Abstract
Objectives:
To investigate the knowledge, attitude, and barriers using evidence based practice (EBP) by future Saudi dentists and physicians.
Methods:
A questionnaire adapted from an EBP questionnaire was distributed to dental and medical final year students and new graduates at King Abdulaziz University, Jeddah, Saudi Arabia during the 2012 to 2013 academic year. The questionnaire consisted of 14 multiple-choice questions, and 2 open ended questions and was divided into 5 sections assessing different categories. Data were grouped as dental (DS) and medical (MS) students. Descriptive and group comparison statistics were conducted.
Results:
Out of 400, 297 students responded (DS=207, MS=90) with a 74% response rate. The students’ knowledge and attitude were low with no significant difference between the 2 groups. Students’ knowledge and attitudes towards EBP were assessed: EBP course attendance (DS=40.1%, MS=13.3%; p=0.000), reading journals (DS=6.3%, MS=3.3%; p=0.313), awareness of EBP components (DS=7.7%, MS=0%; p=0.332), and awareness towards the strongest evidence for EBP (DS=58.9%, MS=53.3%; p=0.370). More than half of the students in both groups did not use EBP in their treatment (DS=85%, MS=84.4%; p=0.842). The greatest reported barriers were; “EBP is difficult to understand” (DS=88.9%, MS=72.2%; p=0.000), and no time (DS=54.6%, MS=46.7%; p=0.210).
Conclusion:
The reported knowledge and attitudes among the junior health care physicians is considered below the required competency standards. These findings highlight the urgent need for changes in the current educational strategies to assure successful implementation of EBP in Saudi Arabia.
Today, the concept of evidence-based practice (EBP) is gaining ground in dental clinical practice as an interprofessional approach that emphasizes the partnership between finding and using the best current research evidence, along with clinical experience, and individual patient needs and choices to help make health-care decisions.1-3 Evidence-based practice favors the early uptake of new and better treatments or results in the early rejection of ineffective treatments in the evolving dental profession. This approach indicates not only better patient care, but also tremendous change in health care management at an economic and professional level.4-6 The term “evidence-based” has had many iterations over the years. It was first used in 1992 by the clinical epidemiology group at McMaster University in Canada, known as evidence based medicine (EBM) working group.7 They studied the influence of evidence-based guidance on health policy and clinical practice and reported important challenges by stating that it; “de-emphasizes intuition, unsystematic clinical experience, and pathophysiogical rationale as sufficient grounds for clinical decision making”.7 The concept of EBP is well established in medicine and started to be a key feature of high-quality health care.7 Substantial medical resources contain EBM including medical journals, summaries, and practice guidelines.8,9 In addition, the Agency for Healthcare Research and Quality has 12 Evidence-Based Practice Centers located in different universities in the United States and Canada that conduct EBM research.10 In dentistry; however, EBP is less developed but quickly gaining momentum. The American Dental Association (ADA) has made a concerted effort to incorporate EBP into the dental field in the United States, and even included in its website, an entire section devoted to evidence-based dentistry.10,11 This is further evidenced by the movement of dental schools introducing evidence-based curriculums, dental journals including a focus on evidence based dentistry, as well as the establishment of 2 centers for evidence-based dentistry and the inclusion of an Oral Health Database established by the Cochrane Collaboration.12 Despite the well reported needs and demands, EBP implementation has been a challenge for more than 20 years. Many studies have assessed the attitude, knowledge, awareness, barriers and potentials of EBP among the health professions and reported varied results, and with limited success in developing a strong strategy for implementing EBP at national and international levels.13-17 One of the reasons for this, as reported by many researchers, is the absence of a valid and standardized means of assessing the actual EBP behavior during daily practice.18-23 From an educational perspective, EBP requires multiple high level skills such as critical and logical thinking and analysis. It also requires clinical expertise to make judgments and decisions. Limited research has been carried out in Saudi Arabia in that field. Standardized longitudinal follow up studies are highly mandated to draw trends and conclusions on the effectiveness of the developed educational programs in this region. A study by Fedorowicz et al5 was conducted 10 years ago to assess the perception and attitude of dental students at King Saud University, Riyadh, Saudi Arabia. The current study will pursue work in the same direction. The sample in the study of Fedorowicz et al5 was from the dental students only. However, in this study, the scope was broadened to students from the medical and dental health professional fields to provide wider visions for policy and decision makers.
