Abstract
Background:
Controlling parenchymal hemorrhage, especially in liver parenchyma, despite all the progress in surgical science, is still one of the challenges surgeons face. Therefore, search for an effective method to control hepatic bleeding is an important research priority.
Objectives:
This study attempted to determine the haemostatic effect of ferric sulfate and compare it with the standard method (suturing technique).
Materials and Methods:
In this animal model study, 60 male Wistar rats were used. An incision (2 cm in length and 1/2 cm in depth) was made on each rat’s liver and the hemostasis time was measured using ferric sulfate with different concentrations (5%, 10%, 15%, 25%, and 50%) and then using simple suturing. The liver tissue was assessed for pathological changes.
Results:
In all the groups, complete hemostasis occurred. Hemostasis times of different concentrations of ferric sulfate were significantly less than those of the control group (P < 0.001).
Conclusions:
Ferric sulfate was effective in controlling hepatic bleeding in rats.
Keywords: Hemostasis, Ferric Sulfate, Liver, Rats
1. Background
Control hemorrhage of a solid organ like the liver, due to its rich vascular network, is a challenging task, even in the operating room. The main problem in the liver is the sinusoidal structures of this organ, where blood vessels are too small to be closed using routine techniques (1). On the other hand, the number of operations in which the liver needs to be cut, are numerous (2, 3). The high morbidity and mortality rates of liver injuries are attributed to the large volume of blood loss and extensive bleeding of the patient (4). This has motivated many studies and led to the introduction of new techniques like intermittent clamping of the portal triad for controlling liver bleeding (5); the goal of these studies has been to introduce a method for liver bleeding control, which can prevent complete resection of the bleeding part of the liver (6-9). Ferric sulfate or Fe2SO4 is a dark brown chemical agent with acidic properties. Ferric sulfate exerts its haemostatic effect through a chemical reaction with blood proteins; this property makes ferric sulfate a very efficient haemostatic agent, without need for help from the haemostatic system to exert its effect; even in the patients with abnormal haemostasis, it adequately controls bleeding (10-12). This property, with regard to the significant amount of proteins in the blood, makes ferric sulfate a very strong haemostatic agent. Although the haemostatic effect of this agent has already been shown (10), evaluating this effect of ferric sulfate in controlling liver bleeding and comparing it with the standard method (suturing technique) has not been performed.
2. Objectives
This study sought to determine the haemostatic effect of ferric sulfate and compare it with the standard method (suturing technique) to control bleeding from liver parenchyma.
3. Materials and Methods
3.1. Study Setting and Animals
This study was performed at the Kashan University of Medical Sciences from December 2013 to March 2014. In this study, 60 male Wistar rats, weighing 180-230 g, were randomly divided into six groups, each containing 10 rats. One week before the study, the animals were kept at 21 ± 1°C with 12-hour light/dark cycles (lights on from 8:00 am to 8:00 pm). They had access to standard rat food and water ad libitum. Animal handling and all the experiments were performed in accordance with the international guidelines set out in the Guide for the Care and Use of Laboratory Animals (Institute of Laboratory Animal Resources, 1996) and approved by the local research council of Kashan University of Medical Sciences, Kashan, Iran.
3.2. Surgery
The rats were anesthetized by intraperitoneal (IP) injection of a ketamine/xylazine mixture (ketamine 100 mg/kg and xylazine 10 mg/kg). The 10% ketamine and the 2% xylazine (Alfasan, Netherland) were purchased from a local supplier. Thereafter, the cutaneous and subcutaneous layers in the abdominal zone were opened; after determining the anatomical position of the liver, the liver lobe was extracted from the abdominal cavity. Next, an incision with 2 cm length and 1/2 cm depth was made on the liver by a scalpel (the depth was determined by a mark made on the scalpel 1/2 cm from the tip, and the length was measured with a ruler on the liver).
