Abstract
Prenatal exposure to gonadal hormones plays a major role in the normal development of the male and female brain and sexually dimorphic behaviors. Hormone-dependent differences in brain structure and function suggest that exposure to exogenous endocrine disrupting chemicals may be associated with sex-specific alterations in behavior. Bisphenol A (BPA) is an environmental chemical that has been shown to alter estrogen, androgen, and thyroid hormone signaling pathways. Epidemiological and experimental studies suggest associations between prenatal exposure to BPA and child behavior, however data are inconsistent, and few studies have examined school age children. We examined BPA concentration in spot urine samples from women at mean 27 weeks of pregnancy in relation to child behavior assessed at age 6-10 years using the parent-completed Child Behavior Checklist (CBCL). We report associations between maternal BPA urinary concentrations and several CBCL scores in 153 children (77 boys, 76 girls). We observed a significant interaction between maternal urinary BPA and sex for several behaviors (externalizing, aggression, Anxiety Disorder, Oppositional/Defiant Disorder and Conduct Disorder traits), but no significant associations between BPA and scores on any CBCL scales. However in analyses restricted to children of mothers with detectable prenatal urinary BPA (n=125), BPA was associated with moderately increased internalizing and externalizing behaviors, withdrawn/depressed behavior, somatic problems, and Oppositional/Defiant Disorder traits in boys. In addition we observed a significant interaction between BPA and sex for several behaviors (externalizing, withdrawn/depressed, rule-breaking, Oppositional/Defiant Disorder traits, and Conduct Disorder traits). These results suggest that prenatal exposure to BPA may be related to increased behavior problems in school age boys, but not girls.
Keywords: Bisphenol A, Child Behavior Problems, Children, Epidemiology
INTRODUCTION
During fetal development, gonadal hormones contribute to the sexual differentiation of the brain by directing diverse processes such as neurogenesis, differentiation, migration, synapse formation, and cell death (Cooke et al. 1998). Sexual differentiation of the male brain is thought to be largely driven by testosterone, which surges between gestational weeks 8 and 24 with a peak at around 16 weeks (Auyeung et al. 2013). Resultant structural differences across sexes may underlie normal sexually dimorphic behaviors as well as differential prevalence of neuropsychiatric disease in males and females. For example, rates of attention deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and schizophrenia are significantly higher in males, while more females are diagnosed with anxiety disorder and depression (Bao and Swaab 2011). While the mechanisms underlying the striking difference in rates and types of behavioral problems across genders are not well studied, laboratory and epidemiological studies suggest that exposure to exogenous endocrine disrupting chemicals during critical windows of brain development may contribute to sex-specific changes in behavior (Paus 2010; Weiss 2012).
Bisphenol A (BPA), an environmental chemical with known estrogenic activity, has been shown to disrupt brain structure and function in laboratory studies (McCaffrey et al. 2013; Richter et al. 2007b). These findings are consistent with some studies in humans reporting associations between prenatal maternal BPA and child behavior and executive function (Braun et al. 2009; Braun et al. 2011b; Harley et al. 2013b; Perera et al. 2012). BPA is used in the manufacture of can linings, plastic food and beverage containers, thermal receipts, medical equipment, cigarette filters, and dental sealants (Duty et al. 2013; Kloukos et al. 2013) (Ehrlich et al. 2014; Liao and Kannan 2011; Rudel et al. 2011). Exposure to BPA is widespread: biomonitoring studies detect BPA in the urine of more than 90% of those tested in the United States, Canada, and Europe (Centers for Disease Control and Prevention 2013; Vandenberg et al. 2010). In addition to activating estrogen receptors, BPA has been shown to bind androgen and thyroid hormone receptors and is associated with disrupted thyroid hormone production and signaling (Chevrier et al. 2013; Gentilcore et al. 2013; Sohoni and Sumpter 1998). BPA exposure has reportedly been associated with a number of adverse health effects including cardiovascular disease (Lang et al. 2008; Melzer et al. 2010; Shankar et al. 2012), respiratory problems (Donohue et al. 2013; Spanier et al. 2012), obesity (Harley et al. 2013a), prematurity (Cantonwine et al. 2010), infertility (Ehrlich et al. 2012; Li et al. 2010; Meeker et al. 2010b; Mok-Lin et al. 2010), and impaired cognition and behavior (Braun et al. 2009; Braun et al. 2011b; Perera et al. 2012; Yolton et al. 2011).
To date, a small number of studies have examined the association between prenatal exposure to BPA and child behavior, with inconsistent findings. Braun et al. found that gestational exposure to BPA was positively associated with externalizing behaviors in girls at age 2 years, and anxiety, depression, and poor emotional control in girls at age 3 years, but saw no associations in boys using the Behavioral Assessment System for Children (BASC-2) (Braun et al. 2009; Braun et al. 2011b). Results were strongest for maternal urinary BPA measured at 16 weeks compared with BPA at 26 weeks (Braun et al. 2009; Braun et al. 2011b). A second study of children aged 3 to 5 years found that boys born to mothers in the upper quartile of prenatal BPA concentration in urine collected during week 34 of pregnancy exhibited increased emotional reactivity and aggressive behavior on the Child Behavior Checklist (CBCL) compared with other boys (Perera et al. 2012). In contrast, the same study found improved performance on all CBCL scales in girls born to mothers in the upper quartile of BPA exposure compared with other girls (Perera et al. 2012). Likewise, a recent study found an association between average prenatal BPA concentration measured during the 14th and 26th week of pregnancy and increased anxiety and depression in boys, but not girls, at age 7 years as measured by the BASC-2 (Harley et al. 2013b). Finally, two independent studies reported no association between prenatal BPA exposure and social impairment as measured by the Social Responsiveness Scale in children age 7 to 9 years (Braun et al. 2014; Miodovnik et al. 2011). As behavior problems in childhood have been shown to predict behavior problems in adolescence and adulthood, better understanding the relationship of BPA to child behavior could inform this important public health issue (Bardone et al. 1998; Fergusson et al. 2005; Goodwin et al. 2009; Kim-Cohen et al. 2003).
In our study we asked whether prenatal urinary BPA concentrations are associated with sex-specific changes in behavior in children age 6-10 years. To maximize the limited power of our small study we used an efficient parameterization to model sex-by-exposure interactions and utilized two methods to account for subjects with non-detectable urinary BPA.
METHODS
Study Population
Mothers participating in this study were recruited between 2002-2005 into the Study for Future Families II (SFFII), a multicenter pregnancy cohort study designed to examine associations between prenatal environmental exposures and reproductive outcomes (N=474). In 2010, those participants who had provided prenatal urine samples and whose children were ages 6-10 were recontacted and asked to complete neurodevelopmental questionnaires including the CBCL. Of 333 recontacted, 176 participated. Children were excluded from the final analysis if they had incomplete covariate data (N=8), serious disability (N=1), or were younger than age 6 (N=14), resulting in a final cohort of 153 mother-child pairs. Of these, 28 (18.3%) women had BPA concentrations below the limit of detection (LOD), which was 0.4 μg/L.
Institutional Review Boards at all participating institutions approved all procedures, and informed consent was received from all subjects. The involvement of the Centers for Disease Control and Prevention (CDC) laboratory was determined not to constitute engagement in human subject research.