Thus, the aim of this study is to investigate the knowledge, attitude, and barriers towards the use of EBP among dental and medical final year students and new graduates at King Abdulaziz University, Jeddah, Saudi Arabia.
Methods
Study design and sample distribution
This is a cross-sectional survey conducted randomly by distributing 400 questionnaire to dental and medical final year students and new graduates at King Abdulaziz University (KAU), Jeddah, Saudi Arabia during 2012 to 2013 academic year.
Questionnaire design
Questionnaire adapted from EBP questionnaire was distributed to assess the views of healthcare providers in different Arab countries.5 A slight modification of the questionnaire was carried out after a thorough literature review on the subject matter to accommodate updates in the field. The questionnaire was in the English language and consisted of 14 multiple-choice questions and 2 open ended questions. It was divided into 5 sections assessing different categories as follows: 1) The demographic data section included; age, gender, specialty, and level of education. 2) The knowledge and attitudes towards EBP section included questions related to the following; attendance at EBP courses, attitudes towards reading journals, knowledge and awareness toward the components of EBP, and the type of studies that provide the strongest evidence to support EBP. 3) Uses and barriers toward the use of EBP section was designed to assess the use of EBP in real life practice as well as all possible barriers in using it as reported in the literature. 4) Other questions were related to cultural application of EBP and the prediction of the patients’ willingness to participate in clinical trial studies, as well as patients’ capabilities to participate in clinical decision-making. 5) The final section was opened for suggestions and recommendations for effective implementation of EBP in Saudi Arabia.
Ethical approval
Ethical approval and a waiver of consent were obtained from the Ethical Committee of the Faculty of Dentistry, King Abdulaziz University. Each participant received a questionnaire with a covering letter describing the rationale for the study and informed verbal consent was obtained prior to the study.
Statistical analysis
The respondents were grouped as dental students (DS) and medical students (MS) and the data was analyzed accordingly using the Statistical Package for Social Services version 16 and 17 (SPSS, IBM, Armonk, NY, USA). The p-value<0.05 was taken as a cutoff for statistical significance and all tests were 2-sided. Descriptive statistics were conducted using mean, standard deviations, and cross tabs. Inferential statistics were conducted to compare groups in all variables assessed using independent sample t-test, Pearson Chi-square, and Mann-Whitney U test. To simplify the results, some categories were grouped as correct and incorrect answers, and agree and disagree.
Results
Sample distribution
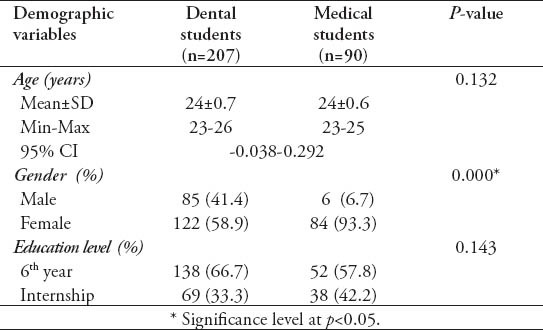
Four hundred questionnaires were randomly distributed to dental and medical students of sixth year and internship level at KAU. Only 297 responded representing a 74% response rate. The data were divided into 2 main groups according to the specialty: DS (n=207) and MS (n=90). Independent sample t-test showed that both groups have a comparable age (Table 1). Mann-Whitney U test revealed a significant difference in gender between the DS and MS groups (p=0.000). The DS group was fairly distributed, while the MS group were mostly females. In both groups, the contribution of the sixth year students was slightly higher than the internship with no significant difference between the groups (p=0.143) (Table 1). Knowledge, attitudes, uses, and barriers of the participants towards EBP were assessed and responses were further analyzed for both groups.
Table 1.
Age, gender, and educational level distribution among the 297 respondents from the 2 assessed groups (dental and medical students).
