Abstract
Objectives:
To compare the effects of regular intermittent bolus versus continuous infusion for epidural labor analgesia on maternal temperature and serum interleukin-6 (IL-6) level.
Methods:
This randomized trial was performed in Nanjing Maternity and Child Health Care Hospital, Nanjing, Jiangsu Province, China between October 2012 and February 2014. Either regular intermittent bolus (RIB, n=66) or continuous infusion (CI, n=66) was used for epidural labor analgesia. A bolus dose (10 ml of 0.08% ropivacaine + 0.4 µg·ml-1 sufentanil) was manually administrated once an hour in the RIB group, whereas the same solution was continuously infused at a constant rate of 10 ml·h-1 in the CI group. Maternal tympanic temperature and serum IL-6 level were measured hourly from baseline to one hour post partum. The incidences of fever (≥38ºC) were calculated.
Results:
The incidence of maternal fever was similar between the 2 groups. There was a rising trend in mean temperature over time in both groups, but no statistical difference was detected between the groups at respective time points; maternal serum IL-6 showed similar changes.
Conclusion:
Compared with continuous infusion, regular intermittent bolus presents with the same incidence of maternal fever for epidural labor analgesia. Interleukin-6 elevation could be involved in mean maternal temperature increase.
The relationship between epidural labor analgesia and maternal intrapartum temperature was investigated, and several lines of studies found that epidural labor analgesia was significantly associated with maternal fever.1-6 Although an antipyretic effect of opioids and altered maternal thermoregulation partly explain the etiology, inflammation is involved in the most likely mechanism of fever, such as elevation of maternal serum interleukin-6 (IL-6) levels.7,8 Regular intermittent epidural bolus, with smaller local anesthetics consumption and better patient satisfaction compared with continuous infusion, is becoming increasingly used for labor analgesia.9-12 On-demand intermittent epidural injections showed a lower incidence of intrapartum fever in the first 4 hours of labor analgesia than continuous infusion, with similar maternal serum IL-6 levels at respective time points.13,14 However, the association between regular intermittent epidural bolus and intrapartum fever is still unclear. The aim of the present study was to compare the effects on maternal temperature and serum IL-6 level of regular intermittent bolus versus continuous infusion for epidural labor analgesia.
Methods
We searched for prior related research on the PubMed website using the key words: intermittent, continuous, intrapartum, fever, epidural, labor, analgesia, and interleukin-6. The study protocol was approved by the Institutional Ethics Committee (Nanjing Maternity and Child Health Care Hospital, Nanjing, Jiangsu Province, China) and registered with ClinicalTrials.gov (NCT01708668). All research participants provided written informed consent following the principles of the Helsinki Declaration. Participants consisted of healthy, American Society of Anesthesiologists grade I or II, nulliparous, term women with singleton, vertex pregnancies, and cervical dilatation of 1-3 cm. Parturients were recruited between October 2012 and February 2014. Exclusion criteria included a contraindication to epidural analgesia, a baseline temperature of ≥37.5°C, age <20 years or >45 years, drug abuse, an indication for cesarean delivery, and high-risk pregnancies such as preeclampsia, placenta previa, placental abruption, diabetes mellitus, and hypertension.
One hundred and thirty-two subjects were randomly allocated to receive either regular intermittent bolus (RIB) or continuous infusion (CI) epidural labor analgesia during the latent phase of labor, 66 in each group. Sequentially numbered opaque sealed envelopes containing computer-generated random numbers were used for the group allocation. The unblinded investigator opened the envelopes at the time of randomization; other study personnel and the parturients were all blinded to group allocation. After entering the labor room, the women were intravenously given normal saline warmed to 37°C at a rate of 100 ml·h-1 throughout labor. The labor and delivery rooms were maintained at a temperature of 22°±2°C. Maternal tympanic temperature (first temp Genius® thermometer, Sherwood Medical, St. Louis, MO, USA), epidural sensory levels, visual analogue scale (VAS, 0=no pain; 10=worst imaginable pain), and modified Bromage scale (MBS, 0=no motor block; 1=hip blocked; 2=hip and knee blocked; 3=hip, knee, and ankle blocked) were recorded and maternal peripheral venous blood was drawn before epidural insertion and hourly thereafter until one hour post partum. The thermometer, which was calibrated and validated before measurement, was placed lightly in the ear canal according to the manufacturer’s guidelines. Maternal fever was defined as a temperature greater than 38 degrees Celsius. Neonatal rectal temperature was collected at one h after delivery. Umbilical venous cord blood was sampled post placental delivery. The blood samples were immediately centrifuged at 3000 g for 10 minutes. The serum was then immediately frozen at -70°C until assay for IL-6. Serum levels of IL-6 were measured in duplicate by enzyme-linked immunosorbent assay (ELISA) with commercially available kits (Quantikine, R&D Systems, Minneapolis, MN, USA). The limit of detection was 0.95 pg/ml for IL-6, and inter- and intra-assay coefficients of variation were below 5%. Additional umbilical cord venous and artery blood were collected for blood gas analysis.
