Abstract
Objectives:
To evaluate the feasibility of a minimally invasive technique using a titanium expandable device to achieve anatomical restoration of vertebral compression fractures (VCF) of the thoracolumbar spine.
Methods:
This prospective study included 27 patients diagnosed with VCF (Magerl classification A.1.2, A.1.3, and A.3.1) of the thoracolumbar spine treated with percutaneous cement augmentation using the SpineJack® device. The study was conducted in Valladolid University Hospital, Valladolid, Spain from January to December 2012, with a minimum one-year follow up. Preoperative evaluation included visual analogue scale (VAS) for pain, and radiological assessment of the VCF using 3-dimensional computed tomography (3D-CT) scans for measurements of vertebral heights and angles. The patients were followed at 3, 6, and 12 months with clinical VAS and radiological assessments.
Results:
The procedure was performed in 27 patients with a mean age of 55.9 ± 17.3 years, 55.6% females. All patients underwent surgery within 6 weeks from time of injury. No procedure related complications occurred. Pain measured by VAS score decreased from 7.0 preoperatively to 3.2 within 24 hours, and remained 2.2 at 3 months, 2.1 at 6 months, and 1.5 at 12-months follow-up (p<0.05). Mean height restorations for the anterior was 3.56 mm, central was 2.49, and posterior vertebral was 1.28 mm, and maintained at 12-months follow-up (p=0.001).
Conclusion:
This new percutaneous technique for VCF has shown good clinical results in pain control and the possibility to reduce both vertebral kyphosis angles and fractured endplates seen in 3D-CT scans assessment method. Further studies are needed to confirm those results on larger cohorts with long-term follow up.
Vertebral compression fractures (VCF) represent a true concern in the aging population with 700,000 osteoporotic VCF reported each year in the United States.1 In 2005, 2 million osteoporotic fractures with a total cost of $17 billion were observed; the number of annual fractures and associated costs is predicted to rise by almost 50% by 2025.2 A recent epidemiological study from Saudi Arabia3 revealed a prevalence of 34% among Saudi population between the ages of 50-79 year of age, with increasing frequency among males. Functional disabilities including neurological deficits, chronic pain, acute and progressive deformation of the spine, changes of mood, and complete disturbance of the quality of life4-7 are some of the symptoms experienced by patients suffering from VCF. Several clinical and epidemiological studies have shown a correlation between vertebra deformation and clinical problems, such as post-traumatic kyphosis, which has been depicted as one of the most serious post-traumatic complications.8-10 Although pain reduction can be achieved with current treatments in the acute phase, more comprehensive solutions should take into account the anatomical restoration of the whole vertebral body geometry (cortical ring and endplates).11 Currently, there are 2 principle ways to reduce VCF: first by indirect action on the vertebral body using the ligamentotaxis effect by positioning the patient (conservative, or surgical treatment, for example, vertebroplasty or percutaneous instrumentation), and secondly by acting directly on the vertebra itself, by exerting direct forces onto the bone (balloon kyphoplasty). If the ligamentotaxis effect can efficiently reduce the cortical ring using the dynamic mobility of the VCF,12 this cannot have any effect on the central part of the endplates.13-15 First described by Galibert et al in 1987,16 vertebroplasty was also intended to reduce the vertebral fracture by correct positioning of the patient using the dynamic vertebral fracture mobility.17 Its principle was to stabilize a fractured vertebra in situ. Later on, percutaneous balloon kyphoplasty (BKP) attempted to allow surgeons to act directly on the vertebral body using inflatable bone tamps. However, the reduction obtained using the bone tamps cannot be maintained after deflation during cement injection,18 and the inflatable bone tamp tends to follow the path of least resistances, which might not be consistent with the reduction direction. Beside, treatment results from BKP are depending on the fact if there is a fresh fracture that can be reduced or not, and the height reduction relies on the fact that only fresh, or mobile fractures can be reduced. While those treatments are able to efficiently reduce pain and improve the quality of life1,19-25 there is no evidence of endplate reduction using only ligamentotaxis or balloon effects. Additionally different patterns of injury and healing of the discs may be responsible for complications arising after incomplete treatment.26 Moreover, as depicted by Wang et al,27 there is a need for traumatic vertebral kyphosis angle reduction to avoid the occurrence of late kyphosis. Height restoration and vertebral kyphosis angle reduction have already been described as beneficial for pulmonary diseases3,7,28 mortality risks reduction,29-32 weight loss avoidance,33 and urinary infection prevention.34 Endplate anatomical restoration shall enhance those clinical outcomes by avoiding chronic pain resulting from a biomechanical unfavorable situation. The aim of this work is to determine whether a surgical procedure involving a new technique can provide an anatomical restoration of the fractured vertebra including cortical ring reduction, as well as, endplate anatomical restoration. Thus, the purpose of this prospective study was not only to assess the ability of a new treatment to achieve the anatomical restoration of the vertebral body prior to its stabilization using polymethylmethacrylate (PMMA) injection, but secondly to assess the efficacy of this method to achieve immediate and sustained pain relief, and finally to develop a method for 3D evaluation of the achieved reduction.
