Abstract
The purpose of this paper is to present an evidence of automated wheeze detection system by a survey that can be very beneficial for asthmatic patients. Generally, for detecting asthma in a patient, stethoscope is used for ascertaining wheezes present. This causes a major problem nowadays because a number of patients tend to delay the interpretation time, which can lead to misinterpretations and in some worst cases to death. Therefore, the development of automated system would ease the burden of medical personnel. A further discussion on automated wheezes detection system will be presented later in the paper. As for the methodology, a systematic search of articles published as early as 1985 to 2012 was conducted. Important details including the hardware used, placement of hardware, and signal processing methods have been presented clearly thus hope to help and encourage future researchers to develop commercial system that will improve the diagnosing and monitoring of asthmatic patients.
Keywords: lung auscultation, lung sounds, wheeze, asthma
INTRODUCTION
Nowadays, asthma is becoming a common disease that may occur at any age and have become a public health challenge to the world today [1]. It is a chronic inflammatory diseases of the respiratory airway and can be hyper-responsiveness to a variety of stimuli [2]. The asthmatic patient suffers attacks such as coughing, dyspnea, and the main manifestation is wheezing [3]. Sounds generated during breathing can be a good source of information on lung’s health [4]. Any characteristic changes of the normal lung sounds can imply a diseased condition that probably is invading the lung. Each type of disease is different from each other and the variation can be ascertained from sound characteristic, pitch, amplitude, frequency, duration, etc. [5]. With regard to asthma, symptoms originating from the wall oscillations of narrowed airways at critical flow rates causes wheeze to occur [3]. Wheeze is one of the adventitious sounds present in lung that is clinically defined as abnormal. The presence of wheeze, its location, duration and its relation to the respiratory cycle can be very useful to assist the physician as it has become a crucial practice in diagnosing and managing a number of pulmonary pathologies such as chronic obstructive pulmonary disease (COPD), bronchiolitis and commonly asthma [6]. Wheezes are continuous adventitious sounds that are superimposed on the normal breath sounds. According to the American Thoracic Society (ATS), the word “continuous” can be defined as the duration of the wheeze that is longer than 250 ms. The ATS also defines wheezes as high-pitched continuous sounds with a dominant frequency of 400 Hz or more. Wheezes can be detected and classified based on the frequency characteristics of its sinusoidal waves that justifies the musical character of the wheeze [7]. Conventionally, stethoscope is used to diagnose and monitor wheezes in asthmatic patients. Although it is well known that auscultation with stethoscope is reliable, fast and non-invasive, continuous monitoring of the respiration condition is impossible [8, 9]. Due to increasing number of asthmatic patients at present, there is a growing demand for automatic monitoring of the wheeze to assist the physicians in diagnosing and monitoring the patient. For asthmatic patients, continuous and automatic monitoring is essential as the daily symptoms can provide crucial information to the medical diagnosis [8]. Therefore, the electronic stethoscope, which is capable of recording and storing lung sounds, is available for many years now. This stethoscope can not only store the data obtained, but such data can be retrieved in future to aid in the interpretation of disease by medical personnel [10]. However, the problem seems to amplify as different physicians interpret the lung sounds differently. To overcome these problems, computerized approach has been developed over the past three decades for automated wheeze detection [11]. It is a bit time-consuming, but low in cost and reliable. Many researchers were involved in developing and improving these automated systems and many have succeeded in their research. A survey of literature shows that the main methodologies can roughly be classified into two categories: Fourier peaks detection and spectrogram image analysis. This review paper is organized as follows. In methodology section, we present how articles have been searched and selected for the review in this paper. In the results section, information from all the chosen papers is summarized in a tabular form and an explanation on the content of these papers is given. In the following section, further discussion on the automated wheeze system based on the table developed is presented. And finally, in conclusion, we show how the system can be very beneficial for asthmatic patients. Some avenues for future work are also suggested.
MATERIALS AND METHODS
Samples and Methodology
A systematic search of articles published as early as 1985 to 2012 was conducted in Universiti Malaysia Perlis (UniMAP). Keywords that were used throughout the search are lung auscultation, lung sound, wheezes, crackle, adventitious sounds and others that are synonymous to the search criteria. Only papers with important information for automated wheeze detection and papers published in English only were reviewed. Some papers may have presented other adventitious sound together with wheezes but only wheeze detection method will be taken into consideration. Moreover, abstracts that have been published as workshop, conference or symposium proceedings were not be considered due to insufficient information presented in them.
