Abstract
Objectives
To determine if mortality varies by time-to-readmission (TTR).
Summary Background Data
While readmissions reduction is a national healthcare priority, little progress has been made toward understand why only some readmissions lead to adverse outcomes.
Methods
In this retrospective cross-sectional cohort analysis, we used 2005–09 Medicare data on beneficiaries undergoing colectomy, lung resection, or CABG (n=1,033,255) to created five TTR groups: no 30-day readmission (n=897,510), <6 days (n=44,361), 6–10 days (n=31,018), 11–15 days (n=20,797), 16–20 days (n=15,483), or >21 days (n=24,086). Our analyses evaluated TTR groups for differences in risk-adjusted mortality (30-, 60-, and 90-day) and complications during the index admission.
Results
Increasing TTR was associated with a stepwise decline in mortality. For example, 90-day mortality rates in patients readmitted between 1–5 days, 6–10 days, and 11–15 days were 12.6%, 11.4%, and 10.4%, respectively (p<0.001). Compared to non-readmitted patients, the adjusted odds ratios (and 95% confidence intervals) were 4.88 (4.72–5.05), 4.20 (4.03–4.37), and 3.81 (3.63–3.99) respectively. Similar patterns were observed for 30- and 60-day mortality. There were no sizable differences in complication rates for patients readmitted within 5 days versus after 21 days (24.8% vs 26.2%, p<0.001).
Conclusions
Surgical readmissions within 10 days of discharge are disproportionately common and associated with increased mortality independent of index complications. These findings suggest 10-day readmissions should be specially targeted by quality improvement efforts.
Introduction
Hospital readmissions are common, costly, and potentially preventable. In the Medicare population, approximately 1 in 5 patients are readmitted within 30-days of discharge, costing the nation nearly $26 billion per year.1 Further, estimates from the Medicare Payment Advisory Counsel’s Report to Congress found 80% are potentially preventable.2 As a result, curbing hospital readmissions has become a primary focus of national quality improvement efforts. In October of 2012, the Affordable Care Act’s Hospital Readmissions Reduction Program (HRRP) took effect, mandating public reporting of readmission rates and financially penalizing institutions for “excessive” readmissions.3
However, the preponderance of surgical research investigates causes of readmission leaving little known about the consequences of readmission.4,5 First, there is no commonly agreed upon measure for readmission (30-day versus 1-year) or mortality (time-to-death versus 1-year mortality).6–9 Second, with only one multi-institutional study and most research evaluating a single operation, there are concerns regarding the generalizability of prior findings. Third, the existing literature reaches different conclusions on whether an association exists between readmission and mortality.6,7,9–11 Most importantly, stakeholders still struggle for a clinically meaningful way to categorize and evaluate readmissions. To make further headway in determining which readmissions are associated with worse outcomes, it may be useful to deconstruct the most popular measure – the 30-day all-cause readmission. One method is to sub-divide based on the duration of time between discharge and the first readmission (time-to-readmission, TTR). Understanding the degree to which TTR impacts post-discharge mortality might reconcile the disparate findings of prior studies and provide clinicians with a simple method for risk-stratification.
In this context, we used three years of data on Medicare beneficiaries undergoing high-risk surgical procedures to investigate whether post-discharge mortality varies by TTR. Specifically, we sought to address two questions. First, is TTR associated with mortality? Second, are any differences in mortality explained by the occurrence of a post-operative complication during the index admission? We hyopthesized that patients with shorter TTR will have both higher mortality and higher index complication rates.
Methods
Data Source, Procedure Selection, and Patient Population
This is a retrospective cohort analysis of Medicare data drawn from the Medicare Provider Analysis and Review (MedPAR) files. MedPAR includes all claims submitted by hospitals for inpatient services rendered to Medicare beneficiaries. In combination with the Medicare Denominator file, our analytic dataset contained patient demographics (age, gender, and race); dates of admission, discharge, and death; and the International Classification of Disease 9th Revision, Clinical Modification (ICD-9-CM) codes for primary and secondary diagnoses and procedures performed during the hospitalization.12
Two features of Medicare administrative data are particularly useful in studies of readmission. First, Medicare tracks readmissions to any hospital, thus permiting a more accurate estimate of the population’s true readmission rate since there is no “lost to follow-up” effect.5,13 Further, the number of hospitals in the Medicare dataset exceeds, by far, the number of hospitals in any clinical registry.
To test whether our results are applicable across subspecialties, we selected a single procedure from general surgery (open colectomy), thoracic surgery (lung resection), and cardiac surgery (coronary artery bypass grafting, CABG). These procedures are likely candidates for scrutiny under a national strategy to reduce readmissions because each is: (1) a common major surgical procedure, (2) performed on an inpatient basis, and (3) has an unadjusted readmission rate of at least 10%. We included all patients between the ages of 65 and 99 who underwent these procedures between January 1, 2005 and December 31, 2009. Supplemental Digital Content 1. We excluded patients not surviving to discharge since they were unable to be readmitted.
Time-to-Readmission
Our primary exposure variable was time-to-readmission (TTR, ie the number of days between discharge from index hospitalization and the first readmission). In accordance with common practice, patients readmitted on the same day as discharge or after 30 days were not considered to have a readmission.14 We created a 6-level TTR variable: not readmitted within 30 days (n = 897,510), readmitted within 1–5 days (n = 44,361), 6–10 days (n = 31,018), 11–15 days (n = 20,797), 16–20 days (n = 15,483), and 21–30 days (n = 24,086). Analyses modeling TTR as a continuous variable (ranging from 1 to 30) yielded qualitatively similar results to modeling TRR as a 6-level categorical variable. For simplicity, we present the findings of our categorical analysis.