Methods
Study population
The study included adult patients (over 18 years) presenting with VCF of the thoracolumbar spine. This 2-year study was conducted between January and December 2012 in the University Hospital Valladolid, Valladolid, Spain. Inclusion criteria were persistent back pain due to VCF for 6 weeks (mobility was confirmed with MRI in those cases needed), and body mass index (BMI) of 30 and less. Following fracture types according to the Magerl classification were included: A1.2, A1.3, and A3.1. Patients were included regardless of the present history of trauma, or osteoporosis. Exclusion criteria were history of pain for more than 6 weeks, VCF of Magerl type more than A3.1, presence of neurological deficit, or pathological (related to metastatic or hematological disease) VCF. Detailed demographics were collected including age, gender, and history of trauma. Clinical evaluation included neurological examination and assessments of pain using visual analogue scale (VAS) at admission, and at 3, 6, and 12 months follow up. Evaluation of the fracture type was performed with plain x-rays, CT, and 3D-CT, and magnetic resonance imaging (MRI) studies before the procedure, and at 3, 6, and 12 months follow up. Bone mineral density (BMD) was measured using DEXA (dual energy X-ray absorptiometry) scan for included patients, and the World Health Organization classification of T-scores for osteoporosis of less than -2.5 was used. Each patient signed an informed consent approved by the institutional review board.
Research design
The study was a prospective, single arm, post-procedure observational study targeted patient with VCF who underwent percutaneous kyphoplasty to examine the efficacy of the implant in achieving and maintaining clinical improvement of pain and radiological restoration of VCF heights.
Assessment of the anatomical restoration
Since there is currently no unanimous method for reporting vertebral height restoration for vertebral fractures after vertebroplasty, and because reporting methods may result in substantial variability, there is a need to define a new method, which can be used to assess the 3D anatomical restoration achieved by this new treatment.16,34,35 The method has been developed in collaboration with a biomechanics laboratory (Paris, France) to quantify the anatomical restoration. Using axial 1 mm slices from CT scan examinations, 3D reconstructions were obtained by segmentation technique. This method has been previously validated,36-39 and was further developed to allow for a 3D comparison between 2 3D vertebral reconstructions. The 2 3D reconstructions are obtained for the same vertebra, preoperatively, and postoperatively; they are superimposed using the fact that the posterior arch is not affected, either by the VCF or the procedure itself. Then, the 2 3D reconstructions are compared by calculating the distance in between the 2 surfaces of any point belonging to the surface of the vertebral body. These calculations can be efficiently presented using color-coded 3D mappings where the calculated distance is represented for any point by a specific color depending on the measured value (Figure 1). The accuracy of these measurements depends on the CT scan cuts thickness. In our application, each 3D reconstruction was obtained using 1-2 mm cuts. Thus, each 3D reconstruction was obtained within an accuracy of +/- 1 mm. These 3D reconstructions enable also to quantify the vertebral angular changes between the endplates without any bias usually met with techniques involving bi-planar projection of a 3D object. Thus, based on the 3D reconstruction, the local sagittal vertebral kyphosis angle was determined using the projection of the 2 vertebral endplates in the sagittal plane (Figure 2).
Figure 1.
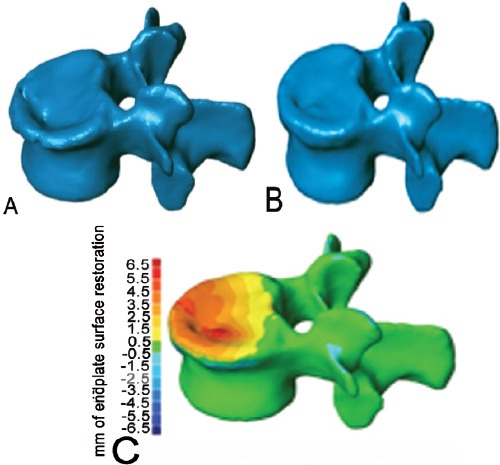
An image showing: 3D computerized CT reconstruction of vertebral compression fractures before (A),and after (B) kyphoplasty with good restoration, and 3D topography reconstruction (C) demonstrates maximum restoration of height (red).
Figure 2.
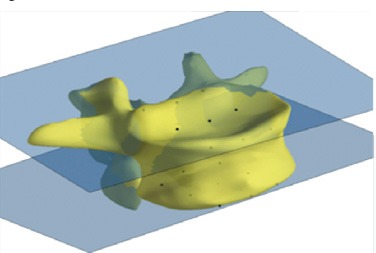
A 3D computerized calculation of the kyphotic angle. The least-squares plane through these points is used to compute the angular orientation of the endplates. The angle measured is the difference between upper and lower vertebral endplates.
Surgical technique
We used a new, minimally invasive procedure using innovative, intravertebral, cranio-caudal expandable titanium implants (SpineJack®, Vexim SA, Balma, France) in order to achieve the anatomical reduction of vertebral compression fractures prior to their stabilization using acrylic cement. The procedure consists of a 2-fold treatment involving a reduction step and a stabilization step. To allow for optimal control of the procedure, the whole surgical intervention is performed under general anesthesia in the operating room with controlled fluoroscopic guidance.