Maternal Urinary BPA Concentrations
Urine samples were collected in BPA-free containers and frozen at −80 °C. Total urinary BPA (free plus conjugated species) was quantified at the Division of Laboratory Sciences, National Center for Environmental Health, CDC by online solid phase extraction-high-performance liquid chromatography-isotope dilution tandem mass spectrometry with peak focusing as previously described (Ye et al. 2005). Each batch of study samples also included analytical standards, reagent blanks, and matrix-based quality control materials at two concentrations (~10 μg/L and ~2.5 μ/L)
Behavioral Assessment
We utilized the parent-rated school-age CBCL, an extensively-validated survey of child behavior (Achenbach T 2001; Greenbaum P 2003; Kamphaus RW 2010). Scores on eight syndrome scales were obtained including: Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints, Social Problems, Thought Problems, Attention Problems, Rule-Breaking Behavior, and Aggressive Behavior. Individual syndrome scores were combined to produce three summary measures; internalizing behavior (sum of Anxious/Depressed, Withdrawn/Depressed, and Somatic Complaints scores), externalizing behavior (sum of Rule-breaking and Aggressive Behavior scores), and a Total Problems score (sum of all scores). In addition, six DSM-oriented scale scores were calculated using scoring of items deemed by child psychiatrists to be consistent with DSM-IV diagnostic categories. These scales include: Affective Problems, Anxiety Problems, Somatic Problems, Attention Deficit/Hyperactivity Problems, Oppositional/Defiant Problems, and Conduct Problems.
For each individual item of the CBCL, parents rated the child on a 3-point scale (0 = “not true”, 1 = “somewhat true”, 2 = “often true”). Each scale consisted of several individual items, and the sum of the parent ratings for each item on an individual scale resulted in a raw score for that scale, where higher scores indicate worse behavior. We utilized continuous raw scores in our primary analyses. Raw scores can be converted to T-scores based on a national normative sample. A T-score of 50 is assigned to raw scores that are at or below the median, thus individual scale T-scores are left truncated and positively skewed. To assess the number of children with scores in the borderline or clinical range on individual scales, we utilized T-scores. Borderline clinical range indicates a score in the 93rd – 97th percentile (T=65-69) of the normative sample for Syndrome and DSM scales and 84th to 90th percentile (T=60-63) for the three summary scales. Clinical range indicates a score above the 97th percentile (T>69) of the normative sample for Syndrome and DSM scales and above the 90th percentile (T>63) for the summary scales (Achenbach T 2001).
Covariates
We collected information on a wide range of variables that are known or suspected to be associated with either child behavior or BPA exposure. These included child sex, child age, prenatal stress, maternal age, maternal education, premature birth (<37 weeks), prenatal smoking, prenatal drug and alcohol use, and maternal depression. Very few (n=0 or 1) subjects reported prenatal drug or alcohol use, or maternal depression, so we were not able to examine these factors in our analysis.
Statistical Analysis
We calculated univariate, descriptive statistics (mean, standard deviation, minimum, median, maximum, or frequencies if applicable) for all covariates and (raw) CBCL outcome measures. We calculated mean, median, geometric mean with 95% confidence interval, and 25th and 75th percentiles for BPA. We measured both specific gravity and urinary creatinine as indicators of urine dilution and found them to be highly correlated with one another. Therefore for descriptive purposes, we accounted for urine dilution by dividing urinary BPA concentration by urinary creatinine concentration to obtain a measure of creatinine-adjusted BPA (μg BPA/g creatinine) (Jackson 1966). In our regression models we used unadjusted BPA and included creatinine as a model covariate. Because of its skewed distribution, we used the natural logarithm (ln) of BPA in our models. Results were considered significant at p<0.05. We examined between-group demographic differences using chi-squared tests and t-tests for normally distributed variables and Mann Whitney U Test for variables that were not normally distributed.
We used multivariate linear regression to examine associations between prenatal urinary BPA and raw CBCL scores. Since previous studies report differences in BPA effects by sex, we fit models both with and without sex-by-BPA interactions. Our first model estimates the overall associations between BPA concentrations and CBCL outcomes, assuming a common slope for boys and girls (Equation 1). Using a re-parameterization of an interaction model (described below) we estimated sex-specific slopes (Equation 2, where sex is coded as 0 for boys and 1 for girls), a model that avoids stratification by sex. Finally, we assessed whether there was a significant interaction between BPA and sex using the interaction model in Equation 3. Equations 2 and 3 are re-parameterizations of the same model, where Equation 3 allows estimation of the significance of the interaction effect, while Equation 2 allows estimation of the sex-specific slopes and their standard errors.
| [1] |
| [2] |
| [3] |
We examined factors reported to affect BPA exposure or our study outcomes for potential inclusion in our multivariable models. Covariates that changed effect estimates by more than 10% or that were hypothesized a priori to be associated with behavioral changes were retained in the final model. These included child sex, child age at time of CBCL completion (in months), mother's education level (at least a college education versus less than a college education), a measure of family stress, and urinary creatinine. Due to the previously reported correlations between prenatal stressful life events (SLEs) and behavioral outcomes in children, we examined the cumulative number of SLEs experienced by both the mother and father during pregnancy (O'Connor et al. 2003; Wadhwa 2005). We asked both parents whether they experienced any of the following during the pregnancy: (1) job loss, (2) serious illness/injury in family, (3) death of close family member, (4) relationship difficulties with partner, (5) legal/financial problems, or (6) any other major event. One point was given for each item on which the mother or father answered “yes” and the sum of all 12 SLEs (six from each parent) were used to generate a summary measure (Dohrenwend et al. 1978).
In our primary analysis, non-detectable maternal urinary BPA concentrations were assigned the value of LOD/√2 as previously recommended (Hornung 1990). We conducted a secondary analysis in which we excluded the 28 subjects with non-detectable maternal urinary BPA concentration, and a tertiary analysis in which maternal urinary BPA was dichotomized at the median. To assess the impact of potentially influential BPA measurements, we conducted a sensitivity analysis in which we excluded subjects with maternal urinary BPA concentration more than three standard deviations from the mean. In addition, each model was checked for statistical outliers, defined as observations with standardized residuals > 3 in absolute value.
Regression assumptions of normality, homoscedasticity and linearity were checked for all models. Based on these diagnostics, we square-root transformed all CBCL raw scores to stabilize the residual variance. This analysis was conducted with SPSS (v21, IBM) and independently verified by a second analyst using R 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Our primary analysis included 153 children (77 boys and 76 girls). Descriptive statistics are shown in Table 1. The average age of the 153 children was 8.5 years, with a range of 6-10.5 years. Mean gestational age at urine collection was 26.6 weeks (range 10-39 weeks) and mean gestational age at birth was 39.3 weeks (range 32-42 weeks). 85% of women had a college education and 92.2% were Caucasian. 90 couples (58.8%) experienced one or more stressful life events during the pregnancy.
Table 1.
Characteristics of 153 subjects in the total cohorta
| All children (n=153) | Boys (n=77) | Girls (n=76) | P-value | |
|---|---|---|---|---|
| Child Age (years); mean±SD | 8.5±1.0 | 8.5±1.0 | 8.5±1.0 | 0.87 |
| Maternal Age at enrollment; mean±SD | 31.1±4.9 | 31.1±4.8 | 31.0±5.1 | 0.81 |
| Gestational age at urine collection in weeks; mean±SD | 26.6±7.2 | 26.9±7.1 | 26.3±7.4 | 0.59 |
| Gestation age at birth in weeks; mean±SD | 39.3±1.6 | 39.2±1.7 | 39.4±1.5 | 0.53 |
| Prematurity (<37 weeks); n(%) | 8(5.3) | 4(5.2) | 4(5.3) | 0.62 |
| Maternal Education; n(%) | 0.24 | |||
| Less than college | 23 (15.0) | 9(11.7) | 14(18.4) | |
| College | 130 (85.0) | 68(88.3) | 62(81.6) | |
| Child Race; n(%) | 0.53 | |||
| Caucasian | 141 (92.2) | 72(93.5) | 69(90.8) | |
| Other | 12 (7.8) | 5(6.5) | 7(9.2) | |
| Family stressful life events during pregnancy n(%) | 0.72 | |||
| 0 | 63(41.2) | 30(39) | 33(43.4) | |
| 1 | 30(19.6) | 17(22.1) | 13(17.1) | |
| >2 | 60(39.2) | 30(39) | 30(39) |
Including children of mothers with prenatal urinary BPA above and below the LOD.
