Abstract
In this investigation, the effects of hypoglycemic coma and alcoholic coma on the blood-brain barrier (BBB) permeability have been compared. Female adult Wistar albino rats weighing 180-230 g were divided into three groups: Control group (n=8), Alcoholic Coma Group (n=18), and Hypoglycemic Coma group (n=12). The animals went into coma approximately 3-4 hours after insulin administration and 3-5 minutes after alcohol administration. Evans blue (4mL/kg) was injected intravenously as BBB tracer. It was observed that the alcoholic coma did not significantly increase the BBB permeability in any of the brain regions when compared to control group. Changes in BBB permeability were significantly increased by the hypoglycemic coma in comparison to the control group values (p<0.01). Our findings suggest that hypoglycemic and alcoholic coma have different effects on the BBB permeability depending on the energy metabolism.
KEY WORDS: blood-brain barrier, hypoglycemic coma, alcoholic coma
INTRODUCTION
Brain tissue is protected by blood-brain barrier (BBB). It is a specialized structure consisting of endothelial cells and tight junctions between them, a continuous basal lamina which surrounds these cells. The tight junctions are reinforced by the foot processes of the astrocytes [1]. There are several reports investigating the effects of convulsions, acute hypertension, brain tumors, ischemia on the BBB permeability [2-7], however, only a few studies have examined effects of the state of coma [8, 9]. Hypoglycemic coma leads to energy deficiency due to a reduction in plasma glucose concentrations, ATP and other nucleoside triphosphates [9]. The energy deficiency with concomitant disruption of the ion homeostasis may cause dysfunctionality of both the neurons and the cerebral endothelial cells composing the BBB [10-12]. Increased BBB permeability causes vasogenic edema under pathological conditions. However, the changes in the BBB permeability during hypoglycemic coma have not precisely been understood. It has been suggested that both acute and chronic administrations of alcohol have disruptive effects on many structures and their functions including the cerebral capillary endothelial cells of the central nervous system [13-16]. While some studies have shown that acute administrations of alcohol increased the BBB permeability, others have suggested that it had no effect [16-19]. There are gender related differences in the central nervous system, and acute and chronic administration of alcohol appears to affect the female brain much more than that of male [20,21]. The reported brain morphological abnormalities could also occur more precociously in alcoholic women than in men [22]. Especially social and environmental, physiological, genetic and neurobiological ones have been demonstrated to contribute to the sex difference in response to alcohol intake, as well as the development of alcoholic complications. A number of neurotransmitters and growth factors may be partially involved in these differences between men and women [23]. In the present study, we have comparatively investigated the effects of hypoglycemic coma and alcoholic coma on BBB permeability in the female rats.
MATERIALS AND METHODS
Animals and Procedure
