Abstract
Background:
The patient decision aids (PDAs), which can facilitate the decision-making process when choosing the optimal method of treatment, are a challenge to patients. This study tried to determine the attitude of physicians on the barriers of using PDAs in the way of prioritizing and proposing solutions to them.
Methods:
This study was a cross-sectional research carried out on 150 clinical faculty members of research centers and scientific associations affiliated with Tehran University of Medical Sciences. The participants were chosen using the convenience sampling method. The attitude of physicians toward the application of PDAs was interviewed using a self-made questionnaire composed of 23 questions. The association between physicians’ attitude to the use of PDAs and their characteristics was examined using the t-test, analysis of variance, and correlation test.
Results:
The mean score of physicians’ attitude was 76.2 (standard deviation =11.9) and the range was 33–107. There was a significant and direct association between the attitude toward the use of PDA and the respondents’ age (r = 0.237, P = 0.007), years of experience (r = 0.205, P = 0.02), being male (P = 0.04), and working in the private sector (P = 0.009). The attitude score of instructors was significantly lower than that of professors (P = 0.02).
Conclusions:
The general attitude of physicians toward the use of PDAs was positive. However, apparently as a result of problems mentioned in this study for the developing countries such as Iran, it is much easier to employ these tools in centers run by the private sector. Usage of such tools in public centers necessitates systemic infrastructure as well as credits and budgets required for the training of patients and physicians.
Keywords: Attitude, developing country, Iran, patient decision aids, physician
INTRODUCTION
Decision-making is a sophisticated process in medicine and in about 83% of the cases, it is not possible to choose the optimal treatment method decisively based on a specific cut-off point.[1] Hence, physicians should collect relevant evidence and reach a proper decision on the optimal treatment method. In such cases, traditional physicians adopt the alternative approach and decide on their own. However, this approach has been very challenging in the past few years.[2] Therefore, methods such as the patient decision aids (PDAs) have been designed to involve equally both physicians and patients in a mutual decision-making process for choosing the optimal treatment. Using the instrument, physicians can examine treatment methods and their consequences with regard to patients’ preferences and conditions.[3]
Some of the advantages of using PDAs include mental preparation,[4,5] higher patient satisfaction,[6,7,8,9] increased patient participation in the decision-making process,[1,10] development of a more realistic approach to the disease and its possible damages and harms,[10,11,12,13] more compliance of patients to the proposed treatment,[6] and reduction in expenses.[1,14] Although numerous advantages have been listed for joint decisions made with the mutual participation of physicians and patients, there are challenges (such as shortage of medical training for joint decision-making, physicians’ time limits, or patient's unwillingness to cooperate) to this end.[15] The tools are designed and used in bedside in the developed countries such as the United States, Canada, and England. However, among developing countries, Saudi Arabia is the only country to design and employ such tools.[16] In Iran, as a developing country, the only research conducted on the use of PDAs is the qualitative study, which analyzes the viewpoints of physicians and patients on the challenges and obstacles to the use of such tools.[15] The above-mentioned substantial and important challenges, which patients and physicians are faced with in using such tools were reported as the findings of this study. However, in addition to this information, quantification of physicians’ opinions on these challenges is required to help prioritize the problems and present solutions in planning on using the tools. However, it is not possible to use the results of qualitative studies to achieve this aim.
Numerous quantitative studies have been globally performed to employ the viewpoints of physicians in the development and assessment of PDAs. The studies have mainly focused on some certain PDAs and have been carried out in the developed countries.[17,18,19,20,21] Since the cultural, economic and social structures of developing countries like Iran are different from those in developed countries, it is necessary to study the attitudes of such countries toward the application of these tools in their cultural and medical structures. The present study aimed to seek, through a questionnaire, the viewpoints of physicians, as the first group to be involved in the design and use of these tools. Findings of this research can be used as a guide to other quantitative studies on the viewpoints of patients, and on the proper use of such tools in Iran and other developing countries.
