Abstract
Purpose
This paper reports on presentations and discussion from the working group on “Influences on Sedentary Behavior & Interventions” as part of the Sedentary Behavior: Identifying Research Priorities Workshop.
Methods
Interventions were discussed in the context of targeting sedentary behavior (SB) as a concept distinct from physical activity (PA). It was recommended that interventions targeting SB should consider a life course perspective, a position predicated on the assumption that SB is age and life stage dependent. Additionally, targeting environments where individuals have high exposure to SB— such as workplace sitting— could benefit from new technology (e.g., computer-based prompting to stand or move), environmental changes (e.g., active workstations), policies targeting reduced sedentary time (e.g., allowing employees regular desk breaks), or by changing norms surrounding prolonged sitting (e.g., standing meetings).
Results & Conclusions
There are limited data about the minimal amount of SB change required to produce meaningful health benefits. In addition to developing relevant scientific and public health definitions of SB, it is important to further delineate the scope of health and quality of life outcomes associated with reduced SB across the life course, and clarify what behavioral alternatives to SB can be used to optimize health gains. SB interventions will benefit from having more clarity about the potential physiological and behavioral synergies with current PA recommendations, developing multi-level interventions aimed at reducing SB across all life phases and contexts, harnessing relevant and effective strategies to extend the reach of interventions to all sectors of society, as well as applying state-of-the-science adaptive designs and methods to accelerate advances in the science of sedentary behavior interventions.
Keywords: physical activity, sedentary behavior, sitting, behavior change
This paper reports on the proceedings as part of a joint workshop sponsored and organized by the National Heart, Lung, and Blood Institute and National Institute on Aging entitled the “Influences on Sedentary Behavior/Interventions to reduce sedentary behavior”. A panel of experts in behavioral health, PA interventions, and health information technology to increase activity levels convened to discuss the major factors that might influence interventions for reducing sedentary behaviors. This workshop was not convened to conduct a systematic review of the literature, since there are several recent publications that have done so (see (7, 10, 21, 31, 37). The working group used an overarching framework involving literature reviews and discussions aimed at elucidating the “WHAT, HOW, with WHOM, in what CONTEXT, and with WHAT EFFECT” of interventions for reducing sedentary behavior. This central framework was expanded through bimonthly conference calls and email discussions. Recommendations evolved from this activity were discussed and presented to an international group of sedentary behavior researchers who participated in a 2.5-hour webinar workshop, and were modified according to the discussion that ensued. It is important to recognize that interventions are substantially influenced by the specific definitions of sedentary behavior that are being applied and which contribute to elevated health risk. For example, the recommendations put forth below should generally apply to a definition of SB that is restricted to activities with intensities ≤1.5 metabolic equivalents or to activities that also consider posture (standing vs. sitting or reclining posture).
Recommendation 1
There is a need to evaluate the feasibility, acceptability, and effectiveness of different SB intervention strategies across the life course; population diversity (emphasizing a range of sample characteristics) should be a key feature of study design that includes different age and cultural groups as well as life phases and roles to address the continued problem of health disparities.
Rationale
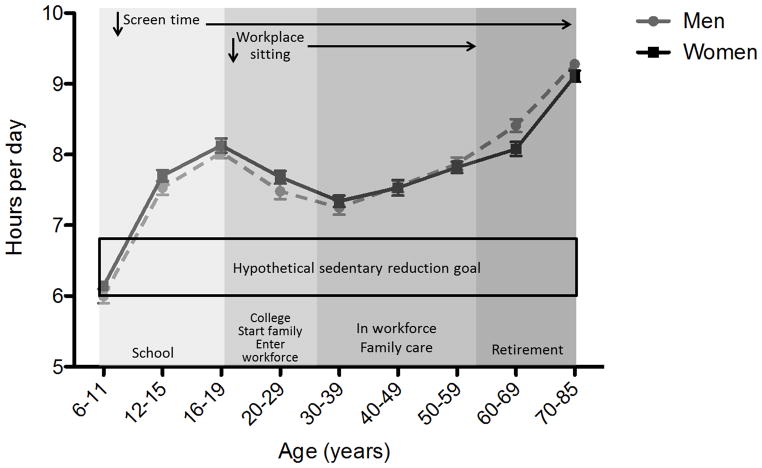
Sedentary behaviors at any age may have important proximal and distal consequences for health and well-being. Thus, a compelling case can be made for SB interventions that consider a life course perspective. Additionally, risk and risk perceptions often change across the lifespan and can be targeted in developing specific age- or life course-related SB interventions (see Figure 1).
