Abstract
We recently characterized the Δlpp Δpla double in-frame deletion mutant of Yersinia pestis CO92 molecularly, biologically, and immunologically. While Braun lipoprotein (Lpp) activates toll-like receptor-2 to initiate an inflammatory cascade, plasminogen activator (Pla) protease facilitates bacterial dissemination in the host. The Δlpp Δpla double mutant was highly attenuated in evoking bubonic and pneumonic plague, was rapidly cleared from mouse organs, and generated humoral and cell-mediated immune responses to provide subsequent protection to mice against a lethal challenge dose of wild-type (WT) CO92. Here, we further characterized the Δlpp Δpla double mutant in two murine macrophage cell lines as well as in primary human monocyte-derived macrophages to gauge its potential as a live-attenuated vaccine candidate. We first demonstrated that the Δpla single and the Δlpp Δpla double mutant were unable to survive efficiently in murine and human macrophages, unlike WT CO92. We observed that the levels of Pla and its associated protease activity were not affected in the Δlpp single mutant, and, likewise, deletion of the pla gene from WT CO92 did not alter Lpp levels. Further, our study revealed that both Lpp and Pla contributed to the intracellular survival of WT CO92 via different mechanisms. Importantly, the ability of the Δlpp Δpla double mutant to be phagocytized by macrophages, to stimulate production of tumor necrosis factor-α and interleukin-6, and to activate the nitric oxide killing pathways of the host cells remained unaltered when compared to the WT CO92-infected macrophages. Finally, macrophages infected with either the WT CO92 or the Δlpp Δpla double mutant were equally efficient in their uptake of zymosan particles as determined by flow cytometric analysis. Overall, our data indicated that although the Δlpp Δpla double mutant of Y. pestis CO92 was highly attenuated, it retained the ability to elicit innate and subsequent acquired immune responses in the host similar to that of WT CO92, which are highly desirable in a live-attenuated vaccine candidate.
Keywords: Yersinia pestis, Braun lipoprotein, plasminogen activator protease, alveolar macrophages, human monocyte-derived macrophages, intracellular survival, innate immunity
1 Introduction
Yersinia pestis is the causative agent of bubonic and pneumonic plague and is classified as a Tier-1 select agent by the Centers for Disease Control and Prevention (CDC) [1]. The number of plague cases is on the rise globally due to climate change and the migration of rodents infected with fleas, which harbor and disseminate the plague bacterium [2–4]. Consequently, the organism is classified as a re-emerging human pathogen by the World Health Organization [1, 4]. Studies have shown that the optimal temperature for Y. pestis survival within a flea vector is 23–30°C, and as the internal flea temperature increases from 26°C, the ability for Y. pestis to cause mid gut blockage (required for bacterial transmission) declines and fails at 30°C due to changes in the iron-acquisition system [5]. Timely intervention with antibiotics is usually successful in controlling plague; however, the window for the treatment against pneumonic plague is narrow [4, 6]. The live-attenuated Y. pestis EV76 strain, deficient in the pigmentation locus (required for iron acquisition), is effective in combating bubonic and pneumonic plague, and, is currently used in the endemic regions within China and the states of the former Soviet Union [6, 7]. However, this vaccine strain is not approved in the United States and its use is discontinued in several other countries because of the reactogenicity and ability to induce a disease similar to that caused by the wild-type (WT) plague bacterium in immuno-compromised individuals or those with other underlying diseases, such as hemochromatosis [8].
The next generation plague vaccines are based on two Y. pestis components, namely capsular antigen F1 and a type 3 secretion system (T3SS) component, low calcium response V antigen (LcrV) [9, 10]. However, since F1 is dispensable for bacterial virulence and LcrV is not highly conserved in different strains of Y. pestis, the use of such vaccines for immunization may not be effective against all plague-causing strains [6]. Further, such subunit vaccines primarily generate a humoral immune response; however, cell-mediated immunity also plays a role in protection of the host against the plague bacterium [11]. Consequently, there is an urgent need for developing and testing alternative vaccine candidates, especially those that are live attenuated and trigger both arms of the immune response (humoral and cellular) in the host.
