Abstract
2,5-Hexanedione (HD) and acrylamide (ACR) are considered to be prototypical among chemical toxicants that cause central-peripheral axonopathies characterized by distal axon swelling and degeneration. Because the demise of distal regions was assumed to be causally related to the onset of neurotoxicity, substantial effort was devoted to deciphering the respective mechanisms. Continued research, however, revealed that expression of the presumed hallmark morphological features was dependent upon the daily rate of toxicant exposure. Indeed, many studies reported that the corresponding axonopathic changes were late developing effects that occurred independent of behavioral and/or functional neurotoxicity. This suggested that the toxic axonopathy classification might be based on epiphenomena related to dose-rate. Therefore, the goal of this mini-review is to discuss how quantitative morphometric analyses and the establishment of dose-dependent relationships helped distinguish primary, mechanistically relevant toxicant effects from non-specific consequences. Perhaps more importantly, we will discuss how knowledge of neurotoxicant chemical nature can guide molecular-level research toward a better, more rational understanding of mechanism. Our discussion will focus on HD, the neurotoxic γ-diketone metabolite of the industrial solvents n-hexane and methyl-n-butyl ketone. Early investigations suggested that HD caused giant neurofilamentous axonal swellings and eventual degeneration in CNS and PNS. However, as our review will point out, this interpretation underwent several iterations as the understanding of γ-diketone chemistry improved and more quantitative experimental approaches were implemented. The chemical concepts and design strategies discussed in this mini-review are broadly applicable to the mechanistic studies of other chemicals (e.g., n-propyl bromine, methyl methacrylate) that cause toxic neuropathies.
Keywords: central-peripheral distal axonopathy; peripheral neuropathy; 2,5-hexanedione; neurotoxicity; γ-diketone; acrylamide; dying back neuropathy
Introduction
Subchronic exposure to a variety of chemical pollutants in the atmosphere, diet, drinking water and occupational setting (Table 1) can result in nerve damage that has been traditionally classified as a central-peripheral distal axonopathy [1, 2]. Based on early morphological studies, the primary neuropathological manifestation of this neuropathy appeared to be retrograde myelinated axon degeneration in the peripheral (PNS) and central (CNS) nervous systems. Although a causal relationship has not been established, this “dying back” degeneration presumably mediated the characteristic toxicant-induced neurological deficits in humans and experimental animals; e.g., uncoordinated gait, skeletal muscle weakness and foot drop. Axon degeneration was often preceded by multifocal paranodal giant axonal swellings and, depending upon the toxicant, these swellings contained accumulations of cytoskeletal components (e.g., neurofilaments), fragments of the smooth endoplasmic reticulum and degenerating mitochondria [1]. Among the compounds listed in Table 1, acrylamide (ACR) and 2,5-hexanedione (HD) are considered to be prototypical toxicants that produce distal axonopathy. ACR is a water-soluble α,β-unsaturated carbonyl derivative of the type-2 alkene chemical class and has extensive manufacturing applications; e.g., paper, textile and fabric industries [2]. HD is the common neurotoxic γ-diketone metabolite of n-hexane and methyl-n-butyl ketone. Both parent compounds are used in fabric manufacturing and have been associated with several human outbreaks of neuropathy following subchronic occupational exposure [1].
Table 1.
| Chemical | Softness (σ, ×10−3eV−1) | Electrophilicity (ω, eV) |
|---|---|---|
| Carbon disulfide | 359 | 3.97 |
| Methyl acrylate | 315 | 3.22 |
| Acrylamide | 315 | 2.62 |
| 2,5-Hexanedione | 310 | 2.09 |
| n-Propyl bromide | 270 | 1.93 |
| Vinyl chloride | 277 | 1.71 |
For each compound, respective orbital energies (ELUMO, EHOMO) were obtained from ground state equilibrium geometries with DF B3LYP-6-31G* in vacuum from 6-31G* initial geometries and were used to calculate softness (σ) and the electrophilic index (ω) as described in LoPachin et al. [35].
Early studies of HD and ACR neurotoxicity were based on the premise that distal axon regions were sites of toxicant action and that axonopathy was the pathognomonic outcome of a specific mechanism; e.g., inhibition of axolemmal Na pumps [3, 4]. Because axonal swellings and degeneration were assumed to be causally related to the onset of neurotoxicity, substantial effort was devoted to deciphering the respective mechanisms [5, 6]. However, ensuing research indicated that the expression of these traditional hallmark features was dependent upon the rate of toxicant exposure. For example, ACR caused axon degeneration at low subchronic exposure rates (10–20 mg/kg/d), whereas higher daily dose-rates (50 mg/kg/d) produced neurotoxicity in the absence of degeneration [7, 8]. This observation lead to quantitative morphometric analyses which showed that nerve terminals in the PNS and CNS were primary sites of ACR action [2, 6]. However, the molecular mechanism of presynaptic toxicity remained elusive until ACR, a α,β-unsaturated carbonyl compound, was recognized to be a soft (polarizable) electrophile (electron deficient species). Moreover, the principles of Hard and Soft, Acids and Bases theory (see ahead) suggested that ACR would preferentially form adducts with soft nucleophiles (polarizable, electron rich species), which in biological systems are anionic sulfhydryl thiolate (RS−) groups on protein cysteine residues. Indeed, subsequent neurochemical, enzymatic and proteomic studies provided corroborative evidence that ACR caused presynaptic toxicity by inhibiting the function of key nerve terminal proteins (e.g., N-ethylmaleimide sensitive factor) through targeting of regulatory cysteine thiolate sites [2, 6].
