Abstract
Few studies have investigated factors associated with continuous positive airway pressure (CPAP) treatment for sleep apnea from the patients’ and their partners’ perspective. This qualitative research study explored patients’ and partners’ experiences of CPAP and facilitators and barriers to CPAP use, and elicited suggestions for a first-time CPAP user program. Data from 27 participants were collected via four sleep apnea patient and four partner focus groups. Qualitative content analysis identified five themes: knowledge of sleep apnea, effects of sleep apnea, effects of CPAP, barriers and facilitators of CPAP, and ideas for a new user support program. Patients and partners emphasized the importance of partner involvement in the early CPAP treatment period. These data suggest consideration of a couple-oriented approach to improving CPAP adherence.
Keywords: sleep apnea, continuous positive airway pressure, partner
Obstructive sleep apnea (OSA) is an increasingly prevalent sleep disorder affecting 3%-7% of adult men and 2%-5% of adult women (Pujabi, 2008). OSA is defined by repetitive apneas and hypopneas caused by upper airway collapse during sleep. The resultant sleep fragmentation and repetitive hypoxemia have a variety of adverse medical and functional consequences, including excessive daytime sleepiness, reduced quality of life, glucose intolerance, and cardiovascular and cerebrovascular disease (Moyer, Sonnad, Garetz, Helman, & Chervin, 2001; Somers et al., 2008). Continuous positive airway pressure (CPAP) therapy is the conventional treatment for OSA and has been shown to reduce breathing disturbances and daytime sleepiness, improve daily functioning and blood pressure, and decrease mortality rates (Antic et al., 2011; Barbe et al., 2010; Campos-Rodriguez et al., 2005). Despite its efficacy, adherence to CPAP therapy is poor. The optimal hours of nightly use required to return to normal levels of subjective daytime sleepiness, objective sleepiness, memory, and daytime functioning are > 4, 6, > 6, and 7.5 hours, respectively (Stradling & Davies, 2000; Weaver et al., 2007; Zimmerman, Arnedt, Stanchina, Millman, & Aloia, 2006). Observational studies report average hours of nightly CPAP use between 4.7 and 5.9 hours (Engleman, Martin, & Douglas, 1994; Sin, Mayers, Man, & Pawluk, 2002). Thus, many patients are not achieving levels of CPAP use necessary for optimal improvements in daytime function.
OSA is a shared problem negatively affecting patients’ and partners’ sleep, quality of life, and relationship (Doherty, Kiely, Lawless, & McNicholas, 2003; McArdle, Kingshott, Engleman, Mackay, & Douglas, 2001; Parish & Lyng, 2003). In patients with chronic disease, perceived spousal support and involvement have been associated with both improvements and decrements in adherence to medical treatments (Dohery, Schrott, Metcalf, & Iasiello-Vailas, 1983; Stephens et al., 2013). Little is known about the role of relationship factors in CPAP use, but available studies suggest that partners likely exert both positive and negative effects on an individual's adoption and use of CPAP (Baron, Gunn, Czajkowski, Smith, & Jones, 2012; Baron et al., 2011; Baron, Smith, Czajkowski, Gunn, & Jones, 2008; Brostrom et al., 2010; Cartwright, 2008; Hoy, Vennelle, Kingshott, Engleman, & Douglas, 1999). Perceived collaborative spousal involvement has been shown to increase following nights with lower CPAP adherence and greater reported CPAP problems, and is associated with greater subsequent CPAP adherence. On the other hand, perceived spousal pressure is not associated with adherence (Baron et al. 2012; Baron et al., 2011).
Examining the perspectives and experiences of patients and partners regarding OSA and CPAP is critical to gain a better understanding of factors that facilitate and hinder CPAP adherence. Qualitative methods using in-depth interviews, or focus groups, complement existing empirical research that has investigated these factors and add a more in-depth and personal perspective to important issues surrounding CPAP adherence. However, few studies have investigated factors associated with CPAP treatment from the patients’ and, as importantly, their partners’ perspectives (Almeida et al., 2012; Brostrom et al., 2010; Sawyer, Deatrick, Juna, & Weaver, 2010; Willman, Igelstrom, Martin, & Asenlof, 2012). In a qualitative study, partners of OSA patients were interviewed to understand their perceptions of the nature and severity of OSA and the effectiveness of OSA treatment and how their experiences of OSA influenced subsequent help-seeking behavior (Henry & Rosenthal, 2013). Female partners described direct strategies (i.e., waking their husbands during the night, vocalizing displeasure, and scheduling husbands’ medical appointments) to get their husbands to accept that they have a problem and need to seek medical help. Male partners often took a more sensitive approach to broaching the subject such as downplaying their wives’ snoring. Semi-structured interviews with partners of new CPAP users revealed that the support they provide during the initial treatment period is negatively influenced by adverse and limited effects of CPAP, practical and psychosocial problems, and insufficient knowledge (Elfstrom et al., 2012). Conversely, improvements in sleep and alertness in both individuals, an understanding of health consequences of OSA, and support from family and health professionals were positive influences on partners’ support.
As evidenced by qualitative studies (Elfstrom et al., 2012; Henry & Rosenthal, 2013), partners’ perspectives are important for shedding light on the experience of OSA. However, few studies have been conducted to better understand partners’ perspective and role in CPAP adherence. To our knowledge, this is the first qualitative study that engaged both patients and their partners to better understand the experience of CPAP, identify facilitators and barriers to CPAP use, and to elicit suggestions for a new CPAP user program.
Methods
Study Participants
Patients were recruited from the University of Pittsburgh Medical Center Sleep Medicine Center. Sleep physicians informed patients about the study during their medical appointments and obtained verbal consent to provide the patients’ telephone numbers to the Principal Investigator (FSL). Subsequently, the PI contacted patients and scheduled them for a focus group. The PI also inquired whether the patient had a partner (i.e., spouse or significant other) who would be interested in participating in a focus group and, if so, contacted the partner of the patient to schedule them for a focus group as well. Participants were also recruited from the University of Pittsburgh Clinical and Translational Science Institute Research Participant Registry and the PROMIS Sleep-Wake project. To participate in the study, patients had to be over 21 years of age and currently treated for OSA with CPAP. Partners had to be over 21 years of age and married to or in a relationship and sharing a residence with the individual currently being treated for OSA with CPAP. Human subjects approval was obtained from the University of Pittsburgh Institutional Review Board.