Figure 1.
Daily hours in sedentary behavior across the lifespan according to accelerometer data collected by the National Health and Nutrition Examination Survey (NHANES). Sedentary behavior is variable across the lifespan and this could have implications on designing interventions according to life situations experienced by each age group.
Age, health status, social and environmental contexts, and life roles are expected to moderate the acceptability and effectiveness of any SB intervention. A useful goal is to explore components of interventions that may generalize across age groups and life situations, thereby enhancing subsequent effects on population health. Additionally, the specific health effects of an intervention are expected to vary in each phase of life — e.g. an older adult might have a larger health benefit from reducing SB than a younger adult. However, little is currently known about such strategies and their health impact in specific life phases. For example, are interventions that modify social norms about sitting equally effective in schools and worksites? Are strategies to reduce television viewing similarly effective for different age groups? Intervening with older adults may require different types of messages and approaches than those used for middle aged or younger adults.
Approaches to public health and medical interventions are typically geared toward those who are exposed to the highest health risk. For SB, this might include occupations as well as recreational pursuits involving prolonged sitting, such as avid “gamers” or those who watch extensive amounts of television. Additionally, it is currently unclear across different life stages or ages whether individuals who meet or exceed PA recommendations, yet accumulate large amounts of SB, should be targeted. Some epidemiological evidence suggests MVPA may not fully protect against the adverse health consequences of prolonged SB (i.e., the two behaviors may have independent consequences for at least some health outcomes and in at least some populations) (17, 18, 22). However, other studies claim that physical activity can ameliorate some of the cardiometabolic risk of SB (11, 27). As such, there remains an important opportunity to study the joint effects of PA and SB interventions on a variety of health outcomes and in a range of populations.
It is further recommended that outcomes be matched to the life course to ensure their relevance to the population segments being targeted. For example, SB interventions with the goal of improving mobility, reducing pain, and/or increasing cognitive function may be particularly relevant for older adults. A growing number of epidemiological studies have examined the association of SB with longer-term health outcomes such as cardiovascular disease, diabetes, and death (9, 16, 22). Unfortunately, such studies do not specifically inform interventions about which health outcomes to pursue in order to optimize the potential benefits of reducing SB. Additionally, a measure of “health” should not be limited to cardiometabolic disease outcomes, where much of the literature currently exists, but also include such areas as musculoskeletal disorders, psychosocial functioning, and the preservations of independent living..
Recommendation 2
There are multiple possible target LEVELS for intervening on SB across the life course, including individual, interpersonal, organizational, environmental, and policy. Multi-level and systems approaches have the potential to have larger-scale effects and should be evaluated. “Solution-oriented” intervention approaches are recommended to advance more rapid changes at multiple levels.
Rationale
SB may be targeted via multiple interconnected levels of influence. Potential levels of intervention include the individual, organizational, environmental, and policy levels. It is beyond the scope of this article to synthesize the vast number of opportunities to intervene at each of these levels. However, the working group suggested approaching SB intervention research across all levels and audiences using a solution-oriented research approach that favors interventions that are directly applicable to policy and practice (33, 36). The rationale behind solution-oriented research is to more rapidly advance the intervention field through targeting questions and employing methods that have direct implications for changing policy and practice (33, 36). A solution may be tested without first demonstrating the actual underlying cause of the problem. An example is using a randomized controlled design, based on current evidence, to test the effects of replacing sugar sweetened drinks in schools with calorie free options on change in weight without first waiting for definitive experimental “proof” that sugar sweetened drinks “cause” weight gain in children (8, 17, 18, 22). Additionally, experimental studies of hypothesized solutions can also contribute important information concerning potential causal relationships, and allows for more relevant exploration of moderators that identify groups likely to be most responsive to an intervention and mediators (potential pathways) of change (9, 16, 22, 33, 36). A solution-oriented experimental design also can more quickly inform the scientific community and public about such relations without potentially redundant observational research that repeatedly identifies the same set of hypothesized putative factors without testing a potential solution (20, 25, 33, 36). SB interventions are well suited for solution-oriented research because there is already a significant amount of knowledge about the general health effects of not engaging in PA. An example can be found in observational data which shows a low correlation between television viewing and childhood obesity (28). Yet, when screen time was experimentally reduced through family-focused or school-based behavior change interventions and limited access, children gained significantly less weight than control groups which did not receive the interventions (12, 34). Thus, without the need to first prove that screen time causes weight gain, these studies found that interventions to reduce screen time can reduce weight gain and the results can be directly translated into practice and policy.