Boys and girls did not differ significantly by child age or maternal age at time of testing, maternal education, family stress level, gestational age at birth, or gestational age at urine collection (Table 1). In multivariable models outcome measures were not altered by more than 10% by inclusion of race, smoking, center location, or gestational age at urine collection so these factors were not included in the final analysis. Although smoking and preterm birth (birth before 37 weeks) are known risk factors for adverse behavioral outcomes in childhood, we did not include either of these in the final model because fewer than 2% of women reported smoking during pregnancy, and only 4 children (3.2%) in the final sample were preterm (Table 1). In addition neither factor was associated with maternal urinary BPA concentrations during pregnancy, and inclusion in the model did not alter the observed association between BPA and behavior by more than 10% (data not shown).
Table 2 shows maternal prenatal urinary BPA concentrations stratified by sex of the child, excluding subjects with non-detectable BPA. Mothers of boys and girls did not differ significantly in their median unadjusted (1.20 vs. 1.00 μg/L) or creatinine adjusted (1.57 vs. 1.56 μg/g creatinine) maternal prenatal urinary BPA concentrations.
Table 2.
Descriptive statistics for prenatal maternal urinary BPA concentration in the total cohorta
| <LOD n(%) | Minimum | 25th | Median | 75th | Maximum | Mean | SD | Geometric Mean | |
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted (μg/L) | |||||||||
| All children (n=153) | 28(18.3) | <LOD | 0.50 | 1.10 | 2.20 | 39.50 | 2.23 | 4.9 | 1.12 |
| Boys (n=77) | 11(14.3) | <LOD | 0.60 | 1.20 | 2.25 | 14.80 | 1.83 | 2.2 | 1.17 |
| Girls (n=76) | 17(22.4) | <LOD | 0.50 | 1.00 | 2.18 | 39.50 | 2.64 | 6.6 | 1.08 |
| Creatinine Adjusted (μg/g creatinine) | |||||||||
| All children (n=153) | 28(18.3) | 0.22 | 1.03 | 1.57 | 2.47 | 190.50 | 3.71 | 15.9 | 1.71 |
| Boys (n=77) | 11(14.3) | 0.36 | 1.08 | 1.57 | 2.31 | 17.50 | 2.36 | 2.5 | 1.75 |
| Girls (n=76) | 17(22.4) | 0.22 | 0.92 | 1.56 | 2.67 | 190.50 | 5.07 | 22.4 | 1.67 |
Including subjects with prenatal maternal urinary BPA above and below the LOD of 0.4 μg/L.
CBCL raw scores stratified by sex are shown in Table 3, where higher scores indicate more parent-reported behavior problems. Behavior among boys was significantly worse than among girls on Attention Problems and Rule-Breaking syndrome scales, Externalizing composite scales, and Affective Disorder, ADHD, Oppositional/Defiant Disorder, and Conduct Disorder DSM scales. The number of boys and girls with scores in the borderline or clinically significant range is given in Supplemental Table 1.
Table 3.
Range and median for raw CBCL scores in boys and girlsa
| Boys (n=77) | Girls (n=76) | |||||
|---|---|---|---|---|---|---|
| Score Range | Mean±SD | Median | Score Range | Mean±SD | Median | |
| Syndrome Scales | ||||||
| Anxious/Depressed | 0-11 | 3.2±2.9 | 2.0 | 0-12 | 2.9±3.0 | 2.0 |
| Withdrawn/Depressed | 0-8 | 1.2±1.8 | 0.0 | 0-10 | 0.9±1.5 | 0.0 |
| Somatic complaints | 0-8 | 1.4±1.7 | 1.0 | 0-8 | 1.3±1.7 | 1.0 |
| Social problems | 0-12 | 2.3±2.4 | 1.0 | 0-7 | 1.8±1.7 | 1.0 |
| Thought problems | 0-11 | 2.2±2.3 | 2.0 | 0-7 | 1.4±1.5 | 1.0 |
| Attention problems | 0-18 | 4.7±3.6 | 4.0** | 0-12 | 2.8±2.9 | 2.0 |
| Rule Breaking | 0-9 | 1.7±1.9 | 1.0* | 0-5 | 0.9±1.1 | 0.5 |
| Aggressive behavior | 0-16 | 4.3±4.2 | 3.0 | 0-14 | 2.9±3.0 | 2.0 |
| Composite Scores | ||||||
| Internalizing | 0-23 | 5.7±5.1 | 5.0 | 0-21 | 5.1±4.7 | 4.0 |
| Externalizing | 0-23 | 6.0±5.7 | 4.0* | 0-16 | 3.8±3.6 | 3.0 |
| Total Problems | 2-70 | 23.8±17.2 | 19.0 | 1-49 | 18.0±11.9 | 15.0 |
| DSM scales | ||||||
| Affective Disorder | 0-8 | 1.6±2.0 | 1.0* | 0-6 | 0.9±1.3 | 0.0 |
| Anxiety Disorder | 0-7 | 1.7±1.8 | 1.0 | 0-8 | 1.4±1.8 | 1.0 |
| Somatic Disorder | 0-7 | 0.8±1.5 | 0.0 | 0-7 | 0.8±1.5 | 0.0 |
| ADHD | 0-11 | 3.9±2.8 | 3.0** | 0-10 | 2.3±2.3 | 2.0 |
| Oppositional/Defiant | 0-8 | 2.3±2.1 | 2.0* | 0-6 | 1.5±1.6 | 1.0 |
| Conduct Disorder | 0-12 | 1.9±2.5 | 1.0** | 0-3 | 0.6±1.0 | 0.0 |
Includes children whose mothers' prenatal BPA concentrations were above and below the LOD
Significantly different from median raw score for girls at p<0.05
Significantly different from median raw score for girls at p<.01. Independent samples Mann-Whitney U Test.
We conducted our primary analysis on 153 subjects in which LOD/√2 was substituted for the 28 subjects with non-detectable urinary BPA. After adjusting for child's age in months, urinary creatinine, child's sex, mother's education (no college vs. college) and SLEs, we observed significant (p<0.05) BPA x Sex interactions (see Equation 3 in Methods) for the aggressive syndrome scale, externalizing composite scale, and Anxiety, Oppositional/Defiant, and Conduct Disorder DSM scales (Table 4). However, no significant associations were observed between BPA and any Syndrome, Composite, or DSM CBCL domains in boys, girls, or the combined cohort (Table 4).
Table 4.
Associations between prenatal maternal urinary (ln)BPA concentration and CBCL Scales in multivariable models in the total cohorta
| Beta(p) Boys + Girls (n=153) | Beta(p) Boys (n=77) | Beta(p) Girls (n=76) | P value for the BPA × Sex Interaction | |
|---|---|---|---|---|
| Syndrome scalesb | ||||
| Anxious/Depressed | −.01(.94) | .15(.28) | −.09(.39) | .13 |
| Withdrawn/Depressed | .04(.56) | .18(.12) | −.03(.72) | .11 |
| Somatic | .12(.10) | .15(.18) | .11(.21) | .75 |
| Social | −.02(.79) | .10(.38) | −.09(.34) | .16 |
| Thought | .06(.45) | .07(.55) | .05(.57) | .89 |
| Attention | −.02(.83) | −.07(.61) | .01(.95) | .63 |
| Rule-Break | −.04(.56) | .11(.31) | −.12(.14) | .06 |
| Aggressive | −.04(.71) | .23(.11) | −.18(.11) | .01 |
| Composite scalesb | ||||
| Internalizing | .12(.28) | .28(.08) | .03(.83) | .16 |
| Externalizing | −.04(.67) | .27(.08) | −.21(.07) | .006 |
| Total Problems | .06(.71) | .29(.19) | −.07(.68) | .15 |
| DSM scalesb | ||||
| Affective | .002(.98) | .02(.89) | −.01(.95) | .87 |
| Anxiety | −.03(.68) | .15(.21) | −.13(.16) | .04 |
| Somatic | .08(.25) | .11(.27) | .06(.44) | .66 |
| ADHD | −.03(.67) | −.05(.70) | −.03(.77) | .89 |
| Oppositional/Defiant | −.02(.77) | .20(.08) | −.14(.10) | .008 |
| Conduct Disorder | −.03(.66) | .22(.05) | −.17(.05) | .003 |
Covariates included in the model: age (months), creatinine, sex, mother's education (no college vs. college), and continuous family stress
Including children of mothers with urinary BPA above and below the LOD, where BPA levels below the LOD were coded as LOD/V2.