Defining molecular mechanisms is a critical step toward reducing the black box nature of toxic neuropathies. However, as the preceding synopsis of ACR research illustrates, this level of understanding requires identifying primary neurotoxicologically relevant effects and, in particular, a detailed knowledge of the corresponding toxicant chemistry. Therefore, the goal of this review is to discuss how a similar approach involving determination of dose-rate specificity, quantitative morphometric analyses and application of chemical principles was used to clarify the neuropathological character and molecular mechanism of γ-diketone neuropathy. As will be evident, ACR and HD are significantly different chemicals with correspondingly different mechanisms of action. This highlights the fact that the chemical concepts and design strategies discussed in this review can be applied to studies of the diverse chemicals that cause toxic neuropathies (Table 1).
γ-Diketone Neuropathy – Morphometric Analyses
Giant multifocal swellings of large myelinated axons in the CNS and PNS have been historically considered the hallmark feature of γ-diketone neuropathy [1]. Accordingly, research conducted over the past 35 years has been directed toward discerning the molecular mechanism of these swellings. Since the swellings contained neurofilament (NF) masses, it was proposed that they resulted from direct HD modification of NF proteins. Covalent NF-NF crosslinks were thought to be formed by autooxidation of the pyrrole rings that result from reaction of ε-amino groups on NF lysine residues with γ-diketones like HD [9]. Theoretically, nascent NF subunits would undergo chemical modification as they progressed along the axon and eventually the resulting cross-linked NFs would accumulate at narrow distal nodes of Ranvier where their anterograde transport is impeded. The subsequent neurofilamentous swellings would initiate axon degeneration and characteristic neurological deficits [4, 10]. Other studies however identified axon atrophy as a significant feature of γ-diketone neuropathy [e.g., see 11, 12]. To resolve this apparent conflict, we conducted a series of quantitative morphometric studies to characterize the spatiotemporal expression of axonal swelling, atrophy and degeneration in conventionally fixed central [13, 14] and peripheral [15, 16] nerves of HD-intoxicated rats. Results showed that swollen axons were an exclusive but infrequent product of long-term (307–98 days) HD intoxication at lower daily dose-rates (100–175 mg/kg/d; respectively; Fig. 1). Higher dose-rates (400 mg/kg/d) produced neurological deficits (e.g., gait abnormalities, reduced hindlimb grip strength) in the absence of neurofilamentous swellings (Fig. 1). These data suggested that swellings were neither necessary nor sufficient for the expression of γ-diketone neurotoxicity. In contrast, quantitative spatiotemporal analyses demonstrated that axonal atrophy was the predominant lesion and that this effect occurred during the early stages of HD intoxication and over a wide range of daily dose-rates (100–400 mg/kg/d). Distal axon atrophy in the PNS preceded the development of neurobehavioral deficits and was temporally correlated with electrophysiological changes (e.g., reduced nerve conduction velocity, increased latency) in tibial, sural and caudal nerve [16]. The composite evidence therefore suggested that neurofilamentous swellings were exclusively related to subchronic HD exposures at lower dose-rates. Furthermore, the swellings were relatively infrequent and their appearance did not correspond to the onset and development of neurotoxicity. These expression characteristics indicated that swellings were an epiphenomenon and that the classification of γ-diketone neuropathy as a “giant neurofilamentous axonopathy” or “distal axonopathy” required revision. In contrast, axon atrophy was the primary neuropathological feature of γ-diketone neuropathy. It occurred irrespective of dose-rate and was not a secondary consequence of neurofilamentous swelling. The temporal development of distal axon atrophy in PNS of HD-intoxicated animals has significant electrophysiological implications and could be causally related to the neurological defects associated with HD intoxication. Although the molecular mechanism of axon atrophy in γ-diketone neuropathy is unknown, in the following section we discuss current areas of research regarding the possible impairment of axonal processes that determine axon caliber.
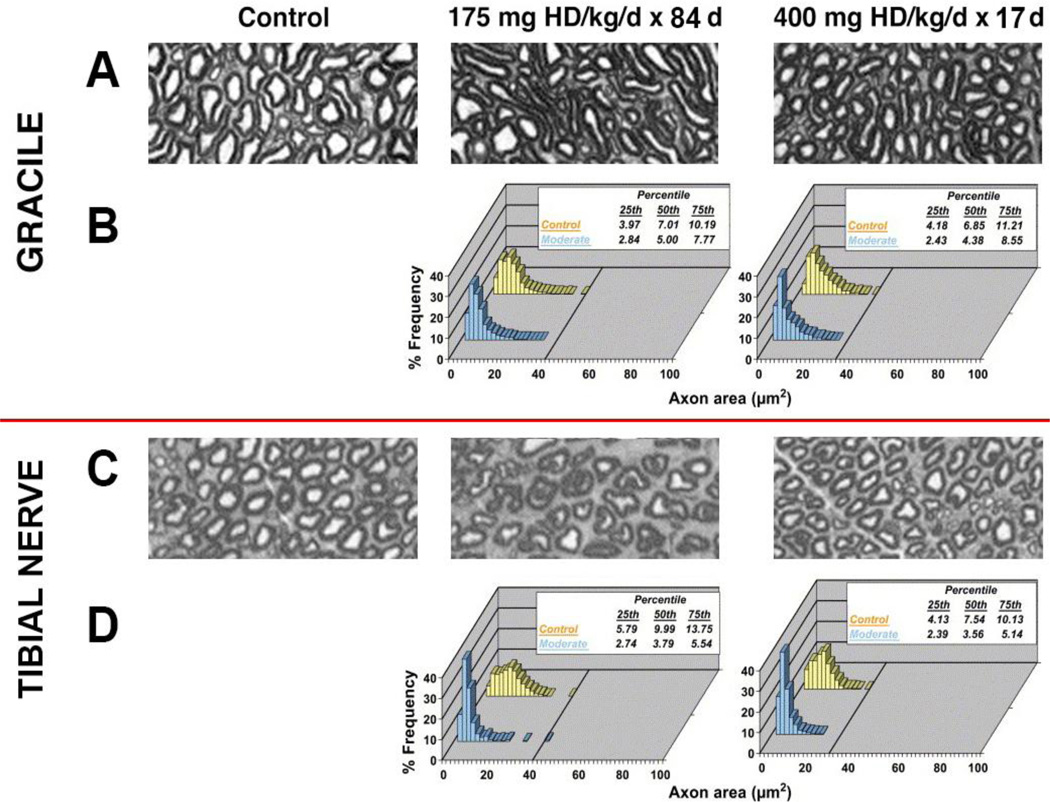
Figure 1.