Data Collection and Analyses
Eight focus groups were conducted between June 2012 and March 2013 until data saturation was achieved. Patients and partners participated in separate focus groups for a total of four patient groups and four partner groups (3-4 participants per group). During the focus groups, a trained moderator (not one of the study investigators) posed questions and directed conversation to address topics including knowledge about OSA, perceived effects of OSA, initial experience with CPAP, barriers and facilitators to CPAP use, and suggestions for a first-time CPAP user program (Table 1). Each of the focus groups lasted approximately 90 minutes. Half of the focus groups were conducted face-to-face and half were conducted by telephone conferencing. The focus groups were audio recorded, transcribed, and coded with the qualitative software package ATLAS.ti. Demographic information and information on self-reported CPAP usage and effects of CPAP on sleep were collected. Quantitative data were entered into SPSS.
Table 1.
| Focus group guides for patients and partners | |
|---|---|
| Patients | Partners |
| 1. Tell me what you know about sleep apnea. | 1. Tell me what you know about sleep apnea. |
| 2. What effect has sleep apnea had on your quality of life? | 2. What effect has your partner's sleep apnea had on your quality of life? |
| 3. What was your experience like the first night of using CPAP at home? | 3. What was your experience like the first night that your partner used CPAP at home? |
| 4. Are there things that have helped you in using CPAP? | 4. Are there things that have helped your partner in using CPAP? |
| a. If yes, what are those? | a. If yes, what are those? |
| b. How did your partner help your CPAP use? | |
| 5. Are there things that have prevented you from using CPAP or feeling like you can use CPAP? | 5. Are there things that have prevented your partner from using CPAP or feeling like he or she can use CPAP? |
| a. If yes, what are those? | a. If yes, what are those? |
| b. How did your partner hinder your CPAP use? | |
| 6. If you were to develop a special program to help first-time CPA users feel comfortable in using CPAP, what would that program look like? | 6. If you were to develop a special program to help first-time CPA users feel comfortable in using CPAP, what would that program look like? |
| a. What things would you include? Spouses or significant others? | a. What things would you include? Spouses or significant others? |
| b. In what ways would such a program have been helpful when you were beginning CPAP? | b. In what ways would such a program have been helpful when your partner began CPAP? |
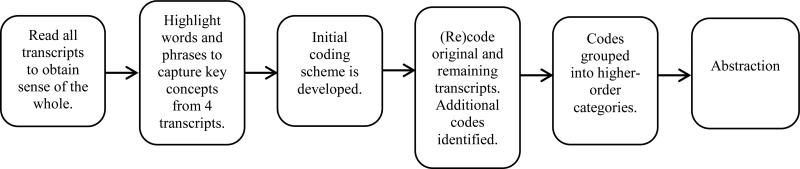
Inductive content analysis was employed, in order to describe the experiences of OSA and CPAP of patients and partners without imposing preconceived categories but rather allowing categories and names of categories to evolve from the data (Elo, & Kyngas, 2008 (Figure 1). To derive these categories, each transcript was read entirely for an overall assessment by two experienced coders. Open coding was completed on 4 of the transcripts during which text was highlighted to denote words or phrases that reflect key concepts. After open coding, preliminary codes were decided upon and a codebook was developed. The original and remaining transcripts were (re)coded using these codes, and new codes were added as needed. Once all transcripts had been coded, codes were grouped into higher-order categories in order to collapse data with similar meaning. Disagreements were resolved through discussion and agreement among the two coders had to be achieved before a response was definitively placed into a specific category. Finally, abstraction was completed by assigning content-based names to the higher-order categories, generic categories, and subcategories. The overall analysis process was overseen by the PI and an expert in qualitative research. The categories are described as a summary of the participants’ statements, and exemplary quotes were selected that best reflect the statements.
Figure 1.
Inductive content analysis process
Results
Participants
The sample included 15 patients with OSA and 12 partners of those patients, for a total of 27 focus group participants. Demographic information was unavailable for one couple who could not be reached to obtain demographic information following the telephone focus groups. The mean age of the patients and partners were 56 years and 54 years, respectively (Table 2). Most patients were males, Caucasian, and had at least some college education. Roughly a third of patients reported having hypertension and/or diabetes, which is consistent with reports from larger, observational studies. Half of patients reported having moderate sleep apnea, and over half reported using their CPAP an average of five to six hours per night. One patient reported not currently using his/her CPAP.
Table 2.
| Demographic characteristics of the focus group participants | ||
|---|---|---|
| Patients (n = 14)1 | Partners (n = 11)1 | |
| Age, mean (SD) | 55.6 (10.3) | 53.5 (16.6) |
| Gender, n (%) male | 9 (64%) | 3 (27.2%) |
| Race, n (%) | ||
| Caucasian | 10 (71.4%) | 8 (72.7%) |
| African-American | 4 (28.6%) | 3 (27.3%) |
| Marital Status, n (%) | ||
| Married | 10 (71.4%) | |
| Living with significant other | 4 (28.6 %) | |
| Education, n (%) | ||
| Less than HS or HS/GED | 4 (28.6%) | 4 (36.4%) |
| Some college or college degree | 5 (35.7%) | 6 (54.5%) |
| Graduate degree | 5 (35.7%) | 1 (9.1%) |
| Self-reported comorbidities, n (%) | ||
| Hypertension | 5 (35.7%) | 3 (27.3%) |
| Coronary heart disease | 1 (7.1%) | 2 (18.2%) |
| Diabetes | 4 (28.6%) | 2 (18.2%) |
| Asthma | 1 (7.1%) | 2 (18.2%) |
| Rheumatoid arthritis | 2 (14.3%) | 0 (0%) |
| Stroke | 0 (0%) | 1 (9.1%) |
| Participants’ sleep quality since CPAP initiation, n (%) | ||
| Very good | 4 (28.6%) | 5 (45.5%) |
| Fairly good | 7 (50%) | 5 (45.5%) |
| Fairly bad | 2 (14.3%) | 0 (0%) |
| Very bad | 1 (7.1%) | 1 (9.1%) |
| Self-reported sleep apnea severity, n (%) | ||
| Mild | 4 (28.6%) | |
| Moderate | 7 (50%) | |
| Severe | 3 (21.4%) | |
| Self-reported Average CPAP usage, n (%) | ||
| Don't use | 1 (7.1%) | |
| 1-3 hours/night | 1 (7.1%) | |
| 4 hours/night | 1 (7.1%) | |
| 5 hours/night | 4 (28.6%) | |
| 6 hours/night | 5 (35.7%) | |
| 7 or more hours/night | 2 (14.3%) | |
| Affected by patient's CPAP, n (%) | ||
| Positive | 7 (63.6%) | |
| Negative | 2 (18.2%) | |
| Neither | 2 (18.2%) | |
Demographic data unavailable for 1 patient and 1 spouse.
