myers LD, Meadows KD, Lockwood RS. Natural history of median nerve sensory conduction in industry: Relationship to symptoms and carpal tunnel syndrome in 558 hands over 11 years. Muscle Nerve. 1998;21:711–21. doi: 10.1002/(sici)1097-4598(199806)21:6<711::aid-mus2>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 6.Bland JD. Do nerve conduction studies predict the outcome of carpal tunnel decompression? Muscle Nerve. 2001;24:935–40. doi: 10.1002/mus.1091. [DOI] [PubMed] [Google Scholar]
- 7.Simpson JA. Electrical signs in the diagnosis of carpal tunnel and related syndromes. J Neurol Neurosurg Psychiatry. 1956;19:275–80. doi: 10.1136/jnnp.19.4.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas PK. Motor nerve conduction in carpal tunnel syndrome. Neurology. 1960;10:1045–50. doi: 10.1212/wnl.10.12.1045. [DOI] [PubMed] [Google Scholar]
- 9.Lambert EH. Diagnostic value of electrical stimulation of motor nerves. Electroencephalogr Clin Neurophysiol. 1962;(Suppl 22):9–16. [Google Scholar]
- 10.Gilliatt RW, Sears TA. Sensory nerve action potentials in patients with peripheral nerve lesions. J Neurol Neurosurg Psychiatry. 1958;21:109–18. doi: 10.1136/jnnp.21.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eklund G. A new electrodiagnostic procedure for measuring sensory nerve conduction across the carpal tunnel. Ups J Med Sci. 1975;80:63–4. doi: 10.3109/03009737509178994. [DOI] [PubMed] [Google Scholar]
- 12.Stevens JC. AAEM minimonograph #26: The electrodiagnosis of carpal tunnel syndrome. American Association of Electrodiagnostic Medicine. Muscle Nerve. 1997;20:1477–86. doi: 10.1002/(sici)1097-4598(199712)20:12<1477::aid-mus1>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 13.Kimura J. The carpal tunnel syndrome: Localization of conduction abnormalities within the distal segment of the median nerve. Brain. 1979;102:619–35. doi: 10.1093/brain/102.3.619. [DOI] [PubMed] [Google Scholar]
- 14.Nathan PA, Keniston RC, Meadows KD, Lockwood RS. Predictive value of nerve conduction measurements at the carpal tunnel. Muscle Nerve. 1993;16:1377–82. doi: 10.1002/mus.880161217. [DOI] [PubMed] [Google Scholar]
- 15.Johnson EW, Kukla RD, Wongsam PE, Piedmont A. Sensory latencies to the ring finger: Normal values and relation to carpal tunnel syndrome. Arch Phys Med Rehabil. 1981;62:206–8. [PubMed] [Google Scholar]
- 16.Monga TN, Laidlow DM. Carpal tunnel syndrome. Measurement of sensory potentials using ring and index fingers. Am J Phys Med. 1982;61:123–9. [PubMed] [Google Scholar]
- 17.Lauritzen M, Liguori R, Trojaborg W. Orthodromic sensory conduction along the ring finger in normal subjects and in patients with carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol. 1991;81:18–23. doi: 10.1016/0168-5597(91)90099-j. [DOI] [PubMed] [Google Scholar]
- 18.Valls J, Llanas JM. Orthodromic study of the sensory fibers innervating the fourth finger. Muscle Nerve. 1988;11:546–52. doi: 10.1002/mus.880110605. [DOI] [PubMed] [Google Scholar]
- 19.Pease WS, Cannell CD, Johnson EW. Median to radial latency difference test in mild carpal tunnel syndrome. Muscle Nerve. 1989;12:905–9. doi: 10.1002/mus.880121106. [DOI] [PubMed] [Google Scholar]
- 20.Preston DC, Logigian EL. Lumbrical and interossei recording in carpal tunnel syndrome. Muscle Nerve. 1992;15:1253–7. doi: 10.1002/mus.880151106. [DOI] [PubMed] [Google Scholar]
