Abstract
Background:
Several measures of adiposity have been used for predicting diabetes. The results of studies regarding superiority of waist circumference (WC) to body mass index (BMI) are inconsistent. This study designed to compare the ability of different anthropometric measures in predicting diabetes and to determine their optimal cut-off values.
Methods:
A population-based cross-sectional study was conducted with 1,000 representative sample among adults aged 20–80 years in Babol, the Northern Iran. The demographic data were collected in a household survey, and the anthropometric measures of weight, height, waist, and hip circumference were measured with a standard method. Fasting blood sugar (FBS) ≥126 mg/dl was considered as diabetes. receiver operating characteristic analysis was used to estimate the predictive ability of different anthropometric indexes and their optimal cut-off values for high FBS.
Results:
The overall prevalence rate of diabetes was 14.0% (14.4% in men vs. 13.5% in women, P = 0.65). The prevalence rate was significantly higher in older age (>60 years), low educated and obese (P = 0.001). The mean of BMI, WC, waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) were significantly higher among diabetic in both sexes (P = 0.001). Among men, WC (area under the ROC curve [AUC] =0.64) and WHtR (AUC = 0.63) have slightly higher accuracy index compared with BMI (AUC = 0.62) or WHR (AUC = 0.60). In contrast, among women, WHtR (AUC = 0.69) and WC (AUC = 0.68) yielded slightly better predictive than BMI (AUC = 0.67). The optimal cut-off values obtained for BMI and WHtR were similar between two sexes (BMI = 24.95 kg/m2 for men and BMI = 25.2 kg/m2 for women, WHtR = 0.51 for both sexes) whereas the optimal cut-off value for WC was higher in men than women (98.5 cm men vs. 89.5 cm women).
Conclusions:
Overall WC and WHtR exhibited a slightly better discriminate performance than BMI for diabetes in both sexes, particularly in women.
Keywords: Body mass index, diabetes, waist circumference, waist-to-height ratio, waist-to-hip ratio
INTRODUCTION
Obesity is a major risk factor for type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular disease, and it is common across various population worldwide particularly in recent decades.[1,2,3] Several indexes such as body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) are used to determine general and central obesity in clinical practice. Although BMI is the most commonly used parameter for evaluation of obesity, but as a measure for identification of body composition as well as regional body fat distribution is not reliable because it is a marker of general obesity rather than central obesity.[4] Whereas, diagnosis of central obesity which correlates with abdominal and the visceral accumulation of adipose tissue and development of subsequent metabolic abnormalities and cardiovascular morbidity is more important.[5] Visceral fats are linked with lipolytic activity and reduce insulin activity through increasing fatty acids.[4,6] Among many anthropometric parameters, WHtR and WC are better measures of visceral and abdominal fat distribution.[4,7] In addition, these measures are better than BMI in predicting cardiovascular diseases.[8]
In spite of some biological plausibility of this evidence, the reports from different studies, remained controversial.[6,9,10,11,12] It was shown that while WC is strongly correlated with BMI but the association between diabetes with WC is greater than BMI which is a measure of general adiposity.[9,10,13] Similarly, WC exhibits greater ability in predicting abnormal fasting blood glucose as compared with BMI. Nonetheless, the cutoff levels for either of these measures depending on the ethnicity of the study populations vary across different studies.[13] This issue is of particular importance, because recognizing patients at higher risk of future development of diabetes or cardiovascular disease is helpful for planning preventive measures. In Northern Iran, obesity, and metabolic syndrome and diabetes is highly common due to changes in lifestyles and background characteristics.[3,14] Nonetheless, data regarding ability of obesity measures in the prediction of diabetes are scarce. Hence, the present study was conducted to estimate the ability of different anthropometric measures for prediction of diabetes and to determine their optimal cutoff level.