Cross-sectional areas from (A) spinal cord gracile regions and (C) distal tibial nerve from age-matched controls and moderately affected rats intoxicated at either 175 mg/kg/d × 84 days or 400 mg/kg/d × 17 days. Also presented are corresponding percentage frequency distributions of cross-sectional areas (µM2) for (B) gracile regions and (D) distal tibial nerve from control and HD-intoxicated rats. For each frequency distribution, corresponding percentile data (µM2) are presented and the horizontal lines represent the upper limit (100th percentile) for the control distributions. Results indicate that, regardless of HD dose-rate, the respective frequency graphs are shifted to the left relative to control distributions. This shift toward smaller diameters is reflected by significant decreases in the corresponding 25th, 50th and 75th percentiles (insert). These data indicate that regardless of dose-rate, axon atrophy developed in gracile and tibial nerve regions was an early consequence of HD intoxication. In both regions, however, giant neurofilamentous swellings were prevalent only in severely intoxicated animals; i.e., 175 mg/kg/d × 98 days and 400 mg/kg/d × 21 days [4, 13, 16].
γ-Diketone Neuropathy – Mechanism of Axon Atrophy
NF content and corresponding spacing (interfilament distances) are important determinants of axon caliber and are, therefore, likely parameters for HD disruption [4, 10]. However, ultrastructural morphometric analyses of CNS myelinated axons (rubrospinal tract) in HD-intoxicated rats failed to find changes in NF-NF or NF-microtubule distances [14]. In contrast, significant decreases in the soluble NF contents of PNS and CNS tissues have been reported in HD-exposed laboratory animals [17–19]. NF depletion appeared to be a specific independent effect, since it was not related to reductions in gene expression [20] or protein synthesis [21], nor was it secondary to the conversion of NF monomers into cross-linked derivatives [17, 19, 22]. Nonetheless, the relationship of NF loss to reductions in axon caliber was not evident. In this regard, we considered the possibility that HD adduction of NF subunits impaired maintenance of the axonal cytoskeleton [22]. According to the subunit-transport hypothesis, the stationary neurofilamentous polymer is maintained by dynamic turnover involving the interaction of a mobile population of NF subunit proteins composed of newly synthesized triplet proteins that replace aged effete NF proteins. The anterograde movement of these NFs is mediated by the fast transport motor protein, kinesin [23]. HD can form selective N-substituted 2,5-dimethylpyrrole adducts with lysine residues of KSP (lys-ser-pro) repeat motifs that are localized to the carboxy-terminal tail regions of medium (NFM) and heavy NF (NFH) protein subunits [24, 25]. These tail regions are thought to mediate insertion of newly synthesized NF proteins into the stationary cytoskeleton [26] and, therefore, the physicochemical consequences of adduct formation at corresponding KSP motifs could jeopardize these turnover-related interactions.
To examine this possibility, we [22] used Triton X-100 extraction of spinal cord followed by differential fractionation to separate different cytoskeletal components. Thus, the low-speed pellet (15,000 × g; P1) of spinal homogenates represented the Triton-insoluble stationary cytoskeleton. Centrifugation (100,000 × g) of the corresponding supernatant (S1) yielded a high-speed pellet (P2), presumably composed of transition NF proteins, and corresponding supernatant (S2) that contained the mobile population of exchangeable subunit monomers. Results demonstrated the selective, near-total depletion of NF subunits in the P2 and S2 fractions. This finding suggested that HD-adducted mobile NF monomers failed to interact with the stationary cytoskeletal polymer and that the lack of interaction resulted in NF loss via accelerated kinesin-mediated anterograde transport and distal proteolytic breakdown. Although the phosphorylation status of NFM and NFH proteins has been considered a determinant of cytoskeletal polymer association, our studies suggested that HD adduct formation did not alter subunit phosphorylation [17, 19, 22]. That interference of the subunit-polymer interaction was mediated by pyrrole formation alone was suggested by the lack of higher molecular weight (HMW) NF proteins in the P2 and S2 fractions. Derivitized NFs were relegated to P1 fractions (stationary cytoskeleton) and were considered to be unavailable for exchange with mobile NFs.
