Abstract
Objectives
To evaluate the impact of birth attendant training using the World Health Organization Essential Newborn Care (ENC) course among traditional birth attendants, with a particular emphasis on the effect of acquisition of skills on perinatal outcomes.
Design
Population-based, prospective, interventional pre-post design study.
Setting
11 rural clusters in Chimaltenango, Guatemala.
Population
Health care providers.
Methods
This study analyzed the effect of training and implementation of the ENC health care provider training course between September 2005 and December 2006.
Outcome measures
The primary outcome measure was the rate of death from all causes in the first seven days after birth in fetuses/infants ≥1500g. Secondary outcome measures were overall rate of stillbirth, rate of perinatal death, which included stillbirths plus neonatal deaths in the first seven days in fetuses/infants ≥1500g.
Results
Perinatal mortality decreased from 39.5/1000 pre-ENC to 26.4 post-ENC (RR 0.72; 95%CI 0.54–0.97). This reduction was attributable almost entirely to a decrease in the stillbirth rate of 21.4/1000 pre-Essential Newborn Care to 7.9/1000 post-ENC (RR 0.40; 95%CI 0.25–0.64). Seven-day neonatal mortality did not decrease (18.3/1000 to 18.6/1000; RR 1.05; 95%CI 0.70–1.57).
Conclusion
Essential Newborn Care training reduced stillbirths in a population-based controlled study with deliveries conducted almost exclusively by traditional birth attendants. Scale-up of this intervention in other settings might help assess reproducibility and sustainability.
Keywords: Developing countries, newborn care, perinatal mortality, stillbirths, traditional birth attendants
Introduction
More than 98% of the estimated 3.7 million neonatal deaths and 3.2 million stillbirths per year occur in low- and middle-income countries (1). Although childhood mortality has decreased in recent years, neonatal mortality has remained steady or even increased in many low- and middle-income countries (2). In these countries, the majority of neonatal deaths occur within the first seven days after birth and as many as one third to one half of all deliveries occur in home settings, either unattended by any type of health care provider or attended by traditional birth attendants (TBAs) (2).
Addressing the high infant mortality and morbidity rates has been a priority of the World Health Organization (WHO) for a number of years. The Essential Newborn Care (ENC) course was developed by the WHO to teach the evidence-based newborn care guidelines (3). The five-day course consists of didactic and practice sessions addressing the ENC topics of cleanliness, routine care of the baby at and following delivery, examining the baby, thermoregulation, breastfeeding, effective communication skills, resuscitation, care for the small baby, and kangaroo mother care, as well as recognition and initial management of complications.
The study reported here was a component of a larger protocol involving six low- and middle-income country populations participating in the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD) Global Network for Women’s and Children’s Health Research. The parent study comprising combined data from all sites has been published (4). A separate report of the intervention outcomes in the Western Highlands of Guatemala is of importance because of the very high proportion of births attended by poorly educated TBAs in this population and the unanticipated outcomes in a study that was not powered on an individual site basis.
The objective of this study was to evaluate the impact of birth attendant training using the WHO ENC course, with particular emphasis on the effect of acquisition of skills on perinatal outcomes among deliveries conducted by TBAs. Our hypothesis was that ENC training would decrease perinatal and early neonatal (<seven days of age) mortality in fetuses/infants ≥1500g in deliveries attended by TBAs in Guatemala.
Material and methods
The study used a population-based, prospective, interventional, pre-post design to assess the effect of training and implementation of the ENC health care provider training course conducted in 11 rural clusters in Chimaltenango, Guatemala, between September 2005 and December 2006. The clusters were selected to be representative of rural areas, to be geographically distinct, and to have 300–500 births per year. The study included all births in the geographic area, including deliveries at public and private health clinics and hospitals as well as home births. Government officials and community leaders in these communities agreed to facilitate the training of all birth attendants in the protocol, data collection, and ENC course and to allow them to obtain consent and data collection. The study was approved by the inter-institutional ethics review committee at INCAP (Instituto de Nutrición de Centro América y Panamá), Research Triangle International, University of Alabama at Birmingham, and the University of Colorado Denver. Informed consent was obtained from the mothers. An independent Data Monitoring Committee appointed by the NICHD reviewed recruitment and adverse events. This trial (NCT00136708) is registered with Clinical-Trials.gov.