METHODS
We analyzed the data of a population-based cross-sectional study of 1,000 representative samples in urban adult aged 20–80 years in Babol, Northern Iran in 2012. This study primarily focused on the prevalence of cardiovascular risk factors and metabolic syndrome. A full description of the method was described elsewhere.[14] In brief, we used the two-stage standard cluster sampling techniques. In the first stage of sampling, we selected 25 clusters randomly based on cumulative frequency of population size of coverage of urban health centers. Then, around the centers of each cluster, about 50 subjects were recruited who met our inclusion. In a household survey, the individuals with history of recent severe cardiovascular atherosclerosis events, diagnosis of cancer under radio-chemotherapy, history of congenital disorders, end stage of kidney disease and also pregnant women were excluded from the study. Data regarding demographic and history of diabetes were collected with interview with a designed questionnaire. All anthropometric measures such as weight, height, WC, hip circumference were measured with a standard method. BMI was calculated as weight in kg divided by height in m2. WHR was defined as the ratio of WC to the hip and WHtR was calculated as the ratio of waist-to-height. After interview and clinical examination, all participants were requested to refer to the central lab in Ayatollah Rohani Hospital. Fasting blood sugar (FBS) was measured after 10–12 h overnight fasting in the morning at 7.00–9.00 by enzymatic method using oxidize test. Diabetes was diagnosed by FBS ≥ 126 mg/dl. We used the WHO criteria of obesity definition: BMI 18.5–24.9 for normal, 25–29.9 for overweight and ≥ 30 as obese. Abnormal WC was diagnosed according to ATP criteria as ≥ 102 for men and ≥ 88 cm in women. A written informed consent was obtained from all participants before study enrollment. The protocol of this study was approved by Ethical Consol of the Babol University of Medical Sciences.
In statistical analysis, we used SPSSS software version 18. The prevalence of diabetes was compared according to age as well as decades of age, sex, educational level, various levels of general and central adiposity regarding BMI, WC, WHR, and WHtR. In addition, subjects of both sexes with without diabetes were compared according to anthropometric measures including, age, weight, height, BMI, WC, WHR, WHtR with two independent samples t-test for normally distributed data and Wilcoxon test for variables without normal distribution. receiver operating characteristic (ROC) analysis was performed and the discriminating ability of BMI, WC, WHR, and WHtR was estimated by determining area under the ROC curve (AUC) and its 95% confidence interval (95%CI) and the optimal cutoff value. Diagnostic performance and the optimal cut-off value for each measure were determined using Yoden index that minimizes 1 – (sensitivity + specificity) or equivalently maximizes the sum of sensitivity and specificity in ROC space. In statistical analysis, the values of P less than 0.05 were considered as a significant level.
RESULTS
The mean age (±standard deviation) of participants was 43.5 ± 14.4 and 41.8 ± 12.6 years in men and women, respectively, (P = 0.06). A total of 450 participants (45%) were men, and 550 (55%) were women. Prevalence rate of diabetes in men and women was 14% and 13.5% (P = 0.65), respectively [Table 1]. Diabetes in subjects > 60 years of age was 25.5% versus 3.7% in younger age group of 20–29 years (P = 0.001). Obesity (BMI > 30 kg/m2 vs. <25 kg/m2) was significantly associated with diabetes (P = 0.001). Prevalence of diabetes was inversely correlated with educational levels (P = 0.001) and the highest prevalence rate was observed in low educated groups (28.6% vs. 6.8% in illiterates and university educated, respectively) [Table 2]. The values of all anthropometric measures in the diabetic group were significantly greater as compared with nondiabetics in both sexes [Table 3]. The ability of all measures for prediction of diabetes in women was greater than in men. WC in men and WHtR in women exhibited the greatest predictive ability for diabetes with respective accuracy of 69% and 64% [Figure 1].
Table 1.
The prevalence of abnormal FBS according to demographic characteristics and obesity indexes
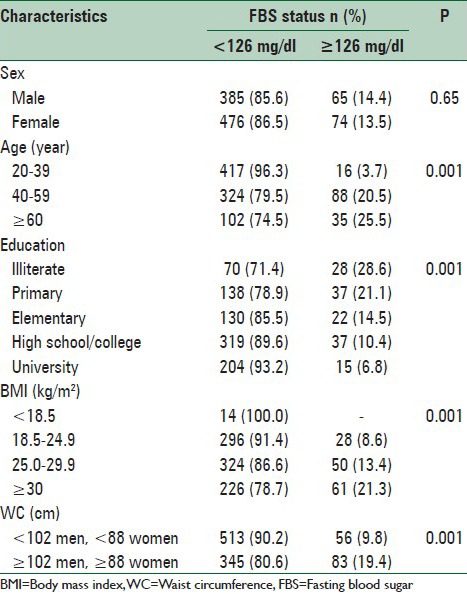
Table 2.