3.3. Ferric Sulfate Administration and Haemostatic Time Measurement
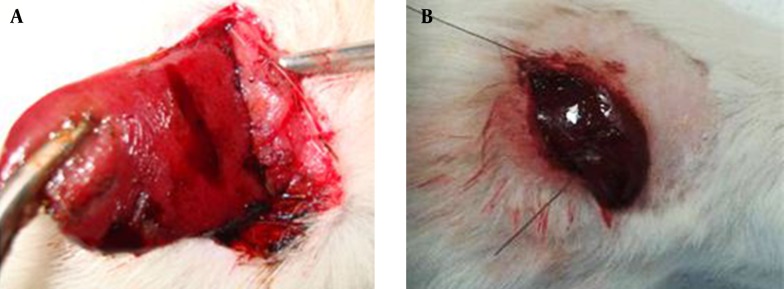
Ferric sulfate was purchased from Merck Company (Darmstadt, Germany). Aqueous solutions of ferric sulfate were prepared in five concentrations of 50%, 25%, 15%, 10% and 5% (w/v) in distilled water; each concentration was used in one group of rats. Half a milliliter of each solution was applied to the incision site by an insulin syringe. The time of hemostasis was measured using a chronometer. The hemostasis time was considered as the time required for complete drying of bleeding and no blood discharge from the incision site (Figure 1). The mean of the measured times in 10 rats of each group was considered as the haemostatic time for each ferric sulfate concentration. Simple suturing using nylon 3-0 was used as the standard method of hemostasis in the control group. All simple sutures were performed by one surgeon. After controlling liver hemorrhage, the subcutaneous layer and skin were closed again, and to prevent infection, each rat received 50 mg of cephalothin through an IP injection. (1 g cefalothin/10 mL, Aspen Pharmacare Australia Pty Ltd, Australia)
Figure 1. Control of the Liver Bleeding. Liver bleeding controlled by ferric sulfate(50%) (A) and the suturing technique (B).
3.4. Pathological Study
Seven days after treatment, all the rats were anesthetized using IP injections of a mixture of ketamine and xylazine (ketamine 100 mg/kg and xylazine 10 mg/kg). Afterwards, the rats were placed in a supine posture on the operating table. Thereafter, an incision was made on the previous site and the rats’ livers were resected and immediately fixed in formalin. Based on the defined pathological grading (12, 13), the pathology results were classified into six groups namely zero, no change; 1, minor inflammatory infiltration without edema; 2, mild to moderate inflammatory infiltration with mild edema; 3, mild to moderate inflammatory infiltration and moderate edema; 4, moderate inflammation with neutrophils scattered and diffuse edema; 5, severe inflammation of the tissue and edematous changes, fibrosis and hemorrhage (Figure 2).
Figure 2. Pathological Effect of Ferric Sulfate (A) and Suturing Technique (B) on the Liver.
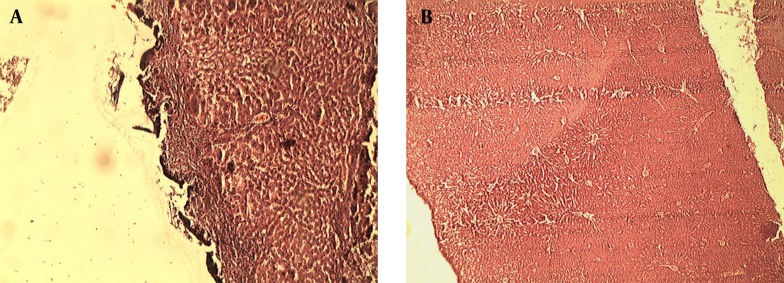
Studying the pathological effect of ferric sulfate and suturing technique on the liver tissue was performed through staining with haematoxylin and eosin (H and E) and light microscopy. The acidic property of ferric sulfate creates a barrier by coagulated proteins and prevents the outflow of blood from vessels. On the other hand, it prevents the ferric sulfate from entering the vessels; and as a result, it prevents potential systemic complications of ferric sulfate.
3.5. Statistical Analysis
Data analysis was performed using SPSS software version 13 (SPSS Inc. Chicago, IL, USA). Kolmogorov-Smirnov test was used to assess normal distribution of data. Kruskal-Wallis test was used to compare the mean hemostasis times in ferric sulfate groups and Mann-Whitney U test was used to compare the mean hemostasis times between ferric sulfate groups and the control group (suturing technique). P-value less than 0.05 was considered significant.
4. Results
4.1. Haemostatic Results
Hemostasis times of the six groups are shown in Table 1. Complete hemostasis occurred in all groups. However, significant difference was observed between the hemostasis times of the six groups (P < 0.001). Moreover, significant differences were observed between the hemostasis times in groups with different concentrations of ferric sulfate and the control group. Hemostasis times in all the experimental groups were significantly less than those of the control group (P < 0.001).