First step
Reduction
Two intravertebral, permanent, cranio-caudal expandable implants made of titanium alloy are placed, in their closed position, in the vertebral body via a transpedicular approach (Figure 3). Optimal placement of the implants according to the reduction strategy can be achieved since they expand in only one direction. By controlling the positioning, the possibility to reduce the fracture based on the preoperative imaging assessments can be carried out. Then, using the instrumentation, one can choose all the positioning parameters for the implant to reduce the fractured vertebral body (antero-posterior placement, height in the vertebral body, and angulation with respect to the broken endplate). Once the fracture has been reduced by the 2 implant’s expansions, the following step consists of stabilizing the reduction to keep the achieved correction while letting the 2 implants in place to keep the correction.
Figure 3.
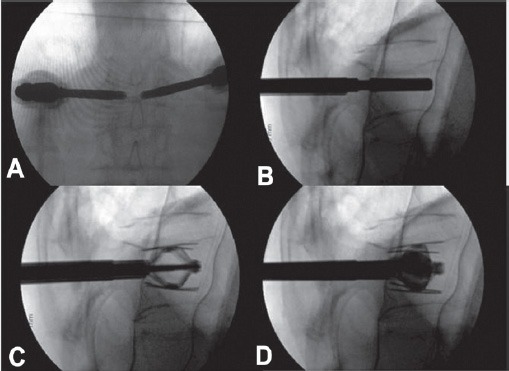
Intraoperative radiographs demonstrating the main steps of the technique. The anterior-posterior (A) and lateral (B) view demonstrate bilateral percutaneous transpedicular placement of the implant. The implant is expanded (C) and after adequate restoration, the cement is injected under fluoroscopic monitoring.
Second step
Stabilization
The stabilization is realized using high viscosity PMMA (Cohesion® Bone Cement, Vexim, Balma, France) injected into the 2 implants through the instrumentation. During the expansion of the implant, multiple windows of trabecular bone become reachable through the implant deployment surface, allowing for ideal cement inter-digitation and, therefore, an optimal mechanical stabilization of the fracture reduction (Figure 4).
Figure 4.
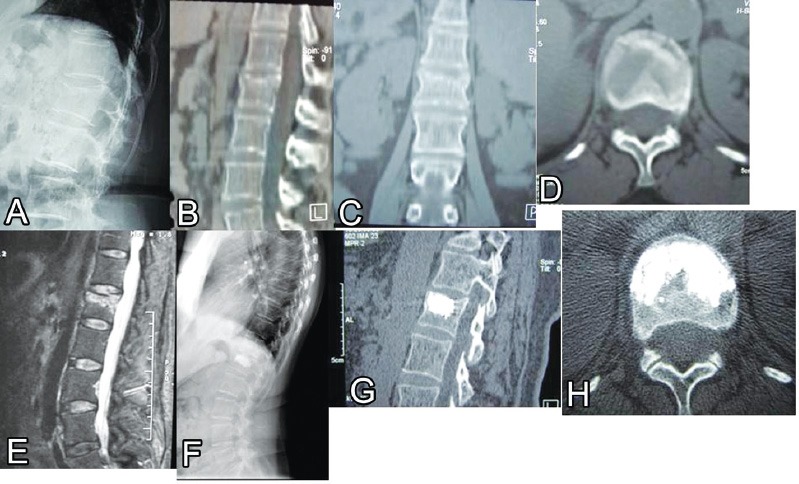
A case illustration of a 42-year-old male presented after a trivial fall with severe lower back pain and normal neurological exam (visual analogue scale 9). Lateral radiograph (A) demonstrated vertebral compression fractures (VCF) (type A1.3). Sagittal B), coronal C), and axial D) CT scans demonstrate fracture of the upper endplate and kyphotic deformity. A T2-WI sagittal MRI scan E) demonstrated high signal intensity (edema) at the fracture site. One-year follow up lateral radiograph F) showing adequate fusion of the VCF was demonstrated on sagittal G) and axial H) CT scans.
Statistical analysis
The normalities of the distributions of the parameters were first analyzed with Shapiro-Wilk tests. All quantitative parameters are described with averages and standard deviations, and the qualitative values are described as frequency distributions. Pearson chi-squared tests were used to evaluate the associations between qualitative parameters. Comparisons of pain evolution between the pre- and postoperative check-ups were performed with t-tests. Friedman test was used to assess changes in pain along the clinical controls and were performed along the period of study. T-student or U de Mann-Whitney were used to compare independent groups, and for correlated groups a T-student or Wilcoxon test was performed whether they followed or not a normal distribution. All data were analyzed with the Statistical Package for Social Sciences version 20. A p<0.05 was considered statistically significant.