Only three partners were males. Over half of partners had some college education. Hypertension, coronary heart disease, diabetes, and asthma were most commonly reported among partners. The majority of partners reported that they were positively affected by their partner's CPAP, but two partners reported being negatively affected. As compared to patients, more partners reported their sleep quality to be very good or fairly good since patients started CPAP.
Given that responses from current users are likely to differ from nonusers (Sawyer et al., 2010), we excluded the one patient who reported not using CPAP at the time of the focus groups and his partner. The data presented from the focus groups will include 14 patients and 11 partners (Table 3).
Table 3.
Focus group categories and subcategories
| Main area | Category | Subcategory (no. of groups in which subcategory was mentioned) |
|---|---|---|
| Knowledge of sleep apnea | Apnea | Stop breathing in middle of night (7) |
| Snoring (7) | ||
| Pauses in breathing cause awakenings (2) | ||
| Brain signals body to start breathing (1) | ||
| Lack of oxygen (2) | ||
| Breathing airway close (1) | ||
| Not only occurs in obese people (2) | ||
| Doesn't know much about OSA (2) | ||
| Surprised to find out diagnosis (2) | ||
| Health Consequences | Sleep loss in patient and partner (3) | |
| Tired/sleepy during day (7) | ||
| Concentration issues (1) | ||
| Cardiovascular problems (3) | ||
| Never woke during night (1) | ||
| Effects of sleep apnea | Physical | Poor sleep (7) |
| Decreased energy (6) | ||
| Morning headaches (2) | ||
| Snoring (6) | ||
| Napping (6) | ||
| Mental/emotional | Patient or spouse scared due to apneas (5) | |
| Irritable (2) | ||
| Interpersonal | Sleeping in separate rooms (3) | |
| Snoring disrupted partner's sleep (5) | ||
| Spouse frustrated (3) | ||
| Effects of CPAP | Initial experience | No problems (3) |
| Determined to use it (3) | ||
| Problems with equipment (6) | ||
| Concerned with noise from CPAP (2) | ||
| Improvements in sleep and energy (3) | ||
| Worried about appearance with mask (2) | ||
| Partner concerned when patient no longer snoring (2) | ||
| Partner provided support (4) | ||
| Physical | Improvements in sleep (5) | |
| Less snoring and apneas (7) | ||
| More energy (6) | ||
| Refreshed in morning (7) | ||
| No improvements in sleep (3) | ||
| Mental/emotional | Improved mood (5) | |
| Less irritable (3) | ||
| Irritated couldn't get mask adjusted (1) | ||
| Felt ashamed (2) | ||
| Interpersonal | Resume bed sharing (2) | |
| Relationship improved (2) | ||
| Impedes intimacy (2) | ||
| Barriers and motivators of CPAP use | Barriers | Mask uncomfortable (6) |
| Inconvenience when traveling (6) | ||
| Cold/sinus infection (4) | ||
| Don't want to put CPAP back on after getting up during night (1) | ||
| Intimacy (2) | ||
| Hard to sleep with CPAP (5) | ||
| Appearance with mask (2) | ||
| Felt ashamed (2) | ||
| Motivators | Better sleep (4) | |
| Feeling refreshed in morning (5) | ||
| Less sleep disruption for partner/family (2) | ||
| Able to engage in activities again (1) | ||
| Spouse support (5) | ||
| Doctor/DME company support (4) | ||
| New user support program | Format options | In-person small groups (2) |
| Lead by respiratory therapist and/or current CPAP user (2) | ||
| Online video (2) | ||
| Question and answer session (3) | ||
| Components | Demonstration of CPAP equipment (4) | |
| Hands-on experience with equipment (2) | ||
| Overnight experience with CPAP in lab with partner (2) | ||
| Education about OSA and CPAP (6) | ||
| Partner participation (4) | ||
| Early follow-up/interaction (5) |
Knowledge of sleep apnea
Patients’ descriptions of sleep apnea were mostly vague and limited to stopping breathing during sleep. Two patients did explain that cessation of breathing at night is due to closing of the airway. Some patients understood that these pauses in breathing disrupt sleep and cause awakenings but that individuals will sometimes not awaken during these episodes. Patients also noted that sleep apnea is common among overweight individuals, although sleep apnea can affect those who are not overweight. Health consequences of sleep apnea such as fatigue, daytime sleepiness, and cardiovascular implications were less commonly included in their explanations of sleep apnea.
Patient: Your brain is not getting enough oxygen because you're stopping breathing because the airway is blocked and you're having sleep interruption which can lead to stroke and other physical issues.
Partners identified sleep apnea as stopping breathing during the night with little to no further explanation. In contrast to patients, partners primarily described sleep apnea as interfering with their own sleep. They also mentioned snoring and tiredness as symptoms and noted heart related consequences of sleep apnea. The best partner explanation of OSA is as follows:
It can be dangerous. They stop breathing, and they also lose sleep themselves, so they're tired during the day, which leads to concentration issues and all that other kind of stuff. Well, I know it's not good for your heart, and it's not good for your blood pressure, because you go a certain amount without oxygen, it's like holding your breath, and so it's strenuous on your cardiovascular system.