Table 1. Hemostasis Times Using Different Concentrations of Ferric Sulfate and Suturing Technique in Liver Parenchyma a.
| Group | Haemostatic Time |
|---|---|
| Ferric sulfate 5% | 41.5 ± 6.65 |
| Ferric sulfate 10% | 31.3 ± 4.11 |
| Ferric sulfate 15% | 23.2 ± 4.75 |
| Ferric sulfate 25% | 14.5 ± 3.4 |
| Ferric sulfate 50% | 8 ± 2.16 |
| Suture | 89.9 ± 7.41 |
| P value | < 0.001 |
a Data are presented as mean ± SD
4.2. Pathological Results
All the wounds were in grade 1 on the seventh day after the experiment except for the wounds in the groups with 25% and 50% concentrations of ferric sulfate (Table 2). No wound was in grades 0, 3, 4 and 5.
Table 2. The Frequency of Liver Pathological Grade Seven Days after Exposure to Different Concentrations of Ferric Sulfate and Suturing Technique a.
| Group | Pathological Grade | ||
|---|---|---|---|
| Grade 1 | Grade 2 | Total | |
| Ferric sulfate 5% | 10 (100) | 0 (0) | 10 (100) |
| Ferric sulfate 10% | 10 (100) | 0 (0) | 10 (100) |
| Ferric sulfate 15% | 10 (100) | 0 (0) | 10 (100) |
| Ferric sulfate 25% | 3 (30) | 7 (70) | 10 (100) |
| Ferric sulfate 50% | 2 (20) | 8 (80) | 10 (100) |
| Suture | 10 (100) | 0 (0) | 10 (100) |
a Data are presented as No. (%).
5. Discussion
The present study aimed to compare the haemostatic effect of ferric sulfate and simple suturing in controlling liver bleeding. We showed that hemostasis time was significantly shorter in the ferric sulfate groups compared to simple suturing. Currently in treatment centers, the choice technique used to minimize bleeding during liver surgery is based on personal preference, physicians’ experience, and the facilities available. The standard method used to control bleeding from liver lacerations are clamps , deep stitches or the packing (14). Liver bleeding control with sutures can cause more injuries, both parenchymal and ischemic, in the normal liver. On the other hand, the liver parenchymal is not a suitable tissue for stitching ; and with an inexperienced surgeon, the sutures will exacerbate the rupture of liver parenchyma. Packing has the risk of rebleeding and abdominal compartment syndrome, which will impose additional surgery on the patient. Intermittent clamping of the portal triad is also associated with more bleeding than continuous clamping(5). Local agents like fibrin sealants provide a matrix for endogenous coagulation; most of local agents currently used to stop liver bleeding stimulate hemostasis on the cut surface and require normal haemostatic functions. This is a big disadvantage , because many of the cases that require surgery, such as cirrhosis of liver due to liver dysfunction, impair normal hemostatic functions of the body (15). In a large randomized controlled trial in 300 patients undergoing partial liver resection, Figueras and his colleagues found no difference in the total blood loss, transfusion requirements, or postoperative morbidity between patients treated with fibrin sealants (n = 150) compared with a control group without fibrin sealants (n = 150)(16). Aprotinin and tranexamic acid led to a significant reduction in blood loss and transfusion requirements of around 30% to 40%. Due to the recent safety concerns, especially the high risk of renal failure and perioperative death in patients given aprotinin during cardiac surgery, marketing of aprotinin has recently been suspended (17). A number of studies on local haemostatic agents indicated the efficacy of these materials in reducing the haemostatic time as well as the patients’ needs for blood or blood products, leading to improved prognosis of patients after surgery (18, 19). Ferric sulfate unlike well-known haemostatic agents exerts its haemostatic effect through a chemical reaction with blood. This makes it a very efficient agent which does not need normal body haemostatic system to exert its effect (13, 20). On the other hand, it prevents ferric sulfate from entering the vessels, which obviates potential systemic complications of ferric sulfate, such as ferric sulfate-induced thrombosis in liver capillaries and iron toxicity (13, 20). Ferric sulfate solution has been known to cause local pathologic effects and