- 21.Padua L, Lo Monaco M, Valente EM, Tonali PA. A useful electrophysiologic parameter for diagnosis of carpal tunnel syndrome. Muscle Nerve. 1996;19:48–53. doi: 10.1002/(SICI)1097-4598(199601)19:1<48::AID-MUS6>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 22.Therimadasamy AK, Li E, Wilder-Smith EP. Can studies of the second lumbrical interossei and its premotor potential reduce the number of tests for carpal tunnel syndrome? Muscle Nerve. 2007;36:491–6. doi: 10.1002/mus.20850. [DOI] [PubMed] [Google Scholar]
- 23.Aurora SK, Ahmad BK, Aurora TK. Silent period abnormalities in carpal tunnel syndrome. Muscle Nerve. 1998;21:1213–5. doi: 10.1002/(sici)1097-4598(199809)21:9<1213::aid-mus16>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 24.Imaoka H, Yorifuji S, Takahashi M, Nakamura Y, Kitaguchi M, Tarui S. Improved inching method for the diagnosis and prognosis of carpal tunnel syndrome. Muscle Nerve. 1992;15:318–24. doi: 10.1002/mus.880150310. [DOI] [PubMed] [Google Scholar]
- 25.Chang CW, Lien IN. Comparison of sensory nerve conduction in the palmar cutaneous branch and first digital branch of the median nerve: A new diagnostic method for carpal tunnel syndrome. Muscle Nerve. 1991;14:1173–6. doi: 10.1002/mus.880141205. [DOI] [PubMed] [Google Scholar]
- 26.Kaul MP, Pagel KJ, Dryden JD. When to use the combined sensory index. Muscle Nerve. 2001;24:1078–82. doi: 10.1002/mus.1113. [DOI] [PubMed] [Google Scholar]
- 27.Simovic D, Weinberg DH. The median nerve terminal latency index in carpal tunnel syndrome: A clinical case selection study. Muscle Nerve. 1999;22:573–7. doi: 10.1002/(sici)1097-4598(199905)22:5<573::aid-mus4>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 28.Gordon C, Bowyer BL, Johnson EW. Electrodiagnostic characteristics of acute carpal tunnel syndrome. Arch Phys Med Rehabil. 1987;68:545–8. [PubMed] [Google Scholar]
- 29.Pease WS, Cunningham ML, Walsh WE, Johnson EW. Determining neurapraxia in carpal tunnel syndrome. Am J Phys Med Rehabil. 1988;67:117–9. doi: 10.1097/00002060-198806000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Lesser EA, Venkatesh S, Preston DC, Logigian EL. Stimulation distal to the lesion in patients with carpal tunnel syndrome. Muscle Nerve. 1995;18:503–7. doi: 10.1002/mus.880180505. [DOI] [PubMed] [Google Scholar]
- 31.Gilliatt RW, Meer J. The refractory period of transmission in patients with carpal tunnel syndrome. Muscle Nerve. 1990;13:445–50. doi: 10.1002/mus.880130512. [DOI] [PubMed] [Google Scholar]
- 32.Palliyath SK, Holden L. Refractory studies in early detection of carpal tunnel syndrome. Electromyogr Clin Neurophysiol. 1990;30:307–9. [PubMed] [Google Scholar]
- 33.Evans BA, Daube JR. A comparison of three electrodiagnostic methods of diagnosing carpal tunnel syndrome. Muscle Nerve. 1984;7:656. [Google Scholar]
- 34.Joynt RL. Comparison of residual latency and palmar stimulation for diagnosis of carpal tunnel syndrome (abstract) Muscle Nerve. 1984;7:565. [Google Scholar]
- 35.Stevens JC. AAEE minimonograph #26: The electrodiagnosis of carpal tunnel syndrome. Muscle Nerve. 1987;10:99–113. doi: 10.1002/mus.880100202. [DOI] [PubMed] [Google Scholar]
- 36.Macleod WN. Repeater F-waves: A comparison of sensitivity with sensory antidromic wrist-to-palm latency and distal motor latency in the diagnosis of carpal tunnel syndrome. Neurology. 1987;37:773–8. doi: 10.1212/wnl.37.5.773. [DOI] [PubMed] [Google Scholar]
- 37.Cioni R, Passero S, Paradiso C, Giannini F, Battistini N, Rushworth G. Diagnostic specificity of sensory and motor nerve conduction variables in early detection of carpal tunnel syndrome. J Neurol. 1989;236:208–13. doi: 10.1007/BF00314501. [DOI] [PubMed] [Google Scholar]