Results
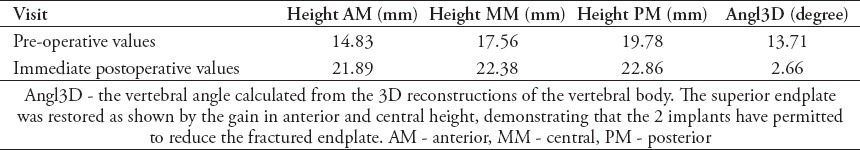
Patient characteristics are summarized in Table 1. The VCF distribution by location was as follows: 2 cases (7.4%) in the T10 level, 4 cases (14.8%) at T12, 13 patients (48.1%) at L1, 6 cases (22.2%) level L2, and 2 patients (7.4%) at L4 level (Figure 5). There was no significant difference in the distribution by levels according to gender and age groups (p=0.347). From the etiological point of view, in 19 cases (70.4%), fractures were the result of low energy trauma with no significant differences according to age distribution. In the group under 55 years, 9 cases had history of trauma, which represents 90% of the cases of this group, and the group of greater than or equal to 55 years are 10 patients who have had a history of trauma, which is 58.8% of patients in that age group. In 19 cases (70.4%), there was osteoporosis, although, in this case the distribution between the 2 age groups presented statistically significant differences (p=0.001) and 16 of the 19 cases belongs to an older age group (Table 2). There was a statistically significance (p<0.05) immediate and long lasting reduction of pain as a result of the procedure (Table 3). The mean VAS preoperatively was 7.0 (range, 6.0-7.4), and was reduced to a mean of 3.2 (range, 3.1-3.4) 24 hours postoperatively. The mean VAS was of 2.2, 2.1, and 1.5 at 3, 6, and 12 months follow-up after the intervention. The mean values show increased postoperative vertebral height compared to pre-intervention values in all 9 measured areas; these increases are statistically significant in all cases (p<0.001) (Table 4). The height preoperative values of vertebral height losses occur in the same statistically significant (p<0.001) relation to the height of the adjacent vertebrae, and could be considered as a reference of the normal anatomy of the patient. The mean values for postoperative vertebral height compared to adjacent vertebrae values are presented for all 9 points in Table 5. The postoperative values differ with respect to the average values of the adjacent vertebra, this difference being statistically lower than the preoperative values. These values show statistically significant differences (p<0.05) in the central areas and former endplate. The sagittal alignment was studied using a comparative analyze of the 3D angle between the preoperative and the postoperative situation. The kyphotic angle was reduced from a mean 12°, 13,° to 5.50,° the difference being statistically significant (p <0,001) (Table 6). Related to the effect of titanium plus cement on the development of adjacent fractures, 2 adjacent fractures (7.4%) at T8 and T10 occurred throughout the follow up, which is a lowered incidence compared to the literature1,3 cement leakage appeared in 5 cases (18.4%), being located all of them into the paravertebral soft tissues without any clinical relevance.
Table 1.
Characteristics of patients included in this study.
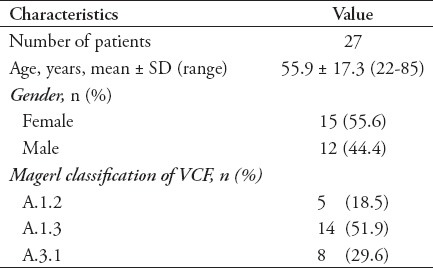
Figure 5.
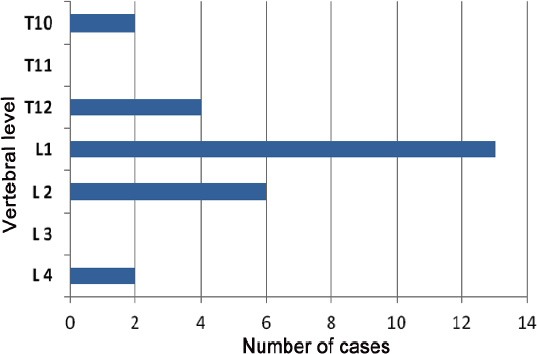
Data distribution according to the location of vertebral compression fractures in the thoracolumbar spine.
Table 2.
Case distribution between the 2 age groups included in this study on the average age and body mass index in osteoporotic and non-osteoporotic vertebral fracture.
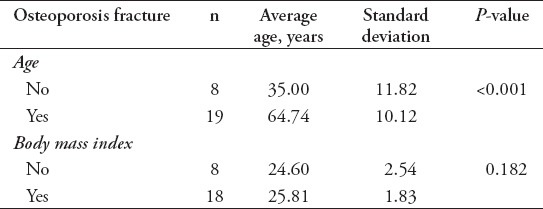
Table 3.
Evolution of visual analogue scale (VAS) value as found in this study.
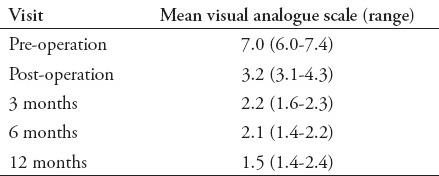
Table 4.
Comparison of mean pre- and post-operative vertebral height measurements.
