Abstract
PURPOSE and METHODS
Though evidence is accumulating that sedentary behavior (SB), independent of moderate-to-vigorous intensity physical activity (MVPA), is associated with cardiometabolic and aging outcomes in adults, several gaps present opportunities for future research. This paper reports on the ‘Research Evidence on Sedentary Behavior’ session of the Sedentary Behavior: Identifying Research Priorities workshop, sponsored by the National Heart, Lung and Blood Institute and the National Institute on Aging, which aimed to identify priorities in SB research.
RESULTS and CONCLUSIONS
A consensus definition of SB has not yet been established, though agreement exists that SB is not simply all behaviors other than MVPA. The two most common definitions are: one based solely on intensity (<1.5 metabolic equivalents (METS)) and another which combines low intensity (≤1.5 METS) with a seated or reclining posture. Thus, for the definition of SB, evaluation of whether or not to include a postural component is a research priority. SB assessment methodologies include self-report and objective measurement, each offering distinct information. Therefore, evaluation, standardization, and comparison across self-report and objective assessment methods are needed. Specific priorities include the development and validation of novel devices capable of assessing posture and standardization of research practices for SB assessment by accelerometry. The prospective evidence that SB relates to health outcomes is limited in that SB is almost exclusively measured by self-report. The lack of longitudinal studies with objectively-measured SB was recognized as a major research gap, making examination of the association between objectively-measured SB and adverse health outcomes in longitudinal studies a research priority. Specifically, studies with repeated measures of SB, evaluating dose-response relationships, with inclusion of more diverse populations are needed.
Keywords: Sedentary behavior, cohort studies, objective activity assessment, epidemiology
This paper reports on the proceedings from the first of four sessions of the Sedentary Behavior: Identifying Research Priorities workshop jointly sponsored and organized by the National Heart, Lung, and Blood Institute and the National Institute on Aging. The first session, ‘Research Evidence on Sedentary Behavior’, discussed the definition of sedentary behavior, measurement of sedentary behavior, and current observational evidence that sedentary behavior is linked to cardiometabolic and aging health outcomes in adult populations. Sedentary behavior research in pediatric populations, an important but separate area of research, was not discussed. The overarching goal of the workshop was to identify the highest research priorities, along with lesser but still important research questions, that could advance the understanding of the impact of sedentary behavior on health. This report describes the proceedings of the workshop.
Recommendation 1
Establish a definition of sedentary behavior.
Rationale
A standardized definition of sedentary behavior has obvious benefits for clarifying the impact of sedentary behavior on health outcomes. Standardization would improve the ability to make comparisons across studies and provide better distinction between physical inactivity (the absence of moderate-to-vigorous intensity physical activity (MVPA)) and a sedentary lifestyle (high levels of sedentary behavior). However, a variety of definitions exist in the literature, varying from self-reported time spent watching television to objectively-measured time at low intensities in a seated position (11).
Of the available definitions, two versions are most commonly utilized, with the main difference being the inclusion of a posture component. The first defines sedentary behavior only by intensity, specifically any waking behavior or activity engendering ≤1.5 metabolic equivalents (METS) (22). This definition only requires measurement of intensity (e.g. by simple accelerometry). Furthermore, this intensity-only definition fits within the context of an overall activity pattern often used in epidemiologic research (see Figure 1A), where non-sedentary waking behavior is classified as light (1.5–2.9 METS), moderate (3.0–5.9 METS), or vigorous (≥6.0 METS) physical activity (19). A weakness of this definition is that it does not include position or posture, a fundamental construct of the word ‘sedentary’ which originates from the Latin origin ‘sedere’ – to sit. Without posture, potentially important hypotheses, for example whether standing is more healthful than sitting, are not able to be tested due to the narrow range and potentially overlapping MET values of these behaviors.
Figure 1.
