Abstract
Background and Objectives:
Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is the standard modality for diagnosing pancreatic masses. We compared the diagnostic yield of a new EUS-guided 22-gauge core needle biopsy to a standard 25-gauge FNA in sampling the same pancreatic lesions during the same EUS.
Patients and Methods:
The main outcomes of the study were the sample adequacy of each method to provide a final pathological diagnosis, and the concordance in diagnosis between core and FNA specimens. The secondary outcomes were the sensitivity and specificity of the findings for each needle and the incremental yield of using both needles compared with using each needle alone.
Results:
A total of 56 patients with 61 solid pancreatic lesions were evaluated. The mean number of passes with FNA was 3.5 (ranges 1-8) and with core biopsy needle was 1.7 (ranges 1-5). The proportions of adequate samples were 50/61 (81.9%) for FNA and 45/61 (73.8%) for core biopsy (P = 0.37). The diagnostic yield was 46/61 (75.4%), 42/61 (68.9%) and 47/61 (77.1%) for FNA, core, and both, respectively. There was a substantial agreement of 87.5% (κ = 0.77; P < 0.001) in the findings of core and FNA specimens. The sensitivity for the diagnosis of malignancy for FNA and core biopsy were 68.1% and 59.6%, respectively (P = no significant [NS]). The specificity was 100% for both methods. The incremental increase in sensitivity and specificity by combining both methods are 1.5% and 0%, respectively.
Conclusion:
There are NS differences in the diagnostic yield between EUS-guided 22-gauge core biopsy and standard 25-gauge FNA for diagnosing pancreatic lesions, but core biopsy required fewer numbers of passes. There was NS incremental diagnostic yield when using both needles during the same procedure.
Keywords: 22-gauge, 25-gauge, core, endoscopic ultrasound, fine-needle aspiration, pancreas
INTRODUCTION
Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) has been shown to be a safe and highly accurate diagnostic modality for pancreatic masses.[1,2] Real time assessment of cytopathology samples at the bedside increases diagnostic accuracy and efficiency of the procedure,[2,3] but this setting is costly, time consuming and not widely available in routine clinical practice.[4] To offset some of these limitations, “Tru-Cut” core needles have been developed to provide larger amounts of tissue with conserved architecture for better histological analysis.[5]
However, compared to the conventional 22-gauge FNA needle, the initial 19-gauge core needle had a lower accuracy for diagnosing pancreatic lesions,[4,6,7] related to the limited flexibility of the needle especially in the setting of an angled scope in the duodenum.[6,7,8] In 2012, a new EUS-guided needle with a side fenestration, also known as core biopsy needle (22-gauge Echo Tip ProCore, Cook Medical Inc., Limerick, Ireland) with improved flexibility was introduced to allow better sampling of pancreatic head lesions. Bang et al. has demonstrated in a randomized trial of 56 patients with solid pancreatic lesions the noninferiority of the 22-gauge core biopsy needle in diagnostic yield, technical performance and safety profiles compared to the 22-gauge FNA.[9] Similarly in a smaller retrospective study of 36 patients, Witt et al. demonstrated that the core 22-gauge needle was similar in terms of cytologic interpretability, adequacy, diagnostic accuracy and amount of cell block material to standard 22-gauge FNA.[10] However, no studies have compared the 22-gauge core needle biopsy to the standard 25-gauge FNA. A recent meta-analysis suggested that 25-gauge FNA needles are more sensitive for diagnosing pancreatic malignancy than 22-gauge FNA needles,[11] for which the use of the 25-gauge FNA has increasingly become the standard. Moreover, it remains unknown if the diagnostic yield of EUS-guided sampling can be improved by combining both standard FNA and core needles while sampling the same lesion.
We conducted the current study to compare the diagnostic yield of EUS-guided 22-gauge core needle biopsy to a 25-gauge FNA in sampling the same pancreatic lesions during the same endoscopic procedure.
PATIENTS AND METHODS
Study population
We conducted a retrospective cohort study in patients with solid pancreatic lesions that were detected on cross-sectional imaging. All patients underwent sampling of these lesions by both EUS-guided 22-gauge core biopsy (needle with a side fenestration) and 25-gauge FNA during the same endoscopic procedure.
Study design
These procedures were performed by two endosonographers (KKP and DYS) during a 13 months period from May 2011 to June 2012 at two tertiary care centers in Houston, Texas. FNA and core biopsy specimens were read by a cytopathologist at both institutions. Bedside assessment of FNA tissue sample adequacy by a cytopathologist was available in only one of the two institutions. At the time of the study, it was our policy to routinely perform three to five passes with the two needles. We obtained information on follow-up for at least 6 months after the procedure by the last date of December 31, 2012. For patients without a cancer diagnosis on the initial EUS-guided sampling by either needle, the final diagnosis was made either by surgical specimen when available or clinical follow-up in combination with imaging after at least 6 months from date of the procedure.