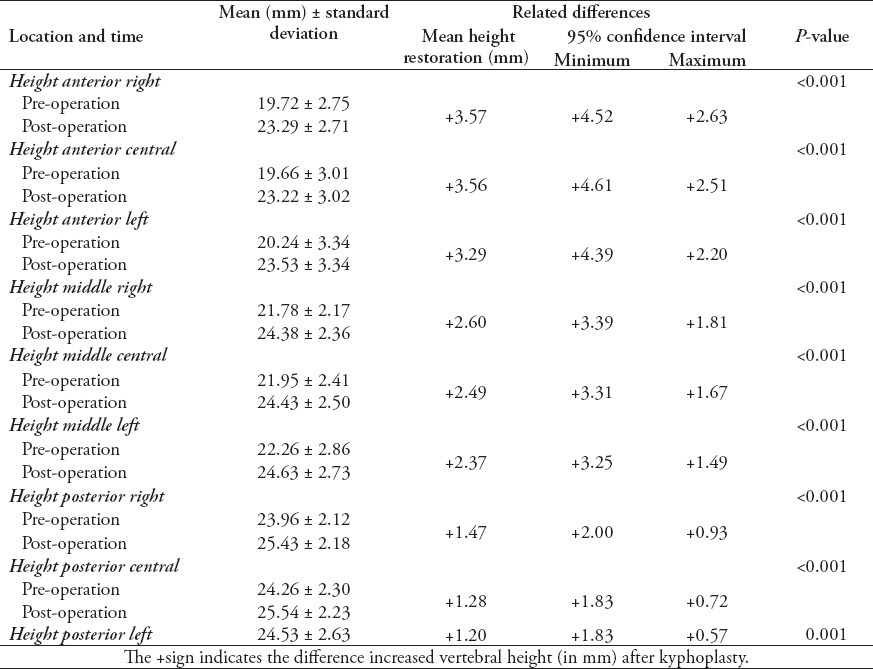
Table 5.
Comparison of mean vertebral height of adjacent vertebra cranial to the fractured versus fractured vertebra post-kyphoplasty.
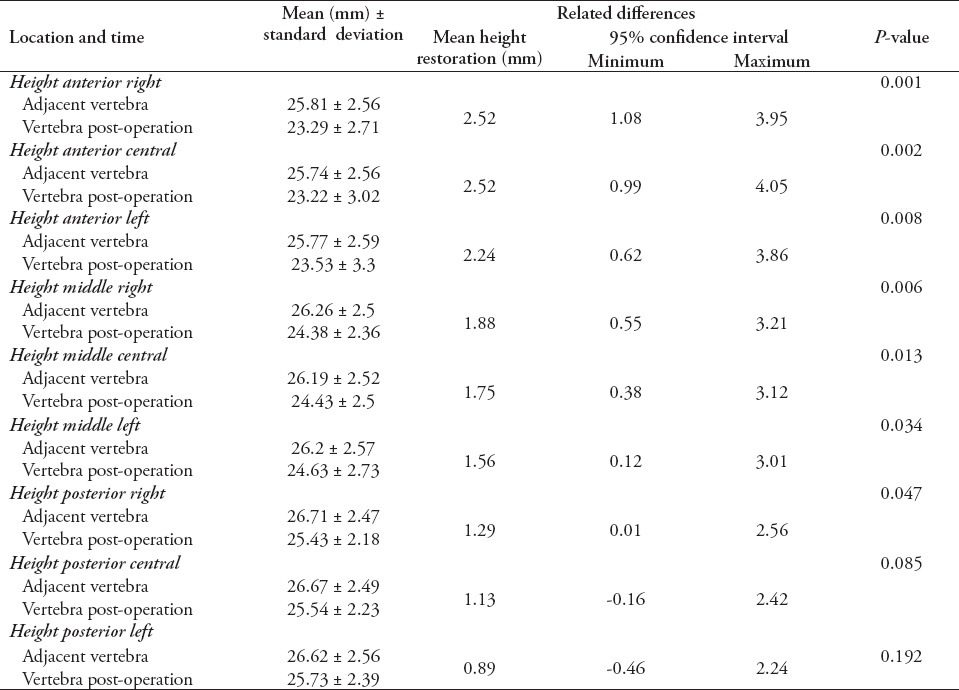
Table 6.
Pre- and post-operative anterior, central, and posterior vertebral height and angle measurements (p<0.05).