Epidural analgesia was initiated at the L3-4 or L2-3 interspace, and the catheter was inserted 3 cm into the epidural space. A 3 ml test dose of 1.5% lidocaine with 1: 200,000 epinephrine was given, followed by 10 ml of 0.125% ropivacaine + 0.4 µg·ml-1 sufentanil. Parturients whose VAS scores were larger than 3 mm 15 minutes after the use of a loading dose were excluded from the study. Two syringe pumps (Graseby 3300; Graseby Medical Ltd., Watford, UK) were connected via a 3-way stopcock to the epidural catheter, one (covered with black paper) set up for either RIB or CI while the other for patient-controlled analgesia (PCA). The epidural solution for both pumps consisted of 0.08% ropivacaine + 0.4 µg·ml-1 sufentanil. In the RIB group, a bolus dose of 10 ml solution was manually given hourly beginning 75 minutes post analgesia. In the CI group, the same solution was continuously infused at a constant rate of 10 ml·h-1 beginning 15 minutes post analgesia. The PCA pump was set to deliver a 5 ml bolus dose with a lockout time of 30 minutes. We advised the parturient to push the PCA button whenever she felt uncomfortable. If the pain relief were inadequate 15 minutes after having activated the PCA bolus, a bolus dose of 5-10 ml of 0.15% ropivacaine was manually given until the VAS was <3 mm. The 2 pumps were discontinued one hour after delivery. Consumption of epidural drugs and number of epidural boluses was noted.
Demographic data were recorded. Obstetric characteristics included group B streptococcus (GBS) colonization, number of vaginal examinations, use of oxytocin augmentation, duration from rupture of the membranes to delivery, mode of membranes ruptured, the durations of labor (epidural insertion to delivery) and analgesia (epidural insertion to discontinuation of the pumps), and mode of delivery. Neonatal weight, Apgar scores, and umbilical cord acid-base status were examined. After delivery, placenta was taken for histopathological examination for inflammation with a grade of 2 or higher according to the previously described method.15
Statistical analysis
Because the incidence of maternal fever during continuous infusion for epidural labor analgesia varied from 10-33%,13,16-19 we presumed that the incidence in the CI group was 22%. We calculated that the sample size of 66 patients per group would maintain an 80% power at a 2-tailed significance level of 0.05 to detect a difference in the incidence of maternal fever between the 2 groups, with an incidence of 5% in the RIB group, and a dropout rate of 10%. Continuous variables were compared between the groups using the Student’s t test, or the Mann-Whitney U test as appropriate. Categorical data were analyzed by x2 or Fisher’s exact test where appropriate. To detect differences of temperature between 2 groups over time, a repeated measures analysis of variance with Bonferroni correction was performed. Statistical analyses were performed using the Statistical Package for Social Sciences for Windows version 17.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
One hundred and twenty-five subjects completed the study protocol and were finally included in the analyses (Figure 1). Three subjects in the RIB group, and 4 women in the CI group were excluded from the study because they opted for a cesarean section without specific reason, with their babies’ Apgar scores ≥9 at one minute, and 10 at 5 minutes. The 2 groups were similar regarding maternal age, height, weight, gestation, and baseline cervical dilatation (Table 1). The VAS pain scores were significantly higher at 3 and 4 hours post analgesia in the CI group compared with those in the RIB group (Figure 2). There were no differences in the epidural sensory levels between the 2 groups (Table 2). For the MBS, all subjects had a score of 0 during the study. There was no difference in the incidence of maternal fever (Table 3) between the 2 groups. In both groups, a rising trend of mean temperatures over time was found, but did reach statistical significance at any time points compared with corresponding baselines (Figure 3). We did not find any statistical difference between the 2 groups at respective time periods regarding mean temperature. Similarly, maternal serum IL-6 levels showed an elevation trend during labor, and reached statistical significance 2 hours post analgesia compared with the respective baselines in the 2 groups (Figure 4). There were no differences in maternal serum IL-6 levels at any time points between the 2 groups. Obstetric, neonatal, and epidural outcomes are listed in Table 4, the number of epidural boluses, consumption of ropivacaine, and sufentanil in the RIB group decreased significantly compared with the CI group. No differences were found between the 2 groups with respect to other outcomes. We did not observe statistical differences between the 2 groups with regard to umbilical cord blood gases analyses (data not shown), which were within normal range in all cases.
