Abstract
Objectives:
To evaluate masticatory efficiency (ME) and oral health-related quality of life (OHRQoL) in patients rehabilitated with implant-retained mandibular overdentures.
Methods:
In this randomized controlled clinical trial, 50 edentulous patients visiting the Implant Center and Department of Prosthodontics, West China College of Stomatology, Sichuan University, Chengdu, China between June 2010 and June 2012 were selected and received 2 implant-retained mandibular overdenture treatments. All patients were rehabilitated with maxillary complete dentures. The ME and OHRQoL were determined both one month before the mandibular complete denture was anchored to the osseointegrated implants, and 6 months after anchoring. Paired t-tests were used to compare means of ME, and oral health impact profile-49 (OHIP-49) domains scores between pre- and post-implant. Linear regression models were utilized to seek correlations between ME and OHIP domains scores.
Results:
The ME increased from pre- to post-implant retained mandibular overdentures significantly (p<0.001). The total OHIP score and 4 subscales scores were changed significantly from pre- to post-implant; namely, functional limitation, psychological discomfort, physical disability, and physical pain. The total OHIP score, functional limitation, physical disability, and physical pain subscale scores were related to ME.
Conclusion:
Implant-retained mandibular over dentures can significantly improve patients’ ME and OHRQoL. The improvement in OHRQoL is mainly because of the improved ME. An improved chewing experience, and pain relief also contributes to improvement of OHRQoL.
For mandibular edentulous patients, conventional complete dentures are not always ideal, although the conventional complete denture procedure is simple, appointment times, and costs less. Many patients are not satisfied with the clinical effects of conventional complete dentures, due to handicaps in eating and speaking, uncomfortable, poor retention, and stability.1-3 An implant-retained complete denture can solve many of the above-mentioned problems and satisfy these patients.4,5 Compared with conventional complete dentures, implant-retained complete dentures have many advantages such as excellent retention, ease of use, and good aesthetics. Masticatory efficiency (ME) with conventional complete denture is almost 30% of natural dentition.6 Thus, as the most important oral function, the ME needs to be improved by implant-retained mandibular overdentures. Many investigators have conducted research, and the results suggest that ME improved substantially after implants are used.4,5,7 Patient-centered standards of oral health-related quality of life (OHRQoL)8 has also been increasingly emphasized in many studies. Restoration success was found to be largely affected by the patient’s point of view, as they feel more subjectively regarding prosthesis stability, comfort, chewing performance, language, and so forth. Compared with conventional complete dentures, 2-implant retained overdentures, as the standard treatment option for mandibular edentulous patients, has lead to a better level of OHRQoL.9,10 It is well known that OHRQoL is influenced by many factors,11 such as the patient’s gender, age, the number of implants, attachment type, level of education, cultural differences, and socio-economic environment,12 all of which are fixed pre-implant parameters and immutable. The role of improved ME in patients with implant-retained mandibular overdentures on improvement in OHRQoL should be detected. The objective of this randomized controlled clinical study was to evaluate ME and OHRQoL in patients rehabilitated with implant-retained mandibular overdentures. In this research, the correlation between improvement of ME and improvement of OHRQoL from pre- to post-implant was also investigated. These findings may be helpful in clinical decision-making regarding implant-retained overdenture options for mandibular edentulous patients.
Methods
A randomized controlled clinical trial was performed in the Department of Prosthodontics, West China College of Stomatology, Sichuan University, Chengdu, China. Patients visiting the West China College of Stomatology account for one-third of the Chinese population, and can therefore be considered representative.
Subjects were selected from mandibular edentulous patients attending the Implant Center and Department of Prosthodontics, West China College of Stomatology, Sichuan University between June 2010 and June 2012 according to the following criteria. Inclusion criteria: 1) age between 55 and 75 years; 2) wearing maxillary and mandibular complete dentures for at least 5 years; 3) willingness to change from the old complete denture; 4) willingness to choose implant-retained mandibular over denture; 5) ability to attend for follow up.