METHODS
Study population and sampling method
This cross-sectional study was conducted on 150 clinical faculty members of research centers and scientific associations affiliated with Tehran University of Medical Sciences. The participants were selected using the convenience sampling method. They were selected through an internet-wide search from centers which PDAs are applicable for their specialty. Samples were selected from three major groups of physicians: General practitioners (GPs), specialists, and subspecialists. In sum, a total of 17 research centers and 26 scientific associations, including the following participated in the study: Surgeons’ society, pediatric surgeons, neurosurgeons, gynecological cancer surgeons, cardiac surgeons, dermatologists and sexually transmitted diseases specialists, Iranian Urological Association, orthopedic surgeons, otolaryngologists, gynecologists, pulmonologists, gastroenterologists, Society of Internists, infectious disease specialists, nephrologists, radiologists, psychiatrists, ophthalmologists, and neurologists.
The participants mostly were not familiar with PDAs but we tried to inform them through a native sample and relevant English samples incorporated into the inquiry packages. The sample size was 150 assuming Z = 1.96, standard deviation (SD) =1.25 (which was obtained from the Pilot section), and d = 0.2. Participants under study were investigated up to 3 visits, but when they continued to refuse cooperation, they were substituted with other candidates.
Data collection tool
In this research, information was collected using a 23-item researcher-made questionnaire, which investigated the attitude of physicians toward the use of PDAs. The including items questioned the following issues:
The effects of using PDAs on the process of treatment and patient decision-making, coordinating values with candidacy of patients, commitment of the patient to health care instructions, physicians’ workload, patient participating in the decision-making process, patient satisfaction, patient expectation from treatment, patient trust in the physician, valuing patient rights, cost-effectiveness of the use of PDAs, patients’ and physicians’ acceptance of PDAs, compliance of PDAs to the culture, patients’ understanding and knowledge, and adequacy of information presented in PDAs for facilitating the decision-making process for the majority of patients.
Content and face validity of the questionnaire was examined in four sessions with a number of physicians. The content validity of the questionnaire was examined considering the appropriateness, relevance, and adequacy of questions. Its face validity was also examined considering the intelligibility, order, and proper sequence of questions. Required modifications were applied to the questionnaire and the initial draft of the questionnaire was prepared for the reliability test.
In order to examine the reliability of the questionnaire, a total of 20 physicians completed the questionnaire twice with a 15-day interval. The reliability of the results obtained from the questionnaires was also measured using the Intraclass Correlation Coefficient (ICC) index. The ICC index obtained for all of the questions was between 0.53 and 0.96 (mean ICC =0.74). The ICC below 0.7 was considered unacceptable[22] and it was below 0.7 for 3 items, because they were ambiguous and unclear. Therefore, during the review process those items were re-written or revised. Moreover, the internal consistency of the items was also measured using the Cronbach's statistic. Considering a cut-off point of 0.7 and more,[22] the value obtained for the Cronbach's alpha (0.74) reflected adequate internal consistency of the items.
The independent variables examined in the research were background information and possible confounders, which included age (years), gender, scientific rank (instructor, assistant professor, associate professor, and professor), experience (year), experience with the private sector (yes or no), and experience with an educational department (GP, specialist, and subspecialist). The attitude of the participants toward the use of PDAs was also the dependent variable.
Ethical considerations
Since physicians were busy working, appointments were set in advance. Participants took part in the study freely and voluntarily and questionnaires did not ask for the names or addresses of the physicians. Prior to the test, physicians were ensured that their information would be recorded anonymously. They were also told that they could write their E-mail address on the questionnaire if they liked to be informed of the test results. Moreover, as an expression of gratitude, gifts was presented to the physicians following their formal consent to take part in the research. The project was passed under 90-04-102-16336 in the Ethics Committee of Tehran University of Medical Sciences.
Statistical analysis
Results of this study are presented in the following two categories: Descriptive results and analytic results. A descriptive analysis was performed to describe each of the items questioning the attitude of physicians. The objective of the analytic analysis was also to study the relationship between the independent variables and the dependent variable (the attitude of physicians toward the use of PDA).
Items were scored based on a five point Likert scale ranging from 1 to 5: (1) Strongly disagree; (2) disagree; (3) neither agree nor disagree; (4) agree; and (5) strongly agree. The mean and SD values of the items were calculated separately and viewpoints were analyzed as positive, neutral, and negative: Scores 4 or 5 (agree or strongly agree) were considered as indicators of positive viewpoint; score 3 (neither agree nor disagree) reflected neutral viewpoint; and scores 1 or 2 (strongly disagree or disagree) showed negative viewpoint. The overall attitude of the physicians was measured based on the total scores of the 23 statements and the scores varied from 23 to 115. We checked the normality of data using Kolmogorov–Smirnov test (P = 0.553) and graphical tests. The t-test, Pearson's Chi-square, one-way analysis of variance, and Pearson correlation were used to analyze the relationships between independent variables and the attitude of physicians. Statistical analyses were performed using the IBM SPSS 20 software.