Effects of sleep apnea
When asked how sleep apnea affected their quality of life, patients often talked about the daytime effects of sleep apnea including decreased energy, napping, daytime sleepiness, irritability, and morning headaches.
Patient: I was tired a lot during the day, especially later in the day. And also, there would be days where I obviously didn't sleep well at all and I would wake up feeling like I was hung over.
Patients also discussed sleep disruption resulting from sleep apnea.
Patient: You figure every half an hour I wasn't sleeping, because I was stopping breathing. So, instead of getting eight hours of sleep I was really getting four hours sleep, and it wasn't quality sleep, so, it's like you're not sleeping every night.
Yet, partners recognized that patients may not realize that sleep apnea was disruptive to their sleep.
Partner: He thought he was sleeping through the night, and I knew neither of us were.
Partners were distressed by witnessing their partners stop breathing during the night and feared that they may not wake up.
Partner: It was sometimes hard for me to go to sleep because of the way he was breathing, and if he would stop breathing, then I would have to wake him up sometimes because I didn't think he was gonna ever breathe.
This fear was also a concern for patients.
Patient: I was afraid to go to sleep because I would gasp for air and my whole body would shake. But, I'm just thankful that I was able to wake up, but then I was afraid to go back to sleep, fearing that I might not wake up.
For partners, patients’ snoring had a significant impact on their sleep and led to the use of sleep aids, such as medication and earplugs, and alterations in their sleep schedule. Patients acknowledged the impact that their snoring had on their partner. Disrupted sleep contributed to frustration, exhaustion, and even interference at work for partners.
Partner: I felt like it made me wake up and be mean and just say, “Oh, I'm just so tired of hearing you breathe like this.”
Partner: It impacts your workday, you're frustrated because you didn't sleep, and then, my job, I'm in charge of people, and I go and snap out on them at work because I'm tired, and you know, that's not the person I wanted to be.
The loss of sleep from sleep apnea in both patients and partners and the partners’ frustration with their partners’ snoring put a strain on the relationship and in some cases resulted in sleeping in separate rooms.
Partner: It can really drive you into not sleeping and having little quarrels about stuff.
Partner: It wasn't good for us. We were still newlyweds and we weren't even able to sleep in the same room together. I couldn't take it—I was staying up all night, I had insomnia because I was listening to him. And then it caused us to sleep in separate rooms.
Effects of CPAP
Patients voiced both positive and negative initial experiences with CPAP when first using it in their homes. Many patients talked about problems with the mask and/or pressure at first, but most were able to adjust to wearing CPAP at night.
Patient: It obviously wasn't great. I put it on, didn't sleep all that great, but I obviously fell asleep some, but I was so tired the next day that when I put it on the second night, I went right to sleep and I woke up at 5:30 in the morning and I felt like a new human being. And that made me fight through any other discomfort until I got really used to it.
Others were determined to use it from the start, and the initial benefits experienced during the first few nights of using CPAP justified “sticking with it.” Less frequently patients reported no improvement in sleep with CPAP or that they slept better after taking it off. One patient was concerned with his wife's reaction to him wearing the mask.
Patient: My first thought of getting the machine is I didn't like the way everything was going to look on me. I just thought, “Oh, my wife ain't going to love me no more with the way I look at night.”
During the first few nights of their partners using CPAP, partners who were used to hearing their partner snore every night were alarmed by the cessation in their partners’ snoring. Aside from this initial “frightening” experience, partners reported improvements in their sleep.
Partner: It was really scary because I didn't hear him. I didn't hear him snore. And that was frightening.
Both patients and partners had concerns about the loudness of the CPAP machine, but found it to be tolerable if not relaxing.
Partner: It's like a white noise machine. It was great. It was like the first night that I actually realized how much I wasn't sleeping. I didn't have to roll over and kick anybody.
Partners played an essential role in supporting their partners’ CPAP use during the initial few weeks by setting up the machine, helping adjust the mask, and telling their partner to put the mask on if they took it off during the night.
Partner: He did the first couple of nights, take it off in the middle of the night. I would hear him snore, and then I would be like, “you just took your thing off,” and I'd have to go make him put it back on. But now he's pretty good with keeping it on all night. Partner: For the first couple of weeks I'd help her put it on, and make sure everything was OK, and set the machine.
More generally, both patients and partners talked about improvements in their sleep such as being able to fall asleep faster and having fewer awakenings at night. Increases in energy levels enabled them to engage in social and recreational activities again because they were not tired during the day. Patients and partners discussed feeling happier and less irritable. CPAP treatment enabled couples to resume bed sharing and improved marital quality.
Patient: My wife's happier because she's sleeping better.
Partner: He wakes up now more refreshed, and I think, a better person – a happier person ‘cause he had a good night's sleep.
Barriers and motivations for CPAP use
Patients and partners described problems with the equipment, interference with sleep and intimacy, logistical issues, side effects of CPAP, lack of support from healthcare providers, and initial feelings of shame as barriers to CPAP adherence.
Difficulties adjusting the mask, discomfort and pain from the mask, and incorrect pressure setting were commonly reported barriers to adherence.
Patient: Sometimes it's just so uncomfortable to put that mask on at night and I wake up in the morning with a big mark on my face. Not that the mark bothers me, but it hurts. It's like sleeping, you know, with something pressing into your face all night. It's not worth it.
Patients also expressed frustration with falling asleep with the mask on, difficulties changing sleeping positions or sleeping on one's side or stomach, and annoyance with having to put the mask back on after getting out of bed during the night.
Patient: If you get up [during the night], you don't want to put it back on. I don't want to wake myself up trying to get that thing threaded through there.
Interference with intimacy was described as a barrier to adherence.
Partner: I think somehow in his mind he thinks that this machine interferes to some extent with intimacy. And it's like, you know what, it's a convenient mask to take off.