Figure 1.
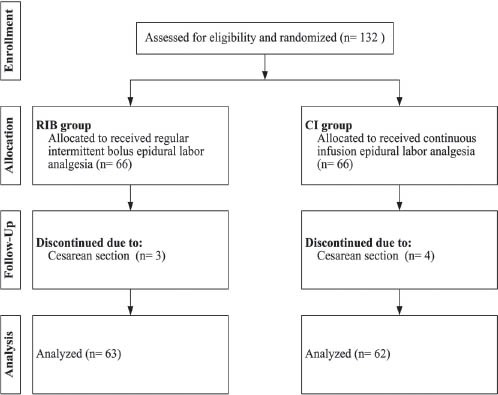
Flow diagram among 132 subjects that completed the study protocol. RIB - regular intermittent bolus, CI - continuous infusion
Table 1.
Baseline demographic characteristics of epidural labor analgesia patients.
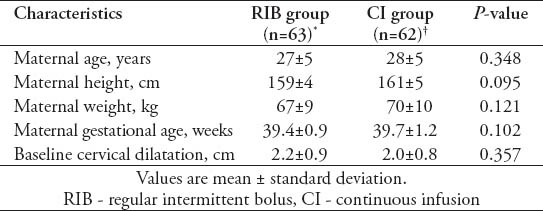
Figure 2.
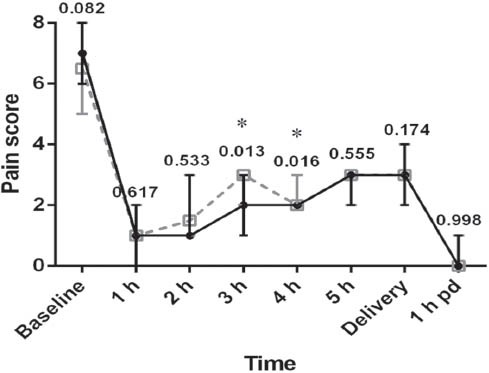
Visual analogue scale pain scores in RIB (black solid line) or CI group (grey dotted line) over time. Error bars are interquartile range. Compared with RIB group, *p<0.05. P-values are presented at corresponding time point. RIB - regular intermittent bolus, CI - continuous infusion, pd - post delivery.
Table 2.
Sensory block levels (thoracic vertebral level).
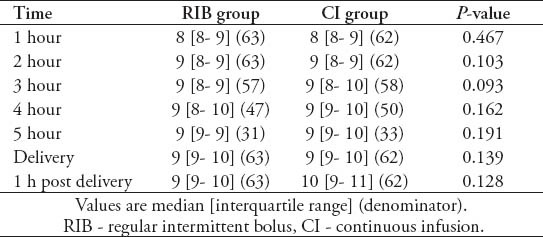
Table 3.
Incidence of maternal fever.
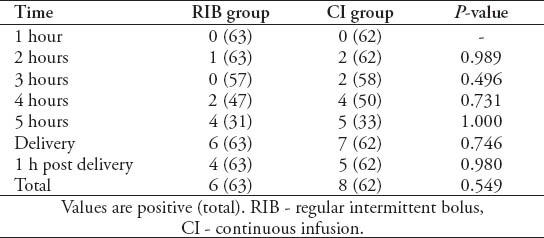
Figure 3.
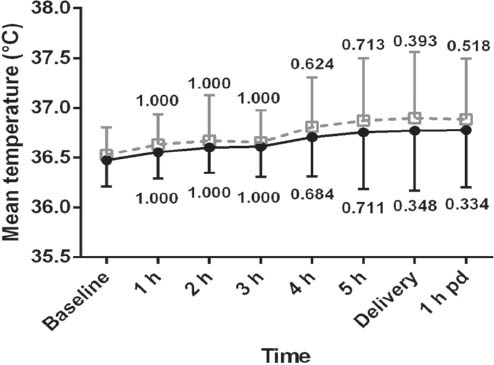
Maternal mean temperatures in RIB (black solid line) or CI group (grey dotted line) over time. Error bars are mean and standard deviation. Compared with baseline, p-values are presented at corresponding time point. RIB - regular intermittent bolus, CI - continuous infusion, pd - post delivery.