The procedures were in accordance with the Helsinki Declaration 2008. The female adult Wistar albino rats weighing 180-230 g were used in the experiments. The rats were divided into three groups: 1. Control (n=8), 2. Alcoholic Coma (n=18) and 3. Hypoglycemic Coma (n=12) group. A cannulation was performed to the animals under diethyl-ether anesthesia. Following the injection of anesthesia through femoral vein, the femoral artery was catheterized to measure systemic arterial blood pressure. BBB permeability was determined using tracer Evans blue (EB) (Sigma Cat no: E-2129) tracer (4 mL/kg, i.v.) [5]. Alcoholic coma was induced by injecting 4 g/kg of ethyl alcohol intraperitoneally. The rats went into coma 3-5 minutes after the alcohol administration [24]. The animals were fasted for 15 hours before the experiments but were allowed free access to water. To induce the hypoglycemic coma, 100 IU/kg crystallin zinc insulin (Eli Lily Co, 12584-58-6) was administrated intraperitoneally under diethyl-ether anesthesia [25]. The rats went into coma approximately 3-4 hours later following insulin administration. The glucose oxidase method (Accu-Check Advantage, Roche Diagnostics GmbH, Mannheim, Germany) was applied to blood samples drawn from the tails to determine the plasma glucose levels [26]. Their brains were washed by 0.9% NaCl perfusion through the left ventricle 25 minutes after the Evans Blue injection. Amount of Evans blue penetrating the tissue was evaluated macroscopically with respect to the Rapoport Criteria [27]. Staining of each hemisphere and of coronal sections by Evans blue was graded as follows: Grade 0, no staining; Grade 1+, slight staining; Grade 2+, moderate; and Grade 3+, marked and dark staining. After decapitation, the brain was quickly removed and dissected into 3 regions; left cerebral cortex, right cerebral cortex, brain stem and cerebellum. The wet weights of the dissected regions were determined. Then, each of the brain area was homogenized in tubes containing 5 mL of 1 N NaOH and 5 mL of phosphate buffer (22.6 g/L NaH2PO42H2O, 25.2 g/L NaOH. 130 ml of NaOH and 870 ml of NaH2PO42H2O were mixed and pH calibrated 7,4). Following the homogenization, they were centrifuged at 4000 rpm for 60 min at +4°C. After centrifuging, each supernatant was transferred into spectrophotometer tubes and the absorbance values at 620 nm wave length were read. The Evans blue values were calculated as mg Evans blue per gram brain tissue by using the obtained absorbance values, the regression equations and regression curves of the Evans blue absorbance-amount [5].
Statistical analysis
The statistical analysis was made with SPSS (Statistical Package for Social Sciences 10.0 ver.). EB-albumin extravasation was expressed as mean±SEM. Data were compared among groups using one way analysis of variance (ANOVA) and subsequently Tukey’s test was performed where ANOVA showed statistical significance (p<0.05).
RESULTS
The values of blood pressure, blood glucose and the changes in BBB permeability with respect to Rapoport criteria [27] are shown in Table 1. The baseline mean value of arterial blood pressure was 89.5±3 mmHg for hypoglycemic coma group and was 88±5.2 mmHg for the alcoholic coma group. No significant change was seen in arterial blood pressure values of the rats after they went into hypoglycemic coma and alcoholic coma (87±10 mmHg, 85±7 mmHg). Plasma glucose levels of the rats in alcoholic coma were found to be within the normal range (131±43 mg/dl), whereas those of rats in hypoglycemic coma were 21± 2.5 mg/dl (Table 1). It has been observed that the alcoholic coma did not increase the BBB permeability significantly in any of the brain regions (p>0.05) when the Evans Blue concentrations in the regions of left hemisphere, right hemisphere, cerebellum and the brain stem (0.33±0.03, 0.31±0.03, 0.33±0.06, 0.47±0.09 μg/mg tissue respectively) of Alcoholic Coma Group were compared with those of Control Group (0.22±0.07, 0.21±0.07, 0.32±0.04, 0.3±0.03 μg/mg tissue respectively) (Figure 1).
TABLE 1.
Values of arterial blood pressure, blood glucose levels and Evans blue albumin extravasation, before and after coma.
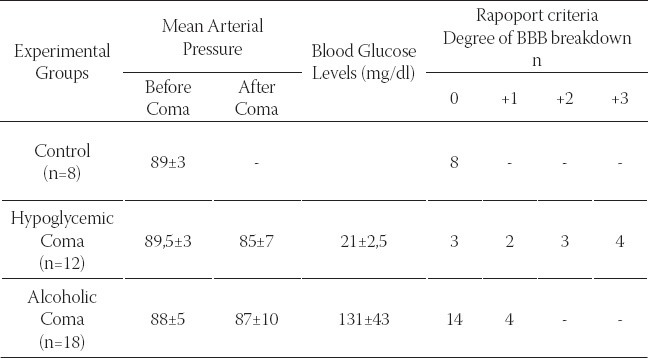
FIGURE 1.