The study was approved by the Research Ethics Committee of Sichuan University, and met the requirements of the Declaration of Helsinki (1989) for prospective clinical studies with humans (informed consent principle).7
Treatment procedure
A new pair of complete dentures was fabricated for each patient. The new dentures were made with semi-anatomically shaped acrylic teeth (Huge Company, Shanghai, China). One month after complete denture delivery, 2 International Team for Implantology (ITI) implants (Strauman Company, Waldenburg, Switzerland) for each subject were placed between the mental foramina, according to a standardized 2-stage surgical protocol.16 The implants were capped with cover screws. One hundred implants with 10 mm length, and 4.1 mm or 4.8 mm diameter were inserted into the 50 subjects. To minimize loading of the implants during the osseointegration period, the tissue surface of the complete denture base corresponding to the implants was ground. Six months after implantation, the second stage of surgery was performed, and abutments were applied. If the interval between the maxillary and mandibular was sufficient enough to accommodate LOCATOR stud attachments, a pair of LOCATOR stud attachments (Straumann Company, City, Switzerland) were applied to anchor the mandibular complete denture, otherwise dental magnetic attachments (Aichi Steel Corp., Tokai, Japan) were applied. After a relining procedure for the intaglio surface of the mandibular denture with self-curing acrylic resin as a final restoration, patients were given instructions on care of the implant-retained overdentures and attachments.
Evaluation
For each subject, the ME, and OHRQoL were determined both one month before the mandibular complete dentures were anchored to the osseointegrated implants, and 6 months after they had been anchored. The ME was evaluated using the gravimetric method. The subjects were instructed to chew test food (4g of peanuts) normally for 20 seconds. The peanuts used in this test were dried and of uniform size. The chewed peanuts were expectorated in a cup, and the mouth thoroughly rinsed twice with water (15 ml). The rinsing was added to the cup to recover all the test food. The whole content of the cup was poured onto a 20-mesh US standard sieve. Fine particles were washed through the sieve with a jet of water. The content of the sieve was dried in an oven and weighed at an electronic balance to get the weight ‘m’. The ME of the patient was ME (ME= 4-m/4 × 100%). This test was repeated 3 times.
The OHRQoL was evaluated using the 49-item version of the Oral Health Impact Profile (OHIP-49). The OHIP-49 is the most standard and validated questionnaire for measuring OHRQoL,17,18 and includes 7 domains: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. The OHIP-49 was translated into Chinese and applied with face-to-face interviews by just one interviewer. Intra-class reliability, test/re-test reliability, and validity were previously evaluated by Slade and Spencer,17 with an intra-class correlation coefficient (ICC) of >0.75. Every item was scaled using a 5-point scale: never = 0, rarely = 1, occasionally = 2, often = 3, very often = 4. The total scores were calculated by adding the 49 items scores and ranged between 0 and 196, with lower scores indicating better OHRQoL. Every domain score of this questionnaire was also calculated.
Statistical analyses
All data were analyzed using the Statistical Package for Social Sciences version 13.0 (SPSS Inc., Chicago, IL, USA). Paired t-tests were used to compare pre- and post-implant ME, OHIP-49 total scores, and every domain score. A level of p<0.05 was considered significant, exact p values and confidence intervals (CI) were used. Effect sizes (ES) were estimated using a procedure recommended by Kazis et al19 to show the size of the change from pre- to post-implant. Effect size can be expressed mathematically as ES = (m1 - m2)/SD, where m1, is the pre-implant mean, m2 the post-implant mean, and SD, the pre-implant standard deviation. Effect size can be used to translate changes in ME and OHIP into a standard unit of measurement that will provide a clearer interpretation of the results. Cohen20 defined an effect size of <0.50 as small, one of 0.50-0.80 as moderate, and one of >0.80 as large. Linear regression models were used to seek correlations between ME and OHIP total scores, and OHIP domains scores. Pearson coefficients of correlation and confidence intervals were used to analyze the strength of haphazard correlations between change of ME and changes of OHIP total scores, and OHIP domains scores. Linear regression models were used to seek the contributions of the confounders (age, gender, living state, education level, and income) on a decrease in OHIP-49 total scores.
