Abstract
Background and Objectives:
It is usually challenging to diagnose intraparenchymal pulmonary nodules and masses that are not adjacent to central airways or esophagus. We evaluated the diagnostic accuracy and safety of endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA) and/or endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) for these lesions.
Materials and Methods:
We performed an Internal Review Board-approved retrospective analysis of all patients who underwent EBUS, EUS, or both for the diagnosis of centrally located pulmonary nodules and masses between November 2008 and July 2013. We report results as median values with ranges.
Results:
We identified 16 consecutive patients who underwent EBUS-TBNA and/or EUS-FNA of pulmonary nodules and masses not adjacent to airways or esophagus. We performed EBUS-FNA in 10 patients, EUS-FNA in five patients, and both EBUS-FNA and EUS-FNA in one patient. Median lung lesion size was 22.5 mm (11-45 mm) and median distance from airway or esophagus was 19 mm (5-30 mm). We obtained a tissue diagnosis in 15 patients (93.8%). There were no procedure-related complications.
Conclusion:
We conclude that EBUS-TBNA and/or EUS-FNA are accurate and safe for the diagnosis of intraparenchymal pulmonary lesions that are not adjacent to central airways or esophagus.
Keywords: Centrally located pulmonary nodule, endobronchial ultrasound, endoscopic ultrasound, needle aspiration
INTRODUCTION
The diagnosis of intraparenchymal pulmonary lesions that are not adjacent to central airways or esophagus can be challenging, since these lesions are often too risky to approach with transthoracic needle biopsy and technically challenging to access with electromagnetic navigation (EMN) bronchoscopy or radial endobronchial ultrasound (EBUS). EBUS-transbronchial needle aspiration (EBUS-TBNA) and endoscopic ultrasound-fine-needle aspiration (EUS-FNA) are well-established techniques for the diagnosis of peribronchial and periesophageal lymph nodes and lung lesions, but until date, there are no reports on the diagnostic efficacy and safety of EBUS-TBNA and/or EUS-FNA for lesions that are not immediately adjacent to the airway or esophagus.[1,2,3,4,5,6,7,8]
The objective of this study was to evaluate the safety and diagnostic accuracy of EBUS-TBNA and/or EUS-FNA for the diagnosis centrally located intraparenchymal lung lesions that are not adjacent to central airways or esophagus.
MATERIALS AND METHODS
Study design
We retrospectively reviewed the chart of patients who underwent EBUS or EUS as a first-line diagnostic approach for centrally located pulmonary nodules that were not immediately adjacent to large airways or esophagus.
Patients
We identified 16 patients evaluated at the University of Minnesota Medical Center from November 2008 to July 2013 who underwent EBUS and/or EUS as first-line diagnostic procedure for an intraparenchymal nodule or mass. The decision of the endoscopic approach was based on a multidisciplinary consensus by thoracic surgeons, an interventional radiologist, and interventional pulmonologists. We defined a centrally located intraparenchymal lung nodule or mass as a lesion that by computed tomography (CT) scan was at least 5 mm away from a large airway or esophagus (the distance from the outer margin of the airway or esophagus to the closest point of the nodule or mass); we recorded lesion size and distance from central airway or esophagus by CT measurements. We excluded the patients with nodules or lesions immediately adjacent to the airway or esophagus from the present study although we do use EBUS and/or EUS for those patients. The Institutional Review Board of the University of Minnesota approved this study.
Procedures
Experienced EBUS and EUS users in a high-volume center performed all the procedures. The decision to perform EBUS and/or EUS was done prior to the procedure and guided by the location of the lesion. We performed all procedures under general anesthesia in the operating room (endotracheal [ET] tube size >8.5 mm or laryngeal mask airway) with dedicated EBUS or EUS endoscopes (GF-UC140P-AL5, BF-UC180F-A and Aloka EU-ME1 ultrasound processor, Olympus, Tokyo, Japan), and 22-gauge needle for EBUS-TBNA (NA-201SX-4022, Olympus, Tokyo, Japan) or 19-gauge needle for EUS-FNA (Boston Scientific, Natick, MA, USA). Although most patients were intubated with an ET tube some required laryngeal mask airway to access the upper-lobe lesions from proximal trachea. For small lesions and lesions that are challenging to image, we often ask the anesthesiologist to remove positive end-expiratory pressure and hold ventilation for a brief period of time to reduce air and motion artifacts.