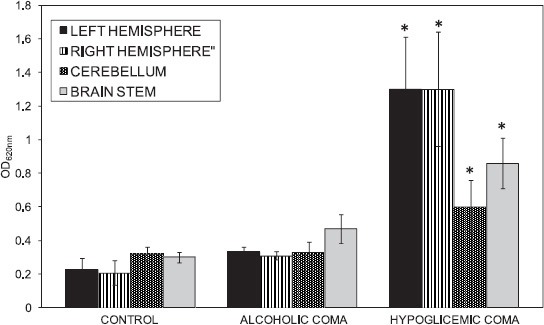
Displaying quantitative measurements of EB dye content (% mg) in the brain regions of the groups. *p<0.01 control vs. hypoglycemic coma
Contrarily, increased BBB permeability was observed in 9 of 12 experimental animals that went into hypoglycemic coma (Table 1).
Evans Blue concentrations in the regions of left hemisphere, right hemisphere, cerebellum and the brain stem (1.3±0.03, 1.3±0.034, 0.6±0.2, 0.86±0.15 μg/mg tissue respectively) of Hypoglycemic Coma Group were compared with those of Control Group (Figure 1). It was determined that hypoglycemic coma increased the BBB permeability significantly in all of the brain regions (p<0.01).
DISCUSSION
Glucose is the main substrate the brain uses to generate energy, which penetrates into the brain by facilitated diffusion through BBB [28]. Hypoglycemia due to the reduced plasma glucose levels below normal range leads to brain dysfunctionalities [29]. Hypoglycemia is a relatively common condition primarily affecting diabetic patients treated with insulin or other hypoglycemic drugs and insulinoma patients. Hypoglycemic effects on the CNS include various symptoms such as irritability and lack of concentration, disruption of cognitive functions, convulsions and unconsciousness. Even a single hypoglycemic episode with convulsions and/or coma may, if prolonged and severe enough, cause permanent degenerative alterations in the cerebral cortex [30]. These symptoms of hypoglycemia suggest the presence of increased intracranial pressure and cerebral edema [31]. In a hypoglycemic coma, neurons and especially cerebral endothelial cells composing the BBB may face energy failure [32]. Endothelial cells of brain capillaries differ than the others with their relatively higher metabolism [33]. The cerebral capillary endothelial cells have mitochondria in large quantities [34] and contain comparatively 500-fold more Na+-K+-ATPase enzymes than the umbilical endothelial cells [35]. Hypoglycemia causes the dysfunctionality of active Na+-K+-ATPases in cerebral endothelial cell membranes due to the energy deficiency. Due to this dysfunctionality, potassium ions exit and ions like sodium and calcium penetrate into the cerebral endothelial cells and the cytotoxic edema occurring as a result of these changes. Thus, it may cause swelling of the endothelial cells and the tight connections between them may detach. The vasogenic edema, occurring as a result of the elevated amount of albumin due to the increased permeability, may be responsible for dysfunctionality of neurons in case of hypoglycemia [9]. Finally, it can not be excluded that hypoglycemia has detrimental effects on mitochondria at the level of the axon, affecting energy production in the axon itself, in the associated Schwann cells, in the local blood vessels and/or in the perineurial sheath [36]. Sekimoto et al. [37] have demonstrated that hypoglycemia damaged the endothelial ultrastructure of cerebral arteries. Hsu and Hedley-Whyte [32] have reported that severe hypoglycemia in mice caused deletion in cerebral vessel walls. It has also been observed in our study that, the hypoglycemia coma significantly increased the BBB permeability in the left cortex, right cortex, cerebellum and brain stem regions of the brain. In addition, lack of any significant change in arterial blood pressure in rats during the hypoglycemic coma suggests that the blood pressure has no effect on the increased BBB permeability in case of hypoglycemia. It has been found that the glucose extraction in the cerebellum is twice more than that of other parts of the brain [38] so that the cerebellum conserves the cellular energy better than the cerebral cortex in case of hypoglycemic coma [10, 39]. Thus, less BBB damage in the cerebellum has been reported in comparison to the other parts of the brain [10, 40]. Similarly, we found less Evans blue-albumin extravasation in the cerebellum when compared to the cerebral cortex. Alcohol is a soluble substance in both water and oil and can easily penetrate the lipid membranes of all the cells in the body. Thus, alcohol can