A six-month prospective baseline period allowed for enrollment of all pregnant women in the study clusters (Figure 1). A train-the-trainers educational program was developed using a variety of teaching methods, including clinical practice sessions and demonstrations. The goal was to train all birth attendants working within each cluster in the study procedures. Country trainers trained and certified one community coordinator (auxiliary nurses with middle or high school education and 10 months of nursing school) in each of the 11 communities during a five-day period. In turn, the community coordinators trained the practicing birth attendants within each community in all procedures, which included evaluation of clinical condition of newborns, specifically the differentiation between stillbirths and live-born infants, and evaluation of Apgar scores. Birth attendants included TBAs, nurses, nurse-midwives, and physicians. Following the pre-ENC data collection period, all practicing birth attendants in the geographic area were trained in ENC and post-ENC data were collected (Figure 1). Six of these clusters went on to receive NRP training, as part of the 43 of 96 clusters in the larger study. These data are not included in the present analyses.
Figure 1.
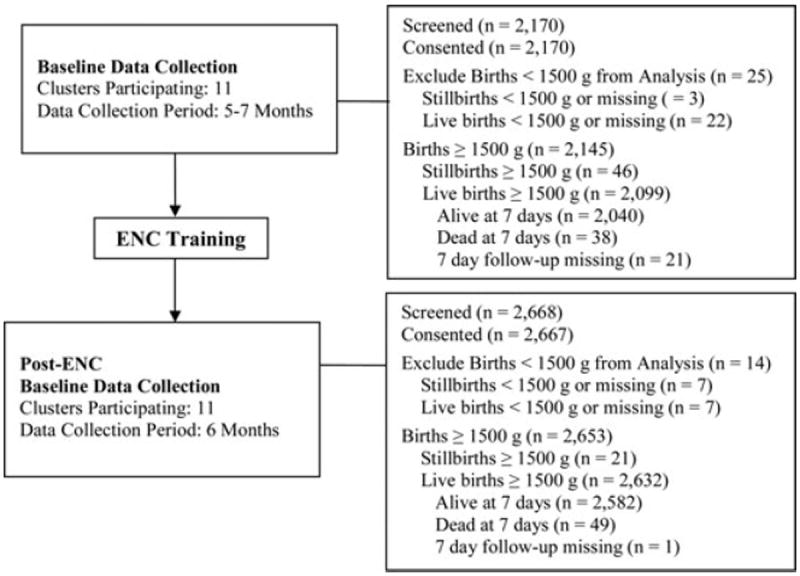
Consort diagram.
An experienced WHO trainer (Ornella Lincetto, MD) conducted the initial ENC training (three days) of the country trainers. Educational materials utilizing clear drawings in lieu of most text were developed locally for the TBA training. Spanish-Cakchiquel (local dialect) translators collaborated in the training process as necessary. During the TBA training, more than 60% of the training time was devoted to practice and acquisition of skills. Additionally, study activities allowed for one-on-one monitoring and follow-up in clinical contexts in the field. Community coordinators worked with TBAs on an ongoing basis over a period of several months to ensure that the acquired skills were put into practice adequately.
Data describing maternal health, pregnancy, delivery, and neonatal variables and exposures, and seven-day outcomes were collected. Auxiliary nurses visited the homes of mothers in the first 24 hours after birth and recorded the information provided to them by the TBAs. Data analyses were limited to the fetuses/neonates with birth weights ≥1500g (or appearing to be ≥1500g if weighing was not possible). Seven-day outcomes were collected on day of life 7±1.
Six ± one month of baseline data were collected prior to initiation of the training period (pre-ENC). Post-ENC data were collected for a further six months. The community coordinators and birth attendants collected all data on standardized data forms (pictorial versions of the same forms were available for the illiterate/semiliterate birth attendants) using numbered patient identifiers. Data forms were reviewed for accuracy by the community coordinators before submission to the local research office for data entry and transmission to the data coordinating center (Research Triangle International, NC, USA). Data edits, including inter- and intra-form consistency checks, were performed upon data entry at each research site with additional edits performed centrally by the data coordinating center.