Square root transformed continuous raw scores.
It has been suggested that the substitution method for handling subjects with non-detectable values produces biased estimates (Nie et al. 2010). Because a larger than expected number of subjects (18%) had non-detectable maternal urinary BPA concentrations, we conducted a secondary analysis in which we excluded subjects with BPA<LOD (n=28). Demographics and BPA statistics for these 125 subjects are shown in Supplemental Tables 2 and 3, respectively. After adjusting for child's age in months, urinary creatinine, child's sex, mother's education (no college vs. college) and SLEs, prenatal urinary concentrations of BPA were significantly and positively associated with somatic problems in the combined cohort (boys and girls), but no other associations reached statistical significance (Table 5). However, the BPA x Sex interactions (see Equation 3 in Methods) were significant (p<0.05) for withdrawn/depressed and rule-breaking syndrome scores, externalizing composite scores and Oppositional/Defiant and Conduct Disorder DSM scores (Table 4). Estimation of sex-specific slopes (see Equation 2 in Methods) shows that increased maternal prenatal urinary BPA concentrations were associated with withdrawn/depressed and somatic complaints syndrome scores, internalizing and externalizing Composite scales, and Somatic Problems and Oppositional/Defiant DSM scales in boys (Table 5). In contrast, maternal urinary BPA concentration during pregnancy was not significantly associated with any CBCL scores in girls, though the trend was towards negative BPA associations with behavior in girls (Table 5).
Table 5.
Associations between prenatal maternal urinary (In) BPA and CBCL scores in multivariable models among subjects born of mothers with detectable BPA concentrations
| Beta(p) Boys+Girls (n=125) | Beta(p) Boys (n=66) | Beta(p) Girls (n=59) | P-value for the BPA × Sex Interaction | |
|---|---|---|---|---|
| Syndrome scalesa | ||||
| Anxious/Depressed | .06(.61) | .18(.30) | −.02(.91) | 0.35 |
| Withdrawn/Depressed | .04(.66) | .30(.03) | −0.11(.31) | 0.02 |
| Somatic | .17(.04) | .28(.03) | .11(.26) | 0.30 |
| Social | −.01(.89) | −.10(.39) | .13(.35) | 0.19 |
| Thought | .10(.28) | .09(.53) | .10(.36) | 0.94 |
| Attention | −.05(.62) | −.08(.64) | −.04(.77) | 0.84 |
| Rule-Break | −.04(.64) | .22(.10) | −.19(.07) | 0.01 |
| Aggressive | .06(.55) | .28(.09) | −.06(.63) | 0.09 |
| Composite scalesa | ||||
| Internalizing | .21(.09) | .45(.02) | .07(.63) | 0.11 |
| Externalizing | .04(.75) | .35(.05) | −.14(.29) | 0.02 |
| Total Problems | .15(.36) | .46(.08) | −.02(.93) | 0.14 |
| DSM scalesa | ||||
| Affective | .06(.51) | .08(.14) | .05(.66) | 0.85 |
| Anxiety | −.02(.86) | .11(.46) | −.09(.45) | 0.27 |
| Somatic | .18(.02) | .30(.01) | .11(.22) | 0.20 |
| ADHD | −.02(.80) | −.05(.76) | −.01(.92) | 0.85 |
| Oppositional/Defiant | .07(.42) | .28(.04) | −.05(.62) | 0.04 |
| Conduct Disorder | −.03(.70) | .25(.07) | −.20(.07) | 0.009 |
Covariates included in the model: age (months), creatinine, sex, mother's education (no college vs. college) and continuous family stress.
Square root transformed continuous raw scores.
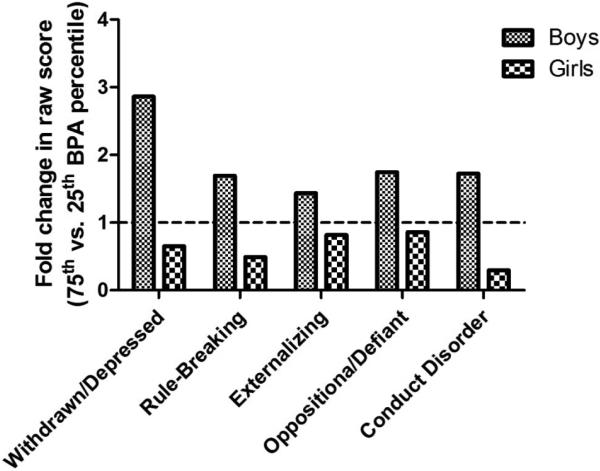
A graph depicting the fold change in raw scores between the 25th and 75th percentiles of BPA on scales in which there was a significant BPA x sex interaction in our secondary analysis of subjects with detectable maternal urinary BPA is shown in Figure 1. We found that boys whose mothers’ urinary BPA concentration was in the 75th percentile had 44% to 186% higher (poorer) scores on withdrawn/depressed and rule breaking syndrome scales, externalizing composite scales, and Oppositional/Defiant Disorder and Conduct Disorder DSM scales relative to boys whose mothers’ urinary BPA concentration was at the 25th percentile. In contrast, girls born to moms in the 75th BPA percentile had scores that were slightly lower (better) than girls born to moms in the 25th percentile on the same domains.
Figure 1.
Fold change in raw scores between the 25th and 75th BPA percentiles for boys and girls on five CBCL domains in which the BPA x Sex interaction term was significant. Covariates in the model include age in months, child sex, maternal education (college vs. no college), and family stress.
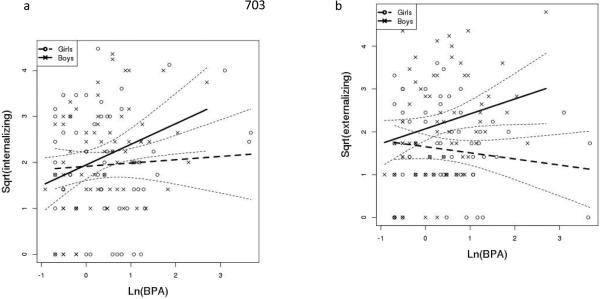
To graphically depict the relationship between ln(BPA) and the square root of internalizing and externalizing composite scores in the subset of subjects with detectable maternal urinary BPA, we generated sex-stratified scatter plots, depicted in Figure 2. The slope of the fitted line shows that the relationship between ln(BPA) and scores on both internalizing (Figure 2a, solid line) and externalizing (Figure 2b, solid line) composite syndrome scales is positive for boys. In contrast, the relationship between ln(BPA) and internalizing behavior in girls approaches the null (Figure 2a, dashed line), and an inverse relationship between ln(BPA) and externalizing scores in girls was observed (Figure 2b, dashed line).
Figure 2.
Scatter plots depicting the association between ln(BPA) and the square root of Externalizing (a) and Internalizing (b) raw scores for boys and girls. The covariate-adjusted slope is depicted for boys (solid line) and girls (dashed line). The dotted lines show 95% confidence intervals for the slopes.
We conducted a tertiary analysis in which we dichotomized BPA at the median and included the children of 28 women with non-detectable BPA (Supplemental Table 4). We observed similar positive trends between prenatal maternal urinary BPA and CBCL scores in boys and not girls. However effects were attenuated compared with our analysis of children whose mothers had detectable BPA.