Randomized controlled trials evaluating the effects of active workstations on reducing workplace SB and, potentially body weight, represent another area amenable to solution-oriented research (20, 25). Although there is currently no direct evidence that workplace SB is a cause of obesity, it is known that people generally sit on average 100 minutes more and stand 75 minutes less on work days than they do when not working (29). Moreover, SB is characterized by low metabolic rate. Therefore, there is sufficient rationale to directly study the effects of workplace interventions to reduce SB for improved energy balance and weight without first proving that workplace SB causes obesity. In fact, pilot studies of treadmill desks have led to reductions in body weight and waist circumference (20, 25). However, for this approach to be effective on a global scale the employer would need to restructure the organization for SB reduction. It’s unclear whether employers could project the cost-to-benefit ratio for absorbing the initial costs associated with purchasing new equipment to implement these workplace interventions. Based on a 2013 survey, 77% of companies that offer health benefits also offer at least one health promotion program and a third of employers place employee health and well-being near the top of their priority list (17, 18, 22, 38). Therefore, it is conceivable that some employers will directly invest in workplace interventions for SB reduction if there is sufficient evidence that the program is sustainable, does not impair productivity, demonstrates medical care savings, reduces absenteeism, and/or enhances the employer’s overall image (6, 9, 15, 16, 22). Unfortunately, to our knowledge, a thorough evaluation of costs and savings of workplace interventions for reducing SB has not been conducted.
There was also group consensus for the need to explore multi-level interventions, i.e., those that attempt to reduce SB at multiple levels of influence. Although evidence is lacking, there is a belief that intervening simultaneously at multiple levels, in multiple settings within levels, and with multiple intervention components within and across levels and settings will produce greater and longer-lasting effects. For example, interventions to reduce screen time in children may be more effective and durable if they include school curricula along with family interventions, screen-use time management technologies, and coordinated community-wide campaigns for a screen-free week. Similarly, workplace SB interventions may be more effective and sustainable if they combine individual smart phone monitoring and feedback about SB levels along with workplace social comparison and competition activities, availability of treadmill desks, and media campaigns to influence social norms about SB. These multi-level approaches need to be tested to see if the expected synergies are in fact realized.
A distinction is also made between multi-level interventions and systems approaches. Systems approaches attempt to design interventions more holistically, to accommodate dynamic and non-linear changes over time, higher order interactions between intervention components and other influences on SB, potential feedback loops that may magnify or attenuate the effects of an intervention, and multiple causal pathways acting simultaneously. This is considered a promising perspective to apply to the reduction of SB.
Recommendation 3
Research is needed on how new technologies can be integrated with principles of behavioral science to reduce SB. Technology should capitalize on interventions at multiple levels of analysis that are designed to accommodate the determinants of SB across the life course.
Rationale
Information technology aimed at intervening on SB received significant attention during working group discussions. Although there are a limited number of studies in this regard, King and colleagues evaluated the initial effects of three smartphone apps designed to promote PA and reduce SB in a group of middle-aged and older adults new to smartphone technology (45 years and older) (24). The apps were designed to reflect three different motivational domains: one that targeted cognitive and self-regulatory skill-building, one that targeted social influence, and a third targeting motivation through operant conditioning principles using an avatar. The apps resulted in an average decrease of ~30 minutes per day of television viewing time (24). These data suggest that adopting dynamic system models for designing technologies can take advantage of concepts from classic theories of behavior change.
Other technology that uses computer software to target people with high levels of work-related sitting is also under development. For example, point-of-choice prompting software programs that remind people to take breaks after prolonged bouts of sitting at a computer have become available. When compared to a group randomized to receive education about health risks of prolonged sitting, a group receiving computer-based prompting had one less prolonged sitting event per hour and one less hour of prolonged sitting per day (13). Newly developed technology takes this concept one step further by implanting a gyroscope and accelerometer in the office chair, which turns the chair into an input device and feedback system for its user (30). This interactive chair tracks movements (rotation, tilt, bounce) that trigger actions on the computer screen, thereby making light movements necessary to control one’s computer. While such technologies have potential for targeting SB, they also have many challenges to overcome including timing and content of the prompts. In addition, it is unclear whether such changes in sitting habits produced by prompting technologies have payoffs for health outcomes.