Figure 4.
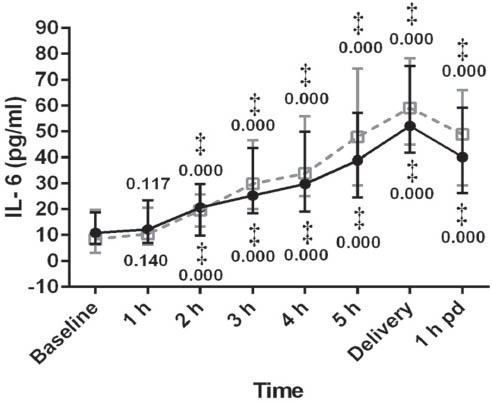
Maternal serum IL-6 levels in RIB (black solid line) or CI group (grey dotted line) over time. Error bars are interquartile range. Compared with baseline, ‡p<0.001. P-values are presented at corresponding time point. RIB - regular intermittent bolus, CI - continuous infusion, pd - post delivery, IL-6 - interleukin-6
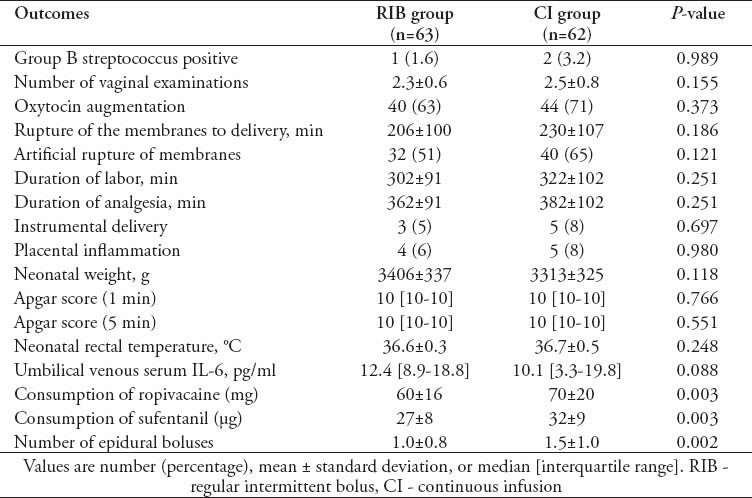
Table 4.
Obstetric, neonatal, and epidural outcomes among 125 subjects.
Discussion
The underlying mechanism of intrapartum maternal hyperthermia during epidural analgesia for labor remains undetermined. However, some studies found that corticosteroids inhibited epidural-associated maternal temperature elevation and reduced the rise of maternal/cord blood IL-6 levels.19,20 The dominant view of epidural-associated hyperthermia rests on maternal inflammation (elevated levels of maternal serum and cord blood IL-6).7 Our study demonstrated that maternal mean temperature increased after initiation of epidural analgesia in both groups despite no significant difference, and was accompanied by a rise in maternal serum IL-6 concentrations, which is similar to a previous study.14 We did not find any difference in neonatal rectal temperature and umbilical venous serum IL-6 between the groups. We compared maternal mean temperature and serum IL-6 hourly following epidural analgesia initiation, and found that IL-6, a marker of the acute inflammation response, more significantly than mean temperature did. Taking into account normal umbilical cord blood gases analyses, we suggest that an increase of maternal serum IL-6 is associated with physical stress and noninfectious inflammation, irrespective of the mode of epidural analgesia.8,21
In the present trial, we employed regular intermittent bolus epidural labor analgesia, which provided lower pain scores and fewer narcotics consumption compared with continuous infusion. This finding is in accordance with earlier observations in which intermittent epidural boluses reduced the incidence of breakthrough pain or local anesthetic consumption.9,12
We found no difference in the incidence of maternal fever between the 2 groups at any time point. This is not consistent with a similar study13 that showed intermittent epidural injections lead to a lower incidence of intrapartum fever in the first 4 hours post analgesia compared with continuous infusion. One reason for this may be due to the difference of bolus interval. Epidural analgesia restrains lower body sweating via blocking sympathetic nerves. In the previous study,13 intermittent boluses were injected at the patients’ request on average every 75 minutes, which was longer than our intervals by 15 minutes. The longer bolus interval perhaps allows more restoration of heat loss, thereby avoiding heat retention resulting from sympathetic blockade. By contrast, continuous epidural infusion continuously produces heat retention, which explains the higher maternal mean temperature compared with intermittent boluses, although no statistical difference was found. The other potential reasons include the differences in analgesic type and labor room temperature.