the concentration of local hemostatic agents like ferric sulfate have been an important aspect of the injury response in mouse models (21) ; however, systemic absorption of ferric sulfate is unlikely since the coagulum isolates it from the vascular supply (22). The lethal dose causing 50% mortality (LD50) for ferrous sulfate has been reported to be 168 mg/kg (IP) and 500 mg/kg (oral); but LD50 intradermally has not been reported because of the mentioned acidic property (23). In this study, after the liver tissues were exposed to ferric sulfate, they were sent to the laboratory for pathological examination and the pathological effect of this haemostatic agent was evaluated. To determine the inflammation of liver caused by exposure to the ferric sulfate as a foreign body, a pathological grading was used. This grading was scored from zero to five, according to the severity of the inflammation. Pathological reports showed that ferric sulfate, even at very high concentrations (50%), did not cause any inflammation greater than grade two, and the immune system reaction to this haemostatic agent did not differ much from that of the standard method (sutures) used to controlling superficial bleeding. In two studies, Nouri . sought to assess the haemostatic effect of ferric sulfate and aluminum chloride on external and hepatic bleeding. They reported that ferric sulfate and aluminum chloride were effective haemostatic agents (13, 24). Pathological changes following administration of ferric sulfate and aluminum chloride were consistent with changes that occurred in the present study. Nouri et al. noted that the skin tissue of Wistar rat had a slight inflammatory reaction to ferric sulfate as a foreign body (13). Another characteristic of ferric sulfate is its powerful antimicrobial effect, which gives it an advantage over other haemostatic agents. In a study designed to investigate the antimicrobial effect of haemostatic agents by Cinar and his colleagues, ferric sulfate had stronger antimicrobial effects than other haemostatic agents, and in addition to the powerful haemostatic effect, ferric sulfate was also helpful in tissue repair by reducing the risk of infection (25).
According to Kim's viewpoint, a good haemostatic agent should not interfere with tissue healing, should stop bleeding in a shortest possible time, be portable, ,impose minimum complications and have a reasonable price (26). Considering the definition of a haemostatic agent ferric sulfate does not need a normal haemostatic system to function is an extremely effective topical haemostatic agent and can control liver bleeding effectively.
Acknowledgments
This article was an M.D. dissertation, approved by the Research Council of Kashan University of Medical Sciences, with grant No. 91124. We thank all the participants and those who assisted us with this study.
Footnotes
Authors' Contributions:Saeed Nouri: acquisition of data, analysis and interpretation of data, study supervision, study concept and design, statistical analysis administrative, technical and material support. Mohammad Reza Sharif: drafting of the manuscript, critical revision of the manuscript for important intellectual content.
Funding/Support:This study was supported financially by the Research Council of Kashan University of Medical Sciences.
References
- 1.Holt DR, Thiel DV, Edelstein S, Brems JJ. Hepatic resections. Arch Surg. 2000;135(11):1353–8. doi: 10.1001/archsurg.135.11.1353. [DOI] [PubMed] [Google Scholar]
- 2.Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236(4):397–406. doi: 10.1097/01.SLA.0000029003.66466.B3. discussion 406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makuuchi M, Sano K. The surgical approach to HCC: our progress and results in Japan. Liver Transpl. 2004;10(2 Suppl 1):S46–52. doi: 10.1002/lt.20044. [DOI] [PubMed] [Google Scholar]
- 4.Clark WR, Leather RP. Hemostasis during liver resections. Surgery. 1970;67(3):556–7. [PubMed] [Google Scholar]
- 5.Helewski K, Kowalczyk-Ziomek G, Czecior E, Wyrobiec G, Harabin-Slowinska M, Juszko-Piekut M, et al. Protective effect of intermittent clamping of the portal triad in the rat liver on liver ischemia-reperfusion injury. Hepat Mon. 2011;11(6):445–51. [PMC free article] [PubMed] [Google Scholar]
