Abstract
Objectives:
To determine the reference values of arterial stiffness indices, particularly augmentation index (AIx) and pulse wave velocity (PWV) using applanation tonometry in a healthy Omani Arab population.
Methods:
This prospective study was carried out in the Department of Clinical Physiology, Sultan Qaboos University Hospital, Muscat, Oman over a 2-year period from June 2011 to June 2013. The central AIx, aortic PWV (AoPWV), and central pulse pressure (CPP) were recorded from 120 healthy subjects recruited randomly from a normal population using a SphygmoCor device. The 2.5th and 97.5th percentiles were used to determine the reference ranges for men and women separately. Analyses were performed using univariate statistics.
Results:
The mean age of the cohort was 38 years for men, and 35 years for women, with the ages ranging from 20-53 years. The overall mean central AIx was 13±11%, and for AoPWV was 6.7±1.6 m/s. The central AIx was higher in women (17 versus 10%; p<0.001), whereas the AoPWV was higher in men (7.1 versus 6.3 m/s; p=0.003). Subjects were categorized according to the gender and age decade, and reference values for CPP, central AIx, and AoPWV were obtained.
Conclusion:
This study reports the reference values for arterial stiffness indices from an Omani Arab population; the results of which should be interpreted in the context of its limitations.
Cardiovascular disease is the leading cause of mortality and morbidity worldwide.1 High central pulse pressure (CPP) and increased aortic pulse wave velocity (AoPWV) resulting from stiffness of large arteries have been recognized as an independent risk factor for cardiovascular disease.2-5 The European Hypertension Society guidelines recommended the pulse wave velocity (PWV) to be used for risk assessment stratification of hypertensive patients.6 Several non-invasive techniques have been developed to assess arterial stiffness parameters.7,8 Applanation tonometry developed by O’Rourke and other investigators9-12 is a simple, reproducible, and validated method used to assess arterial stiffness indices in healthy subjects and in subjects with various cardiovascular diseases. In addition to direct analysis of peripheral pulse wave forms to determine peripheral augmentation indices, this method can also be used to calculate central (aortic) augmentation indices and central blood pressure by using validated algorithms.12 A large number of studies from different European populations, African, and Asian nations have assessed reference ranges and correlates of arterial stiffness using applanation tonometry.13-16 However, studies on reference values of arterial stiffness in Arab populations are scant. Considering variations in genetic and environmental factors between populations, differences in arterial stiffness values in health and cardiovascular disease individuals are expected. There is a lack of previous studies on normal arterial stiffness indices in an Omani Arab population. Normal reference values from healthy subjects are particularly pertinent for proper clinical applications. Therefore, this study aimed to determine the reference values of arterial stiffness indices particularly augmentation index (AIx) and PWV using applanation tonometry in a healthy Omani Arab population.
Methods
This prospective study was carried out in the Department of Clinical Physiology, Sultan Qaboos University Hospital, Muscat, Oman over a 2-year period from June 2011 to June 2013. Participants were recruited from staff and students at Sultan Qaboos University (SQU), Muscat, Oman. Staff and students of SQU are from throughout the country and represent a good random mix of the general population. E-mails were sent to the randomly selected subjects inviting them to participate in the study. Subjects were then invited to the Department of Clinical Physiology at SQU hospital. A verbally read and explained written consent was signed by each participant. A full medical history was obtained from all consenting subjects. Subjects who reported having hypertension, diabetes mellitus, hyperlipidemia, previous or concomitant cardiovascular disease, smokers, or on any medications that have been reported previously to influence pulse wave analysis or velocity were excluded from the study. A total number of 150 subjects were interviewed and 30 subjects (20%) who met the exclusion criteria were removed. Subjects were advised to refrain from coffee intake for at least 5 hours before the examination on the day of appointment.
The study was approved by the Medical Research Committee in the College of Medicine and Health Sciences, SQU. The study was conducted according to the principles of the Helsinki Declaration.