The mean (±SD) of anthropometric measures with respect to the FBS status and gender
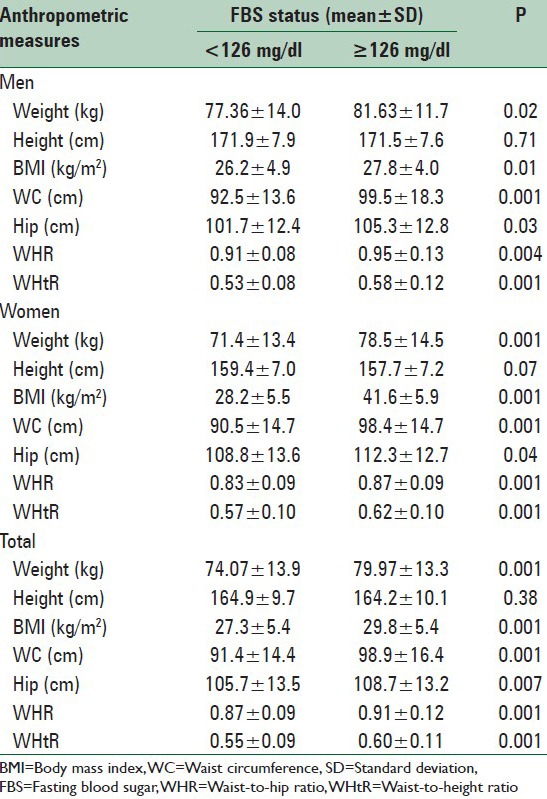
Table 3.
Diagnostic accuracy of different anthropometric measures for detection of abnormal FBS and their optimal cut-off values according to gender
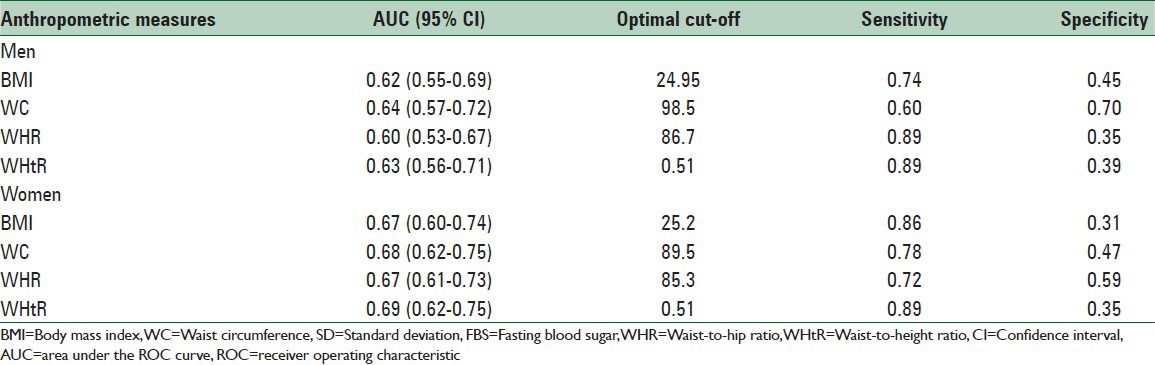
Figure 1.
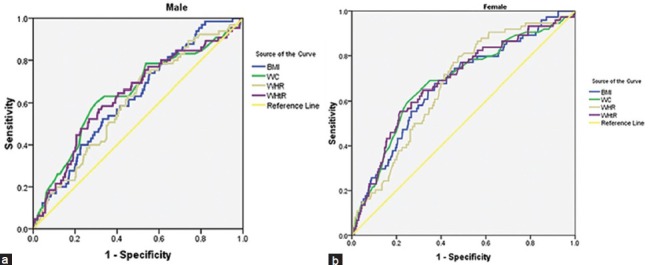
Receiver operating characteristic curves of different anthropometric measures for detection of abnormal fasting blood sugar according to gender (a) male, (b) female
Other measures such as BMI, WHR, and WC yielded comparable predictive ability in women, whereas, their ability in men was lower in particular WHR had the least accuracy of 60% in men. The accuracy of BMI for diabetes in men was much lower than in women (62% vs. 67%, respectively). According to cutoff value, the WC at cutoff level of 98.5 cm or greater yielded highest accuracy in predicting diabetes in men at sensitivity of 60% and specificity of 70% whereas, WHtR at cutoff level of 0.51 yielded the highest accuracy in predicting diabetes in women with sensitivity of 89% and specificity of 35%. However, in women the predictive ability of WC with a cutoff value of 89.5 cm was close to WHtR. Accuracy and cutoff levels of all measures are presented in Table 3. WHR and WHtR were the most sensitive but least specific for predicting diabetes in men with respective sensitivity of 89% and 35% whereas BMI and WHtR were the most sensitive and least specific in women with respective sensitivity of 89% and 39%. On the other hand, WC was the most specific measure of diabetes in women at 70% and the WHR the most specific measure of diabetes in women at 59%.