Y. pestis is a facultative intracellular pathogen, and during the early stages of an infection, the organism invades both macrophages and neutrophils [12, 13]. While neutrophils typically kill Y. pestis, the organism survives, replicates, and acquires anti-phagocytic capabilities (e.g., by synthesizing capsule and activating T3SS) in macrophages [12, 14–16]. This virulence attribute of Y. pestis represents an important first step in subverting the innate immune response of the host, which aids in subsequent bacterial dissemination leading to progressive bubonic, septicemic, and pneumonic plague [17, 18].
Y. pestis hijacks macrophages from within by preventing phagosome acidification and nitric oxide production [19, 20]. Macrophages are one of the key players in innate immunity and they also are central to bridging innate and adaptive immunities against microbial infections [21]. During bubonic and pneumonic plague, macrophages either in the regional lymph nodes or the lungs are the primary targets for initial bacterial replication [15, 17], thus providing the microbe with a unique niche to avoid antigen presentation, and, therefore, delaying the development of specific immune responses in the host.
Macrophages have been classified into various subsets based on their location, surface markers, and function. Two populations of macrophages that reside in the lungs are interstitial and alveolar. Interstitial lung macrophages closely resemble monocytes and are more involved in immune regulation than alveolar macrophages. Further, due to their location, these macrophages are in direct contact with epithelial and endothelial cells and contribute more to the pathology than alveolar macrophages [22]. In contrast, alveolar macrophages have greater functional activities, such as their ability to undergo phagocytosis and to produce reactive oxygen species [17]. The alveolar macrophages reside in an environment of high lung surfactant that provides survival advantage to them due to the activation of pro-survival signaling molecules [23] when compared to the recruited macrophages (e.g., from bone marrow or those circulating in the blood), which have a shorter lifespan [23]. In addition, macrophages possess a variety of receptors for lineage-determining growth factors, and, therefore, classified into two populations: M1 and M2 [24]. The M1 refers to classically activated macrophages that are capable of sustaining an immune response to pathogens through the release of pro-inflammatory factors, as well as efficient antigen presentation and T-cell stimulation. The M2 refers to alternatively activated macrophages, a very heterogeneous group of cells contributing to resolution of inflammation, tissue repair, extracellular matrix remodeling, and pathogen scavenging [25].
In efforts to search for a novel live-attenuated plague vaccine, we recently generated a Δlpp Δpla double mutant of Y. pestis CO92 [26]. Braun lipoprotein (Lpp) is an outer bacterial membrane component that activates toll-like receptor (TLR)-2 of the host to initiate an inflammatory cascade; its role in evoking bubonic and pneumonic plague has been well characterized in our laboratory [27]. Likewise, plasminogen activator (Pla) protease is a proven virulence factor of Y. pestis which facilitates bacterial dissemination during bubonic and pneumonic plague [26, 28]. The generated Δlpp Δpla double mutant of Y. pestis CO92 was highly attenuated at doses of 1,000 and 10,000 (5 × 105 colony forming units [cfu]) equivalent LD50s of WT CO92 with 100% survival rates when delivered by the intranasal or the subcutaneous route in pneumonic and bubonic plague mouse models, respectively [26]. The mutant bacteria were cleared from the mouse organs rapidly, but Δlpp Δpla double mutant still generated adequate humoral and cell-mediated immune responses to significantly protect animals from developing subsequent pneumonic plague caused by infection with WT CO92 [26].
Our recent data indicated that both Lpp and Pla contributed to the survival of Y. pestis CO92 in murine RAW 264.7 macrophages [26]. We also showed that the role of Lpp in Y. pestis CO92 intracellular survival in these macrophages was linked to the decreased production of a heat shock protein GsrA in the microbe [29]. GsrA is a periplasmic protease required for bacterial adaptation to stress stimuli, and it has been implicated in the survival of Y. enterocolitica and E. coli within macrophages [14]. However, the contribution of Pla to intracellular survival of Y. pestis in macrophages represents a new paradigm; as previous studies from other groups have shown that Y. pestis strains lacking pPCP-1 plasmid, which encodes Pla, were still able to replicate inside the macrophages [30–32]. The mechanism(s) by which Pla contributes to Y. pestis intracellular survival is currently unknown.