To assess the impact of possible influential BPA measurements, we conducted a sensitivity analysis in which we excluded the three subjects with maternal urinary BPA concentrations more than three SD above the mean (no subjects had values more than 3 SD below the mean). Exclusion of these 3 subjects strengthened the association between BPA and CBCL outcomes in both the primary and secondary analysis, suggesting that those subjects were not driving significant associations (data not shown). In a separate sensitivity analysis, exclusion of a single statistical outlier with a standardized residual>3 in absolute value did not change the results.
DISCUSSION
This is one of the few published studies to examine associations between prenatal BPA exposure and behavior in school age children. Consistent with previous studies, we observed behavioral sexual dimorphism, with boys showing significantly poorer (i.e. higher) scores than girls in several domains (Achenbach T 2001; Holling et al. 2008). We found significant positive associations in boys between prenatal maternal urinary BPA concentration and subclinical scores in several domains; internalizing and externalizing behaviors, withdrawn/depressed behavior, somatic problems, and oppositional/defiant behaviors. In addition, we found a significant interaction between BPA and child sex for withdrawn/depressed, rule-breaking and externalizing behaviors, and oppositional/defiant and conduct problems, suggesting that the association between prenatal BPA and some behaviors were modulated by child sex.
Our findings are consistent with several, but not all, previous publications. Perera et al reported an association between maternal urinary concentrations of BPA during pregnancy and poorer CBCL scores in boys, and improved CBCL scores in girls aged 3 to 5 years (Perera et al. 2012). They found a significant increase in emotional reactivity and aggressive behavior among the boys in the highest quartile of BPA concentrations compared to the lowest three quartiles of third trimester maternal urinary BPA. Similar to our findings, prenatal concentration in girls was associated with a non-significant improvement in scores on all CBCL domains which reached significance for anxious/depressed behavior and emotional reactivity. Similarly, Harley et al. reported increased internalizing behaviors at age 7 years in boys in relation to the average of BPA in maternal urine samples collected at 13 and 26 weeks of pregnancy, but no significant findings in girls (Harley et al. 2013c). It is interesting to note that although the demographics of our population differ from those of the two aforementioned studies in terms of known behavioral risk factors such as socioeconomic status and maternal education, the associations for prenatal BPA are consistent. This suggests that these associations may be generalizable, however larger confirmatory studies are needed.
In contrast to our findings, Braun et al reported an association between prenatal BPA exposure and externalizing behaviors in girls at age two years, and anxiety, depression, and hyperactivity at age three but no association in boys (Braun et al. 2009; Braun et al. 2011b). Several differences in design between our studies may account for this inconsistency. Findings in their cohort were strongest for BPA concentrations in urine collected at 16 weeks, earlier than the (mean) 27 weeks in our and other previous studies (Harley et al. 2013b, c; Perera et al. 2012). In addition, we utilized different scales (BASC versus CBCL), and children in our cohort were older (age 6-10 versus age 2 years). This suggests that the behavioral effects of BPA exposure may manifest differently depending both on child age and time of exposure. However our findings are consistent with Perera et al whose cohort was 3-5 years old at testing, suggesting that some behavioral effects of prenatal BPA exposures may be long lasting.
The effect of prenatal BPA exposure on childhood behavior is biologically plausible. Disruption of maternal thyroid or gonadal hormones critical to proper brain development may explain the effects of BPA. For example, prenatal BPA exposure is associated with decreased maternal serum free thyroxine (T4)and decreased serum thyroid stimulating hormone (TSH) in male neonates (Chevrier et al. 2013). Several studies have shown associations between urinary BPA concentration and circulating gonadal hormones in adults. In men, urinary BPA has been positively associated with levels of serum testosterone, follicle stimulating hormone (FSH), and sex hormone binding globulin, and inversely associated with estrogen:testosterone ratio and free androgen index (FAI) (Galloway et al. 2010; Meeker et al. 2010a; Mendiola et al. 2010). In adult females, urinary BPA is positively associated with serum sex hormone binding globulin and androgens (Galloway et al. 2010; Takeuchi et al. 2004). Although the relationship between BPA and serum sex hormone levels has not been explored during pregnancy, these findings suggest that alterations in serum gonadal hormones could play a role in sex-specific BPA effects on the developing fetus.
A number of animal studies suggest possible mechanisms by which prenatal BPA exposure may directly alter fetal neurodevelopment (Richter et al. 2007a). Alterations to neocortical structure, changes in estrogen receptor level, disruption of thyroid hormone signaling, and epigenetic changes in the brain have all been described in animal models of prenatal BPA exposure (Itoh et al. 2012; Kundakovic et al. 2013; McCaffrey et al. 2013; Nakamura et al. 2007; Zoeller et al. 2005). Importantly, many of these changes are sexually dimorphic and associated with aberrant behavior.
Our study has several strengths. We utilized the CBCL, a well validated tool for the assessment of child behavior (Achenbach T 2001), and found positive associations between maternal urinary BPA during pregnancy and CBCL raw scores in children at 6-10 years. Raw scores are preferable for statistical analysis given that they provide a continuous measure that reflects all possible variation on a given syndrome or DSM-oriented scale (Achenbach T 2001). In addition, the use of raw scores allows for differentiation between subjects with scores below the clinical or borderline cutoff.
We were able to control for many potential confounders including stressful life events, a measure of prenatal stress, which is a known risk factor for behavioral problems in children (O'Connor et al. 2003; Wadhwa 2005). We considered the role of additional risk factors including prenatal maternal smoking and preterm birth. Finally, we examined outcomes in models that allow a sex-specific BPA slope, a necessity given the known sex differences in child behavior and the endocrine disrupting potential of BPA (Braun and Hauser 2011).
We acknowledge several limitations of this study. Of 333 mothers who had prenatal urinary BPA measurement and complete demographic data only 153 whose children were age 6-10 also completed the CBCL, and of these only 125 had detectable maternal urinary BPA. The 333 women with prenatal urinary BPA measurements did not differ significantly from the final cohort of 125 women in maternal age, maternal urinary BPA concentration, or family stress level (Supplemental Table 5). The sample of 125 subjects with detectable maternal urinary BPA differed from the 333 subjects in the larger cohort in that the smaller sample was significantly more likely to be Caucasian (94% vs 84%, p=0.004) and to have a college education (85% versus 72%, p=0.007). Boys’ mean raw scores in our cohort did not differ significantly in comparison to the normative sample (Achenbach T 2001). However girls performed significantly better than the normative sample on the Rule-Breaking syndrome scale and Oppositional/Defiant and Conduct Disorder DSM scales. Thus, we do not know if our results would generalize to children in higher risk families. It is important to note that few children in our cohort had scores that reached borderline clinical or clinical significance (Supplemental Table 1); further study is needed to determine whether prenatal maternal urinary BPA concentration is associated with clinical diagnoses of one or more behavioral problems.
Although widely utilized, the CBCL is parent-rated, and may be prone to bias and subjectivity (Achenbach T 2001). Future studies should incorporate teacher-rated surveys as well as direct measurement of child behavior, in addition to maternal assessment. In addition, a single spot urine sample is unlikely to provide an accurate estimate of exposure to BPA throughout pregnancy. Recent studies in which multiple urine samples were analyzed indicate considerable variability in urinary concentrations of BPA across pregnancy (Braun et al. 2011a; Braun et al. 2012; Meeker et al. 2013; Philippat et al. 2013; Quiros-Alcala et al. 2013). Moreover, Braun et al reported strongest correlations between adverse behavior and urinary BPA measured at 16 weeks gestation compared with BPA at 26 weeks or at birth (Braun et al. 2009; Braun et al. 2011b). This suggests that our measurements may be subject to misclassification, though this is likely to be nondifferential and it should be noted that the majority of studies that measure BPA have relied on a single spot urine sample. Although we do not have a measure of the child's BPA exposure, two previous studies have shown no association between postnatal exposure and behavior (Braun et al. 2011b; Perera et al. 2012). However, a more recent study did find an association between child urinary BPA at age 5 and problem behaviors at age 7 in both boys and girls, highlighting a need for further research into the role of childhood BPA exposure (Harley et al. 2013c). Because most BPA is rapidly cleared from the body and food is a major source, levels may be confounded by time from last meal as well as time of last urination before urine collection. Inclusion of time of urine collection in the model did not affect outcome measures; however, we lacked information on time of last meal (data not shown).