Knowledge and attitudes
Students’ knowledge and attitudes towards EBP were assessed. Mann-Whitney U test revealed the following results (Figure 1); 1) EBP courses or workshops attendance: The DS group showed significantly higher percentage of EBP course attendance than the MS group (DS=83/207, 40.1%; MS=12/90, 13.3%; p=0.000). 2) Reading journals regularly: both groups reported very low attitudes towards reading journals with no significant difference between them (DS=13/207, 6.3%; MS=3/90, 3.3%; p=0.313). 3) Awareness toward the EBP components: clinical expertise is one of the 3 components of EBP. Students were asked to choose the other 2 from a list that included the following options; famous textbook, senior consultant opinion, the WHO report, EBM resource, and patient choice. Responses were considered correct when both “EB medicine resources” and “patient choice” options were chosen. However, when one of the latter 2 options was chosen, the response was considered partially correct. Other than that it was considered incorrect. Results indicated no significant difference between the 2 groups in their responses (p=0.332). More than half of the students in both groups (DS=133/207, 64.3%; MS=66/90, 73.3%) chose the “EB medicine resource” as an option and were incorrect in the second option. The patient choice was reported by only 7.7% of the DS group (DS=16/207). In addition, the correct option was chosen by 4.3% of the DS group only (DS=9/207). 4) Awareness towards the strongest evidence in the hierarchy of EBP: In the ‘Hierarchy of Evidence’, the students were asked to choose from a list the one study type that provides the strongest ‘evidence’. The list included the following options; animal study, systematic review, cohort study, and case report. Responses were considered correct when the option “systematic review” was chosen. No significant difference was reported between the DS and MS groups (p=0.370). Half of the students from each group chose the correct answer (DS=122/207, 58.9%; MS=48/90, 53.3%).
Figure 1.
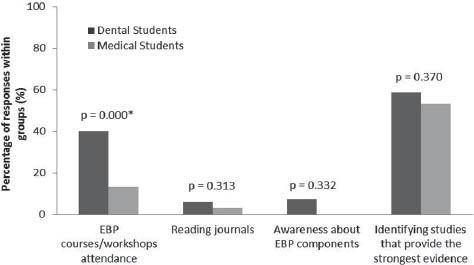
Percentage and significant difference in the response of the dental students and medical students in the categories designed to assess their knowledge and attitudes towards evidence-based practice (EBP) (p<0.05).
Uses and barriers
Students were asked their use regarding of evidence-based approaches in their practices, and the barriers that concerned them. Pearson Chi-square test and Mann-Whitney U test revealed the following results: 1) Have you ever used the EBP approach in ordering tests or treatment? Data of both responses “no” and “not applicable” were grouped to present the percentage of students who did not use EBP in their treatment. Accordingly, most of the students in both groups did not use EBP in ordering tests or treatment with no significant difference between them (DS=167/207, 85%; MS=76/90, 84.4%; p=0.842). 2) What are the most important barriers you are facing in using EBP in your clinical practice (choose 2). Students were given the following list of barriers; internet access, subscription to journals, threat to clinical freedom, it is research and not applicable to clinical practice, evidence is not universally applicable, it is difficult to understand, and no time. Difficult to understand and no time were the greatest reported barriers. Other reported barriers were no subscription to journals and research not applicable to clinical practice (Table 2). 3) If you discover that recent evidence contradicts your clinical judgment what would you do? Students were asked to choose one of the following options; a) discard the evidence, b) follow the evidence, or c) evaluate the evidence. Both groups chose to evaluate the evidence (DS=130/207, 62.8%; MS=68/90, 75.6%) more than following it, and none chose to discard the evidence. However, there was a significant difference between the groups in their responses (p=0.024). 4) The concept of EBP is not applicable to my culture. For meaningful results, data were grouped into 2 components; agree (including results of strongly and partially agree), and disagree (including data of disagree and strongly disagree). A significant difference (p=0.000) between the 2 groups was found in their responses to this statement. Most (DS=155/207, 74.9%) of the DS group agreed that EBP is not applicable to their culture. On the other hand, the MS group responses equally ranged between agreeing (MS=48/90, 46.7%) to disagreeing with the statement (MS=41/90, 36.7%) with one missing response from this group. 5) Patients are willing to participate in clinical decision making. Students were asked about their perception towards the willingness of their patients to participate in clinical decision making as part of the EBP approach. For meaningful results, data were grouped into 2 components; agree (including results of strongly and partially agree), and disagree (including data of disagree and strongly disagree). A significant difference in response was reported between the 2 groups (p=0.000). Almost all the DS group (DS=187/207, 90.3%) expected positive attitudes from patients in participating in clinical decision making. On the other hand, the perception of the MS group ranged between agreeing (MS=64/90, 71.1%), to disagreeing (MS=26/90, 23.3%). 6) What percentage of your patients do you believe would be capable of participating in clinical trial studies? The given choices were 0%, 10%, 25%, 50%, 75%, 100%. Data were grouped into 3 components; <50% (including data of 0%, 10%, 25%), 50% (including data of 50% only), and >50% (including data of 75% only). A significant difference between the MS and DS groups was reported in their estimation of their patients’ participation (p=0.000). Half of the DS group (DS=116/207, 56.0%) felt that 50% of their patients are capable, while half the MS group (MS=61/90, 67.7%) felt that <50% of their patients are capable in participating in clinical trial studies (Figure 2).