penetrate the BBB easily [41]. Alcohol could affect the blood flow of the brain, brain glucose metabolism, synthesis and catabolism of various neurotransmitters [42-44], and also affects many structures and functions including the capillary endothelial cells in central nervous system [13]. In alcoholics, also many physiological dysfunctions occur beside the structural changes in the brain [20]. However, the effects of acute alcohol administration on BBB permeability are controversial, there are studies suggesting that alcohol has no effect on BBB permeability beside the studies indicating that alcohol has increased the BBB permeability against the various tracers [16-19]. Rossner et al. [45], have demonstrated that 10 % ethanol (1-3 g/kg i.v.) increased Evans blue permeability of BBB in a short term. Similarly, Eriksson et al. [46] have administered 20% ethanol (2 g/kg i.p.) and have observed increased BBB permeability in rats. However, Hillbom and Tervo [47] have observed no increase in BBB permeability after administration of 10% ethanol (5 g/kg i.p.) in rats. Effects of ethanol on BBB permeability have also been studied by using 14C-sucrose tracer in rats [16]. They have found that BBB permeability did not increase when they have administered acutely 10% ethanol as 4 g/kg i.p. Gulati et al. [18], using sodium fluorescent as tracer, have injected ethyl alcohol of 30%, 60%, and 90% as 0,568 mg/kg i.v. and consequently found that the BBB permeability has increased significantly. They suggested a correlation between alcohol concentration and BBB permeability, and the ethyl alcohol of 90% has increased the permeability more than the concentrations of 30% and 60%. However, no change in BBB permeability in rats has also been reported following administration of 20% ethanol as 3 g/kg i.p. [17]. In the present study, ethanol administered at the coma dose (4 g/kg) slightly increased the BBB permeability in only four animals. This discrepancy may be attributed to the sex of the animals, concentration and administration pattern of alcohol and the difference between the tracers used for the investigation of BBB permeability. The effect mechanism of alcohol on BBB permeability could have been clarified. In contrast to our findings, Haorah et al. [48] have shown that the alcohol caused deformation of integrity of BBB by causing the increase in reactive oxygen types, activation of myosin light chain kinase and the increase in phosphorilation of myosin light chain and tight connection proteins using primary monolayer human brain microvascular endothelial cell culture. Alcohol is common cause of coma in all age ranges. Alcoholic coma can be associated with head injuries, hypothermia and the presence of other drugs with which its action may be additive. In most cases, coma caused by alcohol will resolve relatively rapidly, the exception being when there is hepatic insufficiency [49]. Excessive alcohol short- or long-term health effects NMDA receptors start to become unresponsive, slowing areas of the brain they are responsible for. Contributing to this effect is the activity which alcohol induces in the gamma-aminobutyric acid system. The GABA system is known to inhibit neural activity in the brain. GABA could also be responsible for the memory impairment [50, 51]. The effects of alcohol on the BBB permeability need to be further elucidated. Since BBB damage may lead to neuroinflammation and neuronal loss, it may be important to establish how BBB affected by alcoholic coma. In this study, we have shown that hypoglycemic coma significantly increases the BBB permeability whereas alcoholic coma causes insignificant catabolism of BBB. The blood glucose level was not affected in alcoholic coma. Therefore, the energy level seems to be sufficient to maintain the structural integrity of the BBB. However, in hypoglycemic coma the blood glucose level was very low for providing the essential energy for BBB integrity.
CONCLUSION
Results of the present study suggest that both hypoglycemic and alcoholic coma have different effects on the BBB permeability depending on the energy metabolism.