Post-Discharge Mortality
Our primary outcome was risk-adjusted mortality at 30, 60, and 90 days from the index operation. Since we excluded patients who did not survive to discharge from the index hospitalization, our point-estimates for mortality rates are lower than appear in prior studies examining surgical mortality since most report a composite endpoint of inpatient mortality or post-discharge mortality (censored at 30-days from the operation).15–17
Major Complications During the Index Hospitalization
To define post-operative surgical complications, we used methodology originally created by the Complication Screening Project.18,19 Specifically, we generated indicator variables for pulmonary failure, pneumonia, myocardial infarction, venous thromboembolism, renal failure, hemorrhage, surgical site infection, and gastrointestinal bleeding. Supplemental Digital Content 2. Complications defined using this approach demonstrate high specificity and sensitivity and have been adopted by prior studies examining of surgical quality.20–22 In the case of CABG, due to an inability to ascertain temporal sequence, we excluded myocardial infarction as a complication. This is the standard approach for studies analyzing complications in Medicare data.
Calculation of Risk-Adjusted Mortality Rates
Our risk-adjustment model included the following covariates: an indicator variable for each of 29 medical comorbidities (Elixhauser’s method);23 a continuous variable for age; indicator variables for Black race, female gender, non-elective admission (i.e. urgent or emergent), and the occurrence of a complication during index admission; a five-level variable for discharge destination (home, skilled nursing facility/intermediate care facility, long-term care facility, other destination); and a continuous variable for index hospitalization length-of-stay. We formulated two models, a complications naïve model, and one adding index complications as a binary predictor variable. Separate models were generated for each operation.
We used separate multiple logistic regression models to generate risk-adjusted rates for mortality at 30, 60, and 90 days. Specifically, we calculated a predicted probability of mortality for each patient based upon his or her mix of covariates. This predicted probability was used to create an observed-to-expected ratio (OER) for each of the six TTR categories. Finally, we determined point estimates for risk-adjusted mortality rates by multiplying the OER for each TRR category by the post-discharge mortality grand mean for the entire study population.24 Our 95% confidence intervals [CI] were adjusted using the cluster option of STATA’s logistic command to account for the non-independence of outcomes among patients treated at the same hospital.
We evaluated model performance using the C statistic (discrimination) and residual plots (calibration). The C statistic is a measure of the model’s ability to differentiate between patients having versus not having the outcome of interest.25 Our C statistics were consistent with prior literature using similar methods (0.72–0.82).26,27 Calibration reflects the ability of a regression model to predict the number of events compared to actual the data.28 We elected to assess calibration visually rather than using the Hosmer-Lemeshow statistic. As Hosmer-Lemeshow test is based upon a chi-square distribution, in large datasets it becomes more statistically significant despite decreasing deviations from perfect calibration.29 Our visual inspection of model calibration suggested improvement by the addition of variables for index complications, discharge destination, and length of stay.30
Analytic Approach
Our primary analysis evaluated the association between mortality and TTR by comparing risk-adjusted mortality rates and adjusted odds ratios (aOR) across categories of TTR. We generated aORs for each category of TTR, by adding a 6-level TTR variable to our regression models. Non-readmitted patients were used as the common referent group for all comparisons.
Our secondary analysis applied two tests to examine whether differences in mortality were explained by differences in the rate of complications during the index hospitalization. First, we evaluated the change in the point estimates for mortality rates when including versus excluding index hospitalization complications as an explanatory variable. Second, we evaluated whether the prevalence of individual complications varied by time-to-readmission. Finally, we tabulated readmission diagnoses using the Agency for Healthcare Research & Quality (AHRQ) Clinical Conditions Software (CCS) for ICD-9-CM.31
Comparisons of baseline demographic characteristics and comorbidities were made using chi-square tests for binary characteristics and a Wilcoxon rank-sum test for age since this variable was non-normally distributed. All statistical tests were 2-tailed, and a p-value of 0.05 was considered statistically significant. Data management and analyses were performed using STATA software (version 12.1/SE; StataCorp LP, College Station, Texas).
Results
Baseline Characteristics
Our study included 1,033,255 operations. There were statistically significant differences with respect to demographic variables as detailed in Table 1. For some characteristics, the magnitudes of these differences were small. For example, across operations, the maximum difference is median age was less than one year. However, differences were larger for other characteristics. For example, of patients readmitted within 5 days of discharge following colectomy, 55% were female; but of patients readmitted after 21 days, 60% were female (p < 0.001). To empirically adjust for differences in demographic characteristics across categories of TTR, we included all statistically significant covariates in the regression model used to generate risk-adjusted rates and odds ratios.
Table 1.