Discussion
Historically, surgical treatment for VCF was limited to aggressive open stabilization procedures.40 However, this was often associated with multiple medical comorbidities, and in some cases the age of the patients was limiting. More recently, 2 percutaneous treatments have been introduced for VCF.41 Vertebroplasty is a percutaneous injection of viscous PMMA into the vertebral body, and was first described by Galibert et al16 in 1987. With kyphoplasty, a balloon is percutaneously inserted into the fractured vertebral body and inflated to create a cavity. The balloon is then deflated and removed, and PMMA is injected. These 2 recent techniques are well-established procedures for VCF treatments; their effectiveness has been widely documented for the treatment of acute, painful vertebral compression fractures, and with a significant improvement in the time of recovery compared to conservative treatment.25 Nevertheless, so far in the current literature1,21,42 there is no clear evidence claiming anatomical reduction of the VCF involving vertebral body height restoration, vertebral kyphosis reduction, as well as, endplate morphology restoration prior to its stabilization. Besides, none of these 2 percutaneous techniques is able to maintain the reduction forces while the cement is injected, and in some cases, with balloon kyphoplasty, some loss of reduction occurs.18
The results presented here are showing that the anatomical restoration of a vertebra after a VCF is possible providing that the device allows for a good control of the reductive actions in amount and direction. Thus, we have learned from the results that it is possible to reconstruct a depressed vertebral body in such a way that mobilization is not delayed, but this is an art that must be mastered and performed in a fully controlled manner, as well as, controlled the long term benefits and the effect on disc degeneration over time, like other load-bearing joints; tibial plateau fractures have 5.3 times risk to develop a posttraumatic arthrosis that needs total knee replacement.43 As Trickey44 said in the mid 1970’s for treatment of fractures of the calcaneus ‘there is nothing wrong with the idea; it is the execution that is at fault’. With this new concept of anatomical restoration taking into account the vertebral body as a whole, we try to go beyond the height restoration often claimed by the existing techniques and introduce the benefits, in the short-term follow-up, of the anatomical reduction of the vertebral body in VCF treatment. The improvement in the reduction should improve the existing long-term results.45 This is in accordance with what we already know regarding any of the joints in the human body, for which it is well known that a good anatomical restoration would resume in better functional and biomechanical results. Already described previously by Trickey,44 injuries with a poor prognosis are those for which a joint surface is distorted with consequent impairment of movement that can be painful. Improved joint function can be achieved by better reshaping of the joint surface. As the spine supports loads during everyday life and activities,46 vertebral joints injuries deserve to be treated on the same principles as any other injury of the weight-bearing joints; that is by biomechanical stable anatomical reduction to allow early mobilization, weight bearing, and thus a biomechanical restoration. As McKiernan11 wrote: “clinical intuition and classic biomechanical teaching suggests that the vertebral height restoration should matter clinically”, we are convinced that endplate restoration should be even more important. Rohlmann47 also found this while considering spinal loads after kyphoplasty in osteoporotic patients, and stated ‘advantages will be apparent only if nearly full fracture reduction is achieved’.
According to the 3D results between 90-95% of vertebral body reduction can be achieved and maintained within the first year, these type of analysis cannot be realized with simple x-rays.48 The clinical benefits are the reduction of the VAS score statistically significantly and stable during the first year, thus these results need to be confirmed in the long term follow-up. Conservative treatment for small defects is the standard treatment, though as described by Tzermiadiamos,49 the lack of reduction will influence an overload of the supradjacent vertebral body, and increase the risk of adjacent fractures.
In conclusion, we believe that this new procedure brings new opportunities for VCF treatment. Indeed, restoring the complete anatomy of the vertebra prior to stabilizing it will be correlated with improved clinical outcomes. Within this study, a new 3D evaluation method has been developed to assess the 3D effect of the procedure on the vertebral levels and enables us to demonstrate the feasibility of such an anatomical restoration of the fractured vertebral body thanks to this new procedure. Thus, clinicians’ expectations are met at one-year follow with respect to feasibility and control of the procedure, safety, and pain relief.
The limitations of this study are the rather small number of patients included, and the limited follow up period. Future studies will consist on one hand, of confirming those preliminary results using larger cohorts with longer follow-up periods or biomechanical testing to clearly demonstrate the advantages of this technique, and on the other hand, to further develop evaluation tools to enable objective quantification of reduction gesture in those procedures.