ACKNOWLEDGEMENT
The authors would like to thank to Professor Bayram Yilmaz of Yeditepe University, Medical School, Department of Physiology in Istanbul for reading and improving the language of the manuscript.
DECLARATION OF INTEREST
Authors do not have any commercial affiliations, or potential conflicts of interest associated with this work submitted for publication.
REFERENCES
- [1].Chaudhuri JD. Blood brain barrier and infection. Med Sci Monit. 2000;6(6):1213–1222. [PubMed] [Google Scholar]
- [2].Bolwig TG, Hertz MM, Westergaard E. Acute hypertension causing blood-brain barrier breakdown during epileptic seizures. Acta Neurol Scand. 1977;56(4):335–342. doi: 10.1111/j.1600-0404.1977.tb01440.x. [DOI] [PubMed] [Google Scholar]
- [3].Brooks DJ, Beaney RP, Lammertsma AA, Leenders KL, Horlock PL, Kensett MJ, et al. Quantitative measurement of blood-brain barrier permeability using rubidium-82 and positron emission tomography. J Cereb Blood Flow Metab. 1984;4(4):535–545. doi: 10.1038/jcbfm.1984.78. [DOI] [PubMed] [Google Scholar]
- [4].Lo EH, Pan Y, Matsumoto K, Kowall NW. Blood-brain barrier disruption in experimental focal ischemia: comparison between in vivo MRI and immunocytochemistry. Magn Reson Imaging. 1994;12(3):403–411. doi: 10.1016/0730-725x(94)92533-x. [DOI] [PubMed] [Google Scholar]
- [5].Oztas B, Kucuk M. Influence of acute arterial hypertension on blood-brain barrier permeability in streptozocin-induced diabetic rats. Neurosci Lett. 1995;188(1):53–56. doi: 10.1016/0304-3940(95)11393-b. [DOI] [PubMed] [Google Scholar]
- [6].Petito CK, Schaefer JA, Plum F. Ultrastructural characteristics of the brain and blood-brain barrier in experimental seizures. Brain Res. 1977;127(2):251–267. doi: 10.1016/0006-8993(77)90539-x. [DOI] [PubMed] [Google Scholar]
- [7].Sadoshima S, Fujishima M, Ogata J, Ibayashi S, Shiokawa O, Omae T. Disruption of blood-brain barrier following bilateral carotid artery occlusion in spontaneously hypertensive rats, A quantitative study. Stroke. 1983;14(6):876–882. doi: 10.1161/01.str.14.6.876. [DOI] [PubMed] [Google Scholar]
- [8].Berbel-Garcia A, Porta-Etessam J, Martinez-Salio A, Ballesta F, Saiz-Diaz RA, Perez-Martinez DA, et al. Transient cerebral oedema associated to hypoglycemia. Rev Neurol. 2004;39(11):1030–1033. [PubMed] [Google Scholar]
- [9].Gisselsson L, Smith ML, Siesjo BK. Influence of hypoglycemic coma on brain water and osmolality. Exp Brain Res. 1998;120:461–469. doi: 10.1007/s002210050419. [DOI] [PubMed] [Google Scholar]
- [10].Agardh CD, Siesjo BK. Hypoglycemic brain injury: phospholipids, free fatty acids, and cyclic nucleotides in the cerebellum of the rat after 30 and 60 minutes of severe insulin-induced hypoglycemia. J Cereb Blood Flow Metab. 1981;1(1):267–275. doi: 10.1038/jcbfm.1981.31. [DOI] [PubMed] [Google Scholar]
- [11].Chapman AG, Westerberg E, Siesjo BK. The metabolism of purine and pyrimidine nucleotides in rat cortex during insulin-induced hypoglycemia and recovery. J Neurochem. 1981;36(1):179–189. doi: 10.1111/j.1471-4159.1981.tb02393.x. [DOI] [PubMed] [Google Scholar]