Results
Table 1 summarizes the baseline information for 50 patients (28 men and 22 women, aged between 55 and 74 years; mean 62 years) enrolled in the study. In Table 2 indicates that the ME of all subjects in this study increased from pre- to post-implant. The mean difference was 15.17%, which was statistically significant. One subject data was not recorded, as patient contact was lost. Table 3 demonstrates that the total OHIP scores, and 4 OHIP subscales scores were changed significantly in all 7 OHIP domains scores. The ES of OHIP subscales scores were favorable and exceeded the threshold value of 0.5 for functional limitation, psychological discomfort, physical disability, total OHIP scores, and physical pain, indicating good sensitivity to the change. As shown in Table 4, the changes of OHIP subscales scores and total scores were taken as dependent variables, and the variation of ME as an independent variable in the linear regression model. It showed that the OHIP subscales scores changes of functional limitation, physical disability, physical pain, and total OHIP scores were influenced by the changes of ME in a statistically significant way. However, the change of psychological discomfort, psychological disability, social disability, and handicap were not influenced by the changes of ME. The change of ME can explain 80% of the variance in functional limitation, 70% of physical disability, 30% of physical pain, and 62% of the OHIP total scores. However, the change of psychological discomfort cannot be explained by the change of ME. Table 5 demonstrates that socio demographic characteristics were not significantly associated with a decrease in OHIP total scores. All the confounders were not positively associated with a decrease in OHIP total scores (R2=0.007).
Table 1.
Socio-demographic characteristics of 50 patients.
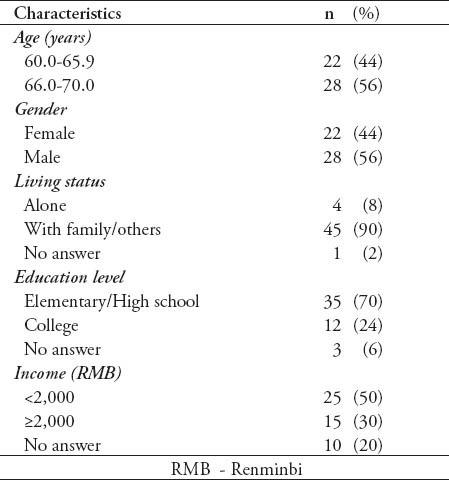
Table 2.
The masticatory efficiency of all subjects increased from pre- to post-implant.

Table 3.
Mean of oral health impact profile (OHIP-49) subscales scores, and effect size (n=50).

Table 4.
Correlation between decrease in Oral Health Impact Profile (OHIP-49) subscale scores and increase in masticatory efficiency (ME).
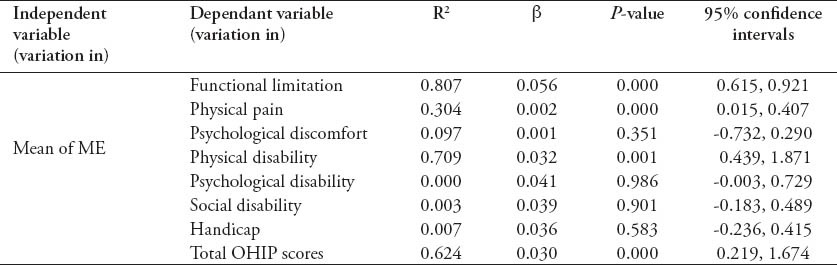
Table 5.
Correlation between sociodemographic characteristics and decrease in oral health impact profile (OHIP-49) total scores.

Discussion
Masticatory efficiency (ME) can exactly reflect a patient’s masticatory function.7 In agreement with the findings of numerous studies,21-23 the ME of all 49 patients increased significantly from pre-implant to post-implant anchor of the complete denture to the mandibular in this study. The retention and stability of the implant-retained mandibular complete denture mainly depend on attachments. The improvement of ME from pre- to post-implantation is mainly because of the improved stability and retention of the complete denture, which also makes the patients feel more comfortable, and easily adapt to the new denture. The width of the chewing cycle affected ME more than the height, mainly during lateral movement.
It is reported that muscle activity is not significantly affected by different attachment types,2 in van der Bilt’s research, 18 patients received 2 implants-retained mandibular overdentures with 3 different attachment modalities: a magnet, a ball, and a bar-clip attachment. Patients’ satisfaction was also reported to not be affected by different attachment styles.24 A recent systematic review by Kimet al25 indicated that the treatment effect with mandibular implant overdenture is not related to attachment system. Thus, the 2 different attachment systems, locator attachment and magnetic attachment, will not influence the results of this study.