Table 2.
Number, percentages, and significant differences in responses between the dental and medical students toward the barriers for evidence-based practice use.
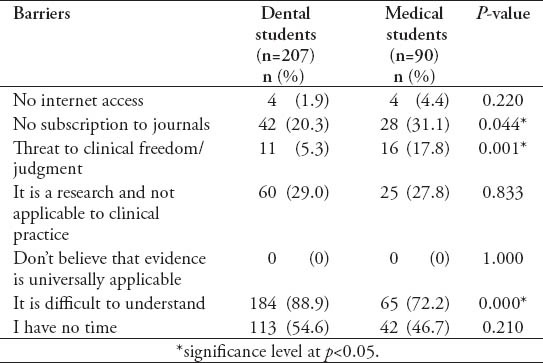
Figure 2.
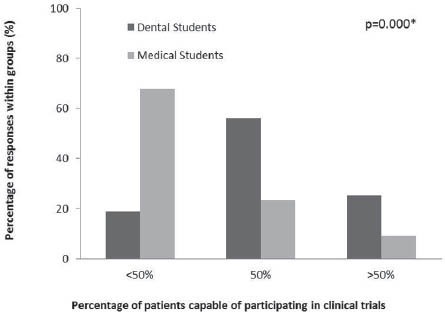
Percentage of responses of the dental students and medical students towards their beliefs in patients’ capabilities of participating in clinical trial studies. *significance level at p<0.05.
For the open ended questions, few responses were reported. The main comments were; lack of incentives for clinicians for implementing EBP, if the treatment was free the patients participation will be higher, clinicians do not give high attention to journal names, and articles are sometimes difficult to understand.
Discussion
The EBP has shifted from the ability to critically appraise the literature into being a key indicator or competency standard for measuring high quality patient-oriented clinical care strategies. This trend has been developed and mandated by the health organizations, such as the National Health Service (NHS), as part of the auditing process and is called clinical governance.24 A further shift in EBP is nowadays moving into safety cultural measures as a competency for designing, developing, and implementing checklists and guidelines for patient safety management.3 An extensive systematic review was conducted by Ubbink et al6 on the knowledge, attitude, and awareness of the health professions towards EBP in attempt to draw a conclusive framework for EBP implementation for policy makers. The framework included proposed structural plans at micro, meso, and macro levels of organizations and stakeholders. Educational institutes are considered the backbone for the success of EBP implementation within that proposed framework. Studying the trends in behavioral changes and competencies among new graduates as part of the outcome assessment of curriculum reforms will guide educators in understanding the needs for educational changes to meet the workforce needs.25 In the current study, the overall general knowledge, and attitude of the students to EBP is substandard to the competency standards that minimally call for skills in critically appraising the evidence.26 The students in the current study reported low attendance of EBP courses as well as poor follow up of journals and updates, especially in the MS group. In the contrary, Fedorowicz et al5 reported that a higher percentage (39%) of their dental students were reading dental journals. Further, nearly 60% of the students in both groups of this study did not use EBP in ordering tests or treatment. Those attitudes may explain their limited awareness of the importance of implementing EBP into their clinical practice. Although the undergraduate medical curriculum at KAU has already incorporated EBP as a major competency standard for more than 6 years, the competence level of the MS group in this area is not positively reflective; thus, further assessment of the undergraduate curriculum from multiple perspectives including, assessing teaching strategies, clinical settings, educators qualifications for EBP, and others is required. On the other hand, the evidence-based competency standard is a new tool in the undergraduate dental curriculum at KAU and has just been implemented. This may explain the results of the DS group in this study.