Considering the curial role of macrophages during Y. pestis infection and the functional heterogeneity of macrophages, it is important to further evaluate interaction of the Δlpp Δpla double mutant of Y. pestis CO92 with different types of macrophages and gauge its potential as a live-attenuated vaccine candidate. Three different types of resting macrophages, namely murine RAW 264.7 and MH-S, and human primary macrophages derived from blood monocytes of healthy donors were used in this study. While the MH-S cell line represents resident lung macrophages, both RAW 264.7 and human primary macrophages closely mimic the recruited macrophages which are derived from the bloodstream monocytes [33–35]. Consequently, due to some intrinsic differences between resident versus recruited macrophages [33, 34], the intracellular survival of Y. pestis mutants could differ in various types of macrophages and was the focus of this study.
Our study showed that the Δpla single and the Δlpp Δpla double mutant was unable to survive efficiently in all tested macrophages compared to WT CO92 and that both Lpp and Pla contributed to intracellular survival by operating through different mechanisms. Importantly, the Δlpp Δpla double mutant retained the ability to elicit innate and subsequent acquired immune responses in the host similar to that of WT CO92. This is the first detailed study delineating the role of Lpp and Pla, as well as their interplay, in the survival of Y. pestis in professional resting macrophages.
2 Results and Discussion
2.1 Survival of various mutant strains of Y. pestis CO92 in murine RAW 264.7 and MH-S macrophages
One of the first steps during Y. pestis infection is the phagocytosis of the pathogen by macrophages within which the organisms survive and replicate before being further disseminated to cause a progressive disease. Consequently, we examined intracellular survival of WT CO92 and its various mutants (Δlpp and Δpla single, and the Δlpp Δpla double), as well as their respective complemented strains in murine RAW 264.7 macrophages when infected at a multiplicity of infection (MOI) of 1. We chose this cell line to confirm our previous findings [26] with additional control strains to authenticate the data.
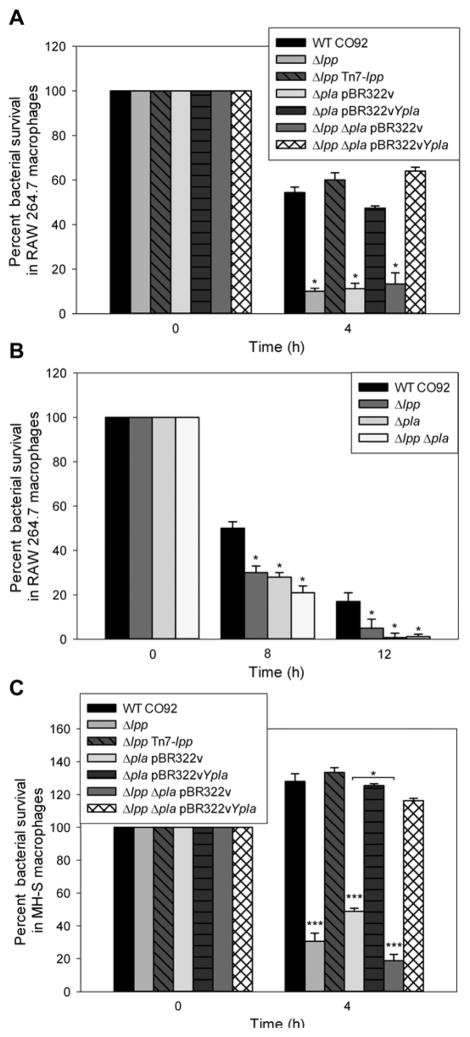
As shown in Fig. 1A, WT CO92 had an intracellular survival rate of 55% at 4 h post-gentamicin treatment (section 4.3), and in comparison, the Δlpp and Δpla single mutants were below 10% survival. Complementation of the Δlpp (Δlpp Tn7-lpp [in cis]) and Δpla (Δpla pBR322vYpla [in trans]) (Table 1) single mutants resulted in restoration of their intracellular survival phenotype similar to that of WT CO92 (~50–60%) (Fig. 1A). Likewise, the Δlpp Δpla double mutant survived minimally in RAW 264.7 macrophages (less than 10%), while complementation of the double mutant with the pla gene (Δlpp Δpla pBR322vYpla [in trans]) exhibited 60% survival rate. These results correlated with our previous study in RAW 264.7 cells which also showed decreased intracellular survival of Δlpp and Δpla single, and the Δlpp Δpla double mutants [26]. Importantly, we have now shown that the decreased intracellular survival of the Δpla single and the Δlpp Δpla double mutant could be fully complemented in trans, confirming the role of Pla in Y. pestis intracellular survival. In another independent experiment, additional time points of 8 and 12 h were examined. We noted a similar decrease in intracellular survival of both the single (Δlpp and Δpla) and the double mutant (Δlpp Δpla) in RAW 264.7 macrophages (Fig. 1B), which continued to decline further at a 24 h time point (data not shown).