In addition to the improvement in ME, a good complete denture can greatly improve the OHRQoL of patients, even though the OHRQoL is a more comprehensive criterion for an edentulous patient. Thus, the evaluation of a restoration’s effect on OHRQoL of patients increased recently.26 In this study, from pro- to post-implant, we found that the average of OHIP total scores reduced from 59.6±25.2 to 39.3±14.7, and reduced by an average of 20.6±28.2 (p<0.001), which indicated that the OHRQoL of patients was significantly improved.
This result was similar to Awad et al,12 who performed an international multicenter study, including 8 centers in North America, South America, and Europe. Their conclusion is that mandibular 2-implant overdentures are more likely than conventional dentures to improve OHRQoL for edentulous patients. The recent review analysis by Thomason27 illustrated that patient OHRQoL is greater with mandibular implant-retained overdentures than conventional dentures; nevertheless, the magnitude of these effects remains uncertain, and heterogeneity of outcomes was observed. An uncertain intensity of effect maybe due to the different characteristics of the population many researchers investigated, and different versions of the OHIP researchers chose, which made the comparisons between studies very difficult. The OHIP-49,17 was the standard to measure OHRQoL with highest level of reliability and validity, from which other versions evolved for simplicity and convenience applications, such as OHIP-EDENT (Oral Health Impact Profile in edentulous adults) questionnaire,8 OHIP-14,15,28 and OHIP-20.29 Although the responsiveness of the 49-item OHIP could be maintained with fewer item versions of OHIP questionnaires, this will lead to compromises in reliability and validity.30 The Chinese version of the OHIP-14 was not tested and verified with the original OHIP-49. We used the translated OHIP-49 in this study, regardless of the fact that this was time consuming and very difficult to analyze.
Seven domains of the OHIP-49 all changed significantly except “psychological disability,” “social disability,” and “handicap”. It can be stated that a mandibular complete denture has little effect on the social function and handicap in the elderly population. The scores at pre-implant in these domains were so low that there is no room for improvement. Preciado et al31 also reported that 100% of patients in his study reported no impact for the ‘‘social disability’’ and ‘‘handicap’’ domains. While, the present study also found no effect of implant overdentures on “psychological disability” domain, this maybe because there are international and cultural differences between different populations investigated.12 The word “disability” has a vague definition in Chinese, which usually refers to severe dysfunction. So the options in “psychological disability” domain may not be understand properly by Chinese patients.
In this study, the effect of implant-retained overdentures on “function limitation (ES=1.3),” “psychological discomfort (ES=1.2),” “physical disability (ES=0.9),” and “physical pain (ES=1.31)” domains was obvious. These findings were very similar to the results reported previously by Jabbour,9 namely, the ES for “functional limitation” was 0.84, “psychological discomfort” was 0.84, and “physical disability” was 1.02. In his study, the domain with the largest ES was “physical pain” (ES=0.5), which means that the effect of implant-retained overdentures on releasing pain more obvious than that in this study. The differences can be attribute to subjects in his studies being of the mean age of 70 years, with reduced adaptive ability, and less likely to adapt to the traditional complete denture. While, in this study, the average age of subjects was 62 years old. “Physical pain and physical disability” and “psychological discomfort and psychological disability” are 2 subscales in the OHIP-49 questionnaire, and there may be a multi-collinearity correlation between them from the view of items in each subscale. However, a discussion of whether subscales in a questionnaire have a multi-collinearity relationship does not make sense, because the reliability of the questionnaire has been previously confirmed.17
In the present study, ME and OHRQoL were determined just 6 months after the mandibular overdentures were anchored to the osseointegrated implants. Such a short-term improvement on OHRQoL was also found by Awad et al,32 who performed a randomized controlled clinical trial with results suggesting that implant treatment provides significant short-term improvement on all subscales of OHRQoL. Although the 49-item version of OHIP was used in Awad et al’s study,32 the samples in the study ranged between the ages of 35-65 and the length of study was not reported. Jabbour9 reported that the effect of 2 implant-retained mandibular overdentures on OHRQoL is stable over a 2-year period.