The main outcomes of the study were (a) the sample adequacy of each method to provide a final pathological diagnosis. Adequacy of the samples was determined from the pathologist's description of the specimen as either satisfactory or unsatisfactory to provide a definitive pathological diagnosis based on the cellularity of the specimen on both the smear and cell block material, and (b) the concordance in diagnosis between the core needle and FNA specimens.
The secondary outcomes were the sensitivity and specificity for each needle, and the incremental yield of using each or both needles compared to using each needle alone. These were secondary aims because the gold standard (surgical specimen) was not available in all cases.
Information on adverse events was also obtained by reviewing the procedure reports for immediate complications and emergency room visits or hospitalizations for delayed complications.
Statistical analysis
Individual patients were the unit of analysis. The diagnostic yield was calculated as the percentage of all cases with adequate specimen diagnosed with malignant or nonmalignant pancreatic lesions by EUS-guided sampling. The diagnostic yield could be malignant or nonmalignant. The sensitivity of any diagnostic modality in the study was calculated as the proportion of patients correctly diagnosed with malignant pancreatic lesions. The specificity was calculated as the proportion of patients correctly diagnosed with a nonmalignant tissue. The gold standard for sensitivity and specificity was the final diagnosis of malignant or nonmalignant pancreatic lesions by EUS, surgery, serial imaging and clinical evaluation during at least 6 months after EUS. The concordance between EUS-guided tissue diagnosis by FNA and core needles was calculated using Lin's concordance coefficient to determine the positive agreement between the FNA and core biopsy samples. The Chi-square test was used to compare proportions, and the t-test was used to compare the number of needle passes between the two methods.
The Institutional Review Board of Baylor College of Medicine approved this study. Informed consent was obtained from all patients prior to EUS.
RESULTS
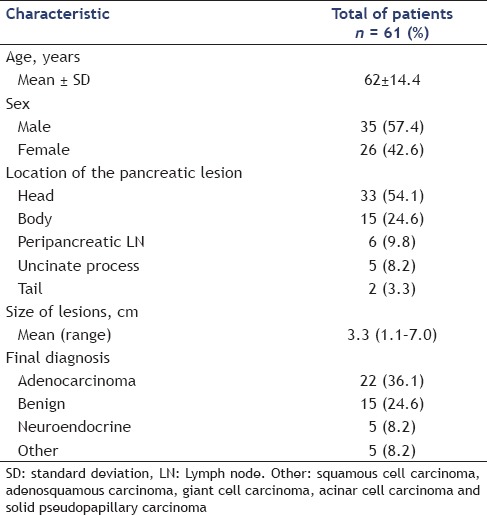
A total of 56 patients with 61 pancreatic lesions were analyzed [Table 1]; 35 were male (57.4%), and the mean age was 61 years (ranges 24-87). Four patients had two separate pancreatic lesions sampled during the same procedure, and one patient had the same lesion sampled during two separate procedures. The lesions were mostly located in the pancreatic head or body, but also in the uncinate process (n = 5), tail (n = 2), and peripancreatic lymph nodes (n = 6).
Table 1.
Characteristics of the study patients and their pancreatic lesions
The proportions of adequate samples were 50/61 (81.9%) for FNA and 45/61 (73.8%) for core biopsy with no significant (NS) differences (P = 0.37). The mean number of passes with FNA was 3.5 (ranges 1-8), and the mean number of passes with the core biopsy needle was 1.7 (ranges 1-5) [Table 2].
Table 2.
Comparison of outcomes of the two procedures

The diagnostic yield (malignant or nonmalignant) was 46/61 (75.4%), 42/61 (68.9%) and 47/61 (77.1%) for EUS-guided FNA, EUS-guided core, and both combined, respectively. There was a substantial agreement of 87.5% (ϰ = 0.77; P < 0.001) between the findings of the core biopsy and FNA.
The diagnostic yield for malignant lesions was 32/40 (80%), 28/40 (70%) and 32/40 (80%) for EUS-guided FNA, EUS-guided core, and both combined, respectively. The histopathologic diagnosis of these malignant lesions was adenocarcinoma (n = 22), neuroendocrine tumors (n = 5) and one each for squamous cell carcinoma, adenosquamous carcinoma, giant cell carcinoma, acinar cell carcinoma, and solid pseudopapillary carcinoma.