Patient Characteristics by Time-To-Readmission Category
| Characteristic | No readmit | Time-to-Readmission Category
|
p Value
|
||||
|---|---|---|---|---|---|---|---|
| 1–5 days | 6–10 days | 11–15 days | 16–20 days | >21 days | >21 days vs 1–5 days | ||
| Colectomy | |||||||
| Count, n | 392,491 | 18,583 | 12,413 | 8,211 | 6,223 | 9,982 | n/a |
| Age over 80, % | 30% | 34% | 34% | 35% | 36% | 36% | < 0.001 |
| Gender, % female | 59% | 55% | 58% | 60% | 61% | 60% | < 0.001 |
| Black Race, % | 8% | 10% | 9% | 10% | 10% | 11% | 0.011 |
| 3+ Comorbidities, % | 35% | 39% | 40% | 40% | 40% | 42% | < 0.001 |
| Major Complications, % | 23% | 33% | 34% | 36% | 37% | 36% | < 0.001 |
| Lung Resection | |||||||
| Count, n | 90,188 | 3,324 | 2,331 | 1,766 | 1,346 | 2,137 | n/a |
| Age over 80, % | 13% | 17% | 16% | 16% | 17% | 16% | 0.526 |
| Gender, % female | 50% | 41% | 42% | 46% | 46% | 46% | 0.002 |
| Black Race, % | 6% | 6% | 5% | 6% | 5% | 6% | 0.385 |
| 3+ Comorbidities, % | 35% | 39% | 41% | 39% | 42% | 42% | 0.084 |
| Major Complications, % | 15% | 21% | 23% | 24% | 24% | 22% | 0.449 |
| CABG | |||||||
| Count, n | 414,831 | 22,454 | 16,274 | 10,820 | 7,914 | 11,967 | n/a |
| Age over 80, % | 14% | 19% | 18% | 18% | 18% | 18% | 0.200 |
| Gender, % female | 31% | 35% | 36% | 38% | 38% | 39% | < 0.001 |
| Black Race, % | 5% | 6% | 6% | 6% | 6% | 7% | 0.008 |
| 3+ Comorbidities, % | 35% | 39% | 40% | 40% | 39% | 41% | < 0.001 |
| Major Complications, % | 14% | 19% | 19% | 18% | 18% | 18% | 0.622 |
p values are based on chi-square test comparing 1–5 day and >21 day Time-to-Readmission categories.
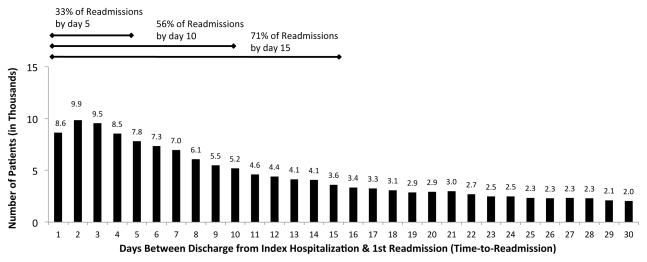
Readmissions
Overall, 13.1% of patients (n = 135,745) were readmitted within 30 days of discharge. Examining each operation separately, the readmission rate was 12.4% for colectomy (n = 55,412), 10.8% for pulmonary resection (n = 10,904), and 14% for CABG (n = 69,429). The frequency of readmission decreased as TTR lengthened. Cumulatively, 50% of all 30-day readmissions occurred within the first 9 days post-discharge, and 75% within 17 days post-discharge. Figure 1. These patterns were similar when we examined each operation individually.
Figure 1.
Frequency of Readmission Following High-Risk Surgery by Time-To-Readmission.
Our study population included 1,033,255 operations with 135,745 (13.1%) readmissions.
The most common reasons for readmission were similar across all TTR groups. By far “post-operative complications” made up the single largest AHRQ Clinical Classification in each TTR category. Table 2 Similarly, congestive heart failure, cardiac dysrhythmia and pneumonia were among the top 4 causes of readmission across all TTR strata.
Table 2.
Top 10 Readmissions Diagnoses Stratified by Time-to-Readmission
| Overall | 1–5 Day Readmission | 6–10 Day Readmission | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Reasons for Readmission | N (% of all readmissions) | Reasons for Readmission | N (%, 1–5d readmissions) | Reasons for Readmission | N (%, 6 –10d readmissions) | |||
| 1 | Post-operative complications | 30,377 | 23.9% | Post-operative complications | 12,225 | 29.2% | Post-operative complications | 7,591 | 26.1% |
| 2 | Congestive heart failure | 11,671 | 9.2% | Congestive heart failure | 4357 | 10.4% | Congestive heart failure | 2,745 | 9.4% |
| 3 | Cardiac dysrhythmias | 6,423 | 5.1% | Cardiac dysrhythmias | 2355 | 5.6% | Cardiac dysrhythmias | 1,469 | 5.1% |
| 4 | Pneumonia | 5,097 | 4.0% | Pneumonia | 1700 | 4.1% | Pneumonia | 1,211 | 4.2% |
| 5 | Pleurisy; pneumothorax | 4,566 | 3.6% | Intestinal obstruction | 1464 | 3.5% | Pleurisy; pneumothorax | 1,122 | 3.9% |