Figure 1. Intracellular survival of WT Y. pestis CO92 and its mutant strains in murine macrophages.
RAW 264.7 macrophages (A & B) and MH-S alveolar macrophages (C) were infected with WT CO92, its single mutants (Δlpp and Δpla), and the Δlpp Δpla double mutant, as well as the complemented strains for 45 min at an MOI of 1. Monolayers were then treated with gentamicin for 1 h, gentamicin was then removed, and the host cells harvested at 0 and 4 h post-gentamicin treatment to determine surviving intracellular bacteria. (B) Additional time points, including 8 and 12 h post-gentamicin treatment, were taken to determine long term intracellular bacterial survival in RAW 264.7 macrophages. Bacteria were enumerated and the percent survival rate was calculated based on the number of bacteria recovered at each specific time point over that at the 0 h time point. At least three independent experiments were performed, and three wells of macrophages for each bacterial strain were used for the infection and plated in duplicate to determine intracellular bacterial counts. The pooled data were shown and error bars indicated standard deviations for percent intracellular bacteria. The data from both of the cell lines were analyzed using One-way ANOVA with Bonferroni correction and p values ≤0.05 were considered significant. Asterisks indicate statistically significant differences when compared to WT CO92-infected cell lines or between two groups indicated by a horizontal line (*p<0.05, ***p<0.01).
Table 1.
Bacterial strains and plasmids used in this study
| Strain/Plasmid | Description and Source | Reference |
|---|---|---|
| Strains | ||
| Y. pestis CO92 | ||
| WT CO92 | Virulent WT Y. pestis isolated in 1992 from a fatal pneumonic plague case, biovar Orientalis, and naturally resistant to polymyxin B | [63, 64] |
| WT CO92 (pBR322vYgsrA) | Y. pestis CO92 WT strain supplied with gsrA via plasmid pBR322vYgsrA (Tcs) | This study |
| Δlpp | lpp deletion mutant of Y. pestis CO92 | [27] |
| Δlpp Tn7-lpp | CO92 Δlpp mutant complemented with lpp in cis by using the targeted Tn7 | [36] |
| Δlpp (pBR322v) | CO92 Δlpp mutant transformed with plasmid pBR322v (Tcs) | [42] |
| Δlpp (pBR322vYgsrA) | CO92 Δlpp mutant complemented with gsrA via plasmid pBR322vYgsrA (Tcs) | [42] |
| Δpla | pla in-frame deletion mutant of Y. pestis CO92 | [26] |
| Δpla (pBR322v) | CO92 Δpla mutant transformed with plasmid pBR322v (Tcs) | [26] |
| Δpla ( pBR322vYpla) | CO92 Δpla mutant complemented via plasmid pBR322vYpla (Tcs) | [26] |
| Δpla ( pBR322vYgsrA) | CO92 Δpla mutant complemented with gsrA via plasmid pBR322vYgsrA (Tcs) | This study |
| Δlpp Δpla | lpp and pla gene double deletion mutant of Y. pestis CO92 | [26] |
