Rabies and Ebola are viruses of the order Mononegavirales, being single-stranded negative sense RNA viruses. Rabies virus, of the family Rhabdoviridae, genus Lyssavirus, consists of 5 genes, which encode for the membrane-associated proteins: matrix (M) and glycoprotein (G); and the structural proteins: nucleoprotein (N), phosophoprotein (P) and polymerase (L) (4, 31). Ebola virus, of the family Filoviridae, consists of 7 genes, which encode for the membrane-associated proteins: matrix (VP40), minor matrix (VP24) and glycoprotein (GP); and the structural proteins: minor nucleoprotein (VP30), nucleoprotein (NP), polymerase cofactor (VP35) and polymerase (L) (10, 29).
The viral glycoproteins have similar functions for the members of the Mononegavirales. Rabies virus (RABV) G facilitates entry into permissive cells, enables cell-to-cell spread of the virus, and supports budding of the virion from the host cell membrane (5, 19, 23, 26). Similarly, EBOV GP is necessary for virion entry and fusion to release the viral capsid (11, 15, 21, 30). Both RABV G and EBOV GP are highly immunogenic, and antibodies generated against these proteins can neutralize virus and block infection (2, 7, 14). RABV neutralizing antibodies toward G are the host’s primary defense against the invading pathogen (9, 26), and pre-exposure vaccination is effective in preventing an otherwise potentially lethal disease (13). Moreover, the passive application of antibodies against RABV G in combination with an active immunization schedule with killed RABV virions successfully prevents rabies after infection when administered appropriately (16). Recent results indicate that, during EBOV infection, CD4+ and CD8+ T cells had a minimal role in providing protection, while anti-GP antibodies induced by the vaccine appeared to be critical for protecting the animals (14).
While Ebola is not a widespread or chronic disease, its pathogenicity, virulence and transmission have generated interest in a vaccine for military and biodefense purposes (12, 24). The current outbreak in West Africa has highlighted the need for an EBOV vaccine. RABV has been shown as an exceptional vaccine vector for multiple antigens including EBOV (6, 20, 27, 28), and RABV is also endemic in areas where EBOV is found. Therefore, a RABV virus that expresses the Ebola GP is an attractive vaccine candidate. Based on our previous research and findings concerning the importance of the elicitation of neutralizing antibodies for protection, the expression of G and GP in our bivalent vaccine is critical to its success (2, 7, 15, 18). In a previous study, our G-deleted RABV expressing GP (RVΔG-GP) provided 50% protection against EBOV challenge in NHPs as compared to 100% protection conferred by the replication competent version of the vaccine. If RVΔG-GP can be optimized for immunogenicity to provide 100% protection from EBOV challenge, it would be an ideal vaccine choice based on safety and efficacy data. Controlled growth is a key safety feature for the potential marketability of this live RABV vaccine. The growth of RVΔG-GP is controlled via an efficient on/off gene expression system. RVΔG-GP was recovered and grown in BSR cells (a hamster kidney cell (BHK) line expressing RABV G (BSR-G)), where G expression is regulated by a Tet-off reporter gene system (3, 8). Whereas VeroE6 cells are approved for production of rabies vaccines (1), it is anticipated that RVΔG-GP would be manufactured on a newly developed VeroE6 cell line expressing G via the same mechanism as BSR-G cells, provided that RVΔG-GP does not grow on VeroE6 alone.
Our goal in this study was to further elucidate the mechanism whereby viral growth is restricted. In so doing, we sought to ensure the safety of the vaccine during future large-scale production on VeroE6 cells, as we had concerns about the functions of residual G and the utilities of GP. Growth limitation of RVΔG-GP based on withholding RABV G has been demonstrated in vitro, and western blotting of virus proteins confirmed the absence of G and presence of GP for our construct (3). Previous studies have shown that RVΔG-GP grows to similar titers as its replication-competent counterpart RVGP, when grown in BSR-G cells, but no infectious RABV is detected when VeroE6 cells are infected (22). We wanted to confirm the lack of growth of infectious virus on VeroE6 cells by multiple methods to answer questions that arose during the development of this vaccine, namely whether: 1) residual G in the supernatant from growth on BSR-G cells permits RVΔG-GP to replicate in VeroE6 cells; 2) RVΔG-GP grows on VeroE6 cells by substituting GP for G, as similar results have been shown for VSV (25). Overall, we sought to determine if the safety profile of RVΔG-GP supports its further optimization and large-scale production for vaccine manufacture.