Inconveniences of traveling with CPAP and lack of access to electricity when camping or traveling were discussed.
Partner: He had to make a trip out of town and he said, “I'm not carrying that on the plane and being worried about whether I leave it somewhere. I'm not doing that.”
Side effects of CPAP including nasal congestion, dry mouth, and irritated eyes and the presence of a cold or sinus infection were described as preventing CPAP use for a brief period of time or even more long term for some patients.
Initially, patients felt shameful for needing CPAP treatment and wearing it in the presence of their partner.
Patient: In the beginning, I had the full mask and it was very disconcerting, not only physically but emotionally. I don't know that anyone else experienced this, but I really felt ashamed. I was mad at myself for being in this position and I had to build up time on the machine.
Partner: My husband was very uncomfortable wearing that mask when he went to bed. He kind of hid because it was, you know, not attractive. It's an apparatus and it was just a very uncomfortable feeling for him.
Partner: My partner was trying it on before he really had to use it. I just happened to come in the living room and he had it on, and I just got the feeling that he didn't want me to see him with it on.
The benefits of using CPAP such as improvements in sleep and mood and feeling refreshed in the morning with more energy during the day were motivations for patients to continue using CPAP.
Patient: I love putting it on every night. I feel night and day differently. My quality of sleep has improved, and my mood and my energy during the days. Now in the mornings, it's so much easier to get up.
Support from partners was expressed by patients as motivation for CPAP adherence. Partners supported patients both emotionally by encouraging their partners to use CPAP and reassuring them that their appearance with the mask on is unimportant and instrumentally via verbal reminders and assistance with setting up the machine and putting on the mask.
Patient: I'm very fortunate to have a lovely wife who has taken charge of the machine and makes sure that I use it. She makes sure that there's water in it and she's very attentive to it, so it makes it easy for me to just go along with it.
Partner: I had to reassure him quite often that, you know what, it makes no difference [what he looks like with the mask on] as long as you have a good night's sleep, you can breathe and you don't feel exhausted in the day, you know? At the end of the day, that's really all that matters.
New user support program
Patients and partners suggested format options and important components that would be valuable in developing a program to help first-time CPAP users feel comfortable using CPAP. Small group sessions led by a respiratory therapist and/or a current CPAP user or an online video were identified by patients as optimal formats for providing the program. Having an opportunity to ask questions and having a hands-on demonstration for setting up the machine and becoming familiar with different mask options were emphasized as important components of the program that could help prepare new users.
Patient: I would make sure that they had good instructions on how to adjust those masks and little different things you can do to them. Just to make the transition a little bit easier. ‘Cause I know it was real difficult for me the first night ‘cause it was the first time I had ever put on one of those full masks. I had a tough time getting the straps all right and situated.
Partner: I think showing it to people ahead of time, what it looks like and what it sounds like before you take it home is important. It's not loud, and it's not this big monstrous machine.
Inclusion of partners in a new user program was discussed as a key component. In addition to patients recommending partner participation, partners voiced their preference to be included in such a program since many partners felt uneducated about sleep apnea and CPAP and would have appreciated the information.
Partner: They [ CPAP provider] showed him the machine, that was it. And I felt funny. “Should I be in there or should I not be in there?” You know? I mean, now thinking back, I should have been in there. I should have stuck my nose in and found out what was going on, other than the fact that he has sleep apnea.
Both patients and partners expressed the importance of providing new CPAP users with education regarding sleep apnea, consequences of sleep apnea, and benefits of CPAP including the impact of sleep apnea and CPAP on their partner.
Partner: I think what would really be helpful would be building into it an educational component. Sitting down with a patient and reviewing the results of their sleep study, and pointing out what some of the risk factors are when you have a diagnosis of sleep apnea. Because I don't think a lot of people know.
Patients emphasized the importance of having early interaction with a healthcare professional following initiation of CPAP. Given that questions or concerns are likely to arise during the first night or weeks of using CPAP, patients suggested having access to a 24 hour hotline and follow-up phone calls from a healthcare professional within the first few days after CPAP initiation. Patients also discussed that early feedback regarding patients’ CPAP usage could be informative for new users.
Patient: If somebody is struggling or has a question or is frustrated or upset, they'd be able to call in and be able to talk to someone. Like a CPAP hotline. So you can ask questions or somebody can just walk you through it and tell you, “It'll be alright, it's hard at first, but eventually you get used to it and it will help you in the long run”. It's different when the techs are at your house telling you that, but then when you're there, at night and you're doing it, it's a different feeling.
Patient: First week, I wanted to know how I was doing. I figured, “Hey, you've got a monitor on here, why doesn't somebody call me and say, ‘You're doing pretty good, lady. You're keeping this thing on for eight hours’.”
Discussion
To our knowledge, this is the first study to employ qualitative methods to describe both patients’ and partners’ experiences of CPAP, facilitators and barriers to CPAP use, and suggestions for a first-time CPAP user program. Overall, our findings suggest that both patients and partners were negatively impacted by sleep apnea; that initial experiences with CPAP are mixed; that support from partners is a motivator for CPAP use; and accordingly, inclusion of partners in a new CPAP user program is an important but overlooked component.
In addition to describing daytime impairments and sleep disruption associated with sleep apnea, patients also acknowledged the negative effect that their sleep apnea symptoms had on their partner's sleep. Partners emphasized the profound impact of their partner's snoring on their sleep, which in some cases contributed to sleeping in separate bedrooms. Partners were also distressed by witnessing their partners stop breathing during the night. Sleep loss often resulted in frustration, exhaustion, and interference at work for both patients and partners. The nighttime and daytime consequences of sleep apnea for both individuals and decreased intimacy due to not sharing a bed contributed to strain relationships.