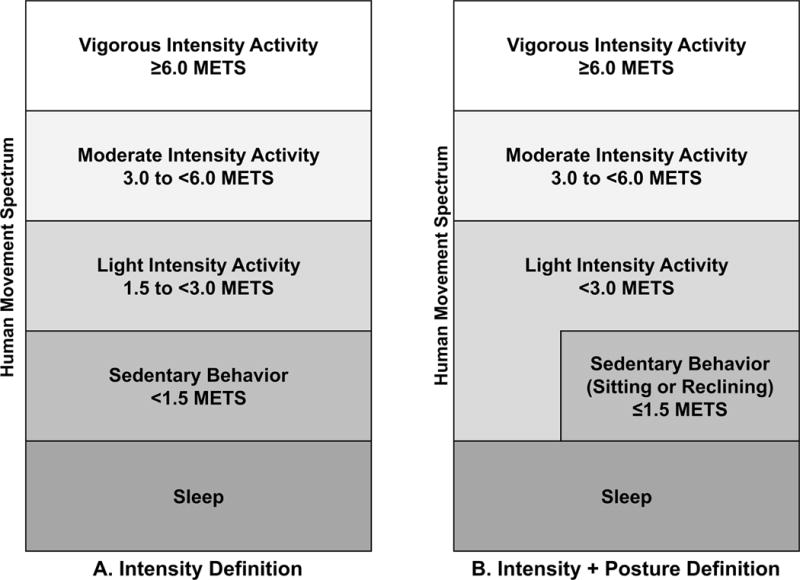
Defining Sedentary Behavior as Part of the Human Movement Spectrum. Sedentary behavior is often defined by intensity alone (A) or intensity + posture (B). The difference between the definitions is that behaviors that are not seated/reclining and are also low intensity (≤1.5 METS), e.g. standing, are considered sedentary behavior by the intensity definition (A) but light intensity by the intensity + posture definition (B).
The second common definition, described in 2012 by the Sedentary Behaviour Research Network, defines sedentary behavior as ‘any waking behavior characterized by an energy expenditure ≤ 1.5 METS while in a sitting or reclining posture’ (25). This definition includes both intensity (≤1.5 METS) and position (sitting or reclining), which is more consistent with the etymology of ‘sedentary’ (Figure 1B). A strength of this definition is that it affords researchers the ability to test posture-based hypotheses. Assessment of posture and intensity is readily available by self-report, and, more recently, commercial devices. However, there are limited commercial devices that have been shown to provide a valid and reliable measure of both intensity and posture. Moreover, there are limited existing datasets available that objectively assess both intensity and posture.
Accumulating epidemiological and clinical trial evidence suggests that non-seated behaviors that engender <1.5 METS (e.g. quiet standing) could contribute to better health. In the Canada Fitness Survey, self-reported proportion of time spent standing had an inverse, dose-response relationship to mortality (13). Though published reports are mostly short-term (e.g., ≤3 months) (1, 3, 23, 27, 31), workplace interventions that replace sitting with standing by using standing desks or other methods have observed distinct improvements in cardiometabolic risk factors, for example in improved HDL cholesterol (1) and post-prandial glucose excursions (3). Laboratory physiological studies can also provide insight, as discussed in more detail in the ‘Physiology of Sedentary Behavior and its Relationship to Health Outcomes’ manuscript from this series (29). For example, a recent study revealed a distinction between standing and sitting postures by showing that muscle activation was almost 2.5 times higher when standing as compared to sitting (30).
Other issues worth mentioning are whether reclining and sleep should be classified as sedentary behaviors. It is unclear if reclining is between sitting down and lying down or includes lying down, which may distinctly lack muscular activation vs. sitting (32). Yet, it is also possible that wakeful, lying down contributes to adverse health outcomes via similar pathways to sitting, and this is an area for future study. Also, technically, sleep could be interpreted as a sedentary behavior and a large body of evidence links both insufficient and excessive sleep to physiologic changes and adverse health outcomes (4, 9). However, in general, sleep has not been included as part of sedentary behavior in the growing body of literature finding associations between sedentary behavior and adverse health outcomes and this is another area for further study.
In summary, while there is agreement that sedentary behavior certainly includes sitting at <1.5 METS while awake, establishing whether low-intensity behaviors at <1.5 METS (e.g. standing) should also be included in the definition is a priority. This task should be undertaken by an expert panel with sufficient resources and authority. In support of this effort, when possible, further research using both definitions in epidemiological studies or evaluating physiological differences between the two definitions in field and laboratory-based studies would be useful. In addition, studies should be transparent about which definition of sedentary behavior is being used and how sedentary behavior is assessed. For example, studies using accelerometry that are not able to assess posture should clearly state the use of the intensity only definition.
Recommendation 2
Improve and standardize methods to assess sedentary behavior.