Fine-needle aspiration provided an incremental diagnostic yield in 4/47 (8.5%) (adenocarcinoma n = 3, atypical cells suspicious of malignancy n = 1) when core biopsy needle was not diagnostic. Conversely, the incremental diagnostic yield of core biopsy needle was 1/47 (2.1%); in that case core biopsy needle provided a diagnostic sample (normal pancreatic tissue) when FNA needle did not, on a patient who had a final diagnosis of focal pancreatitis. The incremental diagnostic yield observed by using information from both techniques was 5/47 (10.6%).
In eight cases both FNA and core missed a malignancy, diagnosis that was later made by surgical specimen resection or by clinical follow-up. These cases included Hodgkin lymphoma (n = 2), neuroendocrine tumor (n = 2) and pancreatic adenocarcinoma (n = 4). Therefore considering a gold standard that combined the diagnostic yield of both needles and clinical and radiological follow-up at least 6 months from date of the procedure, the sensitivity for diagnosing malignancy for FNA and core biopsy were 68.1% and 59.6%, respectively (P = NS). The specificity was 100% for both methods. The incremental increase in sensitivity and specificity by combining both methods during the same procedure are 1.5% and 0%, respectively.
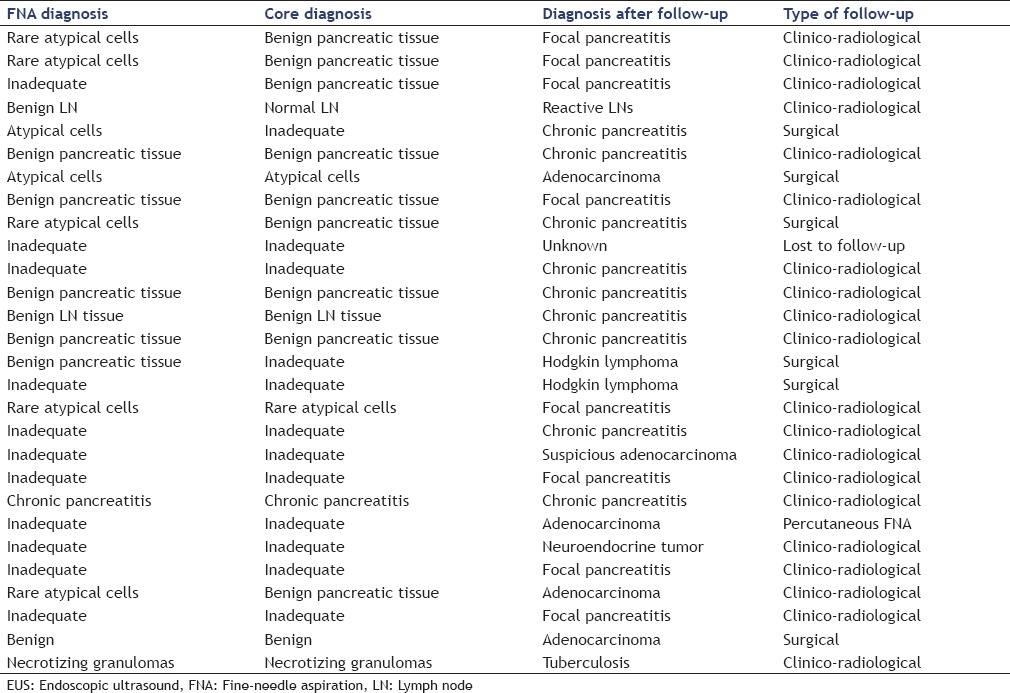
Clinical follow-up in combination with imaging was performed after at least 6 months (mean 9.2; ranges 6-15 months) from the date of the procedure for these cases. The nonmalignant tissue diagnosis by EUS-guided tissue sampling and the final clinico-pathological diagnosis are shown in Table 3.
Table 3.
Initial and final diagnoses on follow-up among 28 cases with EUS-guided nonmalignant samples in either FNA or core
DISCUSSION
This is the largest study to directly compare the diagnostic yield of EUS-guided 22-gauge core needle biopsy (needle with a side fenestration) with 25-gauge standard FNA when sampling a pancreatic lesion during the same endoscopic procedure. There was a substantial agreement for sample adequacy and diagnostic yield between the findings of core biopsy and FNA, but with fewer passes with the core needle. The diagnostic yield and sensitivity were higher with FNA but not statistically significant. There was no incremental yield of using both needles compared to using each needle alone.