Height (to the nearest 2 cm) and weight (to the nearest 0.5 kg) were measured with the participant wearing light clothes and no shoes. Body mass index (BMI) was calculated as weight in kilograms divided by the height in meter square. Brachial blood pressure measurements were recorded according to the recommendation of the European Society of Hypertension.6 After 5 minutes rest in a sitting position, 2 brachial blood pressure measurements were recorded. If the difference between the 2 measurements was more than 5 mm Hg, a third reading was obtained and the average of the closest 2 readings was used for the analysis. All measurements were obtained in a quiet room after the participant had rested for at least 15 minutes in the supine position. Pulse wave analysis and velocity were measured in accordance with the recommendations of the European consensus.7,8
A high-fidelity SPC-301 micromanometer (Millar Instrument, Inc., Houston, TX, USA) interfaced with a laptop computer equipped with the SphygmoCor software (AtCor Medical Pty, New South Wales, Australia) was used to record radial waveform from the dominant arm. Recordings were performed for 8 seconds and any recordings with systolic or diastolic variability of consecutive waveforms exceeding 5%, or if the amplitude of the pulse wave signal was <80 mV were discarded. Central (aortic) pulse waves were then generated by the SphygmoCor software using a generalized transfer function. The AoAIx was used in the analysis and it was defined as the difference between the second and the first systolic peak given as a percentage of the aortic pulse pressure. Blood pressure measurements recorded immediately before the recordings were used to calibrate the pulse wave. The AoPWV was measured by sequential recording of the arterial pressure waveform at the carotid and femoral arteries. Distances from the suprasternal notch to the carotid recording site (distance A), and from the suprasternal notch to the femoral artery site (distance B) were measured. Subtraction distance (distance B minus distance A) was used for AoPWV calculation. The intersecting tangent algorithm was used to detect “the foot” of the analyzed wave. Three PWV measurements were taken for each participant, and the closest 2 readings were used for analysis. All studies were performed by 2 observers. The intra and inter-observer coefficient of variations were 2.85 and 4.6, for central AIx, and 3.7 and 6.2 for AoPWV.
Statistical analyses were performed using version 12.1 of Stata, (StataCorp, College Station, TX, USA). Descriptive statistics were used to describe the data. For categorical variables, frequencies and percentages were reported. For continuous variables, mean and standard deviation, as well as median, and 2.5th and 97.5th percentiles were presented. Differences between groups were analyzed using Student's t-tests. An a priori was set at 0.05.
Results
Characteristics of the participants
Table 1 represents the characteristics of participants by gender. Men (51%) were older than women (p=0.021), they were taller and heavier, but there was no statistical significant difference in body mass index (p>0.05). Both peripheral and central blood pressures except CPP were higher in men (p<0.01 for all). The average central AIx for all participants was 13±11%, and the average aortic PWV was 6.7±1.6 m/s. Central AIx was higher in women (17 verus 10%; p<0.001), whereas AoPWV was higher in men (7.1 versus 6.3 m/s; p=0.003).
Table 1.
Baseline demographic and clinical characteristics (N=120).

Hemodynamic measurements
Table 2 shows detailed statistics for CPP, corrected AIx and PWV stratified by gender and age. Taking the 2.5th and 97.5th percentiles, the table provides the reference ranges for each category for the respective age and gender. For all age categories, men had higher AoPWV and lower central AIx.
Table 2.
Central pulse pressure, corrected augmentation index and pulse wave velocity stratified by gender and age categories (N=120).