We sampled intraparenchymal lung lesions 3 times with 5-10 passes each time; specimens were first flushed on a slide with air, followed by saline flush of the remainder of the specimen on a second slide. A cytology technologist was present to prepare slides for rapid on-site evaluation and to save additional material in formalin for subsequent cell-block analysis. In the case of an on-site cytologic diagnosis of malignancy within the lung lesion, we also systematically sample lymph nodes >5 mm in short axis. We do not routinely perform surgical mediastinal lymph node staging if on-site cytology is negative and lymph nodes are of normal size on imaging. All patients had postprocedure chest X-ray after extubation in the recovery room. Example of EBUS and EUS images with corresponding CT scan images is shown in Figures 1 and 2.
Figure 1.
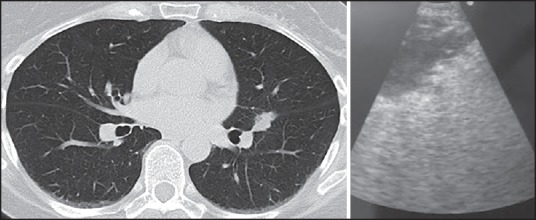
Left - Pulmonary nodule located in the left major fissure, right – Endobronchial ultrasound image of the same nodule
Figure 2.
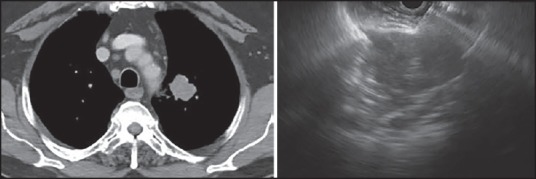
Left – Left upper-lobe mass, right – Endoscopic ultrasound image of fine-needle aspiration through a narrow window superior and posterior to the aortic arch
Definition of diagnosis
The on-site cytologist evaluated all samples to determine the adequacy. The cytologist defined an adequate sample if it provided a diagnosis of malignancy or benign pathology and a nondiagnostic sample if there was no pathologic or insufficient tissue present.
Data analysis
We present data as a number with the percentage (%) or median with range.
RESULTS
Patient characteristics
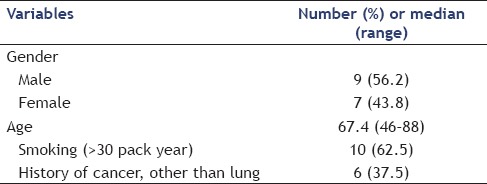
There were nine male patients (56.2%) and the median age was 67.4 years (range of 46-88). Six patients (37.5%) had a history of cancer, including renal cell carcinoma (2), hepatocellular carcinoma (1), head and neck cancer (1), breast cancer (1), and lung cancer (1). The other 10 patients (62.5%) were diagnosed with incidental pulmonary nodule or mass [Table 1].
Table 1.
Patient characteristics
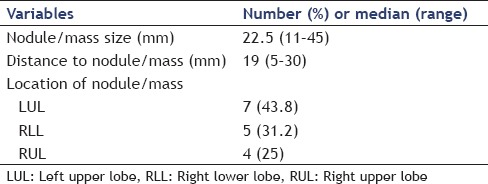
Nodule or mass characteristics
The size of the intraparenchymal lesions on CT scan, the distance from the airway for EBUS or from the esophagus for EUS, and lesion location are shown in Table 2. Nine patients (56%) had a positron emission tomography (PET)-CT scan, and eight patients had a PET positive lesion (SUV, median: 8.6, range: 3.4-32).
Table 2.
Nodule/mass characteristics
Endobronchial ultrasound and endoscopic ultrasound procedures
We used EBUS in five patients, EUS in 10 patients, and both EBUS and EUS in one patient. Eight patients also had lymph node sampling (median: 6.5 mm, range: 5-11 mm) and none was positive for malignancy. There were no procedure-related complications.