Giovannini et al., first evaluated this 22-gauge core needle biopsy in 61 patients, reporting a 90% diagnostic yield, 87% sensitivity and 100% specificity.[12] Subsequent studies, most were published in abstract forms, comparing this 22-gauge core needle biopsy with standard 22-guage FNA showed a comparable or higher sensitivity in favor of the 22-gauge core needle biopsy.[9,13,14,15] Clearly, the 25-gauge FNA is likely to have a better diagnostic yield than the 22-gauge FNA.[11] In our study of 25-gauge FNA, the sample adequacy, diagnostic yield, sensitivity and specificity were at least similar between both methods and numerically higher for sensitivity and diagnostic yield.
We did not find meaningful incremental diagnostic yield when using both needles to sample the same pancreatic lesion during the same procedure when compared with each needle alone. This is consistent with a recent study by Cho et al. who evaluated the added diagnostic yield of sequential EUS-guided 22-gauge core needle after failed adequate tissue sample by EUS-guided FNA in 27 patients with mediastinal lesions.[17] Thus, combined use of both needles appears to the only increase cost with no added diagnostic benefit.
There are other factors in addition to the diagnostic yield, which appears to be similar, that are likely to determine the use of one needle over the other. The use of the on-site cytopathological evaluation increases the diagnostic yield of EUS-guided FNA for the diagnosis of solid pancreatic lesions.[2,3,16] The use of core needles has the advantage of obviating the need for on-site cytopathologist, thus potentially reducing the cost, as well as the total time of the procedure. Furthermore, the reduction in the total number of passes has additional time sparing advantage. In our study, there was a lower number of passes between the core biopsy and FNA; 1.7 versus 3.5, respectively. We did not perform a formal cost analysis and we also did not examine survival as an outcome and, therefore, the cost-effectiveness of these two techniques while likely to be comparable is not clear and much to be further examined.
One of the limitations of the core needle biopsy is the lack of technique standardization, and this may explain the inconsistency of the diagnostic yield with this method. Recently a study comparing three different techniques with this method:
Stylet is rapidly removed before 30 s of half suction (5 mL) is applied followed by five to and fro thrusts of the needle before withdrawal,
Similar to the first technique except full suction (10 mL) is applied, and
Capillary aspiration without suction is used, whereby the stylet is slowly removed over 40 s as the needle is moved to and fro; showed that the capillary biopsy method provided significantly higher tissue adequacy compared to half or full suction methods.[18]
In this study, the core needle missed a diagnosis of malignancy in four cases that FNA had provided a malignant diagnosis. Three of these were lesions in the head of the pancreas. Although the 22-gauge core needle was developed to offset the lack of flexibility of the 19-gauge core needles when sampling lesions in the head of the pancreas, this limitation remains when compared to standard 25-gauge FNA. While the difference did not reach statistical significance in our relatively small sample, their difference could be clinically meaningful. Future studies should further investigate their possible differences. A new 25-gauge core needle has been introduced in the market and studies comparing the 22-gauge versus 25-gauge core needle are required.
Limitations of this study included a lack of information on the sequence of using the needles; it is possible that one needle can impact on the sample obtained by the second needle. Furthermore, the pathologist was not blinded to the samples done by either needle, which could have biased their final interpretation. Due to the retrospective design of the study, we cannot determine how many samples had visible cores when using the side fenestrated needle.