In the current study, only 7.7% of the DS group and none of the MS group identified the 3 components of EBP. The limited awareness of the students in identifying ‘patient’s choice’ as a main component of EBP needs to be highlighted. Other similar surveys27 reinforced this lack of full awareness of the components of EBP by many dentists. Improving such awareness is important to be highlighted in the undergraduate curriculum with more bedside practices to ensure cultural changes. Patient education might also be a possible strategy for supporting and promoting an EBP cultural environment.26 The main barrier to the use of EBP, as reported in this study, was the difficulty in understanding the concept or subject. Time constraints were also a significant barrier as reported by half of the students in both groups. This finding was inconsistent with Fedorowicz et al,5 wherein limited access to EBP resources was reported as the major issue, while lack of time in their study was reported as the second major issue. The issue of availability of time is a complex one, and is often attributed to clinical overload.6 For final year students, their clinical requirements, and load might be the hidden factor behind their attitude to EBP use and interest. Internet access was not noted as a major barrier in this study (DS=1.9% ; MS=4.4%), which is opposite to the results of Fedorowicz et al’s5 findings, where access to internet was considered as a major barrier (46.6%).5 This result is expected, since the substantial revolution in information technology in the last 10 years in Saudi Arabia made it possible for almost any health care professional to access any relevant information. Although our study did not dissect the cultural barriers in depth, our results show responses from strongly agree to disagree on the awareness of the Saudi culture on the applicability and importance of EBP implementation. More than half of the dental students felt that the vast majority of their patients are capable of participating in clinical trials, and a high percentage of the students in both groups expected that patients are willing to be involved in clinical decision-making. Despite these positive predisposing indicators for cultural acceptance, a high number of the dental students reported that EBP is not applicable to their culture. A similar perception was observed by Fedorowicz et al,5 and they suggested that this might be attributed to external as well as internal beliefs such as “doctor knows best” dominant role of most physicians that might be disturbed by the application of EBP. This belief is arguably a fundamental factor supporting the widely prevalent and firmly rooted attitudes of the socio-cultural traditions in this region. If this hypothesis proved true, then such attitudes and beliefs might indirectly be the factor behind the limited awareness of the students to the importance of patient’s choice in their EBP decision making as mentioned earlier.5 Multiple research and agencies claim that the incorporation of EBP competencies into healthcare system expectations and operations can drive higher quality, reliability, and consistency of healthcare as well as reduce costs.12,25,26 However, current research experience indicates that without a well-designed strategy for the integration of EBP into any clinical settings, the outcome is unpredictable and most of the time it is not worth the effort. The EBP requires an inter-professional approach as well as collective competency skills, knowledge, and clinical expertise.3 It also requires a cultural change and awareness at various organizational levels that is; patient care and education, education of the health professions, the availability of EBP specialists, resources, and centers; and the increased role of policy makers and managers in supporting the implementation of EBP.3,12,25,26 The modern curriculum is facing many challenges to cope with the high level skills required by a competent practitioner in the current era.25 The reported knowledge level, attitude, and barriers in the current study reflect the lack of evidence-based oriented clinical practice as part of the undergraduate clinical training at KAU. These findings highlight the urgent need for changes in the current educational strategies in Saudi Arabia. Searching the evidence and critically appraising it are important competency skills required by the undergraduate students and should be well designed in the curriculum. Teamwork and inter-professional skills are also becoming important competency skills in implementing EBP.3 Separating theory from practice will never assure behavioral and attitude changes and can be a recommendation for educational curriculum reform.26 Further, research is needed to develop and validate tools to assess EBP competencies in the undergraduate curriculums. The other perspective of research should be directed to assessing workforce settings. The difference between the academic and non-academic health care professions might be a hidden factor behind the success of EBP in the work sector.