- [12].Katsura K, Folbergrova J, Bengtsson F, Kristian T, Gido G, Siesjo BK. Recovery of mitochondrial and plasma membrane function following hypoglycemic coma: coupling of ATP synthesis, K+transport, and changes in extra- and intracellular pH. J Cereb Blood Flow Metab. 1993;13(5):820–826. doi: 10.1038/jcbfm.1993.104. [DOI] [PubMed] [Google Scholar]
- [13].Karwacka H. Ultrastructural and biochemical studies of the brain and other organs in rats after chronic ethanol administration. I. Electronmicroscopic investigations of the morphologic elements of the blood-brain barrier in the rat after ethanol intoxication. Exp Pathol (Jena) 1980;18(2):118–126. doi: 10.1016/s0014-4908(80)80061-5. [DOI] [PubMed] [Google Scholar]
- [14].Mayhan WG. Responses of cerebral arterioles during chronic ethanol exposure. Am J Physiol. 1992;262(3Pt2):787–791. doi: 10.1152/ajpheart.1992.262.3.H787. [DOI] [PubMed] [Google Scholar]
- [15].Mayhan WG, Didion SP. Acute effects of ethanol on responses of cerebral arterioles. Stroke. 1995;26(11):2097–2101. doi: 10.1161/01.str.26.11.2097. [DOI] [PubMed] [Google Scholar]
- [16].Phillips SC. Does ethanol damage the blood--brain barrier? J Neurol Sci. 1981;50:81–87. doi: 10.1016/0022-510x(81)90043-5. [DOI] [PubMed] [Google Scholar]
- [17].Elmas I, Kuçuk M, Kalayci RB, Çevik A, Kaya M. Effects of profound hypothermia on the blood-brain barrier permeability in acute and chronically ethanol treated rats. Forensic Sci Int. 2001;119(2):121–126. doi: 10.1016/s0379-0738(00)00429-1. [DOI] [PubMed] [Google Scholar]
- [18].Gulati A, Nath C, Shanker K, Srimal RC, Dhawan KN, Bhargava KP. Effects of alcohols on the permeability of blood-brain barrier. Pharmacol Res Commun. 1985;17:85–93. doi: 10.1016/0031-6989(85)90054-2. [DOI] [PubMed] [Google Scholar]
- [19].Oztas B, Kucuk M. Hypertension-induced protein leakage in the brain in chronic ethanol administered rats. Pharmacol Res Commun. 1988;20(2):117–123. doi: 10.1016/s0031-6989(88)80004-3. [DOI] [PubMed] [Google Scholar]
- [20].Kril JJ, Halliday GM. Brain shrinkage in alcoholics: A decade on and what have we learned? Prog Neurobiol. 1999;58(4):381–387. doi: 10.1016/s0301-0082(98)00091-4. [DOI] [PubMed] [Google Scholar]
- [21].Schindler CJ, Veliskova J, Slamberova R, Vathy I. Prenatal morphine exposure alters susceptibility to bicuculline seizures in a sex- and age-specific manner. Brain Res Dev Brain Res. 2000;121(1):119–122. doi: 10.1016/s0165-3806(00)00031-6. [DOI] [PubMed] [Google Scholar]
- [22].Limosin F. Clinical and biological specificities of female alcoholism. Encephale. 2002;28(6):503–509. [PubMed] [Google Scholar]
- [23].Ceylan-Isik AF, McBride SM, Ren J. Sex difference in alcoholism: who is at a greater risk for development of alcoholic complication? Life Sci. 2010;87(5-6):133–138. doi: 10.1016/j.lfs.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Cherian L, Mathew J, Klemm WR. Ethanol-induced hydrolysis of brain sialoglycoconjugates in the rat: effect of sialic acid in antagonizing ethanol intoxication. Alcohol Clin Exp Res. 1989;13(3):435–438. doi: 10.1111/j.1530-0277.1989.tb00349.x. [DOI] [PubMed] [Google Scholar]