RESULTS
One hundred and fifty (response rate =71%) questionnaires were completed out of 212, and 62 physicians refused to cooperate even after three requests. In the case of participants that had refused to complete the questionnaires only information on their specialty was recorded. The difference between the specialties of the physicians who refused to cooperate and those who cooperated was measured using Pearson's Chi-square test. However, the difference was shown to be not statistically significant (P = 0.37). The mean age of participants was 48 years (SD =9.30) and their mean experience was 14.98 years (SD =9.39). 22.7% of the participants were female and the rest were male. 46.7% of the physicians were assistant professors, 27.3% were associate professors, 20.7% were professors, and the rest were instructors. Moreover, 58% of the physicians also worked for the private sector.
More than half of the participants had the positive view that patients would appreciate the PDAs (60.7%). In addition, 44% of the physicians had the positive view that Iranian physicians would welcome the use of such tools. The highest positive attitude (88.7%) was shown to be toward the importance of valuing patient rights [Table 1].
Table 1.
Description of questions about the attitude area (n = 150)
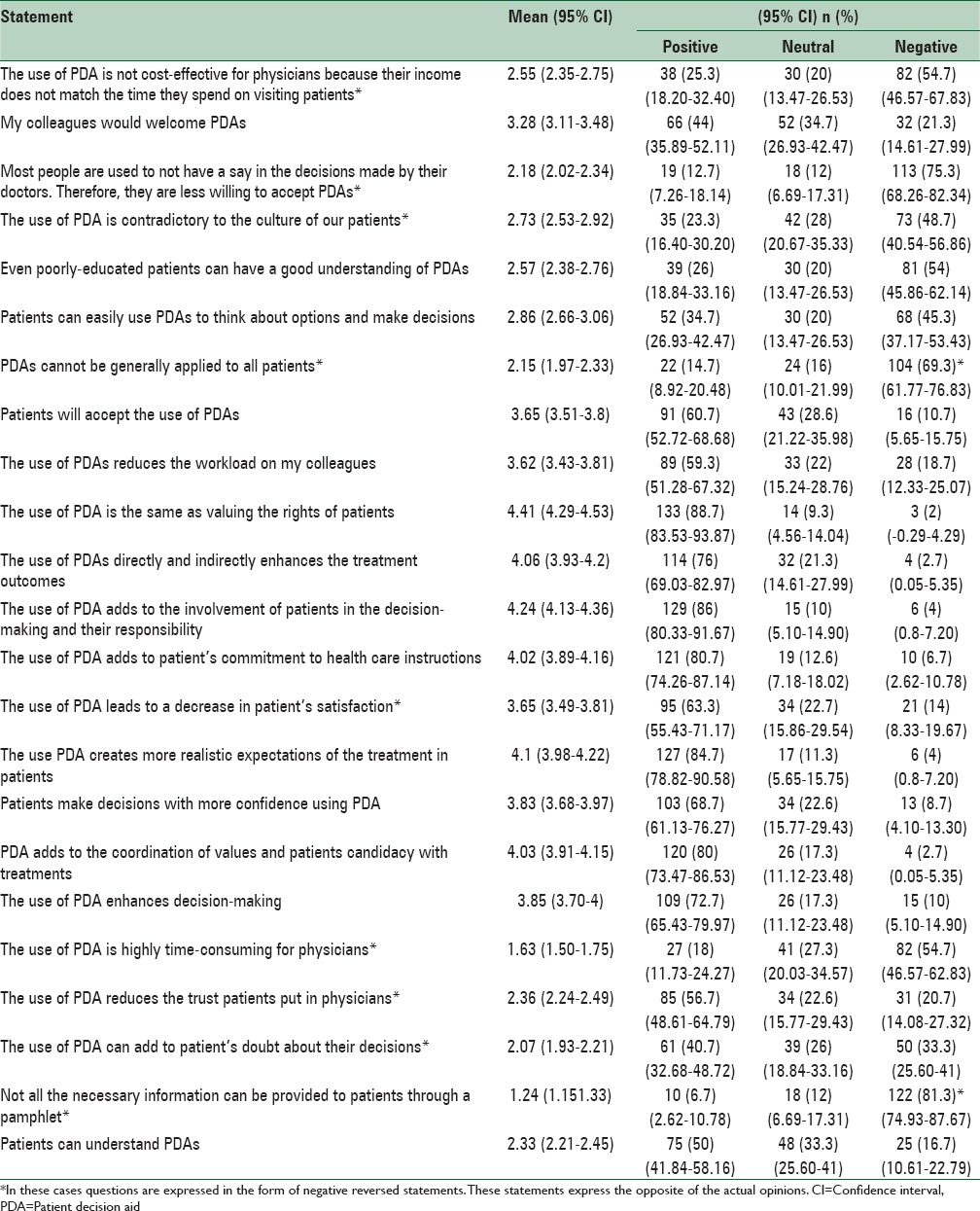
Furthermore, 86% of the physicians were positive about the effect of this tool on the growth of responsibility to and cooperation of patients in the decision-making process. 80.7% of the physicians also agreed that the use of such tools could lead to an increase in the commitment of patients to health care instructions. On the other hand, only 14% of the participants agreed that the use of these tools would bring about an increase in patients’ satisfaction. 20.7% of the physicians also were positive about the effect of these tools on the increase in the trust patients put in their doctors. Development of more realistic expectations from treatment (84.7%), coordination of values and candidacy of patients with treatment methods (80%), direct and indirect improvement of treatment outcomes (76%), and enhanced patient decision-making (72.7%) were among other opinions expressed by other participants. However, it is worth mentioning that 75.3% of the physicians acknowledged that most patients are not accustomed to having a say in the decisions made by their doctors [Table 1].