DISCUSSION
The findings of this study indicated a positive relationship between diabetes and aging, weight, BMI, and WC, as well as an inverse relationship between diabetes and educational level. Among the anthropometric measures, the WC yielded slight superiority to BMI in predicting diabetes in men, whereas in women the predictive ability of WC was close to BMI but with slightly higher specificity and lower sensitivity. Overall, both WC and BMI were more sensitive but less specific in prediction of diabetes in women as compared with men. The ability of other anthropometric measures such as WHR and WHtR were comparable with WC in both sexes, but these measures yielded greater performance in women. Nonetheless, WHtR at cut-off point value of 0.51, yielded the highest sensitivity in both sexes, but lower specificity than WC.
Diabetes is linked to obesity in particular abdominal obesity. Therefore, measure like WC, which estimates abdominal obesity is a better predictor of diabetes than BMI which is a marker of general obesity. Measures of abdominal obesity such as WC, WHR, and WHtR correlate with regional body fat distribution in particular abdominal obesity.[15,16,17,18,19,20,21,22,23,24] Lower predictive ability of BMI in men may be explained by dependency of BMI to height. Men are taller than women and so BMI in men are expected to be more affected by height as compared with women. In women, the predictive ability of BMI is close to WC. Thus in women, all measures of abdominal obesity such as WC, WHR, and WHtR and even BMI have demonstrated comparable predictive ability. Superiority of WC over BMI in predicting diabetes as observed in the present study has been also shown in other studies[10,16,19] including a meta-analysis of 31 studies.[26]
In the present study, performance of WHtR in recognizing diabetes was greater than WC, WHR, and BMI in both sexes as well as in other studies.[16,18,19,25] Even in subjects with normal WC and BMI, the WHtR is helpful in recognizing high-risk subjects.[25] For these reasons, WHtR has been suggested as a simple and useful screening tool for predicting diabetes in Chinese population.[19] It is also a useful tool in recognizing impaired glucose tolerance test in younger age group.[20] Among all central obesity parameters, WHtR yields higher ROC curve than BMI and greater predictive ability for diabetes in men.[16] The findings of the present study are in consistent with a longitudinal study of Iranian population that WHtR yielded the highest ability for future development of diabetes between other anthropometric measures.[17] In another prospective study of Chinese people over a median follow-up duration of 2 years, WHtR with AUC = 0.63 was the best predictor of diabetes in men but WC with AUC = 0.70 was the best predictor of diabetes in women.[22] Nonetheless, in another longitudinal study of Tehranian people WHtR and BMI exhibited similar predictive ability in both sexes.[21]
The clinical significance of anthropometric measures such as WC and WHtR is not limited to their predictive ability for diabetes but also for their potential in recognizing subjects on future development of cardiometabolic complications.[23,26,27,28,29] A systematic review of 22 prospective analyses showed that WHtR and WC significantly predicted cardiovascular outcomes similarly better than BMI.[26] These findings were supported by cross-sectional studies consisted of adults and children.[25] A cut-off value of 0.50 which is close to WHtR cut-off value derived from the present study has been reported from a study consisting of Caucasian, Asian, and Central American subjects from different countries for both men and women. At this cutoff level, WHtR predicted all cardiometabolic outcomes.[30]
The cross-sectional nature of this study may limit causal interpretation of the findings and thus the direction of causality may be unclear. We also used diabetes as dependent variable using fasting glucose criterion. There could be some merit in looking at impaired fasting glucose and another criterion of diabetes diagnosis for future prospective studies. However, our study has some advantage; it is a large sample of population-based study that used a standardized well-validated instruments and appropriate sampling method. Thus, it is expected with minimal bias.
CONCLUSIONS
The results of our study in consistent with earlier studies indicate that WC with respective cut-off value of 98.5 cm and 89.5 cm in men and women, respectively, and WHtR at cut-off value of >0.51 of both sexes predicted diabetes better than BMI and discriminated diabetic from nondiabetic with higher accuracy in both sexes. Regarding high prevalence rate of obesity, metabolic syndrome, diabetes, and cardiovascular diseases in the general population of this geographic region.[3,14,31] The results of this study emphasize application of WHtR and WC as an appropriate discriminative tools for identification of diabetes.