| 6 | Acute renal failure | 3,829 | 3.0% | Pleurisy; pneumothorax | 1378 | 3.3% | Acute renal failure | 903 | 3.1% |
| 7 | Fluid and electrolyte disorders | 3,647 | 2.9% | Gastrointestinal hemorrhage | 1163 | 2.8% | Fluid and electrolyte disorders | 872 | 3.0% |
| 8 | Intestinal obstruction | 3,546 | 2.8% | Respiratory failure | 1133 | 2.7% | Gastrointestinal hemorrhage | 835 | 2.9% |
| 9 | Gastrointestinal hemorrhage | 3,277 | 2.6% | Fluid and electrolyte disorders | 960 | 2.3% | Intestinal obstruction | 810 | 2.8% |
| 10 | Pulmonary heart disease | 2,874 | 2.3% | Acute renal failure | 833 | 2.0% | Pulmonary heart disease | 745 | 2.6% |
| 11–15 Day Readmission | 16–20 Day Readmission | 21+ Day Readmission | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank | Reasons for Readmission | N (% of 11–15d readmissions) | Reasons for Readmission | N (% 16–20d readmissions) | Reasons for Readmission | N (% 21d+ readmissions) | |||
| 1 | Post-operative complications | 4,370 | 22.5% | Post-operative complications | 2,763 | 19.2% | Post-operative complications | 3,428 | 15.3% |
| 2 | Congestive heart failure | 1,677 | 8.6% | Congestive heart failure | 1,156 | 8.0% | Congestive heart failure | 1,736 | 7.8% |
| 3 | Cardiac dysrhythmias | 952 | 4.9% | Cardiac dysrhythmias | 707 | 4.9% | Cardiac dysrhythmias | 940 | 4.2% |
| 4 | Pleurisy; pneumothorax | 745 | 3.8% | Pneumonia | 589 | 4.1% | Pneumonia | 859 | 3.8% |
| 5 | Acute renal failure | 743 | 3.8% | Acute renal failure | 552 | 3.8% | Pleurisy; pneumothorax | 800 | 3.6% |
| 6 | Pneumonia | 738 | 3.8% | Pleurisy; pneumothorax | 521 | 3.6% | Acute renal failure | 798 | 3.6% |
| 7 | Fluid and electrolyte disorders | 645 | 3.3% | Fluid and electrolyte disorders | 490 | 3.4% | Fluid and electrolyte disorders | 680 | 3.0% |
| 8 | Pulmonary heart disease | 507 | 2.6% | Pulmonary heart disease | 366 | 2.6% | Intestinal obstruction | 536 | 2.4% |
| 9 | Gastrointestinal hemorrhage | 478 | 2.5% | Gastrointestinal hemorrhage | 329 | 2.3% | Complication of device | 511 | 2.3% |
| 10 | Intestinal obstruction | 436 | 2.3% | Intestinal obstruction | 300 | 2.1% | Acute myocardial infarction | 482 | 2.2% |
Diagnostic categories are based on AHRQ’s Clinical Classifications Software for ICD-9-CM (available at http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp).
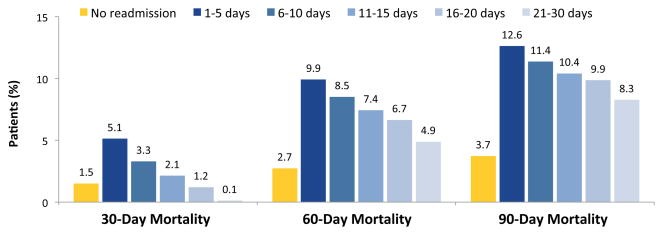
Post-Discharge Mortality
Overall, the risk-adjusted post-discharge mortality rate was 1.7% at 30-days, 3.4% at 60-days, and 4.7% at 90-days. Using 90-day mortality as an example, we had two major findings. First, readmitted patients had higher risk-adjusted post-discharge mortality compared to non-readmitted patients (10.8% vs 3.7%, p < 0.001). Second, risk-adjusted mortality decreased in a linear fashion as TTR increased – 12.7% for patients readmitted within 5 days compared to 8.3% for patients readmitted between 21–30 days (p < 0.001). Figure 2. Patients readmitted within 10 days of discharge had significantly higher mortality compared to patients readmitted after 10 days. For example, readmission within 5 days was associated with a more than 4-fold increase in 90-day mortality (aOR, 4.88; 95% CI 4.72–5.05), while readmission after 21 days was associated with less than a 3-fold difference (aOR, 2.81; 95% CI, 2.67–2.95). Results were qualitatively similar when operations were analyzed individually and for 30- and 60-day mortality. Table 3.
Figure 2.
Rates of Risk-Adjusted Post-Discharge Mortality Following High-Risk Surgery by Time-to-Readmission Category
Table 3.