Only 26% of the physicians agreed that poorly-educated patients could also understand these tools very well. However, 69.3% of the physicians believed that PDAs could be used generally for all patients. In addition, a relatively high percentage of physicians (81.3%) believed that all of the necessary information could be provided to the patients through pamphlets [Table 1]. In general, the attitude score values varied from 33 to 107 and the mean score was calculated to be 76.2 (74.3–78.1).
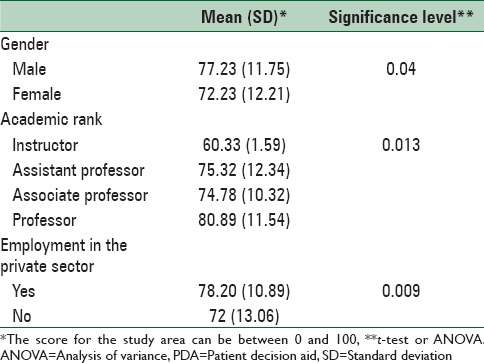
As shown in Table 2, analysis of the association between the demographic variables and attitude of participants toward the use of PDAs revealed that all of the variables, except for the teaching group (GPs, specialists and subspecialists), were significant at a significance level of 0.05. The mean attitude toward the use of PDAs was positively and significantly related with age (r = 0.237, P = 0.007) and years of experience (r = 0.205, P = 0.02). In addition, physicians working for the private sector (P = 0.009) and male participants (P = 0.04) showed a significantly higher positive attitude. Using the analyses of variance and bonferroni comparison test, the average attitude of instructors was found to be significantly lower than that of professors (P = 0.02), while no significant difference was observed between the attitudes of assistant and associate professors (P = 0.99) [Table 2].
Table 2.
Analysis of the association between demographic variables and attitude of physicians to the use of PDA in Iran
DISCUSSION
Findings of this study suggest that physicians have a positive attitude toward the use of PDAs and their positive effect on the relationship between physicians and patients. The findings also indicate that the use of PDAs is more common in private hospitals. Moreover, physicians with more experience or age are probably more familiar with the joint decision-making models and communications skills and therefore have a more positive attitude toward the use of these tools. Male physicians also showed a more positive attitude compared to their female counterparts.