Rationale
The uncertainty surrounding the need for posture in the definition of sedentary behavior poses challenges for measuring and evaluating measures of sedentary behavior, in addition to the difficulty in quantifying human behavior. Current self-report assessment methods for sedentary behavior include questionnaires, behavioral logs, and recalls. Objective measures can include accelerometers, heart rate monitors, inclinometers, and other devices, some of which are combinations of these devices. As reviewed by Healy and colleagues (11), self-report measures are low cost and can assess domain-specific sedentary behavior (e.g. work-related, television). However, self-report of sedentary behavior has measurement error which results in fair-to-good reliability but lower validity when compared to criterion measures. On the other hand, objective monitoring of sedentary behavior can reduce measurement error and provide information about patterns of activity (e.g. breaks, duration of sedentary episodes) and MVPA. Disadvantages of objective monitoring include cost, participant burden, massive amounts of data that must be digested into functional summary statistics, failure of some devices to register both position and intensity or certain types of activity (e.g. riding on a stationary bicycle), and lack of information on specific domain of behavior.
Both self-report and objective measures could be important to move the science forward. In an analysis of data from the National Health and Nutrition Examination Survey (NHANES) 2003–2006, Healy and colleagues (11) demonstrate that self-reported and objective sedentary behavior are complementary and each provides unique information. For example, television viewing time was similar for Mexican Americans and non-Hispanic Blacks (self-report) while total time spent in sedentary behavior was higher in non-Hispanic Blacks vs. Mexican Americans (objective) (11). Thus, understanding and, potentially, improving the validity and reliability of both self-report and objective measures is a priority. Moreover, because of the distinct information offered by each, a better understanding of the performance characteristics across methods is needed. Two specific high priority areas in sedentary behavior research are mentioned below.
Priority 2.1
Develop and/or validate novel objective monitoring devices that can assess posture and intensity.
Rationale
As described in the previous section, posture might be an important component of the sedentary behavior definition. Devices capable of measuring position through, for example, inclinometers or cameras will be valuable for studying the risks of sedentary behavior as defined by low intensity and a seated or lying posture. A recent validity study among 40 University employees (aged 18–70) in free-living conditions (14) compared sedentary behavior assessed by an accelerometer (<100 counts per minute (cpm)) to individually coded images captured by a small, wearable camera. This study found that certain behaviors (e.g. television viewing, computer use, and administrative activities) were usually correctly classified using the standard 100-cpm threshold from simple accelerometry. However, standing still (9% of the total time captured) generated <100 cpm 72% of the time, indicating that the majority of time spent standing would be classified as sedentary behavior when using a simple accelerometer. Similarly, riding in a car generated ≥100 cpm 26% of the time, and would therefore have been incorrectly classified as light activity by the accelerometer about one quarter of the time. This study, and others (16, 21), underscore that specific postural assessment through objective devices will be necessary if a seated or lying position is included in the definition of sedentary behavior. As these devices are developed and optimized, considerations should include: 1) validity and reliability in free-living conditions, 2) simultaneous, accurate measurement of all aspects of activity (e.g. breaks in sedentary behavior; light-, moderate-, and high-intensity physical activity), 3) low burden and high acceptability for participants, and 4) reasonable cost.
Priority 2.2
Standardize data collection and data reduction techniques for measuring sedentary behavior by accelerometry.
Rationale
Accelerometry is the most commonly used objective measure of sedentary behavior in larger studies. However, the variety of data reduction techniques used across studies (e.g. cutpoints, data collection protocols, required wear time, criteria used for defining nonwear time, statistical adjustment for other types of activity) could lead to different findings. For example, a variety of criteria have been used to classify nonwear time in accelerometry ranging from 10 to 180 minutes of consecutive 0 counts and with and without allowance for spurious activity (20). Oliver and colleagues have demonstrated in a sample of office workers that 180 minutes of consecutive 0 counts while wearing an accelerometer does occur (20), and, since time classified as nonwear time displaces time that would otherwise be classified as sedentary, the impact of this potential measurement error on relationships between sedentary behavior and health outcomes is an area in need of further research. It is also not clear how to best capture and code the duration of different “bouts” of sedentary behavior (as distinct from total sedentary behavior). Thus, a final research priority for sedentary behavior measurement is to evaluate and develop standard practices with this commonly used assessment methodology.