The correlation analysis revealed that improvement in ME correlated with a decrease in OHIP scores and R2=0.624, which means 62% of the improvement of OHRQoL can be explained by the improvement of ME. The 80% of change in “function limitation,” and 70% of change in “physical disability” can be explained by the improvement of ME. It is suggested that implant-retained mandibular overdenture improved patients’ OHRQoL, and the contribution of improvement in ME is in prominent aspect.15 The objective results of this study confirm the conclusion from Knipfer’s research,15 which was on implant function for improving OHRQoL in elderly patients; mastication and food intake as well as freedom from pain, might play a prominent role. In this study, only 30% of the “physical pain” relief can be explained by the improvement in ME. The stabilizing effect from implant of mandibular complete dentures on the reduction of pain may be more significant. Research by Emami et al29 illustrated that patients with implant retained mandibular complete dentures who perceived no rotational movement were more satisfied with their complete dentures than those who perceived rotation.
The improvement for “psychological discomfort” domain does not have any correlation with the improvement of ME, although the score in “psychological discomfort” changed largely from pre- to post-implant (ES=1.2). The results can be explained by the study of Farias Neto et al,7 which indicated that implant-retained mandibular overdentures significantly improved chewing experience, although no effect on ME has been observed. The improved chewing experience can attribute to the improved stability and retention of implant-retained mandibular overdentures. On the other hand, implant dentures evoked a change in peri-implantal mechanoreceptors, and thus may help spatial control of jaw movements during chewing,33 perception of food flow as well as patients’ interest in food.
The OHRQoL of patients is not only related to patients’ chewing function, but also related to patients’ life, work, and psychological status. Awad stated that pre-implant OHIP scores, age, gender, and marital status explained 31% of the variation in post-treatment OHIP scores.32 While research by Emami et al29 showed that pre-implant OHIP scores, and rotational movements can explain 58% of the variance in the OHIP change score. Post-implant OHIP score was not affected by age, gender, or type of attachment. This can also be justified in the present study. The decrease in OHIP total scores was not significantly associated with age, gender, living state, education level, and income. Complications such as loose/lost abutments, peri-implantitis, retentive force decrease, and fractured denture/teeth may occur in implant-retained overdentures.34 Patients whose prostheses encountered complications tended to express less satisfaction.31 This can explain a part of the variation in OHIP scores, although negatively correlates to OHRQoL.
Previous studies have explored impact factors for post-treatment OHIP score, most of which were unchangeable. The present study explored the correlation between changes in ME and changes in OHIP scores, which is subjective in determining the nature of the improvement in quality of life, as well as being more meaningful for making a sensible decision to choose the best treatment option for a patient. It will be more meaningful if the sample size were greater, and additional randomized controlled clinical trials should research how the ME affects OHIP scores.
In conclusion, implant-retained mandibular overdentures can significantly improve patients’ ME and OHRQoL. The improvement in OHRQoL is mainly because of the improved ME, and improved ME particularly ameliorates patients’ functional performance. An improved chewing experience and pain relief also plays a role in the improvement of OHRQoL.
Footnotes
Illustrations, Figures, Photographs.
Four copies of all figures or photographs should be included with the submitted manuscript. Figures submitted electronically should be in JPEG or TIFF format with a 300 dpi minimum resolution and in grayscale or CMYK (not RGB). Printed submissions should be on high-contrast glossy paper, and must be unmounted and untrimmed, with a preferred size between 4 × 5 inches and 5 × 7 inches (10 × 13 cm and 13 × 18 cm). The figure number, name of first author and an arrow indicating “top” should be typed on a gummed label and affixed to the back of each illustration. If arrows are used these should appear in a different color to the background color. Titles and detailed explanations belong in the legends, which should be submitted on a separate sheet, and not on the illustrations themselves. Written informed consent for publication must accompany any photograph in which the subject can be identified. Written copyright permission, from the publishers, must accompany any illustration that has been previously published. Photographs will be accepted at the discretion of the Editorial Board.