ACKNOWLEDGMENTS
We would like to acknowledge the Deputy of Research Council of Babol University of Medical Science for their supports and we thank to Dr. Firouzjahi, Mrs. Bagherzadeh, and nursing students of Babol University of Medical Sciences for their assistance in data collection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Seidell JC. The impact of obesity on health status: Some implications for health care costs. Int J Obes Relat Metab Disord. 1995;19(Suppl 6):S13–6. [PubMed] [Google Scholar]
- 2.Eckel RH, Krauss RM. American Heart Association call to action: Obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation. 1998;97:2099–100. doi: 10.1161/01.cir.97.21.2099. [DOI] [PubMed] [Google Scholar]
- 3.Hajian-Tilaki KO, Heidari B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20-70 years, in the north of Iran: A population-based study and regression approach. Obes Rev. 2007;8:3–10. doi: 10.1111/j.1467-789X.2006.00235.x. [DOI] [PubMed] [Google Scholar]
- 4.Kok P, Seidell JC, Meinders AE. The value and limitations of the body mass index (BMI) in the assessment of the health risks of overweight and obesity. Ned Tijdschr Geneeskd. 2004;148:2379–82. [PubMed] [Google Scholar]
- 5.Wu HY, Xu SY, Chen LL, Zhang HF. Waist to height ratio as a predictor of abdominal fat distribution in men. Chin J Physiol. 2009;52:441–5. doi: 10.4077/cjp.2009.amh064. [DOI] [PubMed] [Google Scholar]
- 6.Lara M, Bustos P, Amigo H, Silva C, Rona RJ. Is waist circumference a better predictor of blood pressure, insulin resistance and blood lipids than body mass index in young Chilean adults? BMC Public Health. 2012;12:638. doi: 10.1186/1471-2458-12-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mirmiran P, Esmaillzadeh A, Azizi F. Detection of cardiovascular risk factors by anthropometric measures in Tehranian adults: Receiver operating characteristic (ROC) curve analysis. Eur J Clin Nutr. 2004;58:1110–8. doi: 10.1038/sj.ejcn.1601936. [DOI] [PubMed] [Google Scholar]
- 8.Carlsson AC, Riserus U, Ärnlöv J, Borné Y, Leander K, Gigante B, et al. Prediction of cardiovascular disease by abdominal obesity measures is dependent on body weight and sex – Results from two community based cohort studies. Nutr Metab Cardiovasc Dis. 2014;24:891–9. doi: 10.1016/j.numecd.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Vazquez G, Duval S, Jacobs DR, Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: A meta-analysis. Epidemiol Rev. 2007;29:115–28. doi: 10.1093/epirev/mxm008. [DOI] [PubMed] [Google Scholar]
- 10.Qiao Q, Nyamdorj R. Is the association of type II diabetes with waist circumference or waist-to-hip ratio stronger than that with body mass index? Eur J Clin Nutr. 2010;64:30–4. doi: 10.1038/ejcn.2009.93. [DOI] [PubMed] [Google Scholar]
- 11.Vasques AC, Rosado LE, Rosado GP, Ribeiro Rde C, Franceschini Sdo C, Geloneze B, et al. Predictive ability of anthropometric and body composition indicators in the identification of insulin resistance. Arq Bras Endocrinol Metabol. 2009;53:72–9. doi: 10.1590/s0004-27302009000100011. [DOI] [PubMed] [Google Scholar]
- 12.Wang F, Wu S, Song Y, Tang X, Marshall R, Liang M, et al. Waist circumference, body mass index and waist to hip ratio for prediction of the metabolic syndrome in Chinese. Nutr Metab Cardiovasc Dis. 2009;19:542–7. doi: 10.1016/j.numecd.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Azizi F, Hadaegh F, Khalili D, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate definition of metabolic syndrome among Iranian adults: Report of the Iranian National Committee of Obesity. Arch Iran Med. 2010;13:426–8. [PubMed] [Google Scholar]
- 14.Hajian-Tilaki K, Heidari B, Firouzjahi A, Bagherzadeh M, Hajian-Tilaki A, Halalkhor S. Prevalence of metabolic syndrome and the association with socio-demographic characteristics and physical activity in urban population of Iranian adults: A population-based study. Diabetes Metab Syndr. 2014;8:170–6. doi: 10.1016/j.dsx.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 15.Elbassuoni E. Better association of waist circumference with insulin resistance and some cardiovascular risk factors than body mass index. Endocr Regul. 2013;47:3–14. doi: 10.4149/endo_2013_01_3. [DOI] [PubMed] [Google Scholar]