Recommendation 3
Expand the literature to include more longitudinal studies with objective measures of sedentary behavior as part of the human movement spectrum.
Rationale
At this time, quite a few cross-sectional and longitudinal studies have evaluated relationships between sedentary behavior and risk of hard, clinical outcomes, resulting in several systematic reviews and meta-analyses (2, 28, 33), as well as aging outcomes, such as physical function (26) and successful aging (6). These studies reveal fairly consistent, direct associations between more sedentary behavior and higher risk of cardiovascular disease, type 2 diabetes, adverse aging outcomes, and mortality. These studies find that time spent in sedentary behavior is a risk factor for these outcomes, independent of time spent performing MVPA. Putting aside cross-sectional studies that could be vulnerable to reverse causality and studies of clinical risk factors rather than hard outcomes, the greatest limitation to the available longitudinal evidence is that almost all studies use self-reported sedentary behavior, often television viewing time or time spent sitting, rather than objective measures. As mentioned earlier, objective assessment is less dependent on perception or recall and is able to evaluate total, relative, and patterns of total sedentary behavior.
We are aware of only one longitudinal study with objective assessment of sedentary behavior and future risk of hard, clinical outcomes in a non-patient population. Again in NHANES 2003–2004, Koster and colleagues (15) demonstrate that adults over 50 years old in the higher quartiles of absolute or percent of time spent in sedentary behavior have higher all-cause mortality after adjustment for MVPA over 2.8 years average follow-up. While the consistency of this finding with the self-report literature is reassuring, this study has limited follow-up. As a result, reverse causality, where underlying disease could cause increased sedentary behavior, could be contributing to these findings.
In response to this gap, expanding the available evidence in longitudinal studies using objective measurement of sedentary behavior was recognized as the top research priority. Such studies will be crucial for understanding whether total duration of sedentary behavior and/or patterns of sedentary behavior, including duration of single episodes or breaks in sedentary behavior, are important for health risk. As discussed further in the ‘Novel Strategies for Sedentary Behavior Research’ manuscript from this series (24), researchers with access to large, longitudinal databases with accelerometry or other objective measures should investigate and publish these relationships. It is worth stating that null studies will be just as important as positive findings for clarifying the role of sedentary behavior in future health risk. Specific recommendations to strengthen and broaden the research base are outlined below.
Priority 3.1
Improve the strength of the observational evidence by clarifying dose-response relationships and studying whether changes in repeated, objectively-measured sedentary behavior are associated with changes in risk factors or risk of developing hard health outcomes (e.g. disease incidence, mortality).
Rationale
Similar to the situation with MVPA, observational research of sedentary behavior is also challenged by the clustering of unhealthy behaviors in free-living individuals. For example, there is good evidence that television viewing is associated with worse dietary intake (5, 7, 18). Dietary intake may be poorly measured or not measured in studies and, even with covariate adjustment, could lead to inflated or even spurious associations. Evidence that changes in repeated measures of objective sedentary behavior are linked to health outcomes could improve causal inference with respect to residual confounding, though it is also possible that changes in other unhealthy behaviors could be related to changes sedentary behavior. We are aware of only a single study with sequential measurement of objective sedentary behavior in adults. In this study which used heart rate monitors, Ekelund and colleagues (8) found that several obesity indices predicted sedentary behavior a median of 5.6 years later, but that sedentary behavior did not predict future obesity. These findings place obesity before sedentary behavior in the causal pathway, rather than sedentary behavior causing obesity, which could be important for designing interventions and public health programming. The existence of only one study with repeated, objective measures of sedentary behavior in adults demonstrates how little is known about the temporal relationships among sedentary behavior, obesity, and health outcomes.
Therefore, while there certainly appears to be a signal thus far indicating that sedentary behavior is associated with the risk of type 2 diabetes, cardiovascular disease, aging outcomes, and mortality, we must proceed with caution. For this reason, expanding the available evidence from longitudinal studies with objectively-measured sedentary behavior and health outcomes was determined to be the top priority in epidemiological research.
Priority 3.2
Evaluate relationships between sedentary behavior and health risks in more diverse populations.