RESULTS
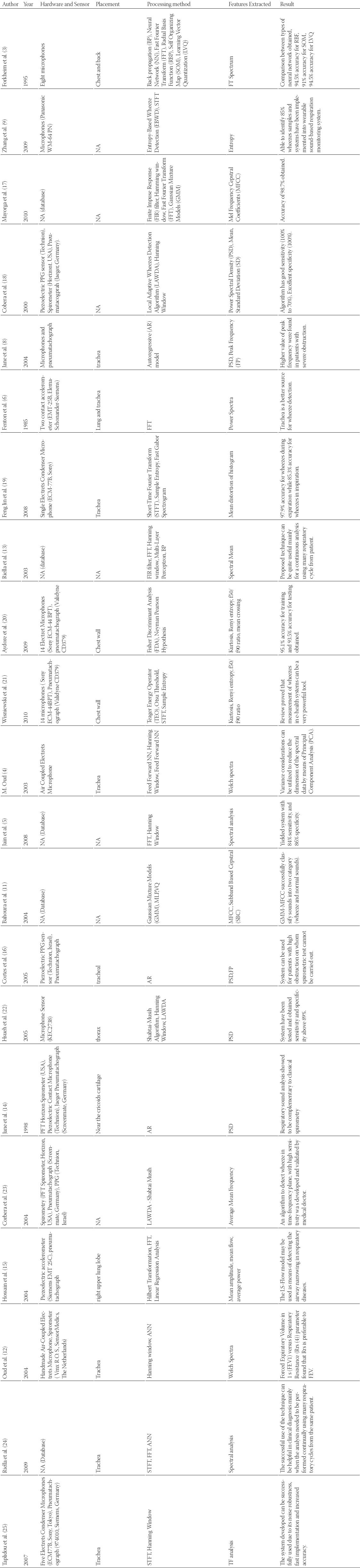
A total of 94 articles were found initially. After, elimination of duplicates and obviously irrelevant titles (n = 67), only 27 articles chosen for this systematic review (see Figure 1). From the total of 94 papers obtained, most of the discarded papers were not related to the discussed automated wheeze detection system. They included several other respiration sounds that are not related to asthma or their study design did not even include any wheezes present even though other lung sounds were discussed. None of the papers included in this systemic review were books or other reports not subject to peer review. From 27 papers chosen, only 21 articles which satisfied the selection criteria are discussed briefly in Table 1. As source of the data obtained is important in developing an automated system, we have listed all the hardware involved in data collection method. It is assured that data collected are from patients suffering from airway obstruction, which led to wheeze formation and the most are from asthmatic patients. No hardware is presented in case researchers used database as their data source. Listed hardware can be very useful for new researchers in developing new automated system for their research. In collecting the data, the placement of the auscultation hardware has been presented as well. This is due to that each point of data collection can result in different quality of the obtained signal. Wheezes have some characteristics that may produce a better signal for certain auscultation placement. Therefore, the placement of auscultation hardware presented may be very useful for collecting the best data for wheezes. The processing method together with the extracted feature used has been listed in Table 1. This seems to be the most crucial part in the successful of an automated system. A poor selection of the processing method and a feature to be extracted from data may cause a system to fail. Therefore, from the table, researchers will be able to choose the best processing method and a best feature to be extracted for a better automated system development. Result from every article may also act as a good reference for the system to be developed.
FIGURE 1.
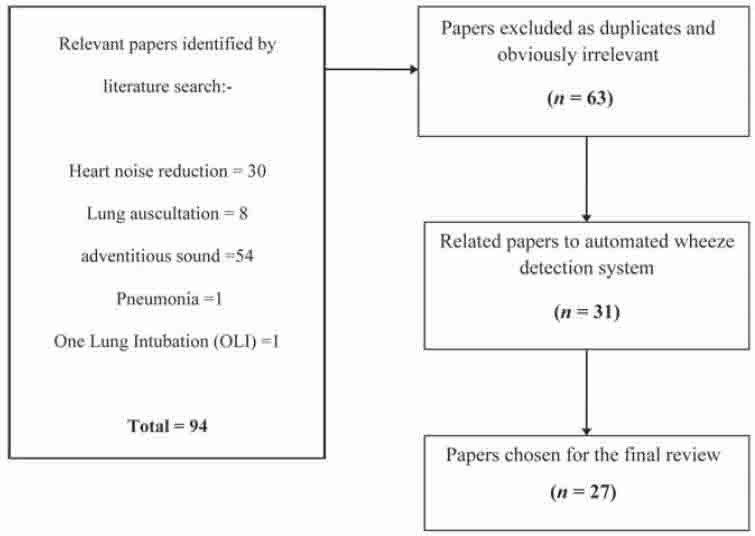
Illustration of studies identified and their management
TABLE 1.