It has been argued that HMW NF species are a consequence of HD reactions with corresponding lysine residues and the subsequent formation of pyrrole-pyrrole cross-links [9]. However, the origin and toxicological significance of these HMW NF derivatives has been recently challenged. Thus, in a co-sedimentation study of rat spinal cord, we [27] showed that detergent insoluble HMW NF derivatives were normal constituents of the axonal cytoskeleton and that HD intoxication elevated these complexes [Fig. 2]. HMW NF complexes can be catalyzed by transglutaminase enzymes, which are calcium-activated zymogens that form covalent ε-(γ-glutamyl)lysine bonds between proteins and thereby instill supramolecular structures (e.g., cytoskeletons) with extra rigidity and resistance to proteolytic degradation [28]. Therefore, the lower HMW NFs observed in control spinal cord preparations [Fig. 2] might represent baseline levels of cytoskeletal proteins that have been cross-linked by the normal activities of axonal transglutaminases. In contrast, the elevated presence of HMW NF complexes in spinal cord samples from HD-intoxicated rats might represent excess fragmentation of stationary cytoskeleton [11] possibly as a result of impaired polymer maintenance.
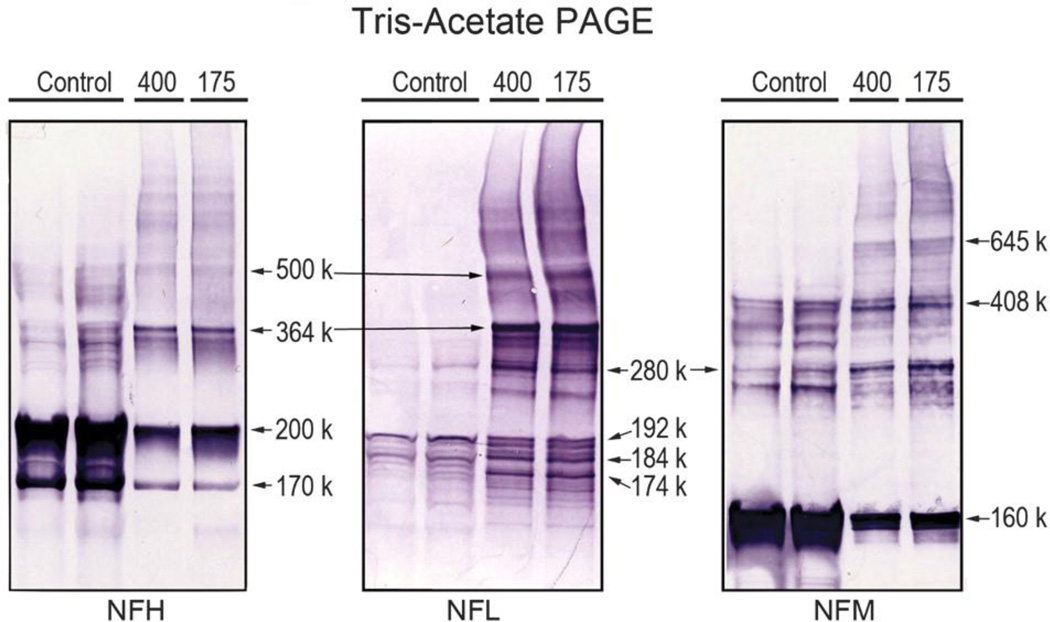
Figure 2.
Representative immunoblots are presented for NF proteins (NFH, NFL and NFM) in co-sedimentation preparations of spinal cord form control and HD-intoxicated (400 and 175 mg/kg/d) rats (Zhang et al. [27]). Separation of proteins in denaturing conditions (tris-acetate/SDS-PAGE) revealed detergent-insoluble HMW bands for all NF subunit proteins in both control and HD samples. These HMW species were present but not prevalent in control as evidenced by the fact that they were detected only when control protein concentrations were higher (25 µg) than the concentrations used for HD samples (5 µg). Furthermore, cross-comparisons among NF proteins from control samples relevaled sevral HMW NFL bands (e.g., 280 kDa, 364 kDa) that were common to both NFH and NFM (see connecting arrows).
As will be discussed, HD is an electrophile that reacts with nucleophilic primary nitrogen groups on lysine residues. Accordingly, substantial data suggested that these residues on NF subunits are neurotoxicologically relevant targets for HD [4, 10]. However, other research has demonstrated the expression of HD neurotoxicity in animal species (crayfish) and transgenic mouse models that lack NF subunits. This suggested that triplet proteins were not an essential HD target [29]. Indeed, specific lysine residues on non-NF proteins are critically involved in the maintenance and operation of the cytoskeleton. Thus, for example, the processivity of the monomeric kinesin motor, KIF1A, is dependent upon interactions of corresponding lysine-rich K-loops with glutamate residues on cognate binding domains of tubulin [30]. This interaction is based on the fact that, at physiological pH, the primary ε-amino group of lysine exists predominately in the protonated (+1; pKa = 10.5) state. This positively charged basic residue can associate electrostatically with negatively charged acidic amino acids (e.g., glutamate) and/or phosphate moieties in the binding domains of cognate proteins. HD adduction of K-loop lysine residues on KIF1A can therefore interfere with corresponding tubulin interactions. Lysine residues on certain cytoskeletal proteins are also sites for posttranslational modification (e.g., lys40 of α-tubulin) that influence polymer stability and motor protein trafficking [31]. Clearly lysine residues on NF and non-NF proteins are critically involved in axonal cytoskeletal form and function and therefore this polymer represents a target-rich environment for HD. To identify potential non-NF cytoskeletal targets in spinal cord of HD intoxicated rats, we [27] characterized protein-protein interactions in taxol-stabilized microtubule-motor protein preparations and in NF-cytoskeletal protein cosedimentation assays. Although the protein associations for a variety of cytoskeletal constituents were determined (e.g., α-tubulin, KIF1A, dynein), our results indicated selective reductions (45%–80%) in MAP1A, MAP1B heavy chain, MAP2 and tau. This suggested that HD intoxication impaired MAP-microtubule binding, presumably through adduction of lysine residues that mediate such interactions. Although the exact molecular consequences of the observed MAP binding defect have not been determined, loss of axon caliber is a possible outcome. Specifically, MAP proteins stabilize axonal/dendritic microtubules and regulate cytoskeletal interfilament distances [32]. Consistent with defective MAP-based interfilament spacing, our ultrastructural morphometric analyses of rubrospinal axons [14] indicated that axon atrophy was associated with an increase in microtubule density. Similar to γ-diketone neuropathy, map2−/− and map1b−/− knockout mice exhibit axonal atrophy, microtubule condensation and gait abnormalities [33]. Growing evidence now indicates that the axon atrophy associated with HD neurotoxicity involves targeting of multiple cytoskeletal proteins; e.g., MAPs, NF triplet proteins, gelsolin and α-internexin [34].