These findings support prior qualitative and quantitative studies that reported poor sleep quality and impaired health-related quality of life in partners of patients with sleep apnea (Brostrom et al., 2010; Doherty et al. 2003; Henry & Rosenthal, 2013; McArdle et al., 2001; Parish & Lyng, 2003). Furthermore, cross-sectional studies have shown adverse associations between sleep apnea and relationship quality as reported by the patient and/or the bed partner (Cartwright, 2008; Virkkula et al., 2005). Interviews with sleep apnea patients and their partners revealed deteriorating or strained relationships resulting from mutual sleep loss due to sleep apnea and spousal anxiety about their partners’ health (Henry & Rosenthal, 2013). Consistent with previous studies (Almeida et al., 2012; Beninati, Harris, Herold, & Shepard, 1999; Doherty et al., 2003; Henry & Rosenthal, 2013; Parish & Lyng, 2003), improvements in sleep and mood and decreases in daytime sleepiness following CPAP treatment were expressed by both patients and partners. Partners indicated reductions in irritability over sleep loss, being able to resume bed sharing, and improved marital quality after CPAP treatment. Limited findings from cross-sectional and longitudinal studies examining the impact of CPAP on relationship functioning suggest that marital satisfaction improves with sleep apnea treatment (Baron et al., 2008; Kiely & McNicholas, 1997; McFadyen, Espie, McArdle, Douglas, & Engleman, 2001).
Whereas several patients had no problems during the initial experience of using CPAP, the majority found it to be challenging with particular difficulties associated with adjustment and comfort of the mask. Despite these challenges, patients acknowledged having positive responses to CPAP treatment (i.e., improved sleep, increased energy) which were motivation for continued use. Few patients reported no improvements in symptoms. Our study results support earlier findings in which adherent users described positive initial experiences and responses to CPAP treatment as influential for continued use (Sawyer et al., 2010). Variability in patients’ initial experiences and reactions to CPAP suggest that patient-centered interventions which personalize sleep apnea symptoms and their impact on individuals’ health and functioning may improve CPAP adoption and adherence, particularly among patients who are ambivalent about treatment (Aloia, Arnedt, Strand, Millman, & Borrelli, 2013; Olsen, Smith, Oei, & Douglas, 2012).
Partners’ descriptions of their partners’ initial CPAP use in the home were both positive with regards to improvements in their sleep and mood and initially disconcerting due to a cessation in their partners’ snoring to which they had become accustomed during the night. Partners reported providing support (e.g., providing assistance with the mask, verbal reminders, encouragement, reassurance of apparent CPAP benefits, and mitigating insecurity about appearance with the mask) during the early treatment period. Spousal involvement in CPAP has been shown to be both a facilitator and barrier to CPAP adherence (Baron et al., 2012; Baron et al., 2011; Baron et al., 2008; Bromstrom et al., 2010; Hoy et al., 1999). Depending on whether negative or positive situations arose during CPAP initiation, partners of OSA patients reported managing these situations differently by allowing the patient to handle the treatment by him/herself, handling the treatment together, or taking over the handling of the treatment (Elfstrom et al., 2012). Our finding that emotional support (i.e., encouraging their partners to use CPAP) and instrumental support (i.e., assistance with setting up the machine and putting on the mask) from partners is a motivator for CPAP use is consistent with previous findings that wife involvement during the first week of treatment is common and that patients’ perceptions of wife support was associated with increased CPAP adherence among patients with more severe sleep apnea (Baron et al., 2011). Moreover, collaborative spousal support during the first week of CPAP treatment was associated with higher CPAP adherence at three month follow-up (Baron et al., 2012).
Our study utilized the unique perspective of current CPAP users and their partners to better understand the challenges, concerns, and needs that they had when first starting CPAP that would be beneficial to address in a new user program. Both patients and partners had a number of recommendations for such a program which included providing education on sleep apnea and CPAP, conducting a demonstration of the CPAP machine and available masks, and providing early feedback and follow-up to inform patients about their CPAP usage and to address concerns or problems. A new user program containing these important components may alleviate fear or uncertainty associated with beginning this new treatment. Our study provides empirical support for comprehensive interventions that provide new CPAP users with education, CPAP instruction and troubleshooting, and intensive follow-up (Smith, Nadig, & Lasserson, 2009; Sparrow, Aloia, DeMolles, & Gottlieb, 2010).
Additionally, the inclusion of partners in a new user program was important to the participants in this study. Partners recognized their lack of knowledge about sleep apnea and CPAP and voiced a desire for information about the condition and its treatment in order to provide more informed support to their partners and be more equipped to address problems should they arise. Lack of knowledge about OSA and CPAP has been identified by partners as negatively impacting their support for their partner's CPAP treatment, thus emphasizing the importance of providing partners with information during the initiation process (Elfstrom et al., 2012). Hoy et al. (1999) and Richards and colleagues (Richards, Bartlett, Wong, Malouff, & Grunstein, 2007) permitted partner attendance in their interventions; however, an important opportunity may have been missed for utilizing this shared experience.
Our study findings support a developmental-contextual model of coping for understanding how couples together appraise and cope with a chronic illness (Berg, & Upchurch, 2007). This model suggests that the ways couples interact in the face of a chronic illness (i.e., dyadic coping) evolve as they move through different stages of dealing with the illness and the involvement of the partner occurs on a continuum from uninvolved (patient is coping individually) to supportive (partner provides instrumental or emotional support) to collaborative (partner is actively involved through joint problem solving and coping) to overinvolved (partner is controlling). Across chronic conditions, partner involvement that is perceived as supportive and collaborative has shown to be associated with improvements in mood in both patients and partners and greater adherence to treatment (Baron et al., 2012; Berg, & Upchurch, 2007; Stephens et al, 2013). Increasing patients’ perceptions of support for CPAP and encouraging couples to collaboratively create problem solving strategies at particularly challenging time points during the course of OSA (e.g., at the time of diagnosis, when treatment is initiated, and daily management) may improve adherence (Baron et al., 2012; Baron et al., 2011). A recent meta-analysis of 25 couple-oriented interventions for chronic illnesses found small but significant effects on patient depressive symptoms, marital functioning, and pain (Martire, Schulz, Helgeson, & Small, 2010). Couple interventions were more efficacious than either patient psychosocial intervention or usual care. Future research that incorporates partners in interventions should consider a tailored approach, examine relationship-related mechanisms of change, and assess outcomes for the partner in addition to the patient (Martire, 2013; Martire et al., 2010). Recent research showing the negative effects of health problems on the partner's sleep suggests that a dyadic approach to intervention for OSA may also benefit the partner's health (Martire, Keefe, Schulz, Stephens, & Mogle, 2013).