- 38.Dunnan JB, Waylonis GW. Wrist flexion as an adjunct to the diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil. 1991;72:211–3. [PubMed] [Google Scholar]
- 39.Schwartz MS, Gordon JA, Swash M. Slowed nerve conduction with wrist flexion in carpal tunnel syndrome. Ann Neurol. 1980;8:69–71. doi: 10.1002/ana.410080111. [DOI] [PubMed] [Google Scholar]
- 40.Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve. 1993;16:1392–414. doi: 10.1002/mus.880161220. [DOI] [PubMed] [Google Scholar]
- 41.Guidelines in electrodiagnostic medicine. American Association of Electrodiagnostic Medicine. Muscle Nerve. 1992;15:229–53. doi: 10.1002/mus.880150218. [DOI] [PubMed] [Google Scholar]
- 42.Jablecki CK, Andary MT, Floeter MK, Miller RG, Quartly CA, Vennix MJ, et al. American Association of Electrodiagnostic Medicine; AmericanAcademy of Neurology; American Academy of Physical Medicine and Rehabilitation. Practice parameter: Electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002;58:1589–92. doi: 10.1212/wnl.58.11.1589. [DOI] [PubMed] [Google Scholar]
- 43.American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: Summary statement. Muscle Nerve. 2002;25:918–22. doi: 10.1002/mus.10185. [DOI] [PubMed] [Google Scholar]
- 44.Ubogu EE, Benatar M. Electrodiagnostic criteria for carpal tunnel syndrome in axonal polyneuropathy. Muscle Nerve. 2006;33:747–52. doi: 10.1002/mus.20518. [DOI] [PubMed] [Google Scholar]
- 45.Terzis S, Paschalis C, Metallinos IC, Papapetropoulos T. Early diagnosis of carpal tunnel syndrome: Comparison of sensory conduction studies of four fingers. Muscle Nerve. 1998;21:1543–5. doi: 10.1002/(sici)1097-4598(199811)21:11<1543::aid-mus28>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 46.Kothari MJ, Rutkove SB, Caress JB, Hinchey J, Logigian EL, Preston DC. Comparison of digital sensory studies in patients with carpal tunnel syndrome. Muscle Nerve. 1995;18:1272–6. doi: 10.1002/mus.880181109. [DOI] [PubMed] [Google Scholar]
- 47.Macdonell RA, Schwartz MS, Swash M. Carpal tunnel syndrome: Which finger should be tested? An analysis of sensory conduction in digital branches of the median nerve. Muscle Nerve. 1990;13:601–6. doi: 10.1002/mus.880130707. [DOI] [PubMed] [Google Scholar]
- 48.Daube JR. Percutaneous palmar median nerve stimulation for carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol. 1977;43:139–40. [Google Scholar]
- 49.Al-Shekhlee A, Fernandes-Filho JA, Sukul D, Preston DC. Optimal recording electrode placement in the lumbrical-interossei comparison study. Muscle Nerve. 2006;33:289–93. doi: 10.1002/mus.20488. [DOI] [PubMed] [Google Scholar]
- 50.Loscher WN, Auer-Grumbach M, Trinka E, Ladurner G, Hartung HP. Comparison of second lumbrical and interosseus latencies with standard measures of median nerve function across the carpal tunnel: A prospective study of 450 hands. J Neurol. 2000;247:530–4. doi: 10.1007/s004150070152. [DOI] [PubMed] [Google Scholar]
- 51.Boonyapisit K, Katirji B, Shapiro BE, Preston DC. Lumbrical and interossei recording in severe carpal tunnel syndrome. Muscle Nerve. 2002;25:102–5. doi: 10.1002/mus.10002. [DOI] [PubMed] [Google Scholar]
- 52.Uncini A, Di Muzio A, Awad J, Manente G, Tafuro M, Gambi D. Sensitivity of three median-to-ulnar comparative tests in diagnosis of mild carpal tunnel syndrome. Muscle Nerve. 1993;16:1366–73. doi: 10.1002/mus.880161215. [DOI] [PubMed] [Google Scholar]
- 53.Pease WS, Cannell CD, Johnson EW. Median to radial latency difference test in mild carpal tunnel syndrome. Muscle Nerve. 1989;12:905–9. doi: 10.1002/mus.880121106. [DOI] [PubMed] [Google Scholar]