This study includes a relatively small sample size without sufficient power to include a large number of covariates. In the future larger studies will be better powered to examine the impact of additional potential confounders. Given that pregnant women are simultaneously exposed to numerous environmental factors that may have additive, antagonistic, or synergistic effects, future studies should also examine the effects of exposures to mixtures on behavioral outcomes. Finally, there may be residual confounding by factors related to BPA exposure and child behavior which we were unable to examine.
Mean and median BPA levels in our population were lower than those reported for the US general population and for other cohort studies during the same time period (Perera 2012, Braun 2009, Braun 2011, Harley 2013) and a higher percentage of subjects in our study (18%) had non-detectable maternal urinary BPA than most studies. Percentage of non-detectable BPA was relatively high in three (MN, 21%; MO, 19%; IA, 18%) out of four of the participating centers in our study. Of the 57 California subjects who had maternal urinary BPA measurements, 7% had non-detectable BPA and only 9 subjects from this center completed the CBCL and were included in this analysis. Thus the high percentage of subjects with non-detectable BPA could be explained, at least in part, by geographical location. Additional factors known to affect BPA exposure include time from last meal and smoking (Braun et al. 2011a; Geens et al. 2014; He et al. 2009). Very few subjects (<2%) in this study were smokers and we lack information on fasting time, so we could not determine whether non-detectable BPA correlated with either of these factors. Finally, non-detectable BPA concentration could be explained by very dilute urine, which can be assessed by measuring urinary creatinine concentration. In our study, mean creatinine was significantly lower for subjects with non-detectable BPA (34.4 mg/dL) than for subjects with detectable BPA (94.2 mg/dL), suggesting that urine dilution could at least partially explain the high percentage of subjects with non-detectable BPA in our cohort.
There has been recent discussion in the literature with regards to statistical treatment of biomarker measures below the LOD (Nie et al. 2010). Substitution of LOD/√2 is one commonly used method, however, a more recent examination of this method reports that substitution can produce biased effect estimates, while excluding subjects with non-detectable values produces unbiased estimates, assuming that the effect is approximately linear in nature (Nie et al. 2010). When we conducted analyses using the substitution method to include the 28 subjects whose mothers had non-detectable BPA concentrations in our cohort, we found several associations between maternal BPA and behavior in boys that were attenuated compared to models without these 11 boys and 17 girls (compare Tables 4 and 5). Although subjects with non-detectable BPA did not appear to differ from subjects with detectable BPA, we cannot rule out differences in unmeasured confounders. Deletion of subjects with non-detectable maternal urinary BPA may not be optimal due to a loss of information about subjects with BPA concentrations close to the LOD. Therefore, we conducted tertiary analyses in which we dichotomized BPA at the median (Supplemental Table 4). Further studies are needed to determine the best method to account for non-detectable urinary concentrations.
In conclusion, we report an association between maternal urinary BPA concentrations during pregnancy and sexually dimorphic behaviors in school age children. We observed differential associations between prenatal BPA concentration and behavior measures in boys and girls, with increased adverse behaviors in boys, but not girls, in whom we saw a weak non-significant trend towards improved behavior on several scales. BPA exposure is widespread in the general population and a number of health effects have been associated with exposure. This study further suggests that the prenatal period may represent one of particular vulnerability for adverse neurobehavioral outcomes. Given recent increases in the prevalence of neurobehavioral disorders (Boyle et al. 2011; Visser et al. 2013), additional studies are warranted to further examine the relationship between maternal urinary BPA concentrations during pregnancy and adverse neurobehavioral outcomes.
Supplementary Material
Highlights.
Bisphenol A is an endocrine disrupting chemical that may affect brain development
We studied prenatal urinary BPA and child behavior in 6-10 year olds
BPA was associated with poorer behavior in boys for several CBCL scales
Sex of the child significantly modified several BPA-behavioral associations
Prenatal BPA exposure may be related to behavior problems in school age boys
ACKNOWLEDGEMENTS
This study was supported by grants from the U.S. Environmental Protection Agency and the National Institutes of Health (5T32HD049311 to Icahn School of Medicine at Mount Sinai, R01-ES09916 to the University of Missouri, MO1-RR00400 to the University of Minnesota, MO1-RR0425 to Harbor-UCLA Medical Center, K12 ES019852 and BPA GO Grant (1 RC2 ES018736-01S1) and BPA GO Grant Supplement (1 RC ES018736-015S1) to the University of Rochester School of Medicine and Dentistry) and by grant 18018278 from the State of Iowa to the University of Iowa. It was also supported by UL1 TR000042, KL2 TR000095, and TL1 TR000096 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health. The authors thank Xiaoyun Ye, Tao Jia, Xiaoliu Zhou, and Amber Bishop (CDC, Atlanta, GA) for measuring the urinary concentrations of BPA.
Abbreviations
- ADHD
attention deficit-hyperactivity disorder
- BPA
Bisphenol A
- CDC
Centers for Disease Control and Prevention
- LOD
limit of detection
- EM
Expectation-Maximization
- ICC
Intraclass Correlation Coefficient
- SFF
Study for Future Families
- CBCL
Child Behavior Checklist
- DSM
Diagnostic and Statistical Manual of Mental Disorders
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institutes of Health.