| Δlpp Δpla (pBR322v) | CO92 Δlpp Δpla double mutant transformed with plasmid pBR322v (Tcs) | [26] |
| Δlpp Δpla (pBR322vYpla) | CO92 Δlpp Δpla double mutant complemented via plasmid pBR322vYpla (Tcs) | [26] |
| Δlpp Δpla (pBR322vYgsrA) | Y. pestis lpp and pla double deletion mutant complemented with gsrA via plasmid pBR322vYgsrA (Tcs) | This study |
| Plasmids | ||
| pBR322v | Cloning vector pBR322 variant and sensitive to tetracycline (Tcs) | [42] |
| pBR322vYpla | Recombinant plasmid containing the pla gene coding region and its putative promoter in vector pBR322v used for complementation (Tcs) | [26] |
| pBR322vYgsrA | Recombinant plasmid containing the gsrA gene coding region and its putative promoter in vector pBR322v (Tcs) | [42] |
TcS=tetracycline sensitive
Our results that the Δpla single mutant was unable to survive in RAW 264.7 macrophages (Fig. 1A&B) contrasted from the earlier study in which we demonstrated that WT CO92 cured for the pPCP-1 plasmid was initially (4 to 8 h) sensitive to the macrophage environment but recovered and had a survived rate similar to that of WT CO92 by 24 h [36]. Therefore, it is tempting to speculate that other genes present on the pPCP-1 plasmid (e.g., pst and pim) might modulate the survival of the plasmid-cured CO92 strain in macrophages compared to that of the Δpla single isogenic mutant which still contained the pPCP-1 plasmid devoid of the pla gene.
Since deletion of both the lpp and pla genes individually decreased intracellular survival of the mutants drastically, we were unable to discern any additive effect of the combined deletion of these two genes from the Δlpp Δpla double mutant (Fig. 1A&B). Supplying pla in trans compensated the deletion effect of lpp in terms of intracellular survival of the Δlpp Δpla double mutant in RAW 264.7 macrophages (Fig. 1A). This was surprising as we anticipated only partial restoration of the intracellular survival phenotype of the double mutant. To further confirm and pursue our findings, MH-S, a murine immortalized alveolar macrophage cell line, was tested, as lungs are the primary target during pneumonic plague infection.
The MH-S cells were infected at an MOI of 1 with WT CO92, its various mutants, and the complemented strains (Fig. 1C). As noted, 4 h post-gentamicin treatment (section 4.3), WT CO92 not only survived but also proliferated in these cells, as the percent survival exceeded 100%. In comparison, the survival rates of the Δlpp and Δpla single mutants were 30 and 45%, respectively. We could fully complement the Δlpp and Δpla single mutants in terms of their intracellular survival phenotype with the corresponding genes (Fig. 1C). Importantly, the Δlpp Δpla double mutant survived minimally (less than 20%) in MH-S cells and exhibited an additive decrease in its ability to survive intracellularly when compared to the Δlpp and Δpla single mutants (Fig. 1C). a phenomenon either not observed (Fig. 1A) or barely noted in RAW 264.7 macrophages (Fig. 1B). Interestingly, complementation of the double mutant with the pla gene restored the intracellular survival phenotype comparable to that of WT CO92 in MH-S macrophages (Fig. 1C), as also noted in the RAW 264.7 cells.