There is little evidence that intrapartum fever is attributed to placental infection in parturients who received epidural labor analgesia or not.8,22 The present study also showed that epidural-associated fever is not necessarily linked to placental inflammation. Despite the presence of clear contrary evidence that epidural-associated fever only developed in those with placental inflammation, still other risk factors (length of labor) are involved.23 Our present study investigated the association between regular intermittent bolus for epidural labor analgesia, which was the optimized method of epidural labor analgesia, and maternal temperature, and the results showed that it did not reduce the incidence of maternal fever when compared with continuous infusion. Although a negative result was indicated, this provides further understanding of the mechanism of intrapartum fever induced by different epidural injection methods, and provides implication for further research.
There are some limitations in our trial. Firstly, we did not use programmable infusion pumps because they were unobtainable, which provide more precise administration of drugs than manual administration. Secondly, sweating was not measured in our study, which may play an important role in fever. Finally, although we recorded maternal temperature from epidural until one hour postpartum, the subsequent temperature change was unknown.
In conclusion, regular intermittent bolus shows a similar incidence of maternal fever and better analgesia compared with continuous infusion during epidural labor analgesia. The epidural-related rise in maternal temperature could be attributed to noninfectious inflammation, such as IL-6 level elevation.
Footnotes
References
- 1.Sharma SK, Rogers BB, Alexander JM, McIntire DD, Leveno KJ. A randomized trial of the effects of antibiotic prophylaxis on epidural-related fever in labor. Anesth Analg. 2014;118:604–610. doi: 10.1213/ANE.0b013e3182a5d539. [DOI] [PubMed] [Google Scholar]
- 2.Greenwell EA, Wyshak G, Ringer SA, Johnson LC, Rivkin MJ, Lieberman E. Intrapartum temperature elevation, epidural use, and adverse outcome in term infants. Pediatrics. 2012;129:e447–e454. doi: 10.1542/peds.2010-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Osborne C, Ecker JL, Gauvreau K, Davidson KM, Lieberman E. Maternal temperature elevation and occiput posterior position at birth among low-risk women receiving epidural analgesia. J Midwifery Womens Health. 2011;56:446–451. doi: 10.1111/j.1542-2011.2010.00064.x. [DOI] [PubMed] [Google Scholar]
- 4.Agakidis C, Agakidou E, Philip Thomas S, Murthy P, John Lloyd D. Labor epidural analgesia is independent risk factor for neonatal pyrexia. J Matern Fetal Neonatal Med. 2011;24:1128–1132. doi: 10.3109/14767058.2010.545923. [DOI] [PubMed] [Google Scholar]
- 5.Wassen MM, Winkens B, Dorssers EM, Marcus MA, Moonen RM, Roumen FJ. Neonatal sepsis is mediated by maternal fever in labour epidural analgesia. J Obstet Gynaecol. 2014:1–5. doi: 10.3109/01443615.2014.925858. [DOI] [PubMed] [Google Scholar]
- 6.Yue HL, Shao LJ, Li J, Wang YN, Wang L, Han RQ. Effect of epidural analgesia with 0.075% ropivacaine versus 0.1% ropivacaine on the maternal temperature during labor: a randomized controlled study. Chin Med J (Engl) 2013;126:4301–4305. [PubMed] [Google Scholar]
- 7.Segal S. Labor epidural analgesia and maternal fever. Anesth Analg. 2010;111:1467–1475. doi: 10.1213/ANE.0b013e3181f713d4. [DOI] [PubMed] [Google Scholar]
- 8.Riley LE, Celi AC, Onderdonk AB, Roberts DJ, Johnson LC, Tsen LC, et al. Association of epidural-related fever and noninfectious inflammation in term labor. Obstet Gynecol. 2011;117:588–595. doi: 10.1097/AOG.0b013e31820b0503. [DOI] [PubMed] [Google Scholar]