REFERENCES
- Achenbach TRL. Manual for the aseba school-age forms & profiles. University of Vermont Research Center for Children, Youth, and Families; Burlington: 2001. [Google Scholar]
- Auyeung B, Lombardo MV, Baron-Cohen S. Prenatal and postnatal hormone effects on the human brain and cognition. Pflugers Arch. 2013;465:557–571. doi: 10.1007/s00424-013-1268-2. [DOI] [PubMed] [Google Scholar]
- Bao AM, Swaab DF. Sexual differentiation of the human brain: Relation to gender identity, sexual orientation and neuropsychiatric disorders. Front Neuroendocrinol. 2011;32:214–226. doi: 10.1016/j.yfrne.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. J Am Acad Child Adolesc Psychiatry. 1998;37:594–601. doi: 10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in us children, 1997-2008. Pediatrics. 2011;127:1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- Braun JM, Yolton K, Dietrich KN, Hornung R, Ye X, Calafat AM, et al. Prenatal bisphenol a exposure and early childhood behavior. Environ Health Perspect. 2009;117:1945–1952. doi: 10.1289/ehp.0900979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun JM, Hauser R. Bisphenol a and children's health. Curr Opin Pediatr. 2011;23:233–239. doi: 10.1097/MOP.0b013e3283445675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun JM, Kalkbrenner AE, Calafat AM, Bernert JT, Ye X, Silva MJ, et al. Variability and predictors of urinary bisphenol a concentrations during pregnancy. Environ Health Perspect. 2011a;119:131–137. doi: 10.1289/ehp.1002366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun JM, Kalkbrenner AE, Calafat AM, Yolton K, Ye X, Dietrich KN, et al. Impact of early-life bisphenol a exposure on behavior and executive function in children. Pediatrics. 2011b;128:873–882. doi: 10.1542/peds.2011-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun JM, Smith KW, Williams PL, Calafat AM, Berry K, Ehrlich S, et al. Variability of urinary phthalate metabolite and bisphenol a concentrations before and during pregnancy. Environ Health Perspect. 2012;120:739–745. doi: 10.1289/ehp.1104139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun JM, Kalkbrenner AE, Just AC, Yolton K, Calafat AM, Sjodin A, et al. Gestational exposure to endocrine-disrupting chemicals and reciprocal social, repetitive, and stereotypic behaviors in 4- and 5- year-old children: The home study. Environ Health Perspect. 2014;122:513–520. doi: 10.1289/ehp.1307261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantonwine D, Meeker JD, Hu H, Sanchez BN, Lamadrid-Figueroa H, Mercado-Garcia A, et al. Bisphenol a exposure in mexico city and risk of prematurity: A pilot nested case control study. Environ Health. 2010;9:62. doi: 10.1186/1476-069X-9-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention C. Centers for disease control and prevention. 2013. [12/10/2013];National report on human exposure to environmental chemicals, updated tables, september 2013. 2013 Available: http://www.cdc.gov/exposurereport/
- Chevrier J, Gunier RB, Bradman A, Holland NT, Calafat AM, Eskenazi B, et al. Maternal urinary bisphenol a during pregnancy and maternal and neonatal thyroid function in the chamacos study. Environ Health Perspect. 2013;121:138–144. doi: 10.1289/ehp.1205092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke B, Hegstrom CD, Villeneuve LS, Breedlove SM. Sexual differentiation of the vertebrate brain: Principles and mechanisms. Front Neuroendocrinol. 1998;19:323–362. doi: 10.1006/frne.1998.0171. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: The peri life events scale. J Health Soc Behav. 1978;19:205–229. [PubMed] [Google Scholar]
- Donohue KM, Miller RL, Perzanowski MS, Just AC, Hoepner LA, Arunajadai S, et al. Prenatal and postnatal bisphenol a exposure and asthma development among inner-city children. J Allergy Clin Immunol. 2013;131:736–742. e736. doi: 10.1016/j.jaci.2012.12.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duty SM, Mendonca K, Hauser R, Calafat AM, Ye X, Meeker JD, et al. Potential sources of bisphenol a in the neonatal intensive care unit. Pediatrics. 2013;131:483–489. doi: 10.1542/peds.2012-1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlich S, Williams PL, Missmer SA, Flaws JA, Ye X, Calafat AM, et al. Urinary bisphenol a concentrations and early reproductive health outcomes among women undergoing ivf. Hum Reprod. 2012;27:3583–3592. doi: 10.1093/humrep/des328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlich S, Calafat AM, Humblet O, Smith T, Hauser R. Handling of thermal receipts as a source of exposure to bisphenol a. JAMA. 2014;311:859–860. doi: 10.1001/jama.2013.283735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: The consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry. 2005;46:837–849. doi: 10.1111/j.1469-7610.2004.00387.x. [DOI] [PubMed] [Google Scholar]
- Galloway T, Cipelli R, Guralnik J, Ferrucci L, Bandinelli S, Corsi AM, et al. Daily bisphenol a excretion and associations with sex hormone concentrations: Results from the inchianti adult population study. Environ Health Perspect. 2010;118:1603–1608. doi: 10.1289/ehp.1002367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geens T, Bruckers L, Covaci A, Schoeters G, Fierens T, Sioen I, et al. Determinants of bisphenol a and phthalate metabolites in urine of flemish adolescents. Environ Res. 2014;134C:110–117. doi: 10.1016/j.envres.2014.07.020. [DOI] [PubMed] [Google Scholar]
- Gentilcore D, Porreca I, Rizzo F, Ganbaatar E, Carchia E, Mallardo M, et al. Bisphenol a interferes with thyroid specific gene expression. Toxicology. 2013;304:21–31. doi: 10.1016/j.tox.2012.12.001. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Sourander A, Duarte CS, Niemela S, Multimaki P, Nikolakaros G, et al. Do mental health problems in childhood predict chronic physical conditions among males in early adulthood? Evidence from a community-based prospective study. Psychol Med. 2009;39:301–311. doi: 10.1017/S0033291708003504. [DOI] [PubMed] [Google Scholar]
- Greenbaum PDR, Lipien L, editors. The child behavior checklist. In: Comprehensive handbook of psychological assessment, personality assessment. John Wiley & Sons; New York: 2003. [Google Scholar]
- Harley KG, Aguilar Schall R, Chevrier J, Tyler K, Aguirre H, Bradman A, et al. Prenatal and postnatal bisphenol a exposure and body mass index in childhood in the chamacos cohort. Environ Health Perspect. 2013a;121:514–520. 520e511–516. doi: 10.1289/ehp.1205548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harley KG, Gunier RB, Kogut K, Johnson C, Bradman A, Calafat AM, et al. Prenatal and early childhood bisphenol a concentrations and behavior in school-aged children. Environ Res. 2013b doi: 10.1016/j.envres.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harley KG, Gunier RB, Kogut K, Johnson C, Bradman A, Calafat AM, et al. Prenatal and early childhood bisphenol a concentrations and behavior in school-aged children. Environ Res. 2013c;126:43–50. doi: 10.1016/j.envres.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y, Miao M, Herrinton LJ, Wu C, Yuan W, Zhou Z, et al. Bisphenol a levels in blood and urine in a chinese population and the personal factors affecting the levels. Environ Res. 2009;109:629–633. doi: 10.1016/j.envres.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Holling H, Kurth BM, Rothenberger A, Becker A, Schlack R. Assessing psychopathological problems of children and adolescents from 3 to 17 years in a nationwide representative sample: Results of the german health interview and examination survey for children and adolescents (kiggs). Eur Child Adolesc Psychiatry 17 Suppl. 2008;1:34–41. doi: 10.1007/s00787-008-1004-1. [DOI] [PubMed] [Google Scholar]
- Itoh K, Yaoi T, Fushiki S. Bisphenol a, an endocrine-disrupting chemical, and brain development. Neuropathology. 2012;32:447–457. doi: 10.1111/j.1440-1789.2011.01287.x. [DOI] [PubMed] [Google Scholar]
- Jackson S. Creatinine in urine as an index of urinary excretion rate. Health Phys. 1966;12:843–850. doi: 10.1097/00004032-196606000-00014. [DOI] [PubMed] [Google Scholar]
- Kamphaus RW FP. Clinical assessment of child and adolescent personality and behavior. 3rd ed. Springer; New York, NY: 2010. [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kloukos D, Pandis N, Eliades T. In vivo bisphenol-a release from dental pit and fissure sealants: A systematic review. J Dent. 2013 doi: 10.1016/j.jdent.2013.04.012. [DOI] [PubMed] [Google Scholar]