Adjusted Odds Ratios for Post-Discharge Mortality Following High-Risk Surgery by Time-to-Readmission and Operation
| Time-to-Readmission | Index Admission Complications
|
30-Day Mortality
|
60-Day Mortality
|
90-Day Mortality
|
||||
|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| All Operations Combined | ||||||||
| not readmitted | Referent | Referent | Referent | Referent | ||||
| 1–5 days | 1.27 | (1.24 – 1.31) | 3.84 | (3.65 – 4.04) | 4.90 | (4.72 – 5.09) | 4.88 | (4.72 – 5.05) |
| 6–10 days | 1.29 | (1.25 – 1.33) | 2.31 | (2.16 – 2.47) | 3.98 | (3.81 – 4.16) | 4.20 | (4.03 – 4.37) |
| 11–15 days | 1.28 | (1.23 – 1.32) | 1.44 | (1.32 – 1.58) | 3.41 | (3.23 – 3.60) | 3.81 | (3.63 – 3.99) |
| 16–20 days | 1.30 | (1.25 – 1.35) | 0.79 | (0.69 – 0.90) | 2.97 | (2.79 – 3.16) | 3.55 | (3.36 – 3.75) |
| 21–30 days | 1.23 | (1.19 – 1.27) | 0.07 | (0.05 – 0.10) | 2.02 | (1.90 – 2.14) | 2.81 | (2.67 – 2.95) |
| Colectomy | ||||||||
| not readmitted | Referent | Referent | Referent | Referent | ||||
| 1–5 days | 1.30 | (1.26 – 1.35) | 3.04 | (2.86 – 3.24) | 4.09 | (3.90 – 4.29) | 4.12 | (3.94 – 4.31) |
| 6–10 days | 1.26 | (1.20 – 1.31) | 1.98 | (1.82 – 2.16) | 3.61 | (3.41 – 3.83) | 3.90 | (3.70 – 4.11) |
| 11–15 days | 1.30 | (1.23 – 1.37) | 1.19 | (1.06 – 1.34) | 3.01 | (2.81 – 3.23) | 3.45 | (3.24 – 3.68) |
| 16–20 days | 1.33 | (1.25 – 1.41) | 0.63 | (0.53 – 0.75) | 2.58 | (2.37 – 2.80) | 3.18 | (2.95 – 3.42) |
| 21–30 days | 1.26 | (1.20 – 1.32) | 0.05 | (0.03 – 0.07) | 1.77 | (1.63 – 1.91) | 2.56 | (2.41 – 2.73) |
| Lung Resection | ||||||||
| not readmitted | Referent | Referent | Referent | Referent | ||||
| 1–5 days | 1.34 | (1.22 – 1.47) | 11.17 | (9.43 – 13.22) | 10.09 | (8.90 – 11.44) | 8.12 | (7.26 – 9.09) |
| 6–10 days | 1.44 | (1.29 – 1.61) | 8.07 | (6.54 – 9.95) | 9.62 | (8.33 – 11.11) | 7.92 | (6.97 – 9.00) |
| 11–15 days | 1.55 | (1.36 – 1.77) | 3.48 | (2.49 – 4.86) | 7.10 | (5.98 – 8.45) | 6.20 | (5.31 – 7.23) |
| 16–20 days | 1.57 | (1.36 – 1.81) | 2.69 | (1.83 – 3.96) | 6.71 | (5.52 – 8.15) | 6.51 | (5.52 – 7.67) |
| 21–30 days | 1.40 | (1.25 – 1.57) | 0.18 | (0.06 – 0.55) | 5.63 | (4.73 – 6.70) | 5.97 | (5.16 – 6.90) |
| CABG | ||||||||
| not readmitted | Referent | Referent | Referent | Referent | ||||
| 1–5 days | 1.25 | (1.21 – 1.30) | 5.07 | (4.67 – 5.51) | 5.91 | (5.56 – 6.29) | 5.83 | (5.52 – 6.17) |
| 6–10 days | 1.28 | (1.23 – 1.34) | 2.54 | (2.26 – 2.85) | 4.05 | (3.76 – 4.37) | 4.24 | (3.97 – 4.53) |
| 11–15 days | 1.21 | (1.15 – 1.27) | 1.85 | (1.58 – 2.16) | 3.64 | (3.31 – 4.02) | 3.99 | (3.68 – 4.34) |
| 16–20 days | 1.19 | (1.12 – 1.27) | 0.96 | (0.75 – 1.23) | 3.15 | (2.83 – 3.51) | 3.60 | (3.27 – 3.97) |
| 21–30 days | 1.14 | (1.09 – 1.20) | 0.14 | (0.08 – 0.24) | 1.99 | (1.78 – 2.22) | 2.63 | (2.41 – 2.88) |
aOR, adjusted odds ratio; CI, Confidence interval
Odds ratios are adjusted for patient demographics, Elixhauser comorbidities, admission status, and discharge destination. Odds ratios for mortality is additionally adjusted for complications during the index admission. 95% Confidence intervals account for the clustering of patients within hospitals.
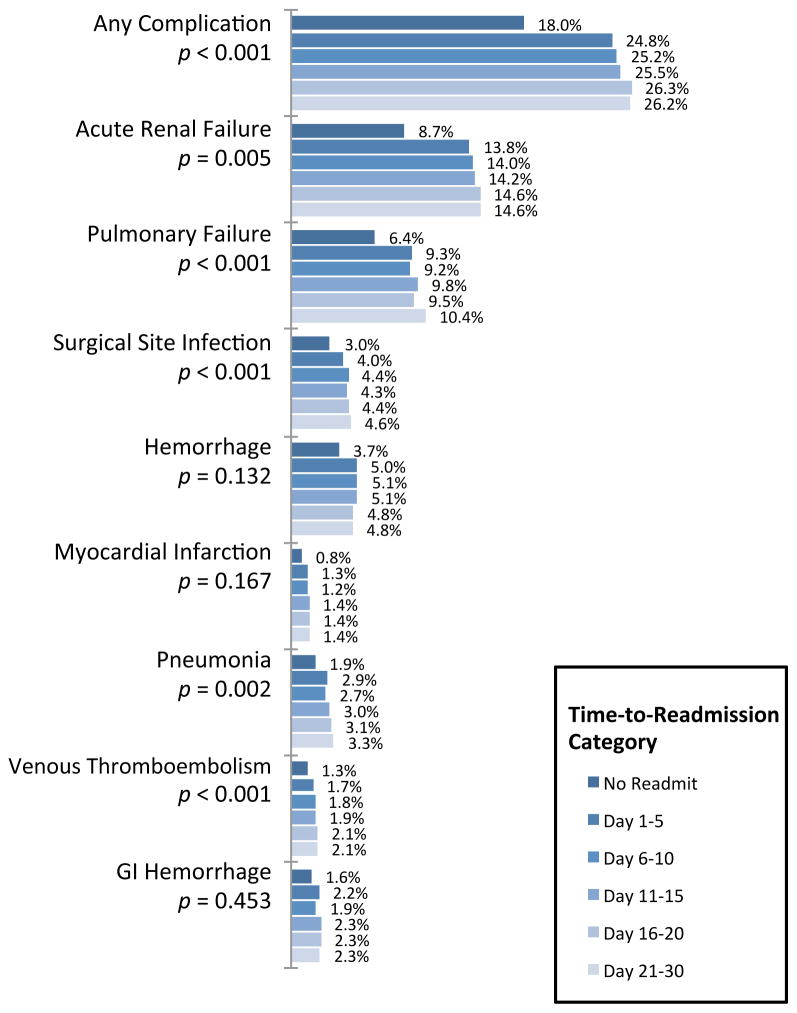
Impact of Complications During Index Hospitalization
Our secondary analysis examined whether the occurrence of a complication during the index hospitalization impacted post-discharge mortality. The difference in rates generated from our complications naïve and complications inclusive models were small. The largest difference in rates was for 90-day mortality – 0.23% on an absolute scale (12.85% vs 12.62%).