The recovery and propagation of the recombinant vaccine viruses used in this study have been described previously (3, 17, 22). BSR cells were originally derived from BHK-21 cells; BSR-G cells stably express RABV G after stimulation with doxycycline (8). VeroE6 cells were from ATCC (CRL-1586). Both cell lines were cultured in DMEM (Gibco) supplemented with 10% FBS (Hyclone).
We previously established that no infectious RVΔG-GP is found in supernatant from growth curves on VeroE6 cells via focus forming assay based on RABV N detection (22). To determine the capability of the virus to spread on VeroE6 cells by utilizing GP or residual G from stock preparation on BSR-G cells, we utilized qRT-PCR, confocal microscopy and electron microscopy to analyze RVΔG-GP passaged on VeroE6 and BSR-G cells.
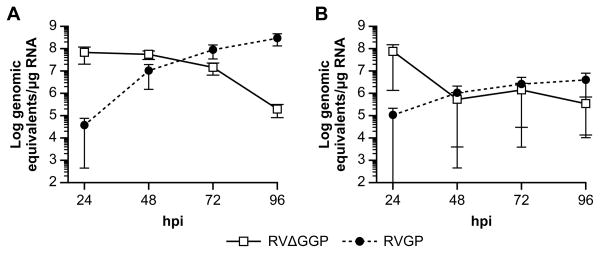
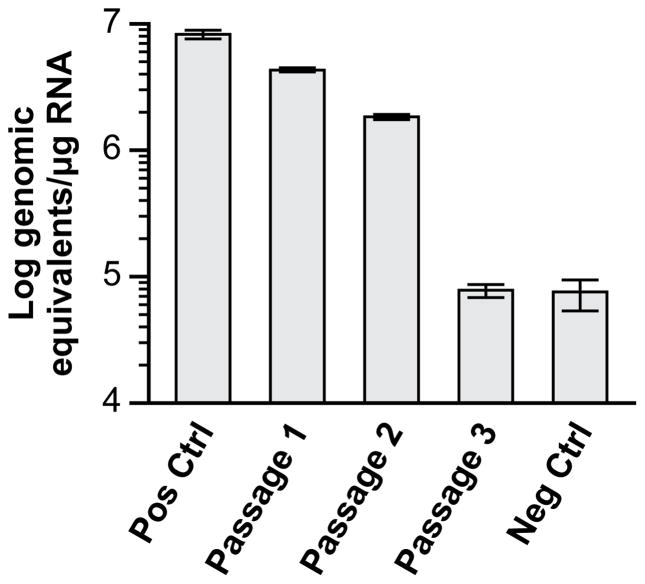
Here, we demonstrate that RVΔG-GP viral genomic RNA can be detected via qPCR at similar levels as RVGP after direct infection of VeroE6 cells (Fig 1). The fact that the level of RABV N genomic material present is comparable for RVΔG-GP on either BSR-G or VeroE6, yet the virus fails to spread from cell to cell in VeroE6, indicates a failure in the assembly or budding of the virion from the cell after entry. To emphasize that RVΔG-GP is not capable of regaining the ability to propagate in VeroE6, we performed a serial passage experiment in VeroE6 (Fig 2). The data suggest that while the starting material RVΔG-GP for the growth curve was infectious, it was not able to propagate and by the third passage RABV N RNA was equal to the negative control. qRT-PCR was performed as follows. RNA was derived from infected cells at indicated timepoints using an RNeasy kit (Qiagen). Reverse transcription was performed using a Transcriptor High Fidelity cDNA Synthesis Kit (Roche) with primer RP381 (5-ACACCCCTACAATGGATGC-3) for RABV N synthesis. Real-time PCR was performed on an ABI7900HT Fast machine using a Dynamo Probe qPCR kit (ThermoScientific). Two replicates were performed in duplicate. The following primers and probes were used: RABV N RNA sense primer (5-AGAAGGGAATTGGGCTCTG-3), RABV N RNA antisense primer (5-TGTTTTGCCCGGATATTTTG-3), RABV N RNA probe (5-CGTCCTTAGTCGGTCTTCTCTTGAGTCTGT-3). Custom primers and probes were purchased from Applied Biosystems.