- 6.Bechstein WO, Neuhaus P. [Bleeding problems in liver surgery and liver transplantation]. Chirurg. 2000;71(4):363–8. doi: 10.1007/s001040051066. [DOI] [PubMed] [Google Scholar]
- 7.Cogbill TH, Moore EE, Jurkovich GJ, Feliciano DV, Morris JA, Mucha P. Severe hepatic trauma: a multi-center experience with 1,335 liver injuries. J Trauma. 1988;28(10):1433–8. [PubMed] [Google Scholar]
- 8.Beal SL. Fatal hepatic hemorrhage: an unresolved problem in the management of complex liver injuries. J Trauma. 1990;30(2):163–9. [PubMed] [Google Scholar]
- 9.David Richardson J, Franklin GA, Lukan JK, Carrillo EH, Spain DA, Miller FB, et al. Evolution in the management of hepatic trauma: a 25-year perspective. Ann Surg. 2000;232(3):324–30. doi: 10.1097/00000658-200009000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fischer DE. Tissue management: a new solution to an old problem. Gen Dent. 1987;35(3):178–82. [PubMed] [Google Scholar]
- 11.Smith NL, Seale NS, Nunn ME. Ferric sulfate pulpotomy in primary molars: a retrospective study. Pediatr Dent. 2000;22(3):192–9. [PubMed] [Google Scholar]
- 12.Nouri S, Sharif MR. Efficacy and safety of ferric chloride in controlling hepatic bleeding; an animal model study. Hepat Mon. 2014;14(6) doi: 10.5812/hepatmon.18652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nouri S, Amirbeigy M, Hosseinpour M, Abdorrahim K, Sharif MR, Amirbeigy M: Evaluation of the Hemostatic Effect of Ferric Sulfate in Controlling Liver Bleeding in Mouse at Kashan University of Medical Sciences, 2012. Iranian J Surg. 2013;21(21-29) [Google Scholar]
- 14.Carrillo EH, Richardson JD. The current management of hepatic trauma. Adv Surg. 2001;35:39–59. [PubMed] [Google Scholar]
- 15.Boonstra EA, Molenaar IQ, Porte RJ, de Boer MT. Topical haemostatic agents in liver surgery: do we need them? HPB (Oxford). 2009;11(4):306–10. doi: 10.1111/j.1477-2574.2009.00065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Figueras J, Llado L, Miro M, Ramos E, Torras J, Fabregat J, et al. Application of fibrin glue sealant after hepatectomy does not seem justified: results of a randomized study in 300 patients. Ann Surg. 2007;245(4):536–42. doi: 10.1097/01.sla.0000245846.37046.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berrevoet F, de Hemptinne B. Use of topical hemostatic agents during liver resection. Dig Surg. 2007;24(4):288–93. doi: 10.1159/000103660. [DOI] [PubMed] [Google Scholar]
- 18.Heaton N. Advances and methods in liver surgery: haemostasis. Eur J Gastroenterol Hepatol. 2005;17 Suppl 1:S3–12. doi: 10.1097/00042737-200504001-00002. [DOI] [PubMed] [Google Scholar]
- 19.Nouri S, Sharif MR, Tabatabaei F, Farokhi S. Investigating the effect of zinc chloride to control external bleeding in rats. Nurs Midwifery Stud. 2014;3(3) doi: 10.17795/nmsjournal22063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lemon RR, Steele PJ, Jeansonne BG. Ferric sulfate hemostasis: effect on osseous wound healing. Left in situ for maximum exposure. J Endod. 1993;19(4):170–3. doi: 10.1016/s0099-2399(06)80681-3. [DOI] [PubMed] [Google Scholar]
- 21.Li W, McIntyre TM, Silverstein RL. Ferric chloride-induced murine carotid arterial injury: A model of redox pathology. Redox Biol. 2013;1(1):50–5. doi: 10.1016/j.redox.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larson PO. Topical hemostatic agents for dermatologic surgery. J Dermatol Surg Oncol. 1988;14(6):623–32. doi: 10.1111/j.1524-4725.1988.tb03390.x. [DOI] [PubMed] [Google Scholar]
- 23.Material Safety Data Sheet – Ferric Sulfate 50% (10% Fe3+) Altiva; 2014. [Google Scholar]
- 24.Nouri S, Sharif MR. Hemostatic effect of aluminum chloride in liver bleeding: an animal model study. Tehran Univ Med J. 2014;72(7):435–42. [Google Scholar]
- 25.Cinar C, Odabas ME, Akca G, Isik B. Antibacterial effect of a new haemostatic agent on oral microorganisms. J Clin Exp Dent. 2012;4(3):e151–5. doi: 10.4317/jced.50750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim S, Rethnam S. Hemostasis in endodontic microsurgery. Dent Clin North Am. 1997;41(3):499–511. [PubMed] [Google Scholar]