γ-Diketone Neuropathy – Target Specificity and Tissue Vulnerability
The proposed mechanism of axon atrophy in γ-diketone neuropathy is based on the selective reaction of HD with lysine residues of proteins. The mechanistic focus on this amino acid is reasonable given the aforementioned cytophysiological roles of lysine in critical protein-protein interactions and the probable molecular consequences of adduct formation with HD. Perhaps more compelling, the chemical character of HD indicates that lysine residues are primary targets. Specifically, HD is an electrophile and can form irreversible covalent bonds with nucleophilic amino acids which, in biological systems, are primarily cysteine, lysine and histidine residues. Electrophiles do not, however, react indiscriminately with nucleophiles. Instead, electrophile-nucleophile interactions exhibit a significant degree of specificity in accordance with the Hard and Soft, Acids and Bases (HSAB) theory of Pearson (35). Electrophilic and nucleophilic molecules are classified as being either soft (polarizable) or hard (non-polarizable) and based on the HSAB principle, electrophiles react selectively with biological targets of comparable softness or hardness (2, 35). Based on HSAB parameters, calculated using quantum mechanical methods, HD is a relatively hard (low σ value; Table 1) but weak electrophile (low ω value) that will preferentially react with hard nucleophiles. Accordingly, cysteine is an unfavorable candidate for HD adduction since the corresponding sulfhydryl thiol group is a soft nucleophile and the adduct product, a hemithioacetal, is reversible. In contrast, the nitrogen groups on lysine (ε-amino group) and histidine (imidazole ring) residues are harder nucleophiles and consequently more favorable targets for a hard electrophile such as HD. Consistent with HSAB predictions, in chemico studies [36] showed that incubation of bovine serum albumin (BSA) with graded HD concentrations caused a concentration- and pH-dependent loss of BSA lysine residues due to adduct formation. HD exposure also reduced BSA histidine content at higher diketone concentrations, which suggested that lysine was the preferential hard nucleophile target. It is now recognized that HD, as a hard diketone electrophile, reacts with hard nucleophilic ε-amine groups on lysine residues to form 2,5-dimethylpyrrole adducts on NF subunits and other proteins (reviewed in 4,10). It is also recognized that pyrrole formation is a necessary step in the production of the γ-diketone neuropathy mediated by lysine adduct formation [37– 39]. However, the levels of protein adducts formed during HD exposure are very low and encompass both neuronal and non-neuronal proteins [18]. Whereas this might indicate a lack of neurotoxicological relevance and target specificity, there is evidence that certain lysine residues are more susceptible to HD adduction; e.g., lysine residues within KSP repeats on tail regions of NFM and NFH subunits [24, 25]. Because HD is a weak electrophile, the nucleophilicity of the reacting lysine will determine the rate of the corresponding second order adduct reaction [24]. In this regard, the previously noted target selectively is likely based on specialized pKa-lowering microenvironments known as catalytic triads or diads were lysine can exist in the more nucleophilic and therefore more reactive deprotonated state (0) [40].
The toxicological effects of HD are restricted to the nervous system and testis; e.g., testicular atrophy, Sertoli cell damage [41]. The basis for the relative vulnerability of these tissues is unknown, but could be related to the slow turnover of resident proteins [9, 42]. Thus, HD is a weak electrophile that slowly forms adducts with reactive lysine residues in catalytic microenvironments. Because axonal protein turnover is slow, HD adducts accumulate slowly to a toxic threshold concentration that causes cumulative γ-diketone neurotoxicity. Similar toxicodynamics appear to underlie the selective nerve terminal toxicity of acrylamide, which is also a weak electrophile [2]. This might also be the mechanism of Sertoli cell toxicity due to HD exposure.