Figure 1.
Quantitative PCR to detect RABV nucleoprotein over time in a multi-step growth curve (moi 0.01). Data points are log mean genomic equivalents per microgram of total RNA (n=2) with SEM error bars. RVΔGGP, □;RVGP, ●. Viral genome replication was not statistically different on A) BSR-G and B) VeroE6 cells for either virus (n=2; Student’s t test, p=0.35 and 0.24 respectively).
Figure 2.
Quantitative PCR to detect RABV nucleoprotein upon serial passage of RVΔGGP on VeroE6 cells. Viral supernatant was passaged at 48h post-infection. Bars are log mean genomic equivalents per microgram of total RNA (n=2) with SEM error bars. Positive control is RNA from the RVΔGGP stock used to infect for passage 1. Negative control is an irrelevant RNA.
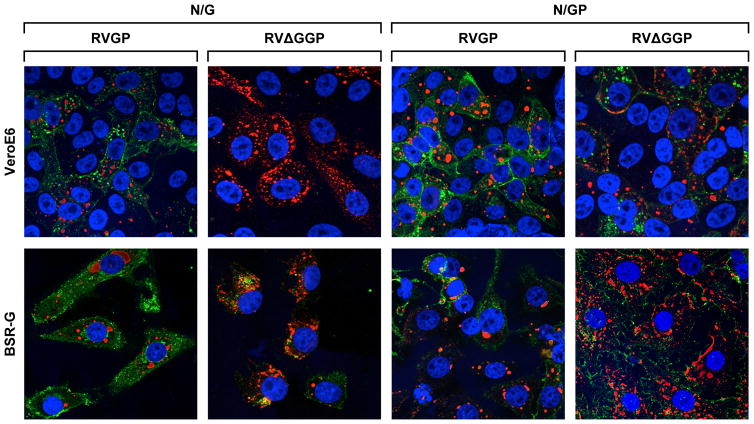
To corroborate these results, RVGP and RVΔG-GP infected Vero E6 and BSR cells were analyzed at 48h post-infection via confocal microscopy. Expression of viral proteins RABV N, G, and EBOV GP was detected using a dual staining method for either RABV N and RABV G or RABV N and EBOV GP (Table 1 and Fig 2). Staining for all three antibodies at once was attempted; however, background fluorescence was increased, and image detail suffered. Therefore, the experiment was performed using the dual staining method as illustrated. Briefly, cells were seeded on glass coverlips in 12 well plates on day 0. On day 1, cells were infected at an MOI of 1 with either RVGP or RVΔG-GP using cellgro Complete serum free media (Mediatech) and incubated for 48h at 37°C/5%CO2. Media was then removed, and wells were gently washed with PBS. Cells were fixed using 4% paraformaldehyde for 20min at RT. Fixed cells were washed 3X with PBS, then blocked and permeabilized in PBS with 1% BSA, 0.3M Glycine and 0.1% Triton X-100 for 1h at RT. Cells were washed 2X with PBS and labeled with primary antibody for RABV N, G or EBOV GP overnight at 4°C. Cells were washed 3X with PBS, and stained with secondary antibody for 1h at RT. Coverslips were then mounted on glass slides using Vectashield mounting media with DAPI (Vector Labs) and visualized using the Broadband Confocal Leica TCS SP5 II and Leica LAS AF software for analysis. RVGP and RVΔG-GP were found in both cell lines as indicated by the presence of RABV N. However, although G and GP were detected in both cell lines for RVGP, RABV G was not detected in RVΔG-GP infected VeroE6 cells (Fig 2, 1B). Of note, fluorescence of G present in the BSR-G cells alone is evident and distinguishable from the presence of G associated with the viral infection of the cell line. The absence of RABV G staining in RVΔG-GP infected VeroE6 cells confirms that RABV G is not synthesized and indicates that residual RABV G from the initial infection is not recycled and incorporated into new budding virions.