Final diagnosis of patients
We obtained a diagnosis of malignancy in 15 of 16 patients (93.8%), and could not obtain a diagnosis in one patient. In patients with a cancer history, four out of six patients (66.7%) were diagnosed with metastatic disease while 2 (33.3%) had new primary lung cancer. In the 10 patients with no prior history of cancer, 9 (90%) were found to have primary nonsmall cell lung cancer (4 squamous cell cancer, 6 adenocarcinoma). One patient who had no history of cancer underwent EBUS and EUS for a right upper-lobe apical nodule but a diagnosis could not be achieved due to the difficulty accessing the lesion. This patient was subsequently sent for CT-guided transthoracic needle aspiration (TTNA) that was positive for adenocarcinoma.
DISCUSSION
Pulmonary nodules are common findings; the diagnosis of indeterminate pulmonary nodules and masses can constitute a considerable challenge in some cases. Guidelines on how to approach pulmonary nodules have been published,[9,10,11] but they do not include the use of EBUS-TBNA and/or EUS-FNA for intraparenchymal lesions not immediately adjacent to central airways or esophagus. The diagnostic approach to suspicious pulmonary nodules depends on the location and size of the lesion. CT-guided TTNA may be a choice for peripheral lesions while centrally located lesions can be reached with various techniques such as conventional bronchoscopy, electromagnetic navigation (EMN) bronchoscopy, and radial probe EBUS or combination. In TTNA, diagnostic yield can be as high as 90% depending upon the length of the needle pass and the size of the nodule.[12,13] Combination of EMN bronchoscopy and radial probe EBUS will increase the sensitivity for diagnostic accuracy to 80-85%, superior to either method alone.[14] Like TTNA, EMN, and radial probe, EBUS are the techniques preferred for peripheral lesions where a visible airway is going into the lesion.
Although the use of EBUS-TBNA and EUS-FNA has been recently published in centrally located lung lesions immediately adjacent to the airway or esophagus[1,2,3,4,5,6] with a diagnostic accuracy range of 86.4-94.3% to date, there are no reports on the use of EBUS-TBNA and/or EUS-FNA to access intraparenchymal lesions not immediately adjacent to central airways or esophagus.
In the present retrospective report, we excluded those patients with nodules or masses adjacent to central airways or esophagus and only included patients with an intraparenchymal nodule or mass >5 mm away from the airway or the esophagus.
We demonstrated that EBUS and/or EUS are useful tools for the diagnosis of centrally located intraparenchymal lesions that are not immediately adjacent to central airways or esophagus with a diagnostic accuracy of 93.8%.
It is important to point out that EBUS and EUS can only reach lesions at needle length that is 4 cm for EBUS and up to 8 cm for EUS. We utilized one of the techniques to reach intraparenchymal lesions away from the airway or the esophagus. Because the needle was passing through normal lung tissue, we hypothesized the risk of pneumothorax would be higher, however, we did not experience any complications including pneumothorax. This could be due to the short distance between the endoscopic puncture sites to the lesion. On the other hand, pneumothorax incidence and need for chest tube insertion in TTNA are 15% to 40% and 10% to 15%, respectively.[15,16]
Our study has the limitations of a retrospective study with a small number case, which allows for selection bias. A prospective and larger study will provide a more accurate sensitivity and specificity of EBUS and/or EUS in cases with true intraparenchymal lesions.
Based on our experience, we favor using EBUS and/or EUS to diagnose centrally located intraparenchymal pulmonary nodules measuring ≥10 mm, as long as the lesions are within the reach of EBUS and EUS needles. We believe that proper patient selection by a multidisciplinary team is essential.