References
- 1.Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 2.Burge R, Dawson-Hudges B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 3.Sadat-Ali M, Al-Habdan IM, Al-Turki HA, Azam MQ. An epidemiological analysis of the incidence of osteoporosis and osteoporosis-related fractures among the Saudi Arabian population. Ann Saudi Med. 2012;32:637–641. doi: 10.5144/0256-4947.2012.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos. 1998;8:261–267. doi: 10.1007/s001980050063. [DOI] [PubMed] [Google Scholar]
- 5.Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1992;13:27–31. doi: 10.1016/8756-3282(92)90193-z. [DOI] [PubMed] [Google Scholar]
- 6.Hall SE, Criddle RA, Comito TL, Prince RL. A case-control study of quality of life and functional impairment in women with long-standing vertebral osteoporotic fracture. Osteoporosis Int. 1999;9:508–515. doi: 10.1007/s001980050178. [DOI] [PubMed] [Google Scholar]
- 7.Yang HL, Zhao L, Liu J, Sanford CG, Jr, Chen L, Tang T, et al. Changes of pulmonary function for patients with osteoporotic vertebral compression fractures after kyphoplasty. J Spinal Disord Tech. 2007;20:221–225. doi: 10.1097/01.bsd.0000211273.74238.0e. [DOI] [PubMed] [Google Scholar]
- 8.Malcolm BW, Bradford DS, Winter RB, Chou SN. Post-traumatic kyphosis. A review of forty-eight surgically treated patients. J Bone Joint Surg Am. 1981;63:891–899. [PubMed] [Google Scholar]
- 9.Oda I, Cunningham BW, Buckley RA, Goebel MJ, Haggerty CJ, Orbegoso CM, et al. Does spinal kyphotic deformity influences the biomechanical characteristics of the adjacent motion segments? An in-vivo animal model. Spine (Phila Pa 1976) 1999;24:2139–2146. doi: 10.1097/00007632-199910150-00014. [DOI] [PubMed] [Google Scholar]
- 10.Whitesides TE. Traumatic kyphosis of the thoracolumbar spine. Clin Orthop Relat Res. 1977;128:78–92. [PubMed] [Google Scholar]
- 11.McKiernan FE, Faciszewski T, Jensen R. Does vertebral height restoration achieved at vertebroplasty matter? J Vasc Interv Radiol. 2005;16:973–979. doi: 10.1097/01.RVI.0000163014.71889.16. [DOI] [PubMed] [Google Scholar]
- 12.McKiernan FE, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res. 2003;18:24–29. doi: 10.1359/jbmr.2003.18.1.24. [DOI] [PubMed] [Google Scholar]
- 13.Goh S, Tan C, Price RI, Edmondston SJ, Song S, Davis S, et al. Influence of age and gender on thoracic vertebral body shape and disc degeneration: an MR investigation of 169 cases. J Anat. 2000;197:647–657. doi: 10.1046/j.1469-7580.2000.19740647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller JA, Schmatz C, Schultz AB. Lumbar disc degeneration: correlation with age, sex and spine level in 600 autopsy specimens. Spine. 1988;13:173–178. [PubMed] [Google Scholar]
- 15.Ochia RS, Ching RP. Internal pressure measurements during burst fracture formation in human lumbar vertebrae. Spine. 2002;27:1160–1167. doi: 10.1097/00007632-200206010-00005. [DOI] [PubMed] [Google Scholar]
- 16.Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty] Neurochirurgie. 1987;33:166–168. French. [PubMed] [Google Scholar]
- 17.Faciszewski T, McKiernan FE. Calling all vertebral fractures, classification of vertebral compression fractures: a consensus for comparison of treatment and outcome. J Bone Miner Res. 2002;17:185–191. doi: 10.1359/jbmr.2002.17.2.185. [DOI] [PubMed] [Google Scholar]
- 18.Verlaan JJ, Van de Kraats EB, Oner FC, van Walsum T, Niessen WJ, Dhert WJ. The reduction of endplate fractures during balloon vertebroplasty: a detailed radiological analysis of the treatment of burst fractures using pedicle screws, balloon vertebroplasty, and calcium phosphate cement. Spine (Phila Pa 1976) 2005;30:1840–1845. doi: 10.1097/01.brs.0000173895.19334.e2. [DOI] [PubMed] [Google Scholar]
- 19.Khanna AJ, Reinhardt MK, Togawa D, Lieberman IH. Functional outcomes of kyphoplasty for the treatment of osteoporotic and osteolytic vertebral compression fractures. Osteoporosis Int. 2006;17:817–826. doi: 10.1007/s00198-006-0068-3. [DOI] [PubMed] [Google Scholar]
- 20.Diamond TH, Bryant C, Browne L, Clark WA. Clinical outcomes after acute osteoporotic vertebral fractures: a 2-year non-randomised trial comparing percutaneous vertebroplasty with conservative therapy. Med J Aust. 2006;184:113–117. doi: 10.5694/j.1326-5377.2006.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 21.Eck JC, Nachtingall D, Humphreys SC, Hodges SD. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008;8:488–497. doi: 10.1016/j.spinee.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Ledlie JT, Renfro MB. Kyphoplasty treatment of vertebral fractures: 2-year outcomes show sustained benefits. Spine (Phila Pa 1976) 2006;31:57–64. doi: 10.1097/01.brs.0000192687.07392.f1. [DOI] [PubMed] [Google Scholar]
- 23.Alvarez L, Alcaraz M, Pérez-Higueras A, Granizo JJ, de Miguel I, Rossi RE, et al. Percutaneous vertebroplasty: Functional improvement in patients with osteoporotic compression fractures. Spine (Phila Pa 1976) 2006;31:1113–1118. doi: 10.1097/01.brs.0000216487.97965.38. [DOI] [PubMed] [Google Scholar]
- 24.De Negri P, Tirri T, Paternoster GL, Modano P. Treatment of painful osteoporotic or traumatic vertebral compression fractures by percutaneous vertebral augmentation procedures: a nonrandomized comparison between vertebroplasty and kyphoplasty. Clin J Pain. 2007;23:425–430. doi: 10.1097/AJP.0b013e31805593be. [DOI] [PubMed] [Google Scholar]