Table 1.
Confocal Staining Method. 4% Paraformaldehyde fixation, then blocked and permeabilized in PBS with 1% BSA, 0.3M Glycine and 0.1% Triton X-100.
| Antibody set | N/G | N/GP |
|---|---|---|
| Primary | Mouse anti-RABV N (Millipore) and Rabbit anti-RABV G1 | Mouse anti-RABV N (Millipore) and Human anti-EBOV GP2 |
| Secondary | anti-mouse594/anti-rabbit488 (AlexaFluor) | anti-mouse594/anti-human488 (AlexaFluor) |
#1063, In-house polyclonal antibody from Matthias Schnell, Thomas Jefferson University.
KZ52, monoclonal antibody kindly provided by D. Burton, The Scripps Research Institute.
Electron microscopy further reinforces that RVΔG-GP is replication deficient and limited at the final steps of assembly and budding of infectious virions in VeroE6 cells (Fig 3). Thin-section electron microscopy was performed as follows. One-day-old 90% confluent T75 flasks of either BSR-G or VeroE6 cells were infected in duplicate at an MOI of 0.1 with either RVGP or RVΔG-GP using cellgro Complete serum free media (Mediatech). Flasks were incubated at 37°C/5%CO2 for 96h. Supernatant was removed, and adherent cells were fixed with 0.1% paraformaldehyde in Millonig’s Sodium Phosphate Buffer for 10min at RT. Cells were washed with media and incubated with primary antibodies for glycoproteins (see Table 1) for 3h at RT followed by gold-conjugated secondary antibodies for 2h at RT. Cells were washed with media and fixed with 2.5% glutaraldehyde + 2% paraformaldehyde. Cells were scraped from the flasks and pelleted by centrifugation. Samples were kept for 24h at 4°C to complete fixation. Post-fixation, staining, embedding, and thin-sectioning were performed as described previously (3). The results are in agreement with previous findings that RABV virion formation and budding is hindered in G-deleted RABV mutants (19). Of RVΔGGP infected BSR-G cells, approximately 95% of all the extracellular and budding particles exhibited GP labeling only, lightly labeled with 15nm gold particles (Fig 3, B). Only 5% of the extracellular or budding particles exhibited labeling with both GP 15nm and G 5nm particles. RVGP labeled for both G and GP in both BSR-G and VeroE6 cells (Fig 3, A and C). Immunogold labeling was not performed for VeroE6 cells infected with RVΔG-GP, due to the tremendous reduction of budding or extracellular virus-like particles in our samples (Fig 3, D). In our RVΔG-GP -infected VeroE6 cells, pleomorphic shapes and VLPs were found in less than 5% of all cells examined. A few cells also exhibited areas of electron-dense material, which may have been an accumulation of viral-related proteins. No gold particles were found in negative control samples, where over 200 sections were analyzed per sample.
Figure 3.
Confocal microscopy at 126X magnification using fluorescently labeled antibodies shows that RVG is not synthesized in RVΔGGP-infected VeroE6 cells. BSR-G and VeroE6 cells were infected with RVGP or RVΔGGP at an MOI of 0.01, and then fix and stained at 48hpi according to staining method in Table 1. Antibody set N/G is for RABV N and RABV G detection; N is red and G is green. Antibody set N/GP is for RABV N and EBOV GP detection; N is red and GP is green.