Generalized estimating equation (GEE) extensions of logistic and proportional odds regression models that adjust for correlation of outcomes within cluster were used to determine differences in maternal and neonatal characteristics between the pre-ENC training and post-ENC training. Logistic models were used for binary data, proportional odds models with cumulative logit were used for ordered multinomial variables, and generalized logit multinomial models were used for nonordered multinomial variables. Adjusted relative risks (RR) and 95% confidence intervals (CI) using GEE extensions of multivariate log-binomial models are reported for the post- vs. the pre-comparison of the effect of training in ENC. The data were analyzed using STATISTICAL ANALYSIS software version 9.2 (SAS, Cary, NC).
Results
The majority of birth attendants were TBAs; 522 TBAs, 10 physicians and 12 nurse/nurse midwives participated in the study (Table 1). The TBAs ranged in age from 15 to 100 years of age. Thirty-three percent of the TBAs were literate. The average number of births attended by each TBA per month ranged from 0 to >20. Most practiced in a geographically defined area close to their home, but others travelled up to 10km to provide services (data not shown).
Table 1.
Neonatal and demographic characteristics.
| Pre-ENC Communities | Post-ENC Communities | p-value* | |
|---|---|---|---|
| Number of deliveries | 2129 | 2637 | |
| Birth attendant type | 2 129 | 2 637 | 0.17 |
| Physician | 8 (0.4) | 5 (0.2) | |
| Nurse/midwife | 5 (0.2) | 6 (0.2) | |
| TBA | 2 107(99.0) | 2 624 (99.5) | |
| Family/unattended/other | 9 (0.4) | 2 (0.1) | |
| Number of infants | 2145 | 2653 | |
| Multiple birth | 32 (1.5) | 32 (1.2) | 0.61 |
| Gender | 2 129 | 2 652 | 0.78 |
| Male | 1 087 (51.1) | 1 344 (50.7) | |
| Female | 1 042 (48.9) | 1 308 (49.3) | |
| Bag and mask ventilation | 1 (0.0) | 35 (1.3) | 0.01 |
p-values are not adjusted for cluster.
Neonatal and demographic characteristics of the birth cohorts were collected during the baseline period of data collection (pre-ENC) and after ENC training (post-ENC). Nearly all deliveries (more than 99%) were conducted by TBAs and in a home setting. Neonatal characteristics, including gender, were comparable between the two time periods (Table 1). In the pre-ENC period, only one of the 2145 infants was resuscitated with bag and mask ventilation compared with 35/2653 in the post-ENC period (p=0.01). Perinatal mortality decreased from 39.5/1000 pre-ENC to 26.4/1000 post-ENC (RR 0.72; 95%CI 0.54–0.97) (Table 2). This was attributable almost entirely to a decrease in the stillbirth rate of 21.4/1000 pre-ENC to 7.9/1000 post-ENC (RR 0.40; 95%CI 0.25–0.64) (Table 3). Seven-day neonatal mortality did not decrease (18.3/1000 to 18.6/1000; RR 1.05, 95%CI 0.70–1.57) (Table 4).
Table 2.
Perinatal mortality.
| Pre-ENC n (rate/1000) | Post-ENC n (rate/1000) | RR* (95%CI) | p-value | |
|---|---|---|---|---|
| Perinatal mortality | 84 (39.5)** | 70 (26.4) | 0.72 (0.54, 0.97) | 0.03 |
| Male | 49 (45.2) | 37 (27.5) | 0.67 (0.44, 1.02) | 0.06 |
| Female | 33 (31.8) | 33 (25.2) | 0.81 (0.61, 1.06) | 0.13 |
RR are adjusted for cluster using GEE modeling.
The gender in two perinatal deaths in the pre-ENC phase is missing.
Table 3.