An overview of developed wheeze automated systems
DISCUSSION
The authors strongly believe that this article is first of its kind since no previous work on summarizing the previous research on automatic wheeze detection systems beneficial seems to be available. In this section, the data collection procedures and the data processing methods by previous researchers are discussed. Few recommendations based on the analysis from the previous work are also suggested.
Data Collection
Nowadays, there are several methods used clinically in detecting wheeze. Methods such as spirometer and other pulmonary function tests are widely used. For an example, Jane et al. [14] in their studies have proved that respiratory sound analysis complementary to the classical spirometry has showed that the automated system can also be reliable as a pulmonary test for detecting wheeze. These methods are time-consuming and also extra effort is needed on part of the patient for such tests. The simplest method to detect wheeze is using microphone mounted on a stethoscope. This method is non-invasive and not time-consuming. This has drawn much attention from researchers to develop automated wheeze detection system. Since automated auscultation technique is not yet implemented in current medical application, the use of current pulmonary function test along with acoustic analysis can improve the reliability of such automated system. While, Hossain [15] have introduced the lung sound-flow rate model that can be used for the detection of airway narrowing occurring in asthmatic patients, Cortes and team [16] in their work proved the unnecessary of using the additional details together with lung sounds. They have successfully developed a system to assist the patient on whom spirometric test cannot be carried out by solely using lung sound signal. From Table 1, it can be observed that most of the previous researchers have collected data by placing the microphone over the trachea region [2, 4, 6, 10, 14, 17, 22, 23]. Riella et al. [12] stressed the reliability of the trachea to be a better location for analyzing wheezes than the lung while Oud et al. [13] claimed that trachea is reliable because all air-propagated lung sound from the two lungs integrates in trachea. Moreover, more frequency information is preserved at the trachea, as the chest wall filters out higher frequencies [12]. This shows that the trachea is the most favorable and reliable position for wheeze data collection.
Data Processing
There are several methods being used by the previous researchers to process the lung sounds for detecting wheeze. The lung sounds are either processed in time domain or frequency domain. The lung sounds are non-stationary and nonlinear. Therefore, analyzing the lung sounds in the time–frequency domain will be more helpful for getting valuable information from the non-stationary signals [26]. Regardless the usefulness of time-frequency domain for analyzing lung sounds, very few researchers have used the methods according to Table 1. The work of Taplidou et al. [25] is the only work being carried out using time-frequency domain. For recognizing the wheeze, the previous researchers have opted to use statistical analysis or machine learning methods. Method such as Fisher Discriminant Analysis (FDA), kurtosis and linear regression analysis are the most commonly used for statistical analysis while neural network (NN), radial basis function (RBP), learning vector quantization (LVQ), Gaussian mixture models (GMM), fast Fourier transform are the most commonly used for machine learning methods. Methods such as genetic algorithm, support vector machine, and practical swarm optimization are yet to be explored in developing the wheeze detection system. The researchers also have not yet touched upon the area of hybrid machine learning algorithm in the detection of wheezes. Hybrid algorithms such as neuro-fuzzy, genetic fuzzy systems, evolutionary neural networks etc, have proved to be effective with other applications [27]. It is recommended to use such algorithms for wheeze detection in the future. As far as the extracted feature are concerned, various type of features have been used by the previous researches such as time-frequency spectrum, entropy, Mel frequency ceptral coefficients (MFCC), power spectral density (PSD), Mean, standard deviation (SD), Peak Frequency (FP), kurtosis, mean crossing, welch spectra, and subband based cepstral (SBC) [3, 4, 8, 9, 11, 17, 19, 21]. It is impossible to choose which features is the best to be extracted, this is because by using the same feature, a system performance can be differ with each other due to different signal processing and classification technique applied. For an example, Corbera et al. [19] successfully obtained 100% specificity while Hsueh et al. [22] only managed to obtained 89% specificity for their system eventhough both of the system uses PSD [19, 22]. Moreover, the higher specificity obtained by Corbera et al. also due to the use of PSD together with SD features resulting a better result for their system. From Table 1, can observed that the most feature used is PSD [6, 8, 14, 16, 18, 22].