Summary
Initial morphological studies of γ-diketone neuropathy were inherently descriptive and focused on visually obvious giant neurofilamentous swellings. Subsequent research was based on the assumption that lysine residues on NF proteins were primary targets and that pyrrole-pyrrole subunit cross-linking was a necessary mechanistic step in HD axonopathy. Multifocal axonal swellings in the CNS and PNS were considered to be the pathognomonic neuropathological feature. However, these early studies lacked dose-rate dependent determinations that were linked to quantitative morphometric analyses. Research designed to decipher neurotoxicological relevance indicated that neurofilamentous swellings were an infrequent epiphenomenon that were unrelated to the production of neurotoxicity. Furthermore, although HMW NF species have been considered to be the HD cross-linked subunits that cause axonal swelling, conclusively identifying their origin and toxicological significance is complicated since as least some of these derivatives represent normal components of the cytoskeleton. In contrast, axonal atrophy was a prevalent effect that occurred regardless of HD dose-rate and was the likely causative factor underlying peripheral nerve dysfunction. Molecular, in chemico and proteomic studies suggested that the mechanism of atrophy involved HD adduction of lysine residues on multiple cytoskeletal proteins (e.g., MAPs, tau and NF subunits). That γ-diketone neuropathy might involve adduct formation with multiple targets is not unique, since it is now recognized that electrophilic toxicants such as ACR and acrolein cause cytotoxicity by reacting with an electrophile-responsive proteome [2]. The resulting changes in physicochemical properties of adducted individual proteins (e.g., solubility, electrostatic potential, tertiary structure) disrupt critical protein-protein interactions involved in cytoskeletal maintenance and function, which lead to subsequent dissolution of the polymer and loss of axon caliber. Calculated HSAB parameters indicated that HD was a relatively hard γ-diketone of low electrophilicity that could be predicted to react preferentially with harder amino acid nucleophiles such as lysine. Proteomic research showed that HD readily formed adducts with specific lysine residues on NF subunits and other proteins. This likely reflects the presence of these residues in pKa-lowering microenvironments where a larger proportion of lysine residues exist in the more nucleophilic deprotonated (0) state. A similar quantitative experimental design guided by an understanding of chemical properties can be used to discern the neurotoxicological mechanisms of other chemicals that cause toxic neuropathies. In this regard, the neurotoxicants listed in Table 1 are electrophiles of varying softness (σ) and electrophilic reactivity (ω). This, and other information related to the respective chemical reactions (e.g., Michael condensation, SN2 substitution, Schiff base formation), can provide a rational platform for the design of subsequent experiments to identify molecular targets, sites of action and mechanisms of inhibition. Studies that address the neurotoxicological significance of a parameter; i.e., primary mechanistic event vs. secondary epiphenomenon, avoid the limitations of a ‘black-box” approach where interpretation of an experimental outcome is compromised by a lack of quantitative information.
Highlights.
We reviewed the neurotoxicity and toxicodynamics of γ-diketone neuropathy.
Axonal swellings and degeneration are epiphenomena related to dose-rate.
Axonal atrophy was shown to be the primary HD-induced neuropathological feature.
HD causes atrophy by forming adducts with lysine residues on cytoskeletal proteins.
This mechanism is based on γ-diketone chemistry and using a quantitative approach.
Acknowledgements
This research was supported by grants RO1 ES03830-26 and RO1 ES07912-11 from the National Institutes of Environmental Health Sciences, National Institutes of Health.
Abbreviations
- CNS
central nervous system
- PNS
peripheral nervous system
- HD
2,5-hexanedione
- ACR
acrylamide
- NF
neurofilament
- NFM
medium molecular weight neurofilament
- NFH
heavy molecular weight neurofilament
- KSP
lysine-serine-proline motif
- P1
low-speed pellet
- P2
high speed pellet
- S1
low-speed supernatant
- S2
high-speed supernatant
- MAP
microtubule associated proteins
- HSAB
Hard and Soft, Acids and Bases
- BSA
bovine serum albumin
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Spencer PS, Schaumburg HH. Classification of neurotoxic disease: a morphological approach. In: Spencer PS, Schaumburg HH, editors. Experimental and Clinical Neurotoxicology. Baltimore, MD: Williams & Wilkins; 1980. pp. 92–99. [Google Scholar]
- 2.LoPachin RM, Gavin T. Molecular mechanism of acrylamide neurotoxicity: lessons learned from organic chemistry. Environ. Health Persp. 2012;120:1650–1657. doi: 10.1289/ehp.1205432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LoPachin RM, Lehning EJ. Acrylamide-induced distal axon degeneration: A proposed mechanism of action. NeuroToxicology. 1994;15:247–260. [PubMed] [Google Scholar]