Stillbirths.
| Pre-ENC, n (rate/1000) | Post-ENC, n (rate/1000) | RR* (95%CI) | p-value | |
|---|---|---|---|---|
| Stillbirth | 46 (21.4)** | 21 (7.9) | 0.40 (0.25, 0.64) | <0.001 |
| Fresh stillbirth | 42 (19.6) | 20 (7.5) | 0.43 (0.28, 0.68) | <0.001 |
| Macerated stillbirth | 4 (1.9) | 1 (0.4) | 0.21 (0.03, 1.81) | 0.16 |
| Male | 30 (27.6) | 11 (8.2) | 0.31 (0.18, 0.54) | <0.001 |
| Female | 15 (14.4) | 10 (7.6) | 0.56 (0.33, 0.95) | 0.03 |
RR are adjusted for cluster using GEE modeling.
The gender in one stillbirth in the pre-ENC phase is missing.
Table 4.
Seven-day neonatal mortality.
| Pre-ENC, n (rate/1000) | Post-ENC, n (rate/1000) | RR* (95%CI) | p-value | |
|---|---|---|---|---|
| Seven-day neonatal mortality | 38 (18.3)** | 49 (18.6) | 1.05 (0.70, 1.57) | 0.81 |
| Male | 19 (18.0) | 26 (19.5) | 1.15 (0.60, 2.20) | 0.68 |
| Female | 18 (17.6) | 23 (17.7) | 0.99 (0.65, 1.50) | 0.95 |
RR are adjusted for cluster using GEE modeling.
The gender in one neonatal death in the pre-ENC phase is missing.
Discussion
The goal of our study was to investigate the impact on perinatal mortality of ENC training of a cohort of birth attendants consisting almost entirely of TBAs. Following ENC training, we observed a decrease in perinatal mortality attributable to a decrease in stillbirths but no change in neonatal mortality. Our mortality rates are similar to those reported in many developing countries (2).
The decline in perinatal mortality does not appear to be attributable to a shift in the type of birth attendant, location of birth, birthweight distribution or other factors during the period of training. We speculate that the decline in stillbirths resulted from an increase of apparently stillborn infants receiving resuscitation techniques which were increasingly employed as birth attendants attempted resuscitation of all infants who were not macerated at birth. In countries with a high proportion of home deliveries, stillbirths often go unreported or are unreliably distinguished from early neonatal death (5). Misclassification of stillbirths and early neonatal deaths may be due to lack of knowledge by birth attendants as well financial or other burdens associated with a particular classification (4). Resuscitation training programs recommend initiation of resuscitation even if no signs of life are present at birth. In this study, the decrease in perinatal mortality following ENC training was not associated with an increase in neonatal deaths and therefore provided an overall benefit.
With the goal of strengthening the capacity of countries to provide essential neonatal interventions, the WHO developed the ENC course (3) for skilled birth attendants which includes evidence-based guidelines for initial management of neonates. Several studies have shown that ENC training increases the use of appropriate practices (6-10). However, most of these studies did not assess the impact of ENC education on perinatal outcomes, nor has the potential benefit of ENC training of TBAs generally been reported. One recent study from Zambia found a significant decrease in early neonatal mortality following TBA training (10).
In many countries, a significant proportion of births occur at home, attended only by TBAs. In the larger Chimaltenango region, nearly 60% of births occurred in the home and were attended by TBAs (11). Nationwide, 63 and 70% of births in rural and indigenous populations, respectively, are attended by TBAs in the home (11). The reported national neonatal mortality rate in Guatemala is 18/1000 and is similar for the Chimaltenango region. Although TBAs are routinely trained by the Ministry of Health two to three hours per month; this was the first experience of an intensive five-day training course followed by close supervision in the field. There has been considerable debate regarding the training of TBAs; however, studies have suggested benefit, especially in the context of a health system (12). The effectiveness of TBAs using neonatal resuscitation improved substantially following ENC training. Our data suggest that TBA training has the potential to be a high impact intervention. An evaluation of scale-up by training TBAs in other areas under local leadership could assist in determining whether the results are reproducible and sustainable. Training should focus on improving TBA perinatal practices and ensuring that all patients with complications are referred promptly to higher level medical facilities. The design of training programs should take into account any pertinent demographic, educational and linguistic characteristics of the TBAs.