Some studies have demonstrated reduced occupational sitting time through environmental changes such as introducing active workstations into the workplace (1, 5, 20, 25). For example, Koepp and colleagues conducted a 12-month intervention where office workers’ “sitting” desks were replaced with a treadmill desk (25). After 6 months, workers decreased their daily sedentary time by an average of 91 minutes, but the effect was diminished at 12 months to 43 minutes. There was some relation of the intervention to changes in body weight, whereby obese workers lost an average of 2.3 kg. However, using a sit-to-stand workstation, Gilson and colleagues failed to show any effect on SB (14). Another study examined seated active workstations where employees were asked to use portable pedal machines to promote “active sitting”. Compared to controls, the intervention group reduced daily sedentary time an average of 58.7 min/day over 3 months (4). Overall, the existing active workstation intervention studies provide some evidence in small groups of people that SB in workplaces can be effectively reduced through environmental modifications.
Recommendation 4
The “drivers” of SB include both elements of conscious decision-making and habitual responses cued or required by the milieu or by public policy. Thus, interventions should take advantage of changes in the built and social environments, the use of social networks, and the promotion of relevant public policy changes.
Rationale
Using proven behavioral strategies, incorporating messages to build awareness, and adopting new technology can provide a foundation for developing SB interventions. Traditional strategies of behavior change that require cognitive awareness might need to be complemented and/or supplemented with interventions that address automatic, habitual action (or inaction). Similarly, dynamic feedback and control systems are being increasingly applied in the mobile technology arena, but have not yet been fully incorporated into traditional strategies for behavior change. These strategies may need modification to optimize effectiveness of dynamic feedback SB interventions (32).
Health messaging can play an important role by motivating and facilitating behavioral change. Given prior research on delivering PA messages, it seems reasonable to apply what was learned from these experiences to SB (3, 17, 19, 23, 39, 40). As reviewed by Brawley and Latimer, messages can follow research established by health communicators and marketers (2, 26). Messages could be tailored to present information in a way that matches the individual’s characteristics to make them more relevant (e.g. messages for a workers in a call center will be different than workers in a warehouse). Second, messages could be framed by emphasizing either the benefits (e.g. stand up for your health) or consequences (e.g. sitting increases your blood sugar). Lastly, the message could target self-efficacy beliefs that encourage participation in the goal activity by making it more feasible and enjoyable (e.g. It’s easy to take a 1 minute standing break once an hour— All office workers can do it!). Some direct messages may include: “sit less”, “sit less & move about instead”, or “instead of sitting, do: active sitting, standing, and light activity”. Indirect messages where the environmental design or social norms are modified to reduce SB can also be developed. For example, reducing air pollution, greenhouse gas emissions, and dependence on foreign oil may be motivating reasons to reduce SB by limiting automobile driving and substituting more active modes of transportation, and providing a basis for “stealth interventions” (35).
The CDC’s “VERB” campaign— a social marketing campaign to increase physical activity among youth— is an example of a large campaign that used such messaging techniques to increase PA awareness and behavior in “teen” children. The campaign used positive messages that portrayed activity as an “opportunity to discover the world around them” or as a “way to have fun with friends”(1–3). Prior to the start of the campaign, extensive research was conducted on youth and parents to gain an understanding of their attitudes, beliefs, and behaviors toward PA. A similar message awareness system could be developed for groups for which SB is highly prevalent, but such messages typically cannot be marketed in isolation. The messages require tailoring to the populations, environment, culture, social context, and many other elements that have been described in detail elsewhere (1, 2).
Conclusions
The charge of the “Influences on Sedentary Behavior & Interventions” working group was to establish recommendations for advancing intervention efforts targeting SB. The group concluded that the design of SB interventions should consider the priorities outlined. Considering the large amount of epidemiological data on the health risks of SB, there is a clear rationale for conducting experimentally based studies on SB interventions that are expected to lead to solutions that increase daily activity— even at a light intensity level. Because the behavior is common and seemingly universal across cultures as well as the life course, identifying effective SB interventions could provide a potentially large impact on population health. Such interventions are urgently needed to combat the pandemic of SB.
Acknowledgments
The workshop was sponsored by the National Heart, Lung and Blood Institute, the National Institute on Aging and the Office of Disease Prevention of the National Institute of Health. The views expressed in this document reflect the collective ideas and opinions of the authors and does not necessarily represent the official views of the National Institutes of Health, or the U.S. Department of Health and Human Services and the other workshop participants. Support for this work was provided in part by R01AG042525 to T.M.M. and the University of Florida’s, Claude D. Pepper Center (P30AG028740). The primary author was provided with an honorarium from the National Institutes of Health for his participation in the workshop. We greatly appreciate the thoughts and comments provided by the following discussants who participated in this webinar: Dr. Jacqueline Kerr (University of California San Diego), Dr. Jo Salmon (Deakin University. -Australia), and Dr. Shawn Youngstedt (University of South Carolina). The results of the present study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
Authors declared no conflicts of interest related to this manuscript.