Study limitations
First, this is a cross-sectional study that was carried out at one time point with no follow up of the sequence of events. However, for future publication it may be more appropriate for the purposes of improving recommendations to conduct a longitudinal study at different subsets and on more than one occasion. Cross-sectional studies do indicate associations that may exist and are therefore, useful in generating hypotheses for future research. A second potential limitation is that we used a convenient sample from KAU. A more heterogeneous sample of students from other universities in the region, and in other regions in Saudi Arabia would have improved generalization. Finally, only 297 responded out of the 400 questionnaires distributed with a 74% response rate. Although we drew statistically significant results; our study sample was small and, thus, results cannot be generalized. Despite those limitations, the results can provide a strong background for more complex research into better incorporation of EBP in the undergraduate curriculum. In-depth analysis of students’ views, and perceptions as well as observational evaluation of students’ bedside implementation of EBP is needed. Research is also needed for assessing the teaching quality and teachers’ qualifications in EBP as well as the institutional funding and support for implementing such strategies especially for adequate access to just in time quality resources in EBP.
In conclusion, this study supports the proposition that well-structured integration of EBP into the under-graduate curriculum as a major competency standard is needed in the Saudi setting. The outcome assessment of such standards should impact not only dental graduates, but also the entire healthcare institution from financial management to patient care levels. It is hoped that the current study would be a pathfinder, in addition to Fedorowicz et al’s5 study that will help health care professions and decision makers in Saudi Arabia to introduce, implement, and evaluate EBP in health care educational institutions. Further studies are needed with more focus group interviews to investigate the hidden factors behind the lack of skills among the undergraduate students in gaining the required competencies for EBP.
Acknowledgment
The authors would like to thank the Deanship of Scientific Research for technical and financial support.
Footnotes
References
- 1.Clarkson J, Harrison JE, Ismail Al Needleman I, Worthington H. London (UK): Martin Dunitz Publishers; 2003. Evidence based dentistry for effective practice. [Google Scholar]
- 2.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitto S, Grant R. Revisiting evidence-based checklists: interprofessionalism, safety culture and collective competence. J Interprof Care. 2014;14:1–3. doi: 10.3109/13561820.2014.916089. [DOI] [PubMed] [Google Scholar]
- 4.Coleman P, Nicholl J. Influence of evidence-based guidance on health policy and clinical practice in England. Qual Health Care. 2001;10:229–237. doi: 10.1136/qhc.0100229... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fedorowicz Z, Almas K, Keenan J. Perceptions and attitudes towards the use of evidence based dentistry (EBD) among final year students and interns at King Saud University, College of Dentistry in Riyadh Saudi Arabia. Brazilian Journal Of Oral Sciences. 2004;3:470–474. [Google Scholar]
- 6.Ubbink DT, Guyatt GH, Vermeulen H. Framework of policy recommendations for implementation of evidence-based practice: a systematic scooping review. BMJ Open. 2013;24:3. doi: 10.1136/bmjopen-2012-001881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evidence-Based Medicine Working Group. Evidence based medicine. JAMA. 1992;268:2420–2425. doi: 10.1001/jama.1992.03490170092032. [DOI] [PubMed] [Google Scholar]
- 8.Washington (DC): National Academy Press; 2001. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. [PubMed] [Google Scholar]
- 9.White B. Making evidence-based medicine doable in everyday practice. Fam Pract Manag. 2004;11:51–58. [PubMed] [Google Scholar]
- 10.ADA Center for Evidence-Based Dentistry. Data Base of Systematic Reviews. [cited September 30, 2009]. Available from: http://ebd.ada.org .