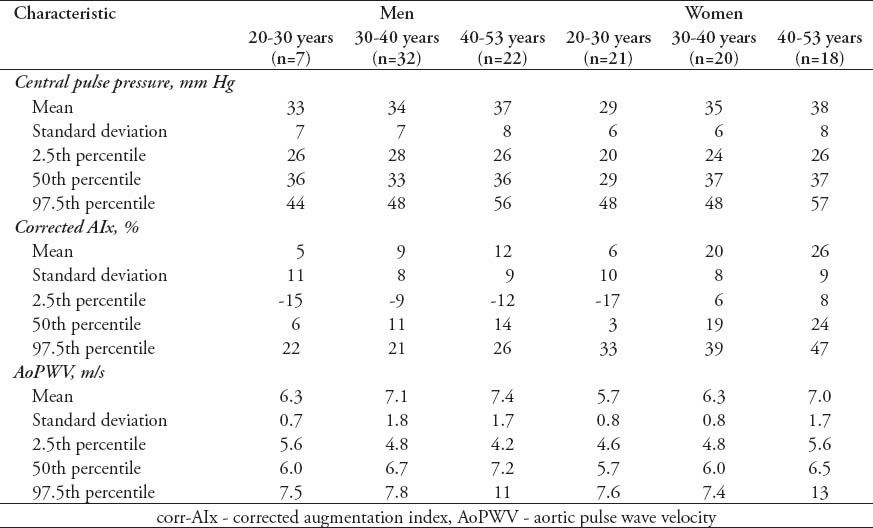
Figures 1-3 demonstrate the relationship of CPP, central AIx and PWV with age in men and women. There was a significant increase in all parameters with an increase in age for men and women. The increase in CPP and central AIx was steeper in women than in men.
Figure 1.

Central pulse pressure against age stratified by gender. The upper and the lower dash lines represent the 2.5th and 97.5th percentile.
Figure 3.
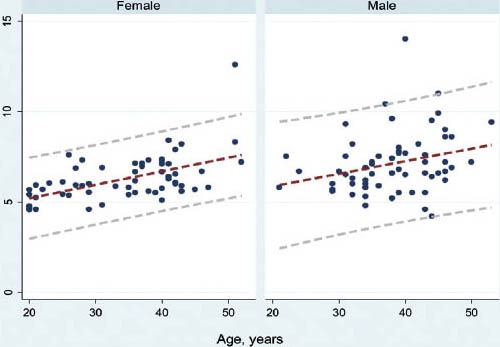
Aortic pulse wav velocity against age stratified by gender. The upper and the lower dash lines represent the 2.5th and 97.5th percentile.
Figure 2.

Corrected augmentation index against age stratified by gender. The upper and the lower dash lines represent the 2.5th and 97.5th percentile
Proposal for diagnostic thresholds
To determine the diagnostic threshold for men and women, the 97.5th percentile at the age of 30 years was used (Figures 1-3). The proposed thresholds from this procedure were as follow; 45 mm Hg for CPP for both men and women, 30% for men and 25% for women for central AIx, and 8 m/s for men and 7 m/s for women for AoPWV. To account for the changes in these parameters with age, these thresholds would need to be adjusted by approximately 3 mm Hg for CPP, 5% for central AIx, and 1 m/s for AoPWV for each decade that age differs from 30 years.
Discussion
In the present study, we determined the reference values and estimated the diagnostic thresholds for arterial stiffness indices in a sample of Omanis. Similar to results from previous studies on different populations, our study also showed a significant increase in CPP, central AIx, and AoPWV with increasing age in men and women. The increase of central AIx and AoPWV with age was more pronounced in women. Therefore, different diagnostic thresholds for these indices were proposed for men and women. Wojciechowska et al,14 reported reference values and the estimated diagnostic thresholds for a white European population from 3 European countries.14 They proposed the following thresholds for subjects at age of 30 years; 38 mm Hg for CPP for both men and women, and 22% for men and 29% for women for central AIx, with a suggestion to adjust the thresholds according to changes with age.14 Our thresholds were slightly higher for CPP and for women's central AIx. In another study of South African subjects,16 the proposed thresholds were 50 mm Hg for CPP, and 40% for central AIx for men and women which are higher than our study and in white Europeans of similar age groups. As the mean age in our study was similar to these 2 studies,14,16 our thresholds were closer to the thresholds of white Europeans than those of black South Africans. In the Framingham Heart Study Offspring Cohort, Wojciechowska et al14 calculated the carotid AIx for healthy subjects with a mean age of 57 years. They estimated thresholds of 33% for men and 37% for women. However, direct comparison of this study with ours is limited due to the differences in age, which is a known factor that affects the AIx.