- [25].Oztaş B, Camurcu S. Blood-brain barrier permeability after electrically induced seizure in normoglycemic, hypoglycemic, and hyperglycemic rats. Psychiatry Res. 1989;29(2):151–159. doi: 10.1016/0165-1781(89)90029-2. [DOI] [PubMed] [Google Scholar]
- [26].Barham D, Trinder P. An improved colour reagent for the determination of blood glucose by the oxidase system. Analyst. 1972;97(151):142–145. doi: 10.1039/an9729700142. [DOI] [PubMed] [Google Scholar]
- [27].Rapoport SI, Fredericks WR, Ohno K, Pettigrew KD. Quantitative aspects of reversible osmotic opening of the blood-brain barrier. Am J Physiol. 1980;238(5):421–431. doi: 10.1152/ajpregu.1980.238.5.R421. [DOI] [PubMed] [Google Scholar]
- [28].Gjedde A, Rasmussen M. Blood-brain glucose transport in the conscious rat: comparison of the intravenous and intracarotid injection methods. J Neurochem. 1980;35:1375–1381. doi: 10.1111/j.1471-4159.1980.tb09012.x. [DOI] [PubMed] [Google Scholar]
- [29].Gerich JE, Mokan M, Veneman T, Korytkowski M, Mitrakou A. Hypoglycemia unawareness. Endocr Rev. 1991;12:356–371. doi: 10.1210/edrv-12-4-356. [DOI] [PubMed] [Google Scholar]
- [30].Mohseni S. Hypoglycemic neuropathy. Acta Neuropathol. 2001;102:413–421. doi: 10.1007/s004010100459. [DOI] [PubMed] [Google Scholar]
- [31].Plum F, Posner JB. Diagnosis of Stupor and Coma. 3rd edn. Philadelphia: FA Davis Co; 1966. Metabolic brain diseases causing coma; p. 132. [Google Scholar]
- [32].Hsu DW, Hedley-Whyte ET. Effects of insulin-induced hypoglycemia on cerebrovascular permeability to horseradish peroxidase. J Neuropathol Exp Neurol. 1980;39(3):265–284. doi: 10.1097/00005072-198005000-00004. [DOI] [PubMed] [Google Scholar]
- [33].Mrsulja BB, Djuricic BM. Biochemical characteristics of cerebral capillaries. Adv Exp Med Biol. 1980;131:29–43. [PubMed] [Google Scholar]
- [34].Oldendorf WH, Cornford ME, Brown WJ. The large apparent work capability of the blood-brain barrier: a study of the mitochondrial content of capillary endothelial cells in brain and other tissues of the rat. Ann Neurol. 1977;1(5):409–417. doi: 10.1002/ana.410010502. [DOI] [PubMed] [Google Scholar]
- [35].Eisenberg HM, Suddith RL. Cerebral vessels have the capacity to transport sodium and potassium. Science. 1979;206(4422):1083–1085. doi: 10.1126/science.227060. [DOI] [PubMed] [Google Scholar]
- [36].Arieff AI, Doerner T, Zelig H, Massry SG. Mechanisms of seizures and coma in hypoglycemia. Evidence for a direct effect of insulin on electrolyte transport in brain. J Clin Invest. 1974;54(3):654–663. doi: 10.1172/JCI107803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Sekimoto H, Shimada O, Matsutani Y, Nakanish T, Nakano T, Katayama O. Influence of insulin-induced hypoglycemia on ul-trastructure of cerebral arterial endothelium. J Cereb Blood Flow Metab. 1983;3(1):461–462. [Google Scholar]
- [38].LaManna JC, Harik SI. Regional comparisons of brain glucose influx. Brain Res. 1985;326(2):299–305. doi: 10.1016/0006-8993(85)90039-3. [DOI] [PubMed] [Google Scholar]