CONCLUSION
This review provides an insight on automatic wheeze detection systems developed by previous researchers and its potential in both clinical and research setting. The literature review was carried out on the 27 articles that satisfied the selection criteria. A brief summary on the 21 out of 27 articles was tabulated. The table clearly discussed the hardware used, sensor placement, data processing methods, feature extraction methods and important outcome of the 21 articles. A brief discussion was done based on the previous works on automated wheeze detection system. Few recommendations on the placement of the sensor and methods that can be applied in future research were also discussed. The research on the developed system has been carried out for the past three decades. Even though wheeze detection systems have been successfully implemented, they are only at research level and still commercially available real-time wheeze detection system is yet to be developed. Therefore, the future researchers are encouraged to develop commercial system that will improve the diagnosis of wheeze in clinical environment.
DECLARATION OF INTEREST
We confirm that this manuscript has not been published elsewhere and is not under consideration by another journal. All authors have approved the manuscript and agree with submission to the Journal of the Association of Basic Medical Sciences of Federation of Bosnia and Herzegovina. The authors have no conflicts of interest to declare.
REFERENCES
- [1].Nikšić D, Saračević E, Ćemerlić-Kulić A, Kurspahić-Mujčić A, Bajraktarević S, Nikšić H. Evaluation of efficiency practical issues in the management of childhood asthma. Bosn J Basic Med Sci. 2005;5(4):40–5. doi: 10.17305/bjbms.2005.3229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mehmedagić A, Vranić E, Hadžović S, Pokrajac M, Milić J, Mehić B, Zutic H, Konjicija A. The new trends in theophylline therapy. Bosn J Basic Med Sci. 2002;2(1-2):62–65. doi: 10.17305/bjbms.2002.3584. [DOI] [PubMed] [Google Scholar]
- [3].Forkheim, Kevin E, Scuse D, Pasterkamp H. Vol. 1. WESCANEX 95 Communications, Power, and Computing Conference Proceedings, IEEE; 1995. A comparison of neural network models for wheeze detection; pp. 214–219. [Google Scholar]
- [4].Oud M. Lung function interpolation by means of neural-network-supported analysis of respiration sounds. Med Eng Phys. 2003;25(4):309–316. doi: 10.1016/s1350-4533(02)00198-4. [DOI] [PubMed] [Google Scholar]
- [5].Jain A, Vepa J. 30th Annual International Conference of the IEEE on Engineering in Medicine and Biology Society; 2008. Lung sound analysis for wheeze episode detection; pp. 2582–2585. [DOI] [PubMed] [Google Scholar]
- [6].Fenton T.R, Pasterkamp H, Tal A, Chernick V. 1. Vol. 32. IEEE Transactions on Biomedical Engineering; 1985. Automated spectral characterization of wheezing in asthmatic children; pp. 50–55. [DOI] [PubMed] [Google Scholar]
- [7].Parkhi A, Pawar M, editors. International Conference on Computational Intelligence and Communication Networks (CICN) IEEE; 2011. Analysis of Deformities in Lung Using Short Time Fourier Transform Spectrogram Analysis on Lung Sound; pp. 177–181. [Google Scholar]
- [8].Jané R, Cortés S, Fiz J, Morera J, editors. 26th Annual International Conference of the IEEE on Engineering in Medicine and Biology Society, IEMBS’ 04; 2004. Analysis of wheezes in asthmatic patients during spontaneous respiration; pp. 3836–3839. [DOI] [PubMed] [Google Scholar]
- [9].Zhang J, Ser W, Yu J, Zhang T, editors. A novel wheeze detection method for wearable monitoring systems. International Symposium on Intelligent Ubiquitous Computing and Education IEEE; 2009. pp. 331–334. [Google Scholar]
- [10].Marshall A, Boussakta S, Pearson S. The 3rd IEEE International Seminar on Medical Applications of Signal Processing; 2005. Applications of signal recognition algorithms to diagnosis and monitoring in chest medicine; pp. 121–124. [Google Scholar]
- [11].Bahoura M, Pelletier C, editors. Vol. 3. Canadian Conference on Electrical and Computer Engineering IEEE; 2004. Respiratory sounds classification using Gaussian mixture models; pp. 1309–1312. [DOI] [PubMed] [Google Scholar]