Evidently, RVΔG-GP is unable to utilize residual G to proliferate from VeroE6 cells, and the translated Ebola GP does not effectively substitute to permit continued viral particle formation or release. Hence, the vaccine is incapable of recombining to a replicative genotype and, furthermore, unable to revert to a pathogenic phenotype. These results bolster the safety profile of this replication-deficient RABV-EBOV bivalent vaccine. Further animal studies would be required to determine if an RVΔG-GP optimized for greater GP incorporation could provide 100% protection from EBOV challenge.
Figure 4.
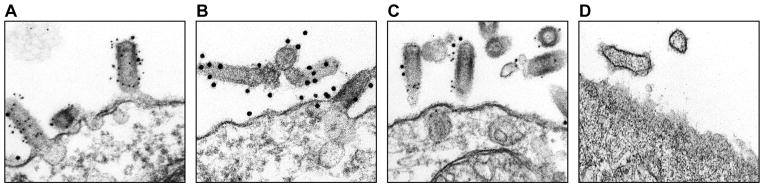
Electron microscopy of VeroE6 and BSR-G cells infected with RVΔGGP and RVGP followed by immunogold labeling for RABV G and EBOV GP at 96hrs post infection. Cells were infected and prepared as described in the text. Gold-tagged antibodies confirm glycoprotein expression on virion surface. A) RVGP in BSR-G cells; B) RVΔGGP in BSR-G cells; C) RVGP in VeroE6 cells; D) RVΔGGP in VeroE6 cells (67900X). 96hpi @ 108000X unless noted. RVG labeled with 5nm particles. GP labeled with 15nM particles. Immunogold labeling of D was not performed due to lack of extracellular virions at sufficient quantities to justify staining.
Highlights.
Our replication deficient rabies-ebolavirus bivalent vaccine candidate is capable of efficient infection in cell culture as evidenced by equivalent genome levels between the rabies virus glycoprotein trans-complementing cell line and target VeroE6 cells.
In our rabies G deleted vaccine construct, RABV-G is not synthesized nor is it recycled and incorporated into budding virions as determined by electron and confocal microscopy.
Acknowledgments
This work was supported by the NIAID Division of Intramural Research and in part by the NIAID Division of Clinical Research. The content of this publication does not necessarily reflect the views or policies of the US Department of Health and Human Services (DHHS) or of the institutions and companies affiliated with the authors. This work was funded in part through Battelle Memorial Institute’s prime contract with the US National Institute of Allergy and Infectious Diseases (NIAID) Division of Clinical Research under Contract No. HHSN272200700016I. The subcontractor to Battelle Memorial Institute who performed this work was: J.G.B. an employee of Tunnell Government Services, Inc. We would like to thank Dr. Owen Schwartz, NIAID/DIR/RTB/BIS, for technical assistance with the Leica TCS SP5 Confocal microscope. We also thank Jiro Wada, NIAID/DCR/OCSIRFF, for his technical assistance in preparing the figures for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Barrett PN, Mundt W, Kistner O, Howard MK. Vero cell platform in vaccine production: moving towards cell culture-based viral vaccines. Expert review of vaccines. 2009;8:607–618. doi: 10.1586/erv.09.19. [DOI] [PubMed] [Google Scholar]
- 2.Blaney JE, Marzi A, Willet M, Papaneri AB, Wirblich C, Feldmann F, Holbrook M, Jahrling P, Feldmann H, Schnell MJ. Antibody quality and protection from lethal Ebola virus challenge in nonhuman primates immunized with rabies virus based bivalent vaccine. PLoS pathogens. 2013;9:e1003389. doi: 10.1371/journal.ppat.1003389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blaney JE, Wirblich C, Papaneri AB, Johnson RF, Myers CJ, Juelich TL, Holbrook MR, Freiberg AN, Bernbaum JG, Jahrling PB, Paragas J, Schnell MJ. Inactivated or live-attenuated bivalent vaccines that confer protection against rabies and Ebola viruses. Journal of virology. 2011;85:10605–10616. doi: 10.1128/JVI.00558-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conzelmann KK, Cox JH, Schneider LG, Thiel HJ. Molecular cloning and complete nucleotide sequence of the attenuated rabies virus SAD B19. Virology. 1990;175:485–499. doi: 10.1016/0042-6822(90)90433-r. [DOI] [PubMed] [Google Scholar]