In summary, there was a high concordance between EUS-guided 22-gauge core biopsy and standard 25-gauge FNA for diagnosing pancreatic lesions. The sample adequacy was not different between the two techniques. There was a small, but not statistically significant incremental diagnostic yield with FNA, but core biopsy required fewer numbers of passes. However, there was no incremental diagnostic yield when using both needles to sample the same pancreatic lesion during the same procedure.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Eloubeidi MA, Chen VK, Eltoum IA, et al. Endoscopic ultrasound-guided fine needle aspiration biopsy of patients with suspected pancreatic cancer: Diagnostic accuracy and acute and 30-day complications. Am J Gastroenterol. 2003;98:2663–8. doi: 10.1111/j.1572-0241.2003.08666.x. [DOI] [PubMed] [Google Scholar]
- 2.Afify AM, al-Khafaji BM, Kim B, et al. Endoscopic ultrasound-guided fine needle aspiration of the pancreas. Diagnostic utility and accuracy. Acta Cytol. 2003;47:341–8. doi: 10.1159/000326531. [DOI] [PubMed] [Google Scholar]
- 3.Iglesias-Garcia J, Dominguez-Munoz JE, Abdulkader I, et al. Influence of on-site cytopathology evaluation on the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of solid pancreatic masses. Am J Gastroenterol. 2011;106:1705–10. doi: 10.1038/ajg.2011.119. [DOI] [PubMed] [Google Scholar]
- 4.Varadarajulu S, Fraig M, Schmulewitz N, et al. Comparison of EUS-guided 19-gauge trucut needle biopsy with EUS-guided fine-needle aspiration. Endoscopy. 2004;36:397–401. doi: 10.1055/s-2004-814316. [DOI] [PubMed] [Google Scholar]
- 5.Levy MJ. Endoscopic ultrasound-guided trucut biopsy of the pancreas: Prospects and problems. Pancreatology. 2007;7:163–6. doi: 10.1159/000104240. [DOI] [PubMed] [Google Scholar]
- 6.Yun SS, Remotti H, Vazquez MF, et al. Endoscopic ultrasound-guided biopsies of pancreatic masses: Comparison between fine needle aspirations and needle core biopsies. Diagn Cytopathol. 2007;35:276–82. doi: 10.1002/dc.20621. [DOI] [PubMed] [Google Scholar]
- 7.Wittmann J, Kocjan G, Sgouros SN, et al. Endoscopic ultrasound-guided tissue sampling by combined fine needle aspiration and trucut needle biopsy: A prospective study. Cytopathology. 2006;17:27–33. doi: 10.1111/j.1365-2303.2006.00313.x. [DOI] [PubMed] [Google Scholar]
- 8.Levy MJ, Wiersema MJ. EUS-guided trucut biopsy. Gastrointest Endosc. 2005;62:417–26. doi: 10.1016/j.gie.2005.04.044. [DOI] [PubMed] [Google Scholar]
- 9.Bang JY, Hebert-Magee S, Trevino J, et al. Randomized trial comparing the 22-gauge aspiration and 22-gauge biopsy needles for EUS-guided sampling of solid pancreatic mass lesions. Gastrointest Endosc. 2012;76:321–7. doi: 10.1016/j.gie.2012.03.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Witt BL, Adler DG, Hilden K, et al. A comparative needle study: EUS-FNA procedures using the HD ProCore(™) and EchoTip(®) 22-gauge needle types. Diagn Cytopathol. 2013;41:1069–74. doi: 10.1002/dc.22971. [DOI] [PubMed] [Google Scholar]
- 11.Madhoun MF, Wani SB, Rastogi A, et al. The diagnostic accuracy of 22-gauge and 25-gauge needles in endoscopic ultrasound-guided fine needle aspiration of solid pancreatic lesions: A meta-analysis. Endoscopy. 2013;45:86–92. doi: 10.1055/s-0032-1325992. [DOI] [PubMed] [Google Scholar]
- 12.Giovannini MM, Iglesias-Garcia J, Larghi A, et al. 796 prospective multicenter evaluation of a novel 22-G echo-tip procore histology EUS-needle in patients with a solid pancreatic mass. Gastrointest Endosc. 2011;73:AB152–3. [Google Scholar]
- 13.Nguyen N. Sa1518 EUS guided fine needle core biopsy versus aspiration for upper gastrointestinal mass lesions: A randomized trial. Gastrointest Endosc. 2012;75:AB188. [Google Scholar]
- 14.Mehendiratta VL, Korenblit J, Infantolino A, et al. Sa1527 type, timing, and route of administration of NSAIDs are important for prevention of post-ERCP pancreatitis: A systematic review and meta-analysis of randomized control trials. Gastrointest Endosc. 2012;75:AB191–2. [Google Scholar]
- 15.Iglesias-Garcia JA, Larino-Noia J, Dominguez-Munoz E. Sa1563 differential diagnosis of solid pancreatic masses: Do procore histology needles improve the diagnostic yield of standard cytology needles? Gastrointest Endosc. 2012;75:AB203. [Google Scholar]
- 16.Alsohaibani F, Girgis S, Sandha GS. Does onsite cytotechnology evaluation improve the accuracy of endoscopic ultrasound-guided fine-needle aspiration biopsy? Can J Gastroenterol. 2009;23:26–30. doi: 10.1155/2009/194351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho CM, Al-Haddad M, Leblanc JK, et al. Rescue endoscopic ultrasound (EUS)-guided trucut biopsy following suboptimal EUS-guided fine needle aspiration for mediastinal lesions. Gut Liver. 2013;7:150–6. doi: 10.5009/gnl.2013.7.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen AM, Pai R, Friedland S, et al. Comparison of EUS-guided pancreas biopsy techniques using the Procore™ needle. Gastrointest Endosc. 2012;75:AB145. [Google Scholar]