We also evaluated whether any individual complication drove differences in across TTR categories. As compared to patients readmitted within 5 days, patients readmitted between 21–30 days had higher rates of acute renal failure, pulmonary failure, surgical site infection, pneumonia, and venous thromboembolism. However, absolute differences were small. For instance, the rate of acute renal failure was 13.8% (TTR < 5 days) versus 14.6% (TTR = 21–30 days), p = 0.005. Figure 4.
Discussion
Our study examined the association between TTR and post-discharge mortality. As TRR increased, we observed a stepwise decrease in mortality. Specifically, patients readmitted within 10 days of discharge had significantly higher risk-adjusted mortality compared to patients readmitted after 10 days. Further, this stepwise decrease in mortality was not explained by differences in the rate of index admission complications. Finally, echoing prior evaluations of surgical patients, we found a disproportionate number of readmissions occurred within one week of discharge.32
While many studies have attempted to determine risk factors for readmission, few have examined the consequences of readmission.33 Gaining further understanding of the relationship between readmission and post-discharge mortality may ultimately facilitate improvements in surgical quality. First, it may identify a specific subset of surgical patients at increased risk of mortality. Heightened vigilance with such patients could assist in preventing or minimizing serious morbidity and mortality. More broadly, the existence of a TTR-mortality relationship may imply hospital profiling should include TTR rather than profiling on readmission rates alone. Not only might this affect performance for public reporting, but it may also influence the specific measures employed by providers to reduce readmissions.
The sparse literature investigating the correlation between readmissions and post-surgical mortality includes two studies utilizing large national datasets. In a study of 42,348 colectomy patients from the Surveillance, Epidemiology, and End Results (SEER) Medicare database, Greenblatt et al found readmitted patients have a two-fold increase in 1-year mortality compared to non-readmitted patients (aOR, 2.44; 95% CI, 2.25 to 2.65).6 To put this difference into a clinical context, Greenblatt et al noted an odds ratio of 2.4 is comparable to upstaging colon cancer patients from stage I to stage III disease.6 The remaining three studies use single-operation or single-institution cohorts and reached different conclusions. A study of CABG and valve operations, showed patients readmitted within 30 days had double the 6-year mortality of non-readmitted patients (14% vs 7%; p < 0.01).7 In contrast, two analyses of patients following major pancreatic resection found no significant differences between the readmitted and non-readmitted groups.8,9
To our knowledge, this is the first study to evaluate the impact of TTR on short-term and mid-term post-operative mortality. Our findings add to the literature on surgical readmissions in two ways. First, we document the first 10-days following discharge as a particularly vulnerable period after high-risk general surgery. This may indicate that the drivers of post-readmission mortality differ depending upon when patients are re-hospitalized.
Second, we observed a relatively weak association between index admission complications and the occurrence of a readmission. Initially, these results may appear to contradict those of a recent study by Lawson et al finding that the occurrence of a post-operative complication increases the probability of readmission by 40% in the ACS-NSQIP dataset.34 However, the discrepancy may be reconciled by a more recent study of clinical registry data from the Veteran’s Administration (VA). In the VA study, Morris et al divided complications into pre- versus post-discharge and found pre-discharge complications were either unassociated or weakly associated with readmission.35 In contrast, post-discharge complications were strongly associated with readmission, with ORs ranging from 7.4 (urinary tract complications) to 59.3 (deep wound infection). One explanation may be that at least some post-discharge complications actually occurred during the index hospitalization but remained unrecognized until readmission.
We extend these prior findings by showing no correlation between TTR and the rate of index admission complications. This suggests varying rates of index complications do not wholly explain differences in post-discharge mortality among readmitted patients. For instance, acute renal failure and pulmonary failure were the most common complications across all TTR categories suggesting no single index complication drives the increased mortality observed following early readmission. From a systems standpoint, this implies that reducing mortality associated with early readmissions may require a comprehensive strategy beyond preventing complications during the index admission.