Because many countries are unlikely to have sufficient numbers of trained birth attendants in the foreseeable future, training programs such as ENC could have an important role in reducing perinatal mortality. Training can be carried out by health personnel with limited training, such as auxiliary nurses, as shown in this study.
In conclusion, ENC training of TBAs was associated with a significant decrease in perinatal mortality in a population-based controlled study. These data suggest that TBA training can be highly effective in helping babies breathe.
Acknowledgments
Ana Garces had primary responsibility for study implementation, patient screening, enrollment, outcome assessment, preliminary data analysis and writing the manuscript. Elizabeth McClure participated in development of the protocol, outcome assessment and analytical framework for the study and contributed to the writing of the manuscript. Michael Hambidge and Nancy Krebs participated in outcome assessment, preliminary data analysis and analytical framework for the study and contributed to the writing of the manuscript. Manolo Mazariegos participated in outcome assessment, preliminary data analysis and analytical framework for the study. Linda Wright participated in protocol development, outcome assessment, preliminary data analysis and manuscript writing. Janet Moore contributed to the statistical analyses. Waldemar Carlo developed the protocol, participated in outcome assessment and analytical framework for the study and contributed to the writing of the manuscript. The Guatemalan Ministry of Health also collaborated closely with study implementation. All authors have read and approved the manuscript.
Funding
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD U01 HD040657 UCD; U01 HD043464 UAB; and U01 HD040636 RTI).
This trial (NCT00136708) is registered with ClinicalTrials.gov
Abbreviations
- ENC
Essential Newborn Care
- GEE
generalized estimating equation
- NICHD
National Institutes for Child and Human Development
- TBA
traditional birth attendants
- WHO
World Health Organization
Footnotes
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
References
- 1.Lawn JE, Lee AC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynaecol Obstet. 2009;107(Suppl 1):S5–18. doi: 10.1016/j.ijgo.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Cousens S, Zupan J. Four million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Essential newborn care. Geneva: WHO; 1996. Contract No.: WHO/FRH/MSM/96.13. [Google Scholar]
- 4.Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362:614–23. doi: 10.1056/NEJMsa0806033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Org. 2005;83:409–17. [PMC free article] [PubMed] [Google Scholar]
- 6.Vidal SA, Ronfani L, da Mota Silveira S, Mello MJ, dos Santos ER, Buzzetti R, et al. Comparison of two training strategies for essential newborn care in Brazil. Bull World Health Org. 2001;79:1024–31. [PMC free article] [PubMed] [Google Scholar]
- 7.Uxa F, Bacci A, Mangiaterra V, Chiaffoni GP. Essential newborn care training activities: 8 years of experience in Eastern European, Caucasian and Central Asian countries. Semin Fetal Neonatal Med. 2006;11:58–64. doi: 10.1016/j.siny.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Carlo W, McClure E, Chomba E, Chakraborty H, Harris H, Lincetto O, et al. Impact of World Health Organization (WHO) Essential Newborn Care Course (ENC) Training: A Multicenter Study. San Francisco: Pediatric Academic Societies; 2006. p. 2806.203. [Google Scholar]
- 9.McClure EM, Carlo WA, Wright LL, Chomba E, Uxa F, Lincetto O, et al. Evaluation of the educational impact of the WHO Essential Newborn Care course in Zambia. Acta Paediatr. 2007;96:1135–8. doi: 10.1111/j.1651-2227.2007.00392.x. [DOI] [PubMed] [Google Scholar]
- 10.Gill CJ, Phiri-Mazala G, Guerina NG, Kasimba J, Mulenga C, MacLeod WB, et al. Effect of training traditional birth attendants on neonatal mortality (Lufwanyama Neonatal Survival Project): randomised controlled study. Br Med J. 2011;342:d346. doi: 10.1136/bmj.d346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Survey on Maternal and Child Health. Guatemala City: Del Valle University; 2010. [Google Scholar]
- 12.Sibley LM, Sipe TA, Brown CM, Diallo MM, McNatt K, Habarta N. Traditional birth attendant training for improving health behaviours and pregnancy outcomes. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD005460.pub2. CD005460. [DOI] [PubMed] [Google Scholar]