More than half of the physicians participating in the study believed that the use of PDAs could lead to a reduction in the reliability of physicians in the eyes of patients or patient satisfaction. Conversely, there was a positive attitude toward the use of PDAs by patients. According to the findings of various studies, a satisfactory level of patient satisfaction and trust is obtained by assessing patients’ tendency to and need for becoming informed. It helps understand the level of tendency of patients to take part in making the decisions on the treatment method. It also reveals patients’ choice of behaviors shown by medics during patient-doctor interactions.[23] The related qualitative study suggests that patients’ tendency to become involved in decision-making depends on the kind and intensity of their disease as well as their education level.[15] Therefore, neglecting this fact can have adverse effects on patient satisfaction and well-being, and can decrease fruitfulness of the treatment method.[24]
Some physicians participating in the research believed that poorly-educated people cannot have a profound understanding of the tools. Moreover, findings of other studies also indicate that patients with lower education levels are less willing to participate in decision-making processes.[25] Hence, in using these tools for patients, personal and personality differences shall be taken into account because it is not possible to treat all patients with the same method. Although decision support technologies have been developing for three decades, PDAs are loosely based on personal needs. Apparently, appropriate use of health innovations (different need-specific technologies such as films, audiovisual equipment, the Internet, and cell phone) can effectively mitigate this problem.[26]
Physicians participating in the present research believed that most patients are used to not having a say in the decisions made by their doctors. Therefore, they can hardly picture themselves participating in the decision-making process. Findings of other studies suggest that as a result of the emergence of new roles, the process of changing the pattern of patient-physician relationship is at first responded with cultural opposition,[27] which will decline after the implementation of the new system. However, findings of different studies[28,29] indicate that most Iranian patients are not aware of their rights because choosing the treatment method is one of the rights of patients.[30] In fact, people's ideas or beliefs about their health conditions can have a significant effect on their behavior and reactions. In this regard, the PDAs are an important contribution to the recognition of this substantial right.[31] Therefore, patients shall be trained on the use of these tools.
Although physicians were shown to be positive about valuing patient's rights by involving them in the decision-making process, only less than half the physicians had a positive attitude toward the acceptance of these tools by their colleagues. This is perhaps because of systemic problems such as improper distribution of human force, shortage of time, awareness and training deficits, and shortage of theoretical and practical clinical trainings in the internship period.[15] Hence, it is particularly important to assess service models and plan on the employment of proper strategies for increasing the awareness of physicians and managing the available bedside resources.[32,33,34]
The advantages enumerated for PDAs in this research were as follows: Development of a more realistic approach to the disease as well as its possible damages and harms,[10,11,12,13] more compliance of patients to the selected treatment,[6] increase in the participation of patients in the decision-making process,[1,10] coordination of values and candidacy of patients with treatment methods,[27] direct and indirect improvement of treatment outcomes.[24] The aforementioned advantages were consistent with the results of the qualitative study carried out in Iran.[15] Moreover, the results of the regular review of 29 clinical experiments with the effectiveness of PDAs indicated that the use of such tools contributes to the improvement of the following decision quality indicators: Awareness of options, realistic interpretations of possible consequences, and compliance between patients’ and options values. It was also indicated that patients using the PDAs actively participate in the decision-making process and are faced with less hesitation or difficulties.[32]
Previous studies suggest that an increase in the physicians’ years of experience leads to a reduction in their tendency to involve patients in decisions. However, this finding is in contrast with the findings of the present study. In this study, any increase in the age and consequently the experience of physicians led to an increase in their positive attitude. Moreover, it was found out that female physicians are less willing to involve patients in the decision-making process compared to the male physicians. This finding is also in accordance with the findings of other studies.[35] It is, therefore, recommended to change the attitude of physicians and encourage them to share decisions with patients and to learn or teach a wide range of communicational and interpersonal skills.[36]
Weaknesses and strengths of the study
Lack of knowledge of PDAs was one of the limitations of the research. However, this limitation was overcome by incorporating a native sample as well as English samples that were relevant to the specialties of the participants into the inquiry packages. Another limitation of this study was convenience sampling which does not guarantee representativeness of the all eligible participants. Hence, we recommend studies with random sampling methods and larger sample sizes.
In addition, one of the weaknesses of the present research is that it was conducted on physicians with different specialties. Therefore, it is recommended to perform more professional studies of the efficiency of PDAs for different specialties by localizing the available foreign tools. Moreover, as a result of the lack of demographic information about the individuals who refused to take part in the study, it was not possible to draw a comparison between their characteristics and those of participants. Therefore, it is not possible to determine the direction of bias resulted from the noncooperation. Nevertheless, there was no significant difference between the specialties of those who took part and those who did not take part in the research. In sum, the level of cooperation was satisfactory.