Limitations
This study is subject to several well known limitations of Medicare data. First, while our model performance was similar to prior Medicare studies, ICD-9 codes may imperfectly account for patient comorbidities, especially with regard to illness severity.16,13,27,36 In addition, administrative data are suboptimal for answering questions relating to (1) specific clinical causes of readmission, (2) determining whether mortality is attributable to the procedure versus progression of disease, and (3) determining which provider made the decision to the readmit a particular patient (i.e. the ER attending, the primary care provider, the hospitalist on duty, the operating surgeon, or the surgeon on call). While AHRQ’s CCS is often used in studies of administrative data, we must stress that these categories are rather broad e.g. “postoperative complication”. Finally, in accordance with the standard practice of censoring readmissions at 30-days (either post-discharge or post-operatively), we did not evaluate patients readmitted after this point in time. However, it should be noted that many of these readmissions might nonetheless be directly related to surgical quality (e.g. wound infections, anastomotic failure).
Conclusion
While reducing readmission is a laudable goal, it is only one stepping-stone on the path to improving post-discharge care. A comprehensive approach to achieve this broader goal will require clinicians, hospitals, and policymakers to have a better understanding of the consequences of readmission. This study identifies patients readmitted within 10 days of discharge as a large and high-mortality subgroup independent of index complications. As ongoing research elucidates the mechanisms behind this increased risk, clinicians might consider paralleling strategies that have improved outcomes in other high-mortality clinical scenarios. For example, the adoption of standardized clinical pathways has led to dramatic reductions in mortality for patients suffering septic shock (Early Goal Directed Therapy), stroke, and acute coronary syndromes (the American Heart Association’s “Get with the Guidelines” recommendations). Perhaps similar approaches might be useful in tackling post-operative readmission-associated mortality. As best practices aimed at preventing readmissions evolve, it is likely hospitals can develop a variety of innovate solutions tailored to specific patient populations and practice environments.
Supplementary Material
PDF. “International Classification of Diseases Procedure Codes Used to Define Operative Cohorts.”
PDF. “International Classification of Diseases Codes Used to Define Post-Operative Complications.”
Figure 3.
Occurrence of Post-operative Complications During Index Hospitalization by Time-to-Readmission Category.
p values refer to chi-square test comparing incidence of a given complication in patients readmitted within 5 days versus readmitted between 21–30 days.
Acknowledgments
Sources of Funding:
This study was supported by grants P01 AG019783-11 (Dr. Birkmeyer), R01 AG0432340-01A1 (Dr. Birkmeyer; Dr. Dimick; Dr. Ghaferi), and R01 AG039434-03 (Dr. Dimick) from the National Institute on Aging; K08 HS017765-04 (Dr. Dimick) from the Agency for Healthcare Research and Quality; a Ruth L. Kirschstein National Research Service Award T32 HL076123-09 from the National Heart Lung and Blood Institute (Dr. Gonzalez), and the Eleanor B. Pillsbury Research Fellowship Award from the University of Illinois Chicago Medical Center (Dr. Gonzalez).
The authors would like to acknowledge Sharmistha Dev, MD for her technical support.
Footnotes
Conflicts of Interest
Drs. Gonzalez, Ghaferi, Abdelsattar, and Mr. Dev have no potential conflicts of interests. Drs. Dimick & Birkmeyer are consultants and equity owners of ArborMetrix, Inc. – an Ann Arbor-based healthcare analytics and information technology firm. ArborMetrix had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication or presentation.
Meeting Presentation: This abstract was presented at the 2014 Academic Surgical Congress in San Diego, CA.
References
- 1.Lavizzo-Mourey R. The Revolving Door: A Report on U.S. Hospital Readmissions [Internet] 2013 Available from: http://bit.ly/1gwqC0V.
- 2.Medicare Payment Advisory Commission (MedPAC) Ch 4 - Refining the hospital readmissions reduction program. Report to the Congress: MEdicare and the Health Care Delivery System [Internet] 2013:91–114. Available from: http://1.usa.gov/1gkJ418.
- 3.Hospital readmissions reduction program 1395ww(q)(1) United States: 42 USC 1395ww(q)(1) 2010
- 4.McPhee JT, Barshes NR, Ho KJ, et al. Predictive factors of 30-day unplanned readmission after lower extremity bypass. J Vasc Surg. 2013;57:955–62. doi: 10.1016/j.jvs.2012.09.077. [DOI] [PubMed] [Google Scholar]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. NEJM. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Greenblatt DY, Weber SM, O’Connor ES, et al. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010;251:659–69. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee R, Homer N, Andrei A, et al. Early readmission for congestive heart failure predicts late mortality after cardiac surgery. J Thorac Cardiovasc Surg. 2012;144:671–6. doi: 10.1016/j.jtcvs.2012.05.031. [DOI] [PubMed] [Google Scholar]
- 8.Emick DM, Riall TS, Cameron JL, et al. Hospital Readmission After Pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1243–53. doi: 10.1016/j.gassur.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Kent TS, Sachs TE, Callery MP, et al. Readmission after major pancreatic resection: a necessary evil? J Amer Coll Surg. 2011;213:515–23. doi: 10.1016/j.jamcollsurg.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 10.McAdams-Demarco MA, Grams ME, King E, et al. Sequelae of early hospital readmission after kidney transplantation. Am J Transplant. 2014;14:397–403. doi: 10.1111/ajt.12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reddy DM, Townsend CM, Kuo Y-F, et al. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–75. doi: 10.1007/s11605-009-1006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Medicare & Medicaid Services. MEDPAR [Internet] 2013 [cited 2014 Mar 17]. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareFeeforSvcPartsAB/MEDPAR.html.