- [39].Ratcheson RA, Blank AC, Ferrendelli JA. Regionally selective metabolic effects of hypoglycemia in brain. J Neurochem. 1981;36(6):1952–1958. doi: 10.1111/j.1471-4159.1981.tb10820.x. [DOI] [PubMed] [Google Scholar]
- [40].Kaya M, Kucuk M, Kalayci RB, Cimen V, Gurses C, Elmas I, et al. Magnesium sulfate attenuates increased blood-brain barrier permeability during insulin-induced hypoglycemia in rats. Can J Physiol Pharmacol. 2001;79(9):793–798. [PubMed] [Google Scholar]
- [41].Janigro D. Blood-brain barrier, ion homeostasis and epilepsy: possible implications towards the understanding of ketogenic diet mechanisms. Epilepsy Res. 1999;37(3):223–232. doi: 10.1016/s0920-1211(99)00074-1. [DOI] [PubMed] [Google Scholar]
- [42].Altura BM, Altura BT. Association of alcohol in brain injury, headaches, and stroke with brain-tissue and serum levels of ionized magnesium: a review of recent findings and mechanisms of action. Alcohol. 1999;19(2):119–130. doi: 10.1016/s0741-8329(99)00025-7. [DOI] [PubMed] [Google Scholar]
- [43].Charness ME, Simon RP, Greenberg DA. Ethanol and the nervous system. N Engl J Med. 1989;321(7):442–454. doi: 10.1056/NEJM198908173210706. [DOI] [PubMed] [Google Scholar]
- [44].Lyons D, Miller MD, Hedgecock-Rowe AA, Craine AM, Porrino LJ. Time-dependent effects of acute ethanol administration on regional cerebral blood flow in the rat. Alcohol. 1998;16(3):213–219. doi: 10.1016/s0741-8329(98)00005-6. [DOI] [PubMed] [Google Scholar]
- [45].Rossner W, Nusstein R. Alcohol and the blood-brain barrier. Zentralbl Veterinarmed A. 1972;19(6):519–522. [PubMed] [Google Scholar]
- [46].Eriksson T, Carlsson A, Liljequist S, Hagman M, Jagenburg R. Decrease in plasma amino acids in rat after acute administration of ethanol. J Pharm Pharmacol. 1980;32:512–513. doi: 10.1111/j.2042-7158.1980.tb12983.x. [DOI] [PubMed] [Google Scholar]
- [47].Hillbom ME, Tervo TM. Ethanol and acetaldehyde do not increase the blood-brain and blood-retinal barrier permeability to sodium fluorescein. Experientia. 1981;37:936–938. doi: 10.1007/BF01971763. [DOI] [PubMed] [Google Scholar]
- [48].Haorah J, Knipe B, Leibhart J, Ghorpade A, Persidsky Y. Alcohol-induced oxidative stress in brain endothelial cells causes blood-brain barrier dysfunction. J Leukoc Biol. 2005;78:1223–1232. doi: 10.1189/jlb.0605340. [DOI] [PubMed] [Google Scholar]
- [49].Gaw A, Murphy MJ, Cowan R, O’Reilly D, Stewart M, Shepherd J. Coma. In: Gaw A, editor. Clinical Biochemistry. 4th edn. Churchill Livingstone Elsevier; 2008. p. 124. [Google Scholar]
- [50].Hanchar HJ, Chutsrinopkun P, Meera P, Supavilai P, Sieghart W, Wallner M, Olsen RW. Ethanol potently and competitively inhibits binding of the alcohol antagonist R015-4513 to α4/6β3δ GABAA receptors. Proc Natl Acad Sci U S A. 2006;103(22):8546–8551. doi: 10.1073/pnas.0509903103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Qiang M, Denny AD, Ticku MK. Chronic intermittent ethanol treatment selectively alters N-methyl-D-aspartate receptor subunit surface expression in cultured cortical neurons. Mol Pharmacol. 2007;72(1):95–102. doi: 10.1124/mol.106.033043. [DOI] [PubMed] [Google Scholar]