CONCLUSIONS
Although physicians generally have a positive attitude toward the use of the PDAs, it seems that private medical centers in developing countries such as Iran will be more successful in employing such tools by considering the characteristics of patients. Usage of such tools in public centers necessitates systemic infrastructure as well as credits and budgets required for the training of patients and physicians.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Canadian Health Service Research Foundation: Introduce Patient Decision Aid to Improve Clinical Decision – Making Quality “Grey Zone” Decision. 2007. [Last accessed on 2013 Sep 25]. Available from: http://www.cfhi-fcass.ca/migrated/pdf/mythbusters/boost9_e.pdf .
- 2.Stacey D, Samant R, Bennett C. Decision making in oncology: A review of patient decision aids to support patient participation. CA Cancer J Clin. 2008;58:293–304. doi: 10.3322/CA.2008.0006. [DOI] [PubMed] [Google Scholar]
- 3.Davis RE, Dolan G, Thomas S, Atwell C, Mead D, Nehammer S, et al. Exploring doctor and patient views about risk communication and shared decision-making in the consultation. Health Expect. 2003;6:198–207. doi: 10.1046/j.1369-6513.2003.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Connor AM, Drake ER, Fiset V, Graham ID, Laupacis A, Tugwell P. The Ottawa patient decision aids. Eff Clin Pract. 1999;2:163–70. [PubMed] [Google Scholar]
- 5.Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients’ participation in medical care: Effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 6.Rothert ML, Holmes-Rovner M, Rovner D, Kroll J, Breer L, Talarczyk G, et al. An educational intervention as decision support for menopausal women. Res Nurs Health. 1997;20:377–87. doi: 10.1002/(sici)1098-240x(199710)20:5<377::aid-nur2>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 7.Roter DL. Physician/patient communication: Transmission of information and patient effects. Md State Med J. 1983;32:260–5. [PubMed] [Google Scholar]
- 8.Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, et al. Preferences of patients for patient centred approach to consultation in primary care: Observational study. BMJ. 2001;322:468–72. doi: 10.1136/bmj.322.7284.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheibler F, Janssen C, Pfaff H. Shared decision making: An overview of international research literature. Soz Praventivmed. 2003;48:11–23. doi: 10.1007/s000380300002. [DOI] [PubMed] [Google Scholar]
- 10.McCaffery K, Irwig L, Bossuyt P. Patient decision aids to support clinical decision making: Evaluating the decision or the outcomes of the decision. Med Decis Making. 2007;27:619–25. doi: 10.1177/0272989X07306787. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions (Review) Cochrane Libr. 2004:4. [Google Scholar]
- 12.O’Connor AM, Fiset V, DeGrasse C, Graham ID, Evans W, Stacey D, et al. Decision aids for patients considering options affecting cancer outcomes: Evidence of efficacy and policy implications. J Natl Cancer Inst Monogr. 1999;1999(5):67–80. doi: 10.1093/oxfordjournals.jncimonographs.a024212. [DOI] [PubMed] [Google Scholar]
- 13.O’Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. Randomized trial of a portable, self-administered decision aid for postmenopausal women considering long-term preventive hormone therapy. Med Decis Making. 1998;18:295–303. doi: 10.1177/0272989X9801800307. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy AD, Sculpher MJ, Coulter A, Dwyer N, Rees M, Abrams KR, et al. Effects of decision aids for menorrhagia on treatment choices, health outcomes, and costs: A randomized controlled trial. JAMA. 2002;288:2701–8. doi: 10.1001/jama.288.21.2701. [DOI] [PubMed] [Google Scholar]
- 15.Rashidian H, Nedjat S, Majdzadeh R, Gholami J, Haghjou L, Abdollahi BS, et al. The perspectives of Iranian physicians and patients towards patient decision aids: A qualitative study. BMC Res Notes. 2013;6:379. doi: 10.1186/1756-0500-6-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ottawa Hospital Research Institute. [Last accessed on 2013 May 11]. Available from: http://www.decisionaid.ohri.ca/cochinvent.php .