References
- 1.Hyland R, Ellis J, Thomason M, El-Feky A, Moynihan P. A qualitative study on patient perspectives of how conventional and implant-supported dentures affect eating. J Dent. 2009;37:718–723. doi: 10.1016/j.jdent.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 2.der Bilt A, van Kampen FM, Cune MS. Masticatory function with mandibular implant-supported overdentures fitted with different attachment types. Eur J Oral Sci. 2006;114:191–196. doi: 10.1111/j.1600-0722.2006.00356.x. [DOI] [PubMed] [Google Scholar]
- 3.Assad AS, Abd El-Dayem MA, Badawy MM. Comparison between mainly mucosa-supported and combined mucosa-implant-supported mandibular overdentures. Implant Dent. 2004;13:386–394. doi: 10.1097/01.id.0000144512.43654.08. [DOI] [PubMed] [Google Scholar]
- 4.Emami E, Heydecke G, Rompre PH, de Grandmont P, Feine JS. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: a meta-analysis of randomized-controlled trials. Clin Oral Implants Res. 2009;20:533–544. doi: 10.1111/j.1600-0501.2008.01693.x. [DOI] [PubMed] [Google Scholar]
- 5.Sadig W. A comparative in vitro study on the retention and stability of implant-supported overdentures. Quintessence Int. 2009;40:313–319. [PubMed] [Google Scholar]
- 6.Heath MR. The effect of maximum biting force and bone loss upon masticatory function and dietary selection of the elderly. Int Dent J. 1982;32:345–356. [PubMed] [Google Scholar]
- 7.Farias Neto A, Pereira BM, Xitara RL, Germano AR, Ribeiro JA, Mestriner Junior W, et al. The influence of mandibular implant-retained overdentures in masticatory efficiency. Gerodontology. 2012;29:e650–e655. doi: 10.1111/j.1741-2358.2011.00539.x. [DOI] [PubMed] [Google Scholar]
- 8.Albaker AM. The oral health-related quality of life in edentulous patients treated with conventional complete dentures. Gerodontology. 2013;30:61–66. doi: 10.1111/j.1741-2358.2012.00645.x. [DOI] [PubMed] [Google Scholar]
- 9.Jabbour Z, Emami E, de Grandmont P, Rompre PH, Feine JS. Is oral health-related quality of life stable following rehabilitation with mandibular two-implant overdentures? Clin Oral Implants Res. 2012;23:1205–1209. doi: 10.1111/j.1600-0501.2011.02289.x. [DOI] [PubMed] [Google Scholar]
- 10.Assunção WG, Barão VA, Delben JA, Gomes EA, Tabata LF. A comparison of patient satisfaction between treatment with conventional complete dentures and overdentures in the elderly: a literature review. Gerodontology. 2010;27:154–162. doi: 10.1111/j.1741-2358.2009.00299.x. [DOI] [PubMed] [Google Scholar]
- 11.Müller F. Interventions for edentate elders--what is the evidence? Gerodontology. 2014;31(Suppl 1):44–51. doi: 10.1111/ger.12083. [DOI] [PubMed] [Google Scholar]
- 12.Awad MA, Rashid F, Feine JS. Overdenture effectiveness study team consortium. The effect of mandibular 2-implant overdentures on oral health-related quality of life: an international multicentre study. Clin Oral Implants Res. 2014;25:46–51. doi: 10.1111/clr.12205. [DOI] [PubMed] [Google Scholar]
- 13.Koshino H, Hirai T, Ishijima T, Tsukagoshi H, Ishigami T, Tanaka Y. Quality of life and masticatory function in denture wearers. J Oral Rehabil. 2006;33:323–329. doi: 10.1111/j.1365-2842.2005.01152.x. [DOI] [PubMed] [Google Scholar]
- 14.Fueki K, Yoshida E, Igarashi Y. A structural equation model relating objective and subjective masticatory function and oral health-related quality of life in patients with removable partial dentures. J Oral Rehabil. 2011;38:86–94. doi: 10.1111/j.1365-2842.2010.02134.x. [DOI] [PubMed] [Google Scholar]
- 15.Knipfer C, Riemann M, Bocklet T, Noeth E, Schuster M, Sokol B, et al. Speech intelligibility enhancement after maxillary denture treatment and its impact on quality of life. Int J Prosthodont. 2014;27:61–69. doi: 10.11607/ijp.3597. [DOI] [PubMed] [Google Scholar]
- 16.Kampen F, Cune M, van der Bilt A, Bosman F. Retention and postinsertion maintenance of bar-clip, ball and magnet attachments in mandibular implant overdenture treatment: an in vivo comparison after 3 months of function. Clin Oral Implants Res. 2003;14:720–726. doi: 10.1046/j.0905-7161.2003.00961.x. [DOI] [PubMed] [Google Scholar]