As alluded to earlier, the role of Lpp in Y. pestis intracellular survival was linked to the decreased production of a heat shock protein GsrA within the microbe [29]. Since the decreased intracellular survivability of the Δlpp Δpla double mutant in both RAW 264.7 and MH-S cells was fully complemented with the pla gene when supplied in trans (Fig. 1A&C), these findings suggested that Lpp and Pla might have had a similar mechanism of action, i.e., decreasing the production of GsrA, and thus production of Pla could compensate the effect of Lpp in the Δlpp Δpla double mutant (Fig. 1A&C). Alternatively, there might be interplay between Pla and Lpp as the deletion of one gene could possibly affect the expression of the other gene, eventually leading to an alteration in the level of GsrA.
2.2 Crosstalk between Lpp and Pla, and the role of GsrA in modulating Y. pestis CO92 survival in macrophages
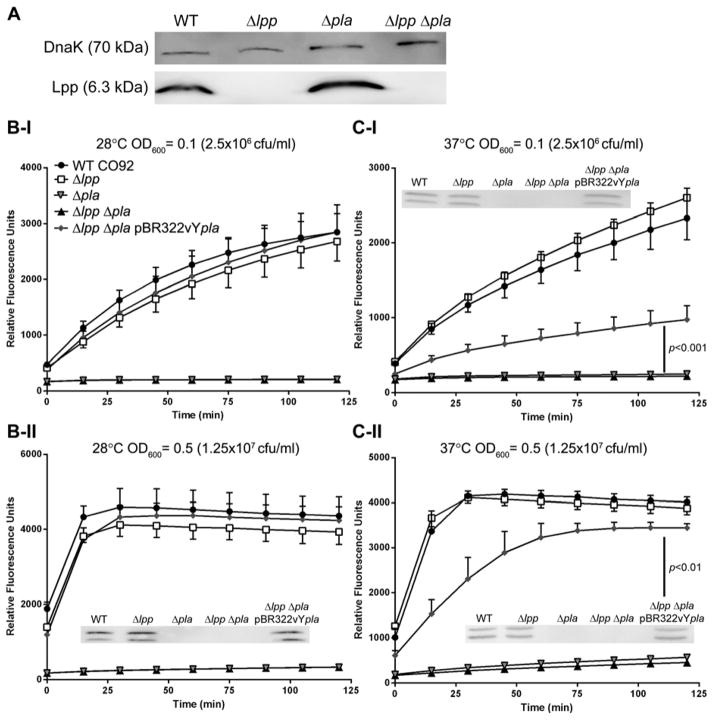
To further dissect the mechanism of Pla in Y. pestis intracellular survival and to test the possibility whether deletion of the pla or the lpp gene from WT CO92 would affect expression and production of these membrane proteins, we performed Western blot analysis and the Pla activity assay. As noted from Fig. 2A, while WT CO92 and the Δpla single mutant had similar levels of Lpp, no Lpp production was noted in the Δlpp single or the Δlpp Δpla double mutant. Likewise, similar levels of Pla were noted in the Δlpp single mutant when compared to its level in the WT CO92 (Fig. 2B&C, insets). However, Pla was absent from the Δpla single and the Δlpp Δpla double mutants. The production of Pla was restored in the above-mentioned Δlpp Δpla double mutant after complementation with the pla gene in trans (Fig. 2B&C, insets).
Figure 2. The expression of lpp and pla genes as well as Pla associated protease activity in various Y. pestis strains.
Yersinia cultures were grown overnight at 28°C. The expression of the lpp gene was evaluated by Western blot analysis using anti-Lpp monoclonal antibodies. The level of DnaK in bacterial pellets was examined by using anti-DnaK antibodies as a loading control (A). For Pla protease activity, Yersinia cultures were grown on the HIB agar plates either at 28°C (B) or 37°C (C) for 20–22 h and suspended in PBS to OD600 of 0.1 (5 × 107 cfu/ml) (B-I and C-I) and 0.5 (B-II and C-II) (2.5 × 108 cfu/ml), respectively. Pla protease activity was measured in a fluorometric assay. The kinetics of substrate cleavage (increase in RFUs vs. time) by Pla was plotted for each bacterial strain. Statistical analysis was performed by One-way ANOVA with a Bonferroni post-hoc test. Statistically significant p values are shown between the groups by a vertical line. The expression of the pla gene in the above-mentioned cultures was evaluated by Western blot analysis with anti-Pla polyclonal antibodies (insets).