- 17.O’Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. A decision aid for women considering hormone therapy after menopause: Decision support framework and evaluation. Patient Educ Couns. 1998;33:267–79. doi: 10.1016/s0738-3991(98)00026-3. [DOI] [PubMed] [Google Scholar]
- 18.Whelan T, Levine M, Willan A, Gafni A, Sanders K, Mirsky D, et al. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery: A randomized trial. JAMA. 2004;292:435–41. doi: 10.1001/jama.292.4.435. [DOI] [PubMed] [Google Scholar]
- 19.Watson E, Hewitson P, Brett J, Bukach C, Evans R, Edwards A, et al. Informed decision making and prostate specific antigen (PSA) testing for prostate cancer: A randomised controlled trial exploring the impact of a brief patient decision aid on men's knowledge, attitudes and intention to be tested. Patient Educ Couns. 2006;63:367–79. doi: 10.1016/j.pec.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Man-Son-Hing M, Laupacis A, O’Connor AM, Biggs J, Drake E, Yetisir E, et al. A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: A randomized controlled trial. JAMA. 1999;282:737–43. doi: 10.1001/jama.282.8.737. [DOI] [PubMed] [Google Scholar]
- 21.Human Development Index (HDI), HDRO (Human Development Report Office), United Nations Development Programme. 2010 [Google Scholar]
- 22.Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 23.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531–5. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: Evidence, models and interventions. Patient Educ Couns. 2006;61:319–41. doi: 10.1016/j.pec.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 25.McKeown RE, Reininger BM, Martin M, Hoppmann RA. Shared decision making: Views of first-year residents and clinic patients. Acad Med. 2002;77:438–45. doi: 10.1097/00001888-200205000-00020. [DOI] [PubMed] [Google Scholar]
- 26.Ng CJ, Lee YK, Lee PY, Abdullah KL. Health innovations in patient decision support: Bridging the gaps and challenges. Australas Med J. 2013;6:95–9. doi: 10.4066/AMJ.2013.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Connor AM, Wennberg JE, Legare F, Llewellyn-Thomas HA, Moulton BW, Sepucha KR, et al. Toward the ‘tipping point’: Decision aids and informed patient choice. Health Aff (Millwood) 2007;26:716–25. doi: 10.1377/hlthaff.26.3.716. [DOI] [PubMed] [Google Scholar]
- 28.Rad M, Mohammd A, Esna Ashari P. Patients and physicians awareness of patients rights and its implementation at Beheshti hospital in Isfahan. Iran J Med Educ. 2004;4:45–54. [Google Scholar]
- 29.Joolaee S, Tschudin V, Nikbakht-Nasrabadi A, Parsa-Yekta Z. Factors affecting patients’ rights practice: The lived experiences of Iranian nurses and physicians. Int Nurs Rev. 2008;55:55–61. doi: 10.1111/j.1466-7657.2007.00584.x. [DOI] [PubMed] [Google Scholar]
- 30.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 31.Silva DD. Evidence: Helping People Share Decision Making. The Health Foundation: Organization the Evidence Centre. 2012:10. [Google Scholar]
- 32.World Health Organization. Health Evidence Network (HEN) Report. Should Patient Decision Aids (PtDAs be Introduced in the Health Care System? 2005. [Last accessed on 2013 Nov 05]. pp. 2–25. Available from: http://www.euro.who.int/__data/assets/pdf_file/0011/74666/E87791.pdf .
- 33.Brace C, Schmocker S, Huang H, Victor JC, McLeod RS, Kennedy ED. Physicians’ awareness and attitudes toward decision aids for patients with cancer. J Clin Oncol. 2010;28:2286–92. doi: 10.1200/JCO.2009.25.2874. [DOI] [PubMed] [Google Scholar]
- 34.Charles C, Gafni A, Whelan T. Self-reported use of shared decision-making among breast cancer specialists and perceived barriers and facilitators to implementing this approach. Health Expect. 2004;7:338–48. doi: 10.1111/j.1369-7625.2004.00299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beisecker AE, Murden RA, Moore WP, Graham D, Nelmig L. Attitudes of medical students and primary care physicians regarding input of older and younger patients in medical decisions. Med Care. 1996;34:126–37. doi: 10.1097/00005650-199602000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Knops AM, Ubbink DT, Legemate DA, de Haes JC, Goossens A. Information communicated with patients in decision making about their abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2010;39:708–13. doi: 10.1016/j.ejvs.2010.02.012. [DOI] [PubMed] [Google Scholar]