- 17.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 18.Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 19.Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27:S178–S189. doi: 10.1097/00005650-198903001-00015. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. United States of America: Lawrence Erlbaum Associates; 1988. Statistical power analysis for the behavioral sciences: Psychology Press. [Google Scholar]
- 21.Müller F, Hernandez M, Grütter L, Aracil-Kessler L, Weingart D, Schimmel M. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: a cross-sectional multicenter study. Clin Oral Implants Res. 2012;23:144–150. doi: 10.1111/j.1600-0501.2011.02213.x. [DOI] [PubMed] [Google Scholar]
- 22.Liao XL, Pan SX, Feng HL, Kang YF, Peng D. [Effect of early-loaded small diameter implants retained mandibular overdentures on masticatory performance] Beijing Da Xue Xue Bao. 2013;45:798–802. Chinese. [PubMed] [Google Scholar]
- 23.Elsyad MA, Hegazy SA, Hammouda NI, Al-Tonbary GY, Habib AA. Chewing efficiency and electromyographic activity of masseter muscle with three designs of implant-supported mandibular overdentures. A cross-over study. Clin Oral Implants Res. 2014;25:742–748. doi: 10.1111/clr.12137. [DOI] [PubMed] [Google Scholar]
- 24.Cordaro L, di Torresanto VM, Petricevic N, Jornet PR, Torsello F. Single unit attachments improve peri-implant soft tissue conditions in mandibular overdentures supported by four implants. Clin Oral Implants Res. 2013;24:536–542. doi: 10.1111/j.1600-0501.2012.02426.x. [DOI] [PubMed] [Google Scholar]
- 25.Kim HY, Lee JY, Shin SW, Bryant SR. Attachment systems for mandibular implant overdentures: a systematic review. J Adv Prosthodont. 2012;4:197–203. doi: 10.4047/jap.2012.4.4.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhai JJ, Wen C, Teng MH, Liang X. Single implant in the mandibular molar region of edentulous patient. Saudi Med J. 2013;34:963–967. [PubMed] [Google Scholar]
- 27.Thomason JM. The use of mandibular implant-retained overdentures improve patient satisfaction and quality of life. J Evid Based Dent Pract. 2012;12(3 Suppl):S182–S184. doi: 10.1016/S1532-3382(12)70032-5. [DOI] [PubMed] [Google Scholar]
- 28.Kuoppala R, Näpänkangas R, Raustia A. Quality of Life of Patients Treated With Implant-Supported Mandibular Overdentures Evaluated With the Oral Health Impact Profile (OHIP-14): a Survey of 58 Patients. J Oral Maxillofac Res. 2013;4:e4. doi: 10.5037/jomr.2013.4204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Emami E, de Souza RF, Bernier J, Rompre P, Feine JS. Patient perceptions of the mandibular three-implant overdenture: a practice-based study. Clin Oral Implants Res. 2014:19. doi: 10.1111/clr.12351. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 30.Awad M, Al-Shamrany M, Locker D, Allen F, Feine J. Effect of reducing the number of items of the Oral Health Impact Profile on responsiveness, validity and reliability in edentulous populations. Community Dent Oral Epidemiol. 2008;36:12–20. doi: 10.1111/j.1600-0528.2006.00364.x. [DOI] [PubMed] [Google Scholar]
- 31.Preciado A, Del Río J, Suárez-García MJ, Montero J, Lynch CD, Castillo-Oyagüe R. Differences in impact of patient and prosthetic characteristics on oral health-related quality of life among implant-retained overdenture wearers. J Dent. 2012;40:857–865. doi: 10.1016/j.jdent.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Awad MA, Locker D, Korner-Bitensky N, Feine JS. Measuring the effect of intra-oral implant rehabilitation on health-related quality of life in a randomized controlled clinical trial. J Dent Res. 2000;79:1659–1663. doi: 10.1177/00220345000790090401. [DOI] [PubMed] [Google Scholar]
- 33.Yan C, Ye L, Zhen J, Ke L, Gang L. Neuroplasticity of edentulous patients with implant-supported full dentures. Eur J Oral Sci. 2008;116:387–393. doi: 10.1111/j.1600-0722.2008.00557.x. [DOI] [PubMed] [Google Scholar]
- 34.Vere J, Hall D, Patel R, Wragg P. Prosthodontic maintenance requirements of implant-retained overdentures using the locator attachment system. Int Journal Prosthodont. 2012;25:392–394. [PubMed] [Google Scholar]