- 4.LoPachin RM, DeCaprio AP. γ-Diketone neuropathy: axon atrophy and the role of cytoskeletal protein adduction. Toxicol. Appl. Pharmacol. 2004;199:20–34. doi: 10.1016/j.taap.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 5.LoPachin RM, Lehning EJ. The relevance of axonal swelling and atrophy to γ-diketone neurotoxicity. NeuroToxicology. 1997;18:7–22. [PubMed] [Google Scholar]
- 6.LoPachin RM, Balaban CD, Ross JF. Acrylamide axonopathy revisited. Toxicol. Appl. Pharmacol. 2003;188:135–153. doi: 10.1016/s0041-008x(02)00072-8. [DOI] [PubMed] [Google Scholar]
- 7.Crofton KM, Padilla S, Tilson HA, Anthony DC, Raymer JH, MacPhail RC. The impact of dose-rate on the neurotoxicity of acrylamide: The interaction of administered dose, target tissue concentration, tissue damage and functional effects. Toxicol. Appl. Pharmacol. 1996;139:163–176. doi: 10.1006/taap.1996.0155. [DOI] [PubMed] [Google Scholar]
- 8.Lehning EJ, Persaud A, Dyer KS, Jortner BS, LoPachin RM. Biochemical and morphological characterization of acrylamide peripheral neuropathy. Toxicol. Appl. Pharmacol. 1998;151:211–221. doi: 10.1006/taap.1998.8464. [DOI] [PubMed] [Google Scholar]
- 9.Graham DG, Amarnath V, Valentine WM, Pyle SJ, Anthony DC. Pathogenic studies of hexane and carbon disulfide neurotoxicity. Crit. Rev. Toxicol. 1995;25:91–112. doi: 10.3109/10408449509021609. [DOI] [PubMed] [Google Scholar]
- 10.LoPachin RM, DeCaprio AP. Protein adduct formation as a molecular mechanism in neurotoxicity. Toxicol. Sci. 2005;86:214–225. doi: 10.1093/toxsci/kfi197. [DOI] [PubMed] [Google Scholar]
- 11.Monaco S, Simonati A, Rizzuto N, Autilio-Gambetti L, Gambetti P. Hexacarbon axonopathy: the morphological expression of altered cytoskeletal translocation. In: Nappi G, et al., editors. Neurodegenerative Disorders: The Role Played by Endotoxin and Xenobiotics. New York: Raven Press; 1988. [Google Scholar]
- 12.LoPachin RM, Lehning EJ, Stack EC, Hussein SJ, Saubermann AJ. 2,5-Hexanedione alters elemental composition and water content of rat peripheral nerve myelinated axons. J. Neurochem. 1994;63:2266–2278. doi: 10.1046/j.1471-4159.1994.63062266.x. [DOI] [PubMed] [Google Scholar]
- 13.LoPachin RM, Jortner BS, Reid M, Das S. γ-Diketone central neuropathy: quantitative morphometric analysis of axons in rat spinal cord white matter regions and nerve roots. Toxicol. Appl. Pharmacol. 2003;193:29–46. doi: 10.1016/j.taap.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 14.LoPachin RM, Jortner BS, Reid M, Monir A. γ-Diketone central neuropathy: quantitative analyses of cytoskeletal components in myelinated axons of rat rubrospinal tract. NeuroToxicology. 2005;26:1021–1030. doi: 10.1016/j.neuro.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Lehning EJ, Dyer KS, Jortner BS, LoPachin RM. Axon atrophy is a specific component of 2,5-hexanedione peripheral neuropathy. Toxicol. Appl. Pharmacol. 1995;135:58–66. doi: 10.1006/taap.1995.1208. [DOI] [PubMed] [Google Scholar]
- 16.Lehning EJ, Jortner BS, Fox JH, Arezzo JC, Kitano T, LoPachin RM. γ-Diketone peripheral neuropathy 1. Quantitative morphometric analyses of axonal atrophy and swelling. Toxicol. Appl. Pharmacol. 2000;165:127–140. doi: 10.1006/taap.2000.8937. [DOI] [PubMed] [Google Scholar]
- 17.Chiu FC, Opanashuk LA, He DK, Lehning EJ, LoPachin RM. γ-Diketone peripheral neuropathy. II. Neurofilament subunit content. Toxicol. Appl. Pharmacol. 2000;165:141–147. doi: 10.1006/taap.2000.8938. [DOI] [PubMed] [Google Scholar]
- 18.DeCaprio AP, O’Neill EA. Alterations in rat axonal cytoskeletal proteins induced by in vitro and in vivo 2,5-hexanedione exposure. Toxicol. Appl. Pharmacol. 1985;78:235–247. doi: 10.1016/0041-008x(85)90287-x. [DOI] [PubMed] [Google Scholar]
- 19.LoPachin RM, He D, Reid ML. 2,5-Hexanedione-induced changes in the neurofilament subunit pools of rat peripheral nerve. NeuroToxicology. 2005;198:229–240. doi: 10.1016/j.neuro.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Opanashuk LA, He D, Lehning EJ, LoPachin RM. γ-Diketone peripheral neuropathy III. Neurofilament gene expression. NeuroToxicology. 2001;22:215–220. doi: 10.1016/s0161-813x(00)00011-5. [DOI] [PubMed] [Google Scholar]
- 21.Sickles DW. Toxic neurofilamentous axonopathies and fast anterograde axonal transport. I. The effects of single doses of acrylamide on the rate and capacity of transport. NeuroToxicology. 1989;10:91–102. [PubMed] [Google Scholar]
- 22.LoPachin RM, He D, Reid ML, Opanashuk LA. 2,5-Hexanedione-induced changes in the monomeric neurofilament protein content of rat spinal cord fractions. Toxicol. Appl. Pharmacol. 2004;198:61–73. doi: 10.1016/j.taap.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Yabe JT, Jung C, Chan WK, Shea TB. Phospho-dependent association of neurofilament proteins with kinesin in situ. Cell Motil. Cytoskeleton. 2000;45:249–262. doi: 10.1002/(SICI)1097-0169(200004)45:4<249::AID-CM1>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 24.DeCaprio AP, Fowke JH. Limited and selective adduction of carboxyl-terminal lysines in the high molecular weight neurofilament proteins by 2,5-hexanedione in vitro. Brain Res. 1992;586:219–228. doi: 10.1016/0006-8993(92)91630-w. [DOI] [PubMed] [Google Scholar]