- 5.Etessami R, Conzelmann KK, Fadai-Ghotbi B, Natelson B, Tsiang H, Ceccaldi PE. Spread and pathogenic characteristics of a G-deficient rabies virus recombinant: an in vitro and in vivo study. The Journal of general virology. 2000;81:2147–2153. doi: 10.1099/0022-1317-81-9-2147. [DOI] [PubMed] [Google Scholar]
- 6.Faber M, Lamirande EW, Roberts A, Rice AB, Koprowski H, Dietzschold B, Schnell MJ. A single immunization with a rhabdovirus-based vector expressing severe acute respiratory syndrome coronavirus (SARS-CoV) S protein results in the production of high levels of SARS-CoV-neutralizing antibodies. The Journal of general virology. 2005;86:1435–1440. doi: 10.1099/vir.0.80844-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faber M, Pulmanausahakul R, Hodawadekar SS, Spitsin S, McGettigan JP, Schnell MJ, Dietzschold B. Overexpression of the rabies virus glycoprotein results in enhancement of apoptosis and antiviral immune response. Journal of virology. 2002;76:3374–3381. doi: 10.1128/JVI.76.7.3374-3381.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gomme EA, Faul EJ, Flomenberg P, McGettigan JP, Schnell MJ. Characterization of a single-cycle rabies virus-based vaccine vector. Journal of virology. 2010;84:2820–2831. doi: 10.1128/JVI.01870-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goudsmit J, Marissen WE, Weldon WC, Niezgoda M, Hanlon CA, Rice AB, Kruif J, Dietzschold B, Bakker AB, Rupprecht CE. Comparison of an anti-rabies human monoclonal antibody combination with human polyclonal anti-rabies immune globulin. The Journal of infectious diseases. 2006;193:796–801. doi: 10.1086/500470. [DOI] [PubMed] [Google Scholar]
- 10.Hartlieb B, Weissenhorn W. Filovirus assembly and budding. Virology. 2006;344:64–70. doi: 10.1016/j.virol.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Hunt CL, Lennemann NJ, Maury W. Filovirus entry: a novelty in the viral fusion world. Viruses. 2012;4:258–275. doi: 10.3390/v4020258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuhn JH, Dodd LE, Wahl-Jensen V, Radoshitzky SR, Bavari S, Jahrling PB. Evaluation of perceived threat differences posed by filovirus variants. Biosecurity and bioterrorism : biodefense strategy, practice, and science. 2011;9:361–371. doi: 10.1089/bsp.2011.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manning SE, Rupprecht CE, Fishbein D, Hanlon CA, Lumlertdacha B, Guerra M, Meltzer MI, Dhankhar P, Vaidya SA, Jenkins SR, Sun B, Hull HFC Advisory Committee on Immunization Practices Centers for Disease and Prevention. Human rabies prevention--United States, 2008: recommendations of the Advisory Committee on Immunization Practices. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports/Centers for Disease Control. 2008;57:1–28. [PubMed] [Google Scholar]
- 14.Marzi A, Engelmann F, Feldmann F, Haberthur K, Shupert WL, Brining D, Scott DP, Geisbert TW, Kawaoka Y, Katze MG, Feldmann H, Messaoudi I. Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:1893–1898. doi: 10.1073/pnas.1209591110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marzi A, Wegele A, Pohlmann S. Modulation of virion incorporation of Ebolavirus glycoprotein: effects on attachment, cellular entry and neutralization. Virology. 2006;352:345–356. doi: 10.1016/j.virol.2006.04.038. [DOI] [PubMed] [Google Scholar]