Limitations
This study had several limitations. First, although focus groups allow for dynamic interactions, this methodology does have some shortcomings including the possibility of “group think” or dominance of the conversation by some focus group members (Morgan, 1997). We used experienced focus group moderators in our study who guided the discussions so all group members were given the opportunity to respond to the questions. Telephone focus groups were utilized in half of the participants. Telephone interviewing has been suggested as a less threatening forum that may allow participants to more freely disclose information (Novick, 2008). However, a lack of visual cues and its potential impact on data quality is a criticism of telephone interviewing, but there is little evidence to suggest lower data quality obtained by telephone interviewing compared to face-to-face interviewing (Novick, 2008). Although saturation was achieved, the sample size was small and included predominately Caucasians, thus these findings have limited population generalizability. All but one patient reported using CPAP at the time of the focus groups; however CPAP adherence was not objectively measured to validate self-reported use. We choose to exclude the one patient who self-reported not using CPAP and his partner in order to focus on CPAP users as it is possible that differences in views and opinions regarding sleep apnea and CPAP exist between patients who are adherent and nonadherent to CPAP treatment (Sawyer et al., 2010). Thus, the experiences and perceptions of CPAP nonusers and their partners were not captured in our study. Finally, patients in our study included both new CPAP users (on treatment for ≤ 3 months) and experienced users. Greater interaction with the machine among experienced users could have either positively or negatively skewed patients’ perceptions of CPAP and initial experiences with CPAP were likely limited to what the patient could recall. Future research should explore differences in perceptions between new and experienced CPAP users and their partners.
Conclusions
This is the first study to explore partners’ perceptions of CPAP and ideas for a new CPAP user program from the individuals who have personally experienced CPAP, patients and their partners. Partners in our study provided support to patients during the early treatment period that was viewed by patients as motivation for continued CPAP use. Inclusion of partners in a new CPAP user program was identified as a key component. To date, CPAP adherence interventions have focused primarily on the patient. It is recommended, based upon this focus group study, that future adherence interventions evaluate a couple-oriented approach to improving CPAP adherence.
Acknowledgements
We would like to thank Martha Terry, PhD for providing comments for a draft of this manuscript. This project was funded by the National Heart Lung Blood Institute (NHLBI) K23HL1058870 and National Institutes of Health U01AR52155. Preparation of the manuscript was supported in part by K02AG039412.
References
- Almeida FR, Henrich N, Marra C, Lynd LD, Lowe AA, Tsuda H, Ayas N. Patient preferences and experiences of CPAP and oral appliances for the treatment of obstructive sleep apnea: a qualitative analysis. Sleep and Breathing. 2012;17:659–666. doi: 10.1007/s11325-012-0739-6. [DOI] [PubMed] [Google Scholar]
- Aloia MS, Arnedt JT, Strand M, Millman RP, Borrelli B. Motivational enhancement to improve adherence to positive airway pressure in patients with obstructive sleep apnea: a randomized controlled trial. Sleep. 2013;36:1655–1662. doi: 10.5665/sleep.3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antic NA, Catcheside P, Buchan C, Hensley M, Naughton MT, Rowland S, McEvoy RD. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34:111–119. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbé F, Durán-Cantolla J, Capote F, de la Pena M, Chiner E, Masa JF, de Atauri JD. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. American Journal of Respiratory and Critical Care Medicine. 2010;181:718–26. doi: 10.1164/rccm.200901-0050OC. [DOI] [PubMed] [Google Scholar]
- Baron KG, Gunn HE, Czajkowski LA, Smith TW, Jones CR. Spousal involvement in CPAP: does pressure help? Journal of Clinical Sleep Medicine. 2012;8:147–153. doi: 10.5664/jcsm.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron KG, Smith TW, Berg CA, Czajkowski LA, Gunn H, Jones CR. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep and Breathing. 2011;15:525–534. doi: 10.1007/s11325-010-0374-z. [DOI] [PubMed] [Google Scholar]
- Baron KG, Smith TW, Czajkowski LA, Gunn HE, Jones CR. Relationship quality and CPAP adherence in patients with obstructive sleep apnea. Behavioral Sleep Medicine. 2008;7:22–36. doi: 10.1080/15402000802577751. [DOI] [PubMed] [Google Scholar]
- Beninati W, Harris CD, Herold DL, Shepard JW., Jr The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clinic Proceedings. 1999;74:955–958. doi: 10.4065/74.10.955. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Broström A, Nilsen P, Johansson P, Ulander M, Strömberg A, Svanborg E, Fridlund B. Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: a qualitative content analysis. Sleep Medicine. 2010;11:126–130. doi: 10.1016/j.sleep.2009.04.010. [DOI] [PubMed] [Google Scholar]
- Campos-Rodriguez F, Pena-Grinan N, Reyes-Nuñez N, De la Cruz-Moron I, Perez-Ronchel J, De la Vega-Gallardo F, Fernandez-Palacin A. Mortality in obstructive sleep apnea-hypopnea patients treated with positive airway pressure. CHEST Journal. 2005;128:624–633. doi: 10.1378/chest.128.2.624. [DOI] [PubMed] [Google Scholar]
- Cartwright R. Sleeping together: a pilot study of the effects of shared sleeping on adherence to CPAP treatment in obstructive sleep apnea. Journal of Clinical Sleep Medicine. 2008;4:123–127. [PMC free article] [PubMed] [Google Scholar]
- Doherty LS, Kiely JL, Lawless G, McNicholas WT. Impact of nasal continuous positive airway pressure therapy on the quality of life of bed partners of patients with obstructive sleep apnea syndrome. CHEST Journal. 2003;124:2209–2214. doi: 10.1378/chest.124.6.2209. [DOI] [PubMed] [Google Scholar]