Rationale
Most of the evidence linking sedentary behavior to health outcomes exists in white or predominately white cohorts. However, the few studies that specifically evaluate non-white populations suggest that extrapolating research from predominantly white populations to nonwhite populations may be premature. A single analysis in the Black Women’s Health Study found that television time was related to increased risk of type 2 diabetes (17), but other cross-sectional studies have shown associations between sedentary behavior with cardiovascular risk factors in white but not black adults in NHANES(12) and with left ventricular mass in the Coronary Artery and Risk Development (CARDIA) Study (10). Evaluating sedentary behavior and health outcomes in other racial/ethnic groups, and potential reasons for different associations (e.g. measurement related, physiological, or cultural), is another area for further research.
Conclusions
In summary, further research is required to understand the impact of sedentary behavior on long-term health. There is not yet consensus on a definition for sedentary behavior, specifically whether or not posture must be included in the definition, and this should be a goal of the research community. Assessment methods – whether subjective or objective – should be developed, standardized, validated, and compared in free-living conditions. Objective measures will be important for decreasing measurement error and providing rich data on patterns of activity, but subjective measures will likely remain important because they are more cost-effective and provide information on domain-specific sedentary behavior. While this fundamental work goes on in the background, this workshop identified expanding the evidence base of longitudinal studies with objective assessment of sedentary behavior as the top epidemiological research priority that is achievable in the short-term. Where possible, this research should also compare sedentary behavior as defined by various criteria and measured by self-report, include repeated measures of sedentary behavior, evaluate dose-response relationships, and study more diverse populations. Along with these priorities in observational research, randomized trials evaluating 1) interventions to reduce sedentary behavior and 2) the effect of reducing sedentary behavior on surrogate endpoints (e.g. adiposity, clinical risk factors, subclinical cardiovascular disease) will offer further insight. These research priorities are not sequential, but simultaneous, and discoveries in one area will inform and focus the others to hopefully bring clarity to the role of sedentary behavior in public health.
Acknowledgments
The workshop was sponsored by the National Heart, Lung and Blood Institute, the National Institute on Aging and the Office of Disease Prevention of the National Institute of Health. The views expressed in this document reflect the collective ideas and opinions of the authors and do not necessarily represent the official views of the National Institutes of Health, or the U.S. Department of Health and Human Services, the other workshop participants, or the American College of Sports Medicine (ACSM). We would like to thank Drs. William Kohl, Dave Bassett, and Genevieve Healy for their contributions to the discussion. Dr. I-Min Lee is supported in part by grant CA154647 from the National Institutes of Health.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Alkhajah TA, Reeves MM, Eakin EG, Winkler EA, Owen N, Healy GN. Sit-stand workstations: a pilot intervention to reduce office sitting time. Am J Prev Med. 2012;43(3):298–303. doi: 10.1016/j.amepre.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 2.Bauman A, Chau JY, Ding D, Bennie J. Too Much Sitting and Cardio-metabolic Risk: An Update on the Epidemiologic Evidence. Curr Cardiovasc Risk Rep. 2013;7:293–8. [Google Scholar]
- 3.Buckley JP, Mellor DD, Morris M, Joseph F. Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion. Occup Environ Med. 2014;71(2):109–11. doi: 10.1136/oemed-2013-101823. [DOI] [PubMed] [Google Scholar]
- 4.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 5.Cleland VJ, Schmidt MD, Dwyer T, Venn AJ. Television viewing and abdominal obesity in young adults: is the association mediated by food and beverage consumption during viewing time or reduced leisure-time physical activity? Am J Clin Nutr. 2008;87(5):1148–55. doi: 10.1093/ajcn/87.5.1148. [DOI] [PubMed] [Google Scholar]
- 6.Dogra S, Stathokostas L. Sedentary behavior and physical activity are independent predictors of successful aging in middle-aged and older adults. J Aging Res. 2012;2012:190654. doi: 10.1155/2012/190654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Circulation. 2010;121(3):384–91. doi: 10.1161/CIRCULATIONAHA.109.894824. [DOI] [PubMed] [Google Scholar]