- 13.Nasir K, Lin Z, Bueno H, et al. Is Same-Hospital Readmission Rate a Good Surrogate for All-hospital Readmission Rate? Med Care. 2010;48:477–81. doi: 10.1097/MLR.0b013e3181d5fb24. [DOI] [PubMed] [Google Scholar]
- 14.Quality Net. Measure Methodology Reports: Readmission Measures [Internet] 2013 [cited 2013 Nov 11]. Available from: http://bit.ly/1hrSC9s.
- 15.Birkmeyer JD, Dimick JB, Staiger DO. Operative mortality and procedure volume as predictors of subsequent hospital performance. Ann Surg. 2006;243:411–7. doi: 10.1097/01.sla.0000201800.45264.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gordon HS, Johnson ML, Wray NP, et al. Mortality after noncardiac surgery: prediction from administrative versus clinical data. Med Care. 2005;43:159–67. doi: 10.1097/00005650-200502000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon Volume and Operative Mortality in the United States. NEJM. 2003;349:2117–27. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 18.Weingart SN, Iezzoni LI, Davis RB, et al. Use of Administrative Data to Find Substandard Care: Validation of the Complications Screening Program. Med Care. 2000;38:796–806. doi: 10.1097/00005650-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Iezzoni LI, Daley J, Heeren T, et al. Identifying Complications of Care Using Administrative Data. Med Care. 1994;32:700–15. doi: 10.1097/00005650-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez AA, Dimick JB, Birkmeyer JD, et al. Understanding the volume-outcome effect in cardiovascular surgery: the role of failure to rescue. JAMA Surg. 2014;149(2):119–23. doi: 10.1001/jamasurg.2013.3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Staiger DO, Dimick JB, Baser O, et al. Empirically derived composite measures of surgical performance. Med Care. 2009;47:226–33. doi: 10.1097/MLR.0b013e3181847574. [DOI] [PubMed] [Google Scholar]
- 22.Dimick JB, Nicholas LH, Ryan AM, et al. Bariatric surgery complications before vs after implementation of a national policy restricting coverage to centers of excellence. JAMA. 2013;309:792–9. doi: 10.1001/jama.2013.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elixhauser A, Steiner C, Harris D, et al. Comorbidity Measures for Use with Administrative Data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Dimick JB, Staiger DO, Baser O, et al. Composite Measures For Predicting Surgical Mortality In The Hospital. Health Aff. 2009;28:1189–98. doi: 10.1377/hlthaff.28.4.1189. [DOI] [PubMed] [Google Scholar]
- 25.Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21:128–38. doi: 10.1097/EDE.0b013e3181c30fb2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital Volume and Failure to Rescue With High-Risk Surgery. Med Care. 2011;49:1076–81. doi: 10.1097/MLR.0b013e3182329b97. [DOI] [PubMed] [Google Scholar]
- 27.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in Hospital Mortality Associated with Inpatient Surgery. NEJM. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 28.Merkow RP, Hall BL, Cohen ME, et al. Relevance of the C-Statistic When Evaluating Risk-Adjustment Models in Surgery. J Amer Coll Surg. 2012;214:822–30. doi: 10.1016/j.jamcollsurg.2011.12.041. [DOI] [PubMed] [Google Scholar]
- 29.Cohen ME, Ko CY, Bilimoria KY, et al. Optimizing ACS NSQIP Modeling for Evaluation of Surgical Quality and Risk: Patient Risk Adjustment, Procedure Mix Adjustment, Shrinkage Adjustment, and Surgical Focus. J Amer Coll Surg. 2013;217:336–56. doi: 10.1016/j.jamcollsurg.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 30.LaValley MP. Logistic regression. Circulation. 2008;117:2395–9. doi: 10.1161/CIRCULATIONAHA.106.682658. [DOI] [PubMed] [Google Scholar]
- 31.Agency for Healthcare Research & Quality. [Accessed June 15, 2014];Clinical Classifications Software (CCS) for ICD-9-CM. Available at http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 32.Fong ZV, Ferrone CR, Thayer SP, et al. Understanding hospital readmissions after pancreaticoduodenectomy: can we prevent them?: a 10-year contemporary experience with 1,173 patients at the Massachusetts General Hospital. J Gastrointest Surg. 2014;18:137–44. doi: 10.1007/s11605-013-2336-9. [DOI] [PubMed] [Google Scholar]
- 33.Lum HD, Studenski SA, Degenholtz HB, et al. Early hospital readmission is a predictor of one-year mortality in community-dwelling older Medicare beneficiaries. J Gen Intern Med. 2012;27:1467–74. doi: 10.1007/s11606-012-2116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: Implications for quality improvement and cost savings. Ann Surg. 2013;258:10–8. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
- 35.Morris MS, Deierhoi RJ, Richman JS, et al. The Relationship Between Timing of Surgical Complications and Hospital Readmission. JAMA Surg. 2014 Feb 12; doi: 10.1001/jamasurg.2013.4064. [online first] [DOI] [PubMed] [Google Scholar]
- 36.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, Failure to Rescue, and Mortality With Major Inpatient Surgery in Medicare Patients. Ann Surg. 2009;250:1029–34. doi: 10.1097/sla.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PDF. “International Classification of Diseases Procedure Codes Used to Define Operative Cohorts.”
PDF. “International Classification of Diseases Codes Used to Define Post-Operative Complications.”