Carotid to femoral PWV is considered the gold standard method for arterial stiffness assessment. Several studies in various populations have reported that an increase in PWV is an independent risk factor for cardiovascular disease.2,5 Pulse wave velocity was also recommended in risk assessment for hypertensive patients.6 In the current study, we are reporting reference values for PWV using a SpygmoCor device. We used the subtraction method to calculate the distance for PWV assessment. A recent invasive study showed that the subtracted distance gave the closest PWV to the value measured using the catheter withdrawal from the ascending aorta to the aortic bifurcation.17 Studies using MRI to measure PWV also supported the use of subtracted distance.18 In the article “The reference values for the arterial stiffness collaboration”14 the investigators reported the reference values for PWV from different techniques used to measure PWV. Some of the studies included in this article used the applanation tonometry by SphygmoCor. However, all data included in this study was from centers in the European countries.14 A more recent study also reported reference levels from a Uruguayan population.15 In comparison to this study, the proposed thresholds for AoPWV at age of 30 in our study (8 m/s for men and 7 m/s for women) were lower. Their threshold was approximately 10 m/s. The threshold for AoPWV in our study was closer to the thresholds published for the European populations.14 Similar thresholds to the current study were also reported from the South African population.16
Study limitations
The results of our study should be interpreted within the context of its limitation. The sample size in the current study was relatively small, and the number of subjects aged 50-60 years was also small. However, all subjects in our study were healthy non-smokers and non-alcoholics with no cardiovascular risk factors. The results of this study should not be extrapolated beyond this age, and further studies need to be conducted to estimate the reference values and thresholds for older age groups. Although the selected population in the study was a good representative of the general Omani population, selection bias could not be excluded and randomized stratified selection would have been more appropriate. The thresholds proposed in this study should be considered as preliminary thresholds for diagnoses of increased arterial stiffness indices. Validation for their use should be confirmed in prospective outcome studies including subjects with different risk factors for cardiovascular disease.
In conclusion, age and gender related reference values for central AIx, Ao PWV and central pulse pressure were obtained for healthy Omani subjects. This is an important step in order to apply these indices clinically for example, in the risk stratification of hypertensive patients and their management as recommended in the European Hypertension Society guidelines and for further research. The diagnostic thresholds for men and women at different age were also estimated. However, the values obtained in this study should be validated in prospective outcome studies including subjects with different risk factors for cardiovascular disease.
Footnotes
Disclosure.
Copyright.
Whenever a manuscript contains material (tables, figures, etc.) which is protected by copyright (previously published), it is the obligation of the author to obtain written permission from the holder of the copyright (usually the publisher) to reproduce the material in Saudi Medical Journal. This also applies if the material is the authors own work. Please submit copies of the material from the source in which it was first published.