- 8.Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ. Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr. 2008;88(3):612–7. doi: 10.1093/ajcn/88.3.612. [DOI] [PubMed] [Google Scholar]
- 9.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18(2):148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 10.Gibbs BB, Reis JP, Schelbert EB, et al. Sedentary Screen Time and Left Ventricular Structure and Function: the CARDIA Study. Med Sci Sports Exerc. 2014;46(2):276–283. doi: 10.1249/MSS.0b013e3182a4df33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults’ sedentary time in population-based studies. Am J Prev Med. 2011;41(2):216–27. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–7. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katzmarzyk PT. Standing and Mortality in a Prospective Cohort of Canadian Adults. Med Sci Sports Exerc. 2014;46(5):940–6. doi: 10.1249/MSS.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 14.Kerr J, Marshall SJ, Godbole S, et al. Using the SenseCam to improve classifications of sedentary behavior in free-living settings. Am J Prev Med. 2013;44(3):290–6. doi: 10.1016/j.amepre.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7(6):e37696. doi: 10.1371/journal.pone.0037696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43(8):1561–7. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 17.Krishnan S, Rosenberg L, Palmer JR. Physical activity and television watching in relation to risk of type 2 diabetes: the Black Women’s Health Study. Am J Epidemiol. 2009;169(4):428–34. doi: 10.1093/aje/kwn344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowry R, Wechsler H, Galuska DA, Fulton JE, Kann L. Television viewing and its associations with overweight, sedentary lifestyle, and insufficient consumption of fruits and vegetables among US high school students: differences by race, ethnicity, and gender. J Sch Health. 2002;72(10):413–21. doi: 10.1111/j.1746-1561.2002.tb03551.x. [DOI] [PubMed] [Google Scholar]
- 19.Norton K, Norton L, Sadgrove D. Position statement on physical activity and exercise intensity terminology. J Sci Med Sport. 2010;13(5):496–502. doi: 10.1016/j.jsams.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Oliver M, Badland HM, Schofield GM, Shepherd J. Identification of accelerometer nonwear time and sedentary behavior. Res Q Exerc Sport. 2011;82(4):779–83. doi: 10.1080/02701367.2011.10599814. [DOI] [PubMed] [Google Scholar]
- 21.Oliver M, Schofield GM, Badland HM, Shepherd J. Utility of accelerometer thresholds for classifying sitting in office workers. Prev Med. 2010;51(5):357–60. doi: 10.1016/j.ypmed.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 22.Pate RR, O’Neill JR, Lobelo F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008;36(4):173–8. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 23.Reiff C, Marlatt K, Dengel DR. Difference in caloric expenditure in sitting versus standing desks. J Phys Act Health. 2012;9(7):1009–11. doi: 10.1123/jpah.9.7.1009. [DOI] [PubMed] [Google Scholar]
- 24.Rosenberg DE, Lee I, Young DR, Prohaska TR, Owen N, Buchner DM. Novel Strategies for Sedentary Behavior Research. currently under review by MSSE. 2014 doi: 10.1249/MSS.0000000000000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sedentary Behaviour Research N. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–2. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 26.Seguin R, Lamonte M, Tinker L, et al. Sedentary Behavior and Physical Function Decline in Older Women: Findings from the Women’s Health Initiative. J Aging Res. 2012;2012:271589. doi: 10.1155/2012/271589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Speck RM, Schmitz KH. Energy expenditure comparison: a pilot study of standing instead of sitting at work for obesity prevention. Prev Med. 2011;52(3–4):283–4. doi: 10.1016/j.ypmed.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41(2):207–15. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 29.Thyfault JP, Du M, Kraus BE, Levine JA, Booth FW. Physiology of Sedentary Behavior and its relationship with health outcomes. currently under review by MSSE. 2014 doi: 10.1249/MSS.0000000000000518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tikkanen O, Haakana P, Pesola AJ, et al. Muscle activity and inactivity periods during normal daily life. PLoS One. 2013;8(1):e52228. doi: 10.1371/journal.pone.0052228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tudor-Locke C, Schuna JM, Jr, Frensham LJ, Proenca M. Changing the way we work: elevating energy expenditure with workstation alternatives. Int J Obes (Lond) 2014;38(6):755–65. doi: 10.1038/ijo.2013.223. [DOI] [PubMed] [Google Scholar]
- 32.Viir R, Veraksits A. Discussion of “letter to the editor: standardized use of the terms sedentary and sedentary behaviours” – sitting and reclining are different states. Appl Physiol Nutr Metab. 2012;37(6):1256. doi: 10.1139/h2012-123. discussion 7. [DOI] [PubMed] [Google Scholar]
- 33.Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]