- 25.Chen AT, Cohen DB, Skolasky RL. Impact of nonoperative treatment, vertebroplasty and kyphoplasty on survival and morbidity after vertebral compression fracture in the medicare population. J Bone Joint Surg Am. 2013;95:1729–1736. doi: 10.2106/JBJS.K.01649. [DOI] [PubMed] [Google Scholar]
- 26.Lin RM, Panjabi MM, Oxland TR. Functional radiographs of acute thoracolumbar burst fractures. A biomechanical study. Spine. 1993;18:2431–2437. doi: 10.1097/00007632-199312000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Wang XY, Dai LY, Xu HZ, Chi YL. Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures. J Neurosurg Spine. 2008;8:246–254. doi: 10.3171/SPI/2008/8/3/246. [DOI] [PubMed] [Google Scholar]
- 28.Lombardi Oliveira LM, Jr, Mayer AF, Jardim JR, Natour J. Evaluation of pulmonary function and quality of life in women with osteoporosis. Osteoporos Int. 2005;16:1247–1253. doi: 10.1007/s00198-005-1834-3. [DOI] [PubMed] [Google Scholar]
- 29.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:56–61. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 30.Center JR, Nguyen TV, Schneider D. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 31.Gold DT, Silverman SL. Cedars-Sinai Medical Center 2003. Los Angeles (CA): Remedica Communications, Inc; 2003. The downward spiral of vertebral osteoporosis: consequences (Monograph) [Google Scholar]
- 32.Bliuc D, Nguyen ND, Milch VE. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 33.Ryan PJ, Blake G, Herd R. A clinical profile of back pain and disability in patients with spinal osteoporosis. Bone. 1994;15:27–30. doi: 10.1016/8756-3282(94)90887-7. [DOI] [PubMed] [Google Scholar]
- 34.Popa RI, Gray LA, Kallmes DF. Urinary tract infections in the potential vertebroplasty patient: incidence, significance, and management. AJNR Am J Neuroradiol. 2009;30:227–231. doi: 10.3174/ajnr.A1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKiernan FE, Faciszewski T, Jensen R. Reporting height restoration in vertebral compression fracture. Spine. 2003;28:2517–2521. doi: 10.1097/01.BRS.0000092424.29886.C9. [DOI] [PubMed] [Google Scholar]
- 36.Nelson D, Peterson E, Tilley B, O’Fallon WM, Chao E, Riggs BL, et al. Measurement of vertebral area on spine x-rays in osteoporosis: Reliability of digitizing technique. J Bone Miner Res. 1990;5:707–716. doi: 10.1002/jbmr.5650050707. [DOI] [PubMed] [Google Scholar]
- 37.Aubin CE, Dansereau J, Parent F, Labelle H, de Guise JA. Morphometric evaluations of personalised 3D reconstructions and geometric models of the human spine. Med Biol Eng Comput. 1997;35:611–618. doi: 10.1007/BF02510968. [DOI] [PubMed] [Google Scholar]
- 38.Kim DO, Kim HJ, Jung H, Jeong HK, Hong SI, Kim KD. Quantitative evaluation of acquisition parameters in three-dimensional imaging with multidetector computed tomography using human skull phantom. J Digit Imaging. 2002;15(Suppl 1):254–257. doi: 10.1007/s10278-002-6002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DeVries NA, Gassman EE, Kallemeyn NA, Shivanna KH, Magnotta VA, Grosland NM. Validation of phalanx bone three-dimensional surface segmentation from computed tomography images using laser scanning. Skeletal Radiol. 2008;37:35–42. doi: 10.1007/s00256-007-0386-3. [DOI] [PubMed] [Google Scholar]
- 40.Mikles MR, Stchur RP, Graziano GP. Posterior instrumentation for thoracolumbar fractures. J Am Acad Orthop Surg. 2004;12:424–435. doi: 10.5435/00124635-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Deramond H, Saliou G, Aveillan M, Lehmann P, Vallée JN. Respective contributions of vertebroplasty and kyphoplasty to the management of osteoporotic vertebral fractures. Joint Bone Spine. 2006;73:610–613. doi: 10.1016/j.jbspin.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 42.Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures - A comparative systematic review of efficacy and safety. Spine. 2006;31:2747–2755. doi: 10.1097/01.brs.0000244639.71656.7d. [DOI] [PubMed] [Google Scholar]
- 43.Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am. 2014;96:144–150. doi: 10.2106/JBJS.L.01691. [DOI] [PubMed] [Google Scholar]
- 44.Trickey EL. Editorial: Treatment of fractures of the calcaneus. J Bone Joint Surg Br. 1975;57:411. [PubMed] [Google Scholar]
- 45.Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and non-operated vertebral fracture patients in the medicare population. J Bone Min Res. 2011;26:1617–1626. doi: 10.1002/jbmr.353. [DOI] [PubMed] [Google Scholar]
- 46.White AA, III, Panjabi MM. 2nd ed. Philadelphia (PA): Lippincott; 1990. Clinical Biomechanics of the Spine. [Google Scholar]
- 47.Rohlmann A, Zander T, Bergmann G. Spinal loads after osteoporotic vertebral fractures treated by vertebroplasty or kyphoplasty. Eur Spine J. 2006;15:1255–1264. doi: 10.1007/s00586-005-0018-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grados F, Fechtebaum J, Flipon E, Kolta S, Roux C, Fardellone P. Radiographic methods for evaluating osteoporotic vertebral fractures. Joint Bone Spine. 2009;76:241–247. doi: 10.1016/j.jbspin.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 49.Tzermiadianos M, Renner S, Phillips F, Hadjipavlou A, Zindrick M, Havey R, et al. Altered disc pressure profile after an osteoporotic vertebral fracture is a risk factor for adjacent vertebral body fracture. Eur Spine J. 2008;17:1522–1530. doi: 10.1007/s00586-008-0775-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