- Doherty WJ, Schrott HG, Metcalf L, Iasiello-Vailas L. Effect of spouse support and health beliefs on medication adherence. Journal of Family Pratice. 1983;17:837–841. [PubMed] [Google Scholar]
- Elfström M, Karlsson S, Nilsen P, Fridlund B, Svanborg E, Broström A. Decisive situations affecting partners’ support to continuous positive airway pressure–treated patients with obstructive sleep apnea syndrome: a critical incident technique analysis of the initial treatment phase. Journal of Cardiovascular Nursing. 2012;27:228–239. doi: 10.1097/JCN.0b013e3182189c34. [DOI] [PubMed] [Google Scholar]
- Elo S, Kyngäs H. The qualitative content analysis process. Journal of advanced nursing. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Engleman HM, Martin SE, Douglas NJ. Compliance with CPAP therapy in patients with the sleep apnoea/hypopnoea syndrome. Thorax. 1994;49:263–266. doi: 10.1136/thx.49.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry D, Rosenthal L. “Listening for his breath”: The significance of gender and partner reporting on the diagnosis, management, and treatment of obstructive sleep apnea. Social Science & Medicine. 2013;79:48–56. doi: 10.1016/j.socscimed.2012.05.021. [DOI] [PubMed] [Google Scholar]
- Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? American Journal of Respiratory and Critical Care Medicine. 1999;159:1096–1100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- Kiely JL, McNicholas WT. Bed partners’ assessment of nasal continuous positive airway pressure therapy in obstructive sleep apnea. CHEST Journal. 1997;111:1261–1265. doi: 10.1378/chest.111.5.1261. [DOI] [PubMed] [Google Scholar]
- Martire LM. Couple-oriented interventions for chronic illness: where do we go from here? Journal of Social and Personal Relationships. 2013;30:207–214. [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Stephens MAP, Mogle JA. The impact of daily arthritis pain on spouse sleep. Pain. 2013;154:1725–1731. doi: 10.1016/j.pain.2013.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle N, Kingshott R, Engleman H, Mackay T, Douglas N. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56:513–518. doi: 10.1136/thorax.56.7.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadyen T, Espie C, McArdle N, Douglas N, Engleman H. Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. European Respiratory Journal. 2001;18:996–1002. doi: 10.1183/09031936.01.00209301. [DOI] [PubMed] [Google Scholar]
- Morgan David L. Focus groups as qualitative research. 2nd ed. Vol. 16. Sage Publications, Inc.; Thousand Oaks, CA: 1997. [Google Scholar]
- Moyer CA, Sonnad SS, Garetz SL, Helman JI, Chervin RD. Quality of life in obstructive sleep apnea: a systematic review of the literature. Sleep Medicine. 2001;2:477–491. doi: 10.1016/s1389-9457(01)00072-7. [DOI] [PubMed] [Google Scholar]
- Novick G. Is there a bias against telephone interviews in qualitative research? Research in Nursing & Health. 2008;31:391–398. doi: 10.1002/nur.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen S, Smith SS, Oei TP, Douglas J. Motivational interviewing (MINT) improves continuous positive airway pressure (CPAP) acceptance and adherence: A randomized controlled trial. Journal of consulting and clinical psychology. 2012;80:151–163. doi: 10.1037/a0026302. [DOI] [PubMed] [Google Scholar]
- Parish JM, Lyng PJ. Quality of life in bed partners of patients with obstructive sleep apnea or hypopnea after treatment with continuous positive airway pressure. CHEST Journal. 2003;124:942–947. doi: 10.1378/chest.124.3.942. [DOI] [PubMed] [Google Scholar]
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proceedings of the American Thoracic Society. 2008;5:136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30:635–640. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]
- Sawyer AM, Deatrick JA, Kuna ST, Weaver TE. Differences in perceptions of the diagnosis and treatment of obstructive sleep apnea and continuous positive airway pressure therapy among adherers and nonadherers. Qualitative Health Research. 2010;20:873–892. doi: 10.1177/1049732310365502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. CHEST Journal. 2002;121:430–435. doi: 10.1378/chest.121.2.430. [DOI] [PubMed] [Google Scholar]
- Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea. The Cochrane Database of Systemic Reviews. 2009;2:CD007736. doi: 10.1002/14651858.CD007736. [DOI] [PubMed] [Google Scholar]
- Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Olson LJ. Sleep Apnea and Cardiovascular Disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement From the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. Journal of the American College of Cardiology. 2008;52:686–717. doi: 10.1016/j.jacc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Sparrow D, Aloia M, DeMolles DA, Gottlieb DJ. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax. 2010;65:1061–1066. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]
- Stephens MA, Franks MM, Rook RS, Iida M, Hemphill RC, Salem JK. Spouses’ attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes. Health Psychology. 2013;32:1029–37. doi: 10.1037/a0030018. [DOI] [PubMed] [Google Scholar]
- Stradling JR, Davies RJ. Is more NCPAP better? Sleep. 2000;23:S150–S153. [PubMed] [Google Scholar]
- Virkkula P, Bachour A, Hytönen M, Malmberg H, Salmi T, Maasilta P. Patient-and bed partner-reported symptoms, smoking, and nasal resistance in sleep-disordered breathing. CHEST Journal. 2005;128:2176–2182. doi: 10.1378/chest.128.4.2176. [DOI] [PubMed] [Google Scholar]
- Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, Pack AI. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willman M, Igelström H, Martin C, Åsenlöf P. Experiences with CPAP treatment in patients with obstructive sleep apnea syndrome and obesity. Advances in Physiotherapy. 2012;14:166–174. [Google Scholar]
- Zimmerman ME, Arnedt JT, Stanchina M, Millman RP, Aloia MS. Normalization of memory performance and positive airway pressure adherence in memory-impaired patients with obstructive sleep apnea. CHEST Journal. 2006;130:1772–1778. doi: 10.1378/chest.130.6.1772. [DOI] [PubMed] [Google Scholar]