- Kundakovic M, Gudsnuk K, Franks B, Madrid J, Miller RL, Perera FP, et al. Sex-specific epigenetic disruption and behavioral changes following low-dose in utero bisphenol a exposure. Proc Natl Acad Sci U S A. 2013 doi: 10.1073/pnas.1214056110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang IA, Galloway TS, Scarlett A, Henley WE, Depledge M, Wallace RB, et al. Association of urinary bisphenol a concentration with medical disorders and laboratory abnormalities in adults. JAMA. 2008;300:1303–1310. doi: 10.1001/jama.300.11.1303. [DOI] [PubMed] [Google Scholar]
- Li DK, Zhou Z, Miao M, He Y, Qing D, Wu T, et al. Relationship between urine bisphenol-a level and declining male sexual function. J Androl. 2010;31:500–506. doi: 10.2164/jandrol.110.010413. [DOI] [PubMed] [Google Scholar]
- Liao C, Kannan K. Widespread occurrence of bisphenol a in paper and paper products: Implications for human exposure. Environ Sci Technol. 2011;45:9372–9379. doi: 10.1021/es202507f. [DOI] [PubMed] [Google Scholar]
- McCaffrey KA, Jones B, Mabrey N, Weiss B, Swan SH, Patisaul HB. Sex specific impact of perinatal bisphenol a (bpa) exposure over a range of orally administered doses on rat hypothalamic sexual differentiation. Neurotoxicology. 2013;36:55–62. doi: 10.1016/j.neuro.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeker JD, Calafat AM, Hauser R. Urinary bisphenol a concentrations in relation to serum thyroid and reproductive hormone levels in men from an infertility clinic. Environ Sci Technol. 2010a;44:1458–1463. doi: 10.1021/es9028292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeker JD, Ehrlich S, Toth TL, Wright DL, Calafat AM, Trisini AT, et al. Semen quality and sperm DNA damage in relation to urinary bisphenol a among men from an infertility clinic. Reprod Toxicol. 2010b;30:532–539. doi: 10.1016/j.reprotox.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeker JD, Cantonwine DE, Rivera-Gonzalez LO, Ferguson KK, Mukherjee B, Calafat AM, et al. Distribution, variability, and predictors of urinary concentrations of phenols and parabens among pregnant women in puerto rico. Environ Sci Technol. 2013;47:3439–3447. doi: 10.1021/es400510g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melzer D, Rice NE, Lewis C, Henley WE, Galloway TS. Association of urinary bisphenol a concentration with heart disease: Evidence from nhanes 2003/06. PLoS One. 2010;5:e8673. doi: 10.1371/journal.pone.0008673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendiola J, Jorgensen N, Andersson AM, Calafat AM, Ye X, Redmon JB, et al. Are environmental levels of bisphenol a associated with reproductive function in fertile men? Environ Health Perspect. 2010;118:1286–1291. doi: 10.1289/ehp.1002037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miodovnik A, Engel SM, Zhu C, Ye X, Soorya LV, Silva MJ, et al. Endocrine disruptors and childhood social impairment. Neurotoxicology. 2011;32:261–267. doi: 10.1016/j.neuro.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mok-Lin E, Ehrlich S, Williams PL, Petrozza J, Wright DL, Calafat AM, et al. Urinary bisphenol a concentrations and ovarian response among women undergoing ivf. Int J Androl. 2010;33:385–393. doi: 10.1111/j.1365-2605.2009.01014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura K, Itoh K, Sugimoto T, Fushiki S. Prenatal exposure to bisphenol a affects adult murine neocortical structure. Neurosci Lett. 2007;420:100–105. doi: 10.1016/j.neulet.2007.02.093. [DOI] [PubMed] [Google Scholar]
- Nie L, Chu H, Liu C, Cole SR, Vexler A, Schisterman EF. Linear regression with an independent variable subject to a detection limit. Epidemiology 21 Suppl. 2010;4:S17–24. doi: 10.1097/EDE.0b013e3181ce97d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor TG, Heron J, Golding J, Glover V. Maternal antenatal anxiety and behavioural/emotional problems in children: A test of a programming hypothesis. J Child Psychol Psychiatry. 2003;44:1025–1036. doi: 10.1111/1469-7610.00187. [DOI] [PubMed] [Google Scholar]
- Paus T. Sex differences in the human brain: A developmental perspective. Prog Brain Res. 2010;186:13–28. doi: 10.1016/B978-0-444-53630-3.00002-6. [DOI] [PubMed] [Google Scholar]
- Perera F, Vishnevetsky J, Herbstman JB, Calafat AM, Xiong W, Rauh V, et al. Prenatal bisphenol a exposure and child behavior in an inner-city cohort. Environ Health Perspect. 2012;120:1190–1194. doi: 10.1289/ehp.1104492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philippat C, Wolff MS, Calafat AM, Ye X, Bausell R, Meadows M, et al. Prenatal exposure to environmental phenols: Concentrations in amniotic fluid and variability in urinary concentrations during pregnancy. Environ Health Perspect. 2013 doi: 10.1289/ehp.1206335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quiros-Alcala L, Eskenazi B, Bradman A, Ye X, Calafat AM, Harley K. Determinants of urinary bisphenol a concentrations in mexican/mexican-american pregnant women. Environ Int. 2013;59:152–160. doi: 10.1016/j.envint.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter CA, Birnbaum LS, Farabollini F, Newbold RR, Rubin BS, Talsness CE, et al. In vivo effects of bisphenol a in laboratory rodent studies. Reprod Toxicol. 2007a;24:199–224. doi: 10.1016/j.reprotox.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter CA, Taylor JA, Ruhlen RL, Welshons WV, Vom Saal FS. Estradiol and bisphenol a stimulate androgen receptor and estrogen receptor gene expression in fetal mouse prostate mesenchyme cells. Environ Health Perspect. 2007b;115:902–908. doi: 10.1289/ehp.9804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudel RA, Gray JM, Engel CL, Rawsthorne TW, Dodson RE, Ackerman JM, et al. Food packaging and bisphenol a and bis(2-ethyhexyl) phthalate exposure: Findings from a dietary intervention. Environ Health Perspect. 2011;119:914–920. doi: 10.1289/ehp.1003170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar A, Teppala S, Sabanayagam C. Bisphenol a and peripheral arterial disease: Results from the nhanes. Environ Health Perspect. 2012;120:1297–1300. doi: 10.1289/ehp.1104114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohoni P, Sumpter JP. Several environmental oestrogens are also anti-androgens. J Endocrinol. 1998;158:327–339. doi: 10.1677/joe.0.1580327. [DOI] [PubMed] [Google Scholar]
- Spanier AJ, Kahn RS, Kunselman AR, Hornung R, Xu Y, Calafat AM, et al. Prenatal exposure to bisphenol a and child wheeze from birth to 3 years of age. Environ Health Perspect. 2012;120:916–920. doi: 10.1289/ehp.1104175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi T, Tsutsumi O, Ikezuki Y, Takai Y, Taketani Y. Positive relationship between androgen and the endocrine disruptor, bisphenol a, in normal women and women with ovarian dysfunction. Endocr J. 2004;51:165–169. doi: 10.1507/endocrj.51.165. [DOI] [PubMed] [Google Scholar]
- Vandenberg LN, Chahoud I, Heindel JJ, Padmanabhan V, Paumgartten FJ, Schoenfelder G. Urinary, circulating, and tissue biomonitoring studies indicate widespread exposure to bisphenol a. Environ Health Perspect. 2010;118:1055–1070. doi: 10.1289/ehp.0901716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, et al. Trends in the parent-report of health care provider-diagnosed and medicated adhd disorder: United states, 2003—2011. J Am Acad Child Adolesc Psychiatry. 2013 doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadhwa PD. Psychoneuroendocrine processes in human pregnancy influence fetal development and health. Psychoneuroendocrinology. 2005;30:724–743. doi: 10.1016/j.psyneuen.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Weiss B. The intersection of neurotoxicology and endocrine disruption. Neurotoxicology. 2012;33:1410–1419. doi: 10.1016/j.neuro.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X, Kuklenyik Z, Needham LL, Calafat AM. Quantification of urinary conjugates of bisphenol a, 2,5-dichlorophenol, and 2-hydroxy-4-methoxybenzophenone in humans by online solid phase extraction-high performance liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem. 2005;383:638–644. doi: 10.1007/s00216-005-0019-4. [DOI] [PubMed] [Google Scholar]
- Yolton K, Xu Y, Strauss D, Altaye M, Calafat AM, Khoury J. Prenatal exposure to bisphenol a and phthalates and infant neurobehavior. Neurotoxicol Teratol. 2011;33:558–566. doi: 10.1016/j.ntt.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoeller RT, Bansal R, Parris C. Bisphenol-a, an environmental contaminant that acts as a thyroid hormone receptor antagonist in vitro, increases serum thyroxine, and alters rc3/neurogranin expression in the developing rat brain. Endocrinology. 2005;146:607–612. doi: 10.1210/en.2004-1018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.