- 9.Lim Y, Sia AT, Ocampo C. Automated regular boluses for epidural analgesia: a comparison with continuous infusion. Int J Obstet Anesth. 2005;14:305–309. doi: 10.1016/j.ijoa.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Fettes PD, Moore CS, Whiteside JB, McLeod GA, Wildsmith JA. Intermittent vs continuous administration of epidural ropivacaine with fentanyl for analgesia during labour. Br J Anaesth. 2006;97:359–364. doi: 10.1093/bja/ael157. [DOI] [PubMed] [Google Scholar]
- 11.Capogna G, Camorcia M, Stirparo S, Farcomeni A. Programmed intermittent epidural bolus versus continuous epidural infusion for labor analgesia: the effects on maternal motor function and labor outcome. A randomized double-blind study in nulliparous women. Anesth Analg. 2011;113:826–831. doi: 10.1213/ANE.0b013e31822827b8. [DOI] [PubMed] [Google Scholar]
- 12.Wong CA, Ratliff JT, Sullivan JT, Scavone BM, Toledo P, McCarthy RJ. A randomized comparison of programmed intermittent epidural bolus with continuous epidural infusion for labor analgesia. Anesth Analg. 2006;102:904–909. doi: 10.1213/01.ane.0000197778.57615.1a. [DOI] [PubMed] [Google Scholar]
- 13.Mantha VR, Vallejo MC, Ramesh V, Phelps AL, Ramanathan S. The incidence of maternal fever during labor is less with intermittent than with continuous epidural analgesia: a randomized controlled trial. Int J Obstet Anesth. 2008;17:123–129. doi: 10.1016/j.ijoa.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Mantha VR, Vallejo MC, Ramesh V, Jones BL, Ramanathan S. Maternal and cord serum cytokine changes with continuous and intermittent labor epidural analgesia: a randomized study. Scientific World Journal 2012. 2012 doi: 10.1100/2012/607938. 607938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salafia CM, Weigl C, Silberman L. The prevalence and distribution of acute placental inflammation in uncomplicated term pregnancies. Obstet Gynecol. 1989;73(3)(Pt 1):383–389. [PubMed] [Google Scholar]
- 16.Philip J, Alexander JM, Sharma SK, Leveno KJ, McIntire DD, Wiley J. Epidural analgesia during labor and maternal fever. Anesthesiology. 1999;90:1271–1275. doi: 10.1097/00000542-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Ramin SM, Gambling DR, Lucas MJ, Sharma SK, Sidawi JE, Leveno KJ. Randomized trial of epidural versus intravenous analgesia during labor. Obstet Gynecol. 1995;86:783–789. doi: 10.1016/0029-7844(95)00269-w. [DOI] [PubMed] [Google Scholar]
- 18.Sharma SK, Alexander JM, Messick G, Bloom SL, McIntire DD, Wiley J, et al. Cesarean delivery: a randomized trial of epidural analgesia versus intravenous meperidine analgesia during labor in nulliparous women. Anesthesiology. 2002;96:546–551. doi: 10.1097/00000542-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Wang LZ, Hu XX, Liu X, Qian P, Ge JM, Tang BL. Influence of epidural dexamethasone on maternal temperature and serum cytokine concentration after labor epidural analgesia. Int J Gynaecol Obstet. 2011;113:40–43. doi: 10.1016/j.ijgo.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 20.Goetzl L, Zighelboim I, Badell M, Rivers J, Mastrangèlo MA, Tweardy D, et al. Maternal corticosteroids to prevent intrauterine exposure to hyperthermia and inflammation: a randomized, double-blind, placebo-controlled trial. Am J Obstet Gynecol. 2006;195:1031–1037. doi: 10.1016/j.ajog.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 21.De Jongh RF, Bosmans EP, Puylaert MJ, Ombelet WU, Vandeput HJ, Berghmans RA. The influence of anaesthetic techniques and type of delivery on peripartum serum interleukin-6 concentrations. Acta Anaesthesiol Scand. 1997;41:853–860. doi: 10.1111/j.1399-6576.1997.tb04800.x. [DOI] [PubMed] [Google Scholar]
- 22.Evron S, Parameswaran R, Zipori D, Ezri T, Sadan O, Koren R. Activin betaA in term placenta and its correlation with placental inflammation in parturients having epidural or systemic meperidine analgesia: a randomized study. J Clin Anesth. 2007;19:168–174. doi: 10.1016/j.jclinane.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 23.Dashe JS, Rogers BB, McIntire DD, Leveno KJ. Epidural analgesia and intrapartum fever: placental findings. Obstet Gynecol. 1999;93:341–344. doi: 10.1016/s0029-7844(98)00415-3. [DOI] [PubMed] [Google Scholar]