- 16.Hadaegh F, Zabetian A, Harati H, Azizi F. Waist/height ratio as a better predictor of type 2 diabetes compared to body mass index in Tehranian adult men – a 3.6-year prospective study. Exp Clin Endocrinol Diabetes. 2006;114:310–5. doi: 10.1055/s-2006-924123. [DOI] [PubMed] [Google Scholar]
- 17.Hadaegh F, Shafiee G, Azizi F. Anthropometric predictors of incident type 2 diabetes mellitus in Iranian women. Ann Saudi Med. 2009;29:194–200. doi: 10.4103/0256-4947.51788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cai L, Liu A, Zhang Y, Wang P. Waist-to-height ratio and cardiovascular risk factors among Chinese adults in Beijing. PLoS One. 2013;8:e69298. doi: 10.1371/journal.pone.0069298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jayawardana R, Ranasinghe P, Sheriff MH, Matthews DR, Katulanda P. Waist to height ratio: A better anthropometric marker of diabetes and cardio-metabolic risks in South Asian adults. Diabetes Res Clin Pract. 2013;99:292–9. doi: 10.1016/j.diabres.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 20.Lopatynski J, Mardarowicz G, Szczesniak G. A comparative evaluation of waist circumference, waist-to-hip ratio, waist-to-height ratio and body mass index as indicators of impaired glucose tolerance and as risk factors for type-2 diabetes mellitus. Ann Univ Mariae Curie Sklodowska Med. 2003;58:413–9. [PubMed] [Google Scholar]
- 21.Bozorgmanesh M, Hadaegh F, Azizi F. Diabetes prediction, lipid accumulation product, and adiposity measures; 6-year follow-up: Tehran lipid and glucose study. Lipids Health Dis. 2010;9:45. doi: 10.1186/1476-511X-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jia Z, Zhou Y, Liu X, Wang Y, Zhao X, Wang Y, et al. Comparison of different anthropometric measures as predictors of diabetes incidence in a Chinese population. Diabetes Res Clin Pract. 2011;92:265–71. doi: 10.1016/j.diabres.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Ware LJ, Rennie KL, Kruger HS, Kruger IM, Greeff M, Fourie CM, et al. Evaluation of waist-to-height ratio to predict 5 year cardiometabolic risk in sub-Saharan African adults. Nutr Metab Cardiovasc Dis. 2014;24:900–7. doi: 10.1016/j.numecd.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Meseri R, Ucku R, Unal B. Waist: Height ratio: A superior index in estimating cardiovascular risks in Turkish adults. Public Health Nutr. 2014;17:2246–52. doi: 10.1017/S136898001300267X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu Q, Shen F, Ye T, Zhou Q, Deng H, Gu X. Waist-to-height ratio is an appropriate index for identifying cardiometabolic risk in Chinese individuals with normal body mass index and waist circumference. J Diabetes. 2014;6:527–34. doi: 10.1111/1753-0407.12157. [DOI] [PubMed] [Google Scholar]
- 26.Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes Rev. 2012;13:275–86. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- 27.Can AS, Bersot TP, Gönen M, Pekcan G, Rakicioglu N, Samur G, et al. Anthropometric indices and their relationship with cardiometabolic risk factors in a sample of Turkish adults. Public Health Nutr. 2009;12:538–46. doi: 10.1017/S1368980008002474. [DOI] [PubMed] [Google Scholar]
- 28.Dong X, Liu Y, Yang J, Sun Y, Chen L. Efficiency of anthropometric indicators of obesity for identifying cardiovascular risk factors in a Chinese population. Postgrad Med J. 2011;87:251–6. doi: 10.1136/pgmj.2010.100453. [DOI] [PubMed] [Google Scholar]
- 29.Marcadenti A, Fuchs SC, Moreira LB, Wiehe M, Gus M, Fuchs FD. Accuracy of anthropometric indexes of obesity to predict diabetes mellitus type 2 among men and women with hypertension. Am J Hypertens. 2011;24:175–80. doi: 10.1038/ajh.2010.212. [DOI] [PubMed] [Google Scholar]
- 30.Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- 31.Hosseini SR, Cumming RG, Kheirkhah F, Nooreddini H, Baiani M, Mikaniki E, et al. Cohort profile: The Amirkola Health and Ageing Project (AHAP) Int J Epidemiol. 2014;43:1393–400. doi: 10.1093/ije/dyt089. [DOI] [PubMed] [Google Scholar]