- 11.Rabb-Waytowich D. You ask, we answer: Evidence-based dentistry: Part 1. an over-view. J Can Dent Assoc. 2009;75:27–28. [PubMed] [Google Scholar]
- 12.Ubbink DT, Legemate DA. Evidence-based surgery. Br J Surg. 2004;91:1091–1092. doi: 10.1002/bjs.4717. [DOI] [PubMed] [Google Scholar]
- 13.Burgers JS, Cluzeau FA, Hanna SE, Hunt C, Grol R. Characteristics of high-quality guidelines: evaluation of 86 clinical guidelines developed in ten European countries and Canada. Int J Technol Assess Health Care. 2003;19:148–157. doi: 10.1017/s026646230300014x. [DOI] [PubMed] [Google Scholar]
- 14.Cluzeau FA, Burgers JS, Brouwers M, Grol R, Makela M, Littlejohns P, et al. Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: The AGREE project. Qual Saf Health Care. 2003;12:18–23. doi: 10.1136/qhc.12.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCaughey D, Bruning NS. Rationality versus reality: the challenges of evidence-based decision making for health policy makers. Implement Sci. 2010;5:39. doi: 10.1186/1748-5908-5-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shiffman RN, Shekelle P, Overhage JM, Slutsky J, Grimshaw J, Deshpande AM. Standardized reporting of clinical practice guidelines: a proposal from the Conference on Guideline Standardization. Ann Intern Med. 2003;139:493–498. doi: 10.7326/0003-4819-139-6-200309160-00013. [DOI] [PubMed] [Google Scholar]
- 17.Zwolsman S, te Pas E, Hooft L, Wieringa-de Waard M, van Dijk N. Barriers to GPs’ use of evidence-based medicine: a systematic review. Br J Gen Pract. 2012;62:e511–e521. doi: 10.3399/bjgp12X652382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aitken LM, Hackwood B, Crouch S, Clayton S, West N, Carney D, et al. Creating an environment to implement and sustain evidence based practice: A developmental process. Aust Crit Care. 2011;24:244–254. doi: 10.1016/j.aucc.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ. 2004;329:1017. doi: 10.1136/bmj.329.7473.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kitto S, Petrovic A, Gruen RL, Smith JA. Evidence-based medicine training and implementation in surgery: the role of surgical cultures. J Eval Clin Pract. 2011;17:819–826. doi: 10.1111/j.1365-2753.2010.01526.x. [DOI] [PubMed] [Google Scholar]
- 21.Oude Rengerink K, Zwolsman SE, Ubbink DT, Mol BW, van Dijk N, Vermeulen H. Tools to assess evidence-based practice behaviour among healthcare professionals. Evid Based Med. 2013;18:129–138. doi: 10.1136/eb-2012-100969. [DOI] [PubMed] [Google Scholar]
- 22.Shaneyfelt T, Baum KD, Bell D, Feldstein D, Houston TK, Kaatz S, et al. Instruments for evaluating education in evidence-based practice: a systematic review. JAMA. 2006;296:1116–1127. doi: 10.1001/jama.296.9.1116. [DOI] [PubMed] [Google Scholar]
- 23.Thangaratinam S, Barnfield G, Weinbrenner S, Meyerrose B, Arvanitis TN, Horvath AR, et al. Teaching trainers to incorporate evidence-based medicine (EBM) teaching in clinical practice: the EU-EBM project. BMC Med Educ. 2009;9:59. doi: 10.1186/1472-6920-9-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Majid S, Foo S, Luyt B, Zhang X, Theng YL, Chang YK, et al. Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. J Med Libr Assoc. 2011;99:229–236. doi: 10.3163/1536-5050.99.3.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lang LA, Teich ST. A critical appraisal of evidence-based dentistry: The best available evidence. J Prosthet Dent. 2014;111:485–492. doi: 10.1016/j.prosdent.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Melnyk BM, Gallagher-Ford L, Long LE, Fineout-Overholt E. The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews Evid Based Nurs. 2014;11:5–15. doi: 10.1111/wvn.12021. [DOI] [PubMed] [Google Scholar]
- 27.Dijk N, Hooft L, Wieringa-de Waard M. What are the barriers to residents’ practicing evidence-based medicine? A systematic review. Acad Med. 2010;85:1163–1170. doi: 10.1097/ACM.0b013e3181d4152f. [DOI] [PubMed] [Google Scholar]