References
- 1.Alkhajah TA, Reeves MM, Eakin EG, Winkler EA, Owen N, Healy GN. Sit–Stand workstations: A pilot intervention to reduce office sitting time. American Journal of Preventive Medicine. 2012;43(3):298–303. doi: 10.1016/j.amepre.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 2.Brawley LR, Latimer AE. Physical activity guides for canadians: Messaging strategies, realistic expectations for change, and evaluation this article is part of a supplement. Applied Physiology, Nutrition, and Metabolism. 2007;32(S2E):S170–S184. doi: 10.1139/H07-159. [DOI] [PubMed] [Google Scholar]
- 3.Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Education and Counseling. 1999;36(2):181–192. doi: 10.1016/s0738-3991(98)00134-7. [DOI] [PubMed] [Google Scholar]
- 4.Carr LJ, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: A randomised controlled trial. BMJ Open. 2013;3(10):e003261-2013-003261. doi: 10.1136/bmjopen-2013-003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carr LJ, Walaska KA, Marcus BH. Feasibility of a portable pedal exercise machine for reducing sedentary time in the workplace. British Journal of Sports Medicine. 2012;46(6):430–435. doi: 10.1136/bjsm.2010.079574. [DOI] [PubMed] [Google Scholar]
- 6.Cherniack M, Lahiri S. Barriers to implementation of workplace health interventions: An economic perspective. Journal of Occupational and Environmental Medicine / American College of Occupational and Environmental Medicine. 2010;52(9):934–942. doi: 10.1097/JOM.0b013e3181f26e59. [DOI] [PubMed] [Google Scholar]
- 7.Costigan SA, Barnett L, Plotnikoff RC, Lubans DR. The health indicators associated with screen-based sedentary behavior among adolescent girls: A systematic review. Journal of Adolescent Health. 2013;52(4):382–392. doi: 10.1016/j.jadohealth.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 8.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. New England Journal of Medicine. 2012;367(15):1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 9.Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting–a health hazard. Diabetes Research and Clinical Practice. 2012;97(3):368–376. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 10.Dunstan DW, Barr EL, Healy GN, Salmon J, Shaw JE, Balkau B, Owen N. Television viewing time and mortality: The australian diabetes, obesity and lifestyle study (AusDiab) Circulation. 2010;121(3):384–391. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 11.Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A International Children’s Accelerometry Database (ICAD) Collaborators. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. Jama. 2012;307(7):704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, Robinson TN. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Archives of Pediatrics & Adolescent Medicine. 2008;162(3):239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans RE, Fawole HO, Sheriff SA, Dall PM, Grant PM, Ryan CG. Point-of-choice prompts to reduce sitting time at work: A randomized trial. American Journal of Preventive Medicine. 2012;43(3):293–297. doi: 10.1016/j.amepre.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Gilson ND, Suppini A, Ryde GC, Brown HE, Brown WJ. Does the use of standing ‘hot’desks change sedentary work time in an open plan office? Preventive Medicine. 2012;54(1):65–67. doi: 10.1016/j.ypmed.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Goetzel RZ, Ozminkowski RJ. The health and cost benefits of work site health-promotion programs. Annu Rev Public Health. 2008;29:303–323. doi: 10.1146/annurev.publhealth.29.020907.090930. [DOI] [PubMed] [Google Scholar]
- 16.Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: A meta-analysis. JAMA. 2011;305(23):2448–2455. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. European Heart Journal. 2011;32(5):590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289(14):1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 19.Huhman ME, Potter LD, Duke JC, Judkins DR, Heitzler CD, Wong FL. Evaluation of a national physical activity intervention for children: VERB™ campaign, 2002–2004. American Journal of Preventive Medicine. 2007;32(1):38–43. doi: 10.1016/j.amepre.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 20.Jones RA, Hinkley T, Okely AD, Salmon J. Tracking physical activity and sedentary behavior in childhood: A systematic review. American Journal of Preventive Medicine. 2013;44(6):51–658. doi: 10.1016/j.amepre.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 22.Katzmarzyk PT. Physical activity, sedentary behavior, and health: Paradigm paralysis or paradigm shift? Diabetes. 2010;59(11):2717–2725. doi: 10.2337/db10-0822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.King AC, Hekler EB, Grieco LA, Winter SJ, Sheats JL, Buman MP, Cirimele J. Harnessing different motivational frames via mobile phones to promote daily physical activity and reduce sedentary behavior in aging adults. PloS One. 2013;8(4):e62613. doi: 10.1371/journal.pone.0062613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koepp GA, Manohar CU, McCrady-Spitzer SK, Ben-Ner A, Hamann DJ, Runge CF, Levine JA. Treadmill desks: A 1-year prospective trial. Obesity. 2013;21(4):705–711. doi: 10.1002/oby.20121. [DOI] [PubMed] [Google Scholar]