References
- 1.Geneva (CH): World Health Organization; [Accessed 2014 June 30]. World Health Organization. The top 10 causes of death (online database) Available at: http://www.who.int/mediacentre/factsheets/fs310/en . [Google Scholar]
- 2.Laurent S. Predictors of cardiovascular mortality and morbidity in hypertension. Curr Med Res Opin. 2005;21(Suppl 5):S7–S11. doi: 10.1185/030079905X56420. [DOI] [PubMed] [Google Scholar]
- 3.Baumann M, Wassertheurer S, Suttmann Y, Burkhardt K, Heemann U. Aortic pulse wave velocity predicts mortality in chronic kidney disease stages 2-4. J Hypertens. 2014;32:899–903. doi: 10.1097/HJH.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 4.Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113:664–670. doi: 10.1161/CIRCULATIONAHA.105.579342. [DOI] [PubMed] [Google Scholar]
- 5.Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113:657–663. doi: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 6.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–536. doi: 10.1093/eurheartj/ehm236. Epub 2007 Jun 11. [DOI] [PubMed] [Google Scholar]
- 7.Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254. Epub 2006 Sep 25. [DOI] [PubMed] [Google Scholar]
- 8.Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens. 2012;30:445–448. doi: 10.1097/HJH.0b013e32834fa8b0. [DOI] [PubMed] [Google Scholar]
- 9.Payne RA, Wilkinson IB, Webb DJ. Arterial stiffness and hypertension: emerging concepts. Hypertension. 2010;55:9–14. doi: 10.1161/HYPERTENSIONAHA.107.090464. [DOI] [PubMed] [Google Scholar]
- 10.McEniery CM, Spratt M, Munnery M, Yarnell J, Lowe GD, Rumley A, et al. An analysis of prospective risk factors for aortic stiffness in men: 20-year follow-up from the Caerphilly prospective study. Hypertension. 2010;56:36–43. doi: 10.1161/HYPERTENSIONAHA.110.150896. [DOI] [PubMed] [Google Scholar]
- 11.O’Rourke MF, Adji A. Noninvasive generation of aortic pressure from radial pressure waveform by applanation tonometry, brachial cuff calibration, and generalized transfer function. Am J Hypertens. 2014;27:143–145. doi: 10.1093/ajh/hpt226. [DOI] [PubMed] [Google Scholar]
- 12.Hirata K, Kawakami M, O’Rourke MF. Pulse wave analysis and pulse wave velocity: a review of blood pressure interpretation 100 years after. Korotkov Circ J. 2006;70:1231–1239. doi: 10.1253/circj.70.1231. [DOI] [PubMed] [Google Scholar]
- 13.Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J. 2010;31:2338–2350. doi: 10.1093/eurheartj/ehq165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wojciechowska W, Staessen JA, Nawrot T, Cwynar M, Seidlerová J, Stolarz K, et al. Reference values in white Europeans for the arterial pulse wave recorded by means of the SphygmoCor device. Hypertens Res. 2006;29:475–483. doi: 10.1291/hypres.29.475. [DOI] [PubMed] [Google Scholar]
- 15.Farro I, Bia D, Zócalo Y, Torrado J, Farro F, Florio L, et al. Pulse wave velocity as marker of preclinical arterial disease: Reference levels in a Uruguayan population considering wave detection algorithms, paths lengths, aging and blood pressure. Int J Hypertens 2012. 2012 doi: 10.1155/2012/169359. 169359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shiburi CP, Staessen JA, Maseko M, Wojciechowska W, Thijs L, Van Bortel LM, et al. Reference values for SphygmoCor measurements in South Africans of African ancestry. Am J Hypertens. 2006;19:40–46. doi: 10.1016/j.amjhyper.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Weber T, Ammer M, Rammer M, Adji A, O’Rourke MF, Wassertheurer S, et al. Noninvasive determination of carotid-femoral pulse wave velocity depends critically on assessment of travel distance: a comparison with invasive measurement. J Hypertens. 2009;27:1624–1630. doi: 10.1097/HJH.0b013e32832cb04e. [DOI] [PubMed] [Google Scholar]
- 18.Joly L, Perret-Guillaume C, Kearney-Schwartz A, Salvi P, Mandry D, Marie PY, et al. Pulse wave velocity assessment by external noninvasive devices and phase-contrast magnetic resonance imaging in the obese. Hypertension. 2009;54:421–426. doi: 10.1161/HYPERTENSIONAHA.109.133645. [DOI] [PubMed] [Google Scholar]