- [12].Oud M, Maarsingh E. Spirometry and forced oscillometry assisted optimal frequency band determination for the computerized analysis of tracheal lung sounds in asthma. Physiol Meas. 2004;25(3):595–606. doi: 10.1088/0967-3334/25/3/001. [DOI] [PubMed] [Google Scholar]
- [13].Riella R, Nohama P, Borges R, Stelle A, editors. Vol. 3. Proceedings of the 25th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2003. Automatic wheezing recognition in recorded lung sounds; pp. 2535–2538. [Google Scholar]
- [14].Jané R, Salvatella D, Fiz J, Morera J, editors. Vol. 6. Proceedings of the 2th Annual International Conference on Engineering in Medicine and Biology Society; 1998. Spectral analysis of respiratory sounds to assess bronchodilator effect in asthmatic patients; pp. 3203–3206. [Google Scholar]
- [15].Hossain I, Moussavi Z, editors. Vol. 2. 26th Annual International Conference of the IEEE on Engineering in Medicine and Biology Society, IEMBS’ 04; 2004. Finding the lung sound-flow relationship in normal and asthmatic subjects; pp. 3852–3855. [DOI] [PubMed] [Google Scholar]
- [16].Cortes S, Jané R, Fiz J, Morera J, editors. Monitoring of wheeze duration during spontaneous respiration in asthmatic patients. 27th Annual International Conference of the IEEE on Engineering in Medicine and Biology Society, IEEE-EMBS; 2005. pp. 6141–6144. [DOI] [PubMed] [Google Scholar]
- [17].Mayorga P, Druzgalski C, Morelos R, Gonzalez O, Vidales J, editors. Annual International Conference of the IEEE on Engineering in Medicine and Biology Society (EMBC); 2010. Acoustics based assessment of respiratory diseases using GMM classification; pp. 6312–6316. [DOI] [PubMed] [Google Scholar]
- [18].Homs-Corbera A, Jané R, Fiz J.A, Morera J, editors. Vol. 4. Proceedings of the 22nd Annual International Conference of the IEEE on Engineering in Medicine and Biology Society; 2000. Algorithm for time-frequency detection and analysis of wheezes; pp. 2977–2980. [Google Scholar]
- [19].Jin F, Sattar F, Goh D.Y.T, editors. 30th Annual International Conference on Engineering in Medicine and Biology Society, 2008 EMBS; 2008. Automatic wheeze detection using histograms of sample entropy; pp. 1890–1893. [DOI] [PubMed] [Google Scholar]
- [20].Aydore S, Sen I, Kahya Y.P, Mihcak M.K, editors. Classification of respiratory signals by linear analysis. Annual International Conference on Engineering in Medicine and Biology Society IEEE, EMBC; 2009. pp. 2617–2620. [DOI] [PubMed] [Google Scholar]
- [21].Wisniewski M, Zielinski T, editors. International Conference on Signals and Electronic Systems IEEE (ICSES); 2010. Digital analysis methods of wheezes in asthma; pp. 69–72. [Google Scholar]
- [22].Hsueh M.L, Chien J.C, Chang F.C, Wu H.D, Chong F.C, editors. 27th Annual International Conference of the Engineering in Medicine and Biology Society, 2005 IEEE-EMBS; 2006. Respiratory wheeze detection system; pp. 7553–7559. [DOI] [PubMed] [Google Scholar]
- [23].Homs-Corbera A, Fiz J.A, Morera J, Jané R. 1. Vol. 51. IEEE Transactions on Biomedical Engineering; 2004. Time-frequency detection and analysis of wheezes during forced exhalation; pp. 182–186. [DOI] [PubMed] [Google Scholar]
- [24].Riella R, Nohama P, Maia J. Method for automatic detection of wheezing in lung sounds. Braz J Med Biol Res. 2009;42(7):674–684. doi: 10.1590/s0100-879x2009000700013. [DOI] [PubMed] [Google Scholar]
- [25].Taplidou S.A, Hadjileontiadis L.J. Wheeze detection based on time-frequency analysis of breath sounds. Comput Biol Med. 2007;37(8):1073–1083. doi: 10.1016/j.compbiomed.2006.09.007. [DOI] [PubMed] [Google Scholar]
- [26].Kandaswamy A, Kumar C.S, Ramanathan R.P, Jayaraman S, Malmurugan N. Neural classification of lung sounds using wavelet coefficients. Comput Biol Med. 2004;34(6):523–537. doi: 10.1016/S0010-4825(03)00092-1. [DOI] [PubMed] [Google Scholar]
- [27].Yang J.Y, Yang M.Q, Luo Z, Ma Y, Li J, Deng Y, et al. A hybrid machine learning-based method for classifying the Cushing's Syndrome with comorbid adrenocortical lesions. BMC Genomics. 2008;9(Suppl 1):S23. doi: 10.1186/1471-2164-9-S1-S23. [DOI] [PMC free article] [PubMed] [Google Scholar]