- 25.Latimer AE, Brawley LR, Bassett RL. A systematic review of three approaches for constructing physical activity messages: What messages work and what improvements are needed? The International Journal of Behavioral Nutrition and Physical Activity. 2010;7:36–5868-7-36. doi: 10.1186/1479-5868-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levine JA, Miller JM. The energy expenditure of using a “walk-and-work” desk for office workers with obesity. British Journal of Sports Medicine. 2007;41(9):558–561. doi: 10.1136/bjsm.2006.032755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maher C, Olds T, Mire E, Katzmarzyk PT. Reconsidering the sedentary behaviour paradigm. PloS One. 2014;9(1):e86403. doi: 10.1371/journal.pone.0086403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marshall SJ, Biddle SJ, Gorely T, Cameron N, Murdey I. Relationships between media use, body fatness and physical activity in children and youth: A meta-analysis. International Journal of Obesity. 2004;28(10):1238–1246. doi: 10.1038/sj.ijo.0802706. [DOI] [PubMed] [Google Scholar]
- 29.McCrady SK, Levine JA. Sedentariness at work: How much do we really sit? Obesity. 2009;17(11):2103–2105. doi: 10.1038/oby.2009.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Probst K, Lindlbauer D, Greindl P, Trapp M, Haller M, Schwartz B, Schrempf A. Rotating, tilting, bouncing: Using an interactive chair to promote activity in office environments. Paper presented at the CHI’13 Extended Abstracts on Human Factors in Computing Systems; 2013. pp. 79–84. [Google Scholar]
- 31.Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: A systematic review. American Journal of Preventive Medicine. 2012;42(3):e3–e28. doi: 10.1016/j.amepre.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 32.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: Are our theories up to the task? Translational Behavioral Medicine. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robinson TN. Reducing children’s television viewing to prevent obesity: A randomized controlled trial. JAMA. 1999;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 34.Robinson TN. Save the world, prevent obesity: Piggybacking on existing social and ideological movements. Obesity. 2010;18(S1):S17–S22. doi: 10.1038/oby.2009.427. [DOI] [PubMed] [Google Scholar]
- 35.Robinson TN. Solution-oriented policy research: Using research to drive obesity prevention and control policies. Archives of Pediatrics & Adolescent Medicine. 2012;166(2):189–190. doi: 10.1001/archpediatrics.2011.1411. [DOI] [PubMed] [Google Scholar]
- 36.Robinson TN, Sirard JR. Preventing childhood obesity: A solution-oriented research paradigm. American Journal of Preventive Medicine. 2005;28(2):194–201. doi: 10.1016/j.amepre.2004.10.030. [DOI] [PubMed] [Google Scholar]
- 37.Salmon J, Tremblay MS, Marshall SJ, Hume C. Health risks, correlates, and interventions to reduce sedentary behavior in young people. American Journal of Preventive Medicine. 2011;41(2):197–206. doi: 10.1016/j.amepre.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 38.Stein AD, Shakour SK, Zuidema RA. Financial incentives, participation in employer-sponsored health promotion, and changes in employee health and productivity: HealthPlus health quotient program. Journal of Occupational and Environmental Medicine. 2000;42(12):1148–1155. doi: 10.1097/00043764-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Wijndaele K, Brage S, Besson H, Khaw KT, Sharp SJ, Luben R, Ekelund U. Television viewing time independently predicts all-cause and cardiovascular mortality: The EPIC norfolk study. International Journal of Epidemiology. 2011;40(1):150–159. doi: 10.1093/ije/dyq105. [DOI] [PubMed] [Google Scholar]
- 40.Wong F, Huhman M, Heitzler C, Asbury L, Bretthauer-Mueller R, McCarthy S, Londe P. VERB - a social marketing campaign to increase physical activity among youth. Preventing Chronic Disease. 2004;1(3) [PMC free article] [PubMed] [Google Scholar]