- 25.DeCaprio AP, Kinney EA, Fowke JH. Regioselective binding of 2,5-hexanedione to high-molecular-weight rat neurofilament proteins in vitro. Toxicol. Appl. Pharmacol. 1997;145:211–217. doi: 10.1006/taap.1997.8181. [DOI] [PubMed] [Google Scholar]
- 26.Ackerley S, Thornhill P, Grierson AJ, Brownlees J, Anerton BH, Leigyh PN, Shaw CE, Miller CCJ. Neurofilament heavy chain side arm phosphorylation regulates axonal transport of neurofilaments. J. Cell Biol. 2003;161:489–495. doi: 10.1083/jcb.200303138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang L, Gavin T, DeCaprio AP, LoPachin RM. γ-Diketone axonopathy: analyses of cytoskeletal motors and highways in CNS myelinated axons. Toxicol. Sci. 2010;117:180–189. doi: 10.1093/toxsci/kfq176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lorand L, Graham RM. Transglutaminases: crosslinking enzymes with pleiotropic functions. Nat. Rev. Mol. Cell Biol. 2003;4:140–156. doi: 10.1038/nrm1014. [DOI] [PubMed] [Google Scholar]
- 29.Sickles DW, Pearson JK, Beall A, Testino A. Toxic axonal degeneration occurs independent of neurofilament accumulation. J. Neurosci. Res. 1994;39:347–354. doi: 10.1002/jnr.490390312. [DOI] [PubMed] [Google Scholar]
- 30.Okada Y, Hirokawa N. Mechanism of the single-headed processivity: diffusional anchoring between the K-loop of kinesin and the C terminus of tubulin. Proc. Natl. Acad. Sci. 2000;97:640–645. doi: 10.1073/pnas.97.2.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iwabata J, Yoshida M, Komatsu Y. Proteomic analysis of organ-specific post-translational lysine-acetylation and –methylation in mice by use of anti-acetyllysine and –methyllysine mouse monoclonal antibodies. Proteomics. 2005;5:4653–4664. doi: 10.1002/pmic.200500042. [DOI] [PubMed] [Google Scholar]
- 32.Hirokawa N. Microtubule organization and dynamics dependent on microtubule-associated proteins. Curr. Opin. Cell Biol. 1994;6:74–81. doi: 10.1016/0955-0674(94)90119-8. [DOI] [PubMed] [Google Scholar]
- 33.Edlemann W, Zervas M, Costello P, Roback L, Fischer I, Hammarback JA, Cowan N, Davies P, Wainer B, Kucherlapati R. Neuronal abnormalities in microtubule-associated protein 1B mutant mice. Proc. Natl. Acad. Sci. 1996;93:1270–1275. doi: 10.1073/pnas.93.3.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tshala-IKatumbay D, Monterroso V, Kayton R, Lasarev M, Sabri M, Spencer P. Probing mechanism of axonopathy. Part II: protein targets of 2,5-hexanedione, the neurotoxic metabolite of the aliphatic solvent n-hexane. Toxicol. Sci. 2009;107:482–489. doi: 10.1093/toxsci/kfn241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.LoPachin RM, Gavin T, DeCaprio A, Barber DS. Application of the Hard and Soft, Acids and Bases (HSAB) theory to toxicant-target interactions. Chem. Res. Toxicol. 2012;25:239–251. doi: 10.1021/tx2003257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DeCaprio AP, Jackowski SJ, Regan KA. Mechanism of Formation and quantitation of imines, pyrroles, and stable nonpyrrole adducts in 2,5-heanedione-treated protein. Molec. Pharmacol. 1987;32:542–548. [PubMed] [Google Scholar]
- 37.DeCaprio AP, Olajos EJ, Weber P. Covalent binding of a neurotoxic n-hexane metabolite: conversion of primary amines to substituted pyrrole adducts by 2,5-hexanedione. Toxicol. Appl. Pharmacol. 1982;65:440–450. doi: 10.1016/0041-008x(82)90389-1. [DOI] [PubMed] [Google Scholar]
- 38.DeCaprio AP, Briggs RG, Jackowski JJ, Kim JCS. Comparative neurotoxicity and pyrrole-forming potential of 2,5-hexanedione and perdeuterio-2,5-hexanedione in the rat. Toxicol. Appl. Pharmacol. 1988;92:75–85. doi: 10.1016/0041-008x(88)90229-3. [DOI] [PubMed] [Google Scholar]
- 39.Genter MB, Szakal-Quin G, Anderson CW, Anthony DC, Graham DG. Evidence that pyrrole formation is a pathogenic step in γ-diketone neuropathy. Toxicol. Appl. Pharmacol. 1987;87:351–362. doi: 10.1016/0041-008x(87)90296-1. [DOI] [PubMed] [Google Scholar]
- 40.Mukouyama SB, Oguchi M, Kodera Y, Maeda T, Suzuki H. Low pka lysine residues at the active site of sarcosine oxidase from Corynebacterium sp. U-96. Biochem. Biophys. Commun. 2004;320:846–851. doi: 10.1016/j.bbrc.2004.05.219. [DOI] [PubMed] [Google Scholar]
- 41.Boekelheide K, Fleming SL, Allio T, Embree-Ku ME, Hall SJ, Johnson KJ, Kwon EJ, Patel SR, Rasoulpour RJ, Schoenfeld HA, Thompson S. 2,5-Hexanedione-induced testicular injury. Annu. Rev. Pharmacol. Toxicol. 2003;43:125–147. doi: 10.1146/annurev.pharmtox.43.100901.135930. [DOI] [PubMed] [Google Scholar]
- 42.DeCaprio AP. Molecular mechanisms of diketone neurotoxicity. Chem.-Biol. Interactions. 1985;54:257–270. doi: 10.1016/s0009-2797(85)80167-8. [DOI] [PubMed] [Google Scholar]