- 16.McGettigan JP. Experimental rabies vaccines for humans. Expert review of vaccines. 2010;9:1177–1186. doi: 10.1586/erv.10.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGettigan JP, Pomerantz RJ, Siler CA, McKenna PM, Foley HD, Dietzschold B, Schnell MJ. Second-generation rabies virus-based vaccine vectors expressing human immunodeficiency virus type 1 gag have greatly reduced pathogenicity but are highly immunogenic. Journal of virology. 2003;77:237–244. doi: 10.1128/JVI.77.1.237-244.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKenna PM, Aye PP, Dietzschold B, Montefiori DC, Martin LN, Marx PA, Pomerantz RJ, Lackner A, Schnell MJ. Immunogenicity study of glycoprotein-deficient rabies virus expressing simian/human immunodeficiency virus SHIV89.6P envelope in a rhesus macaque. Journal of virology. 2004;78:13455–13459. doi: 10.1128/JVI.78.24.13455-13459.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mebatsion T, Konig M, Conzelmann KK. Budding of rabies virus particles in the absence of the spike glycoprotein. Cell. 1996;84:941–951. doi: 10.1016/s0092-8674(00)81072-7. [DOI] [PubMed] [Google Scholar]
- 20.Mebatsion T, Schnell MJ, Cox JH, Finke S, Conzelmann KK. Highly stable expression of a foreign gene from rabies virus vectors. Proceedings of the National Academy of Sciences of the United States of America. 1996;93:7310–7314. doi: 10.1073/pnas.93.14.7310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS pathogens. 2010;6:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papaneri AB, Wirblich C, Cann JA, Cooper K, Jahrling PB, Schnell MJ, Blaney JE. A replication-deficient rabies virus vaccine expressing Ebola virus glycoprotein is highly attenuated for neurovirulence. Virology. 2012;434:18–26. doi: 10.1016/j.virol.2012.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pulmanausahakul R, Li J, Schnell MJ, Dietzschold B. The glycoprotein and the matrix protein of rabies virus affect pathogenicity by regulating viral replication and facilitating cell-to-cell spread. Journal of virology. 2008;82:2330–2338. doi: 10.1128/JVI.02327-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson JS, Dekker JD, Croyle MA, Kobinger GP. Recent advances in Ebolavirus vaccine development. Human vaccines. 2010;6:439–449. doi: 10.4161/hv.6.6.11097. [DOI] [PubMed] [Google Scholar]
- 25.Schnell MJ, Buonocore L, Boritz E, Ghosh HP, Chernish R, Rose JK. Requirement for a non-specific glycoprotein cytoplasmic domain sequence to drive efficient budding of vesicular stomatitis virus. The EMBO journal. 1998;17:1289–1296. doi: 10.1093/emboj/17.5.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schnell MJ, McGettigan JP, Wirblich C, Papaneri A. The cell biology of rabies virus: using stealth to reach the brain. Nature reviews. Microbiology. 2010;8:51–61. doi: 10.1038/nrmicro2260. [DOI] [PubMed] [Google Scholar]
- 27.Schnell MJ, Mebatsion T, Conzelmann KK. Infectious rabies viruses from cloned cDNA. The EMBO journal. 1994;13:4195–4203. doi: 10.1002/j.1460-2075.1994.tb06739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith ME, Koser M, Xiao S, Siler C, McGettigan JP, Calkins C, Pomerantz RJ, Dietzschold B, Schnell MJ. Rabies virus glycoprotein as a carrier for anthrax protective antigen. Virology. 2006;353:344–356. doi: 10.1016/j.virol.2006.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stahelin RV. Membrane binding and bending in Ebola VP40 assembly and egress. Frontiers in microbiology. 2014;5:300. doi: 10.3389/fmicb.2014.00300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takada A. Filovirus tropism: cellular molecules for viral entry. Frontiers in microbiology. 2012;3:34. doi: 10.3389/fmicb.2012.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tordo N, Poch O, Ermine A, Keith G, Rougeon F. Walking along the rabies genome: is the large G-L intergenic region a remnant gene? Proceedings of the National Academy of Sciences of the United States of America. 1986;83:3914–3918. doi: 10.1073/pnas.83.11.3914. [DOI] [PMC free article] [PubMed] [Google Scholar]