In summary, this is the first study that shows that inexperienced hands, EBUS and/or EUS are safe methods with good diagnostic yield in patients with central intraparenchymal lesions away from the airway or the esophagus. This study broadens the indications and diagnostic application of EBUS and EUS.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Verma A, Jeon K, Koh WJ, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for the diagnosis of central lung parenchymal lesions. Yonsei Med J. 2013;54:672–8. doi: 10.3349/ymj.2013.54.3.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bugalho A, Ferreira D, Eberhardt R, et al. Diagnostic value of endobronchial and endoscopic ultrasound-guided fine needle aspiration for accessible lung cancer lesions after non-diagnostic conventional techniques: A prospective study. BMC Cancer. 2013;13:130. doi: 10.1186/1471-2407-13-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatti HA, Bajwa A, Bhatti JA, et al. Diagnostic yield of EBUS-TBNA for the evaluation of centrally located peribronchial pulmonary lesions. J Bronchology Interv Pulmonol. 2013;20:107–12. doi: 10.1097/LBR.0b013e3182903d86. [DOI] [PubMed] [Google Scholar]
- 4.Nakajima T, Yasufuku K, Fujiwara T, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for the diagnosis of intrapulmonary lesions. J Thorac Oncol. 2008;3:985–8. doi: 10.1097/JTO.0b013e31818396b9. [DOI] [PubMed] [Google Scholar]
- 5.Eckardt J, Olsen KE, Licht PB. Endobronchial ultrasound-guided transbronchial needle aspiration of undiagnosed chest tumors. World J Surg. 2010;34:1823–7. doi: 10.1007/s00268-010-0536-y. [DOI] [PubMed] [Google Scholar]
- 6.Tournoy KG, Rintoul RC, van Meerbeeck JP, et al. EBUS-TBNA for the diagnosis of central parenchymal lung lesions not visible at routine bronchoscopy. Lung Cancer. 2009;63:45–9. doi: 10.1016/j.lungcan.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Alsharif M, Andrade RS, Groth SS, et al. Endobronchial ultrasound-guided transbronchial fine-needle aspiration: The University of Minnesota experience, with emphasis on usefulness, adequacy assessment, and diagnostic difficulties. Am J Clin Pathol. 2008;130:434–43. doi: 10.1309/BLLQF8KDHWW6MJNQ. [DOI] [PubMed] [Google Scholar]
- 8.Andrade RS, Groth SS, Rueth NM, et al. Evaluation of mediastinal lymph nodes with endobronchial ultrasound: The thoracic surgeon's perspective. J Thorac Cardiovasc Surg. 2010;139:578–82. doi: 10.1016/j.jtcvs.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Detterbeck FC, Lewis SZ, Diekemper R, et al. Executive Summary: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:7S–37. doi: 10.1378/chest.12-2377. [DOI] [PubMed] [Google Scholar]
- 10.van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med. 2009;361:2221–9. doi: 10.1056/NEJMoa0906085. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen JH, Ashraf H, Dirksen A, et al. The Danish randomized lung cancer CT screening trial – overall design and results of the prevalence round. J Thorac Oncol. 2009;4:608–14. doi: 10.1097/JTO.0b013e3181a0d98f. [DOI] [PubMed] [Google Scholar]
- 12.Khouri NF, Stitik FP, Erozan YS, et al. Transthoracic needle aspiration biopsy of benign and malignant lung lesions. AJR Am J Roentgenol. 1985;144:281–8. doi: 10.2214/ajr.144.2.281. [DOI] [PubMed] [Google Scholar]
- 13.Fraser RS. Transthoracic needle aspiration. The benign diagnosis. Arch Pathol Lab Med. 1991;115:751–61. [PubMed] [Google Scholar]
- 14.Eberhardt R, Anantham D, Ernst A, et al. Multimodality bronchoscopic diagnosis of peripheral lung lesions: A randomized controlled trial. Am J Respir Crit Care Med. 2007;176:36–41. doi: 10.1164/rccm.200612-1866OC. [DOI] [PubMed] [Google Scholar]
- 15.Ohno Y, Hatabu H, Takenaka D, et al. CT-guided transthoracic needle aspiration biopsy of small (< or = 20 mm) solitary pulmonary nodules. AJR Am J Roentgenol. 2003;180:1665–9. doi: 10.2214/ajr.180.6.1801665. [DOI] [PubMed] [Google Scholar]
- 16.Hur J, Lee HJ, Nam JE, et al. Diagnostic accuracy of CT fluoroscopy-guided needle aspiration biopsy of ground-glass opacity pulmonary lesions. AJR Am J Roentgenol. 2009;192:629–34. doi: 10.2214/AJR.08.1366. [DOI] [PubMed] [Google Scholar]