It has been reported that lipooligosaccharide (LOS) present on the bacterial surface can affect the conformation of Pla, with the more biologically active form of Pla being displayed on the bacterial surface at 37°C [37]. Since both Lpp and Pla are also bacterial outer membrane components, we measured protease activity associated with Pla to ensure that the enzymatic activity of this protein remained unaffected by deletion of the lpp gene from WT CO92 by using a fluorometric assay and a hexapeptide substrate [38]. The Pla protease assay was performed at two different bacterial concentrations and temperatures to measure the kinetics of substrate cleavage. The use of two growth temperatures allowed us to measure Pla protease activity at both flea (28°C) and human body temperatures (37°C).
Further, as mentioned earlier, the bacterial surface structure changes at different temperatures. For examples, the F1 capsular antigen is primarily synthesized at 37°C, the lipid A of Y. pestis LOS shifts from a hexa-acylated form to a tetra-acylated form when the temperature shifts from 21–27°C to 37°C [39]. In addition, the production of Attachment Invasion Locus (Ail), another bacterial outer membrane component, is up regulated at 37°C [40]. These surface alterations could affect the conformation of Pla and its associated enzymatic activity and was tested.
As noted in Fig. 2B, when various bacterial strains were grown at 28°C and adjusted to an OD600 of 0.1 (2.5 × 106 colony forming units [cfu] in 50 μl reaction per well) (I) or 0.5 (1.25 × 107 cfu in 50 μl reaction per well) (II) (section 4.6), WT CO92 and its Δlpp single mutant had essentially similar kinetics of Pla substrate cleavage. The Δpla single and the Δlpp Δpla double mutant in comparison showed minimal background activity. Complete restoration of Pla protease activity was noted when the Δlpp Δpla double mutant was complemented with the pla gene in trans and was comparable to that of WT CO92 and its Δlpp single mutant, with essentially similar Pla substrate cleavage kinetic curves over time (Fig. 2B-I&II).
When the bacteria were grown at 37°C (Fig. 2C), a similar kinetics of substrate cleavage by Pla was noted at both ODs of 0.1 (I) and 0.5 (II) for WT CO92, its single mutants Δlpp and Δpla, as well as the Δlpp Δpla double mutant as was also observed at 28°C (Fig. 2B-I&II). However, only partial restoration of Pla protease activity was seen when the Δlpp Δpla double mutant (OD of 0.1) was complemented with the pla gene in trans, although it was still significantly higher when compared to the Δpla single and the Δlpp Δpla double mutant (Fig. 2C-I).
The kinetics of substrate cleavage by Pla was also slower initially for the Δlpp Δpla double mutant complemented strain at an OD600 of 0.5 (Fig. 2C-II); however, it exhibited a kinetic curve similar to that of WT CO92 and its Δlpp mutant over a period of 2 h, indicating that Pla protease activity almost reached saturation at an OD600 of 0.5 (Fig. 2C-II). These data suggested that a temperature shift did not significantly impact Pla protease activity in these strains. However, misfolding of Pla could most likely account for the relatively lower Pla protease activity observed for the Δlpp Δpla double mutant complemented strain at 37°C (Fig. 2C).
These data were further validated as the level of Pla production in this complemented strain was similar to that of WT CO92 based on Western blot analysis both at ODs of 0.1 and 0.5 (Fig. 2C-I&II-insets) as both the pPCP-1 (harboring the pla gene) and pBR322v are low-medium copy number plasmids [41]. The autoproteolysis of Pla is responsible for the appearance of two bands during the Pla Western blot analysis; however, it is not known whether autoprocessed or unprocessed Pla forms are equally active. Clearly, there did not seem to have a direct interaction between Pla and Lpp in terms of their production levels and Pla protease activity (Fig. 2).
The data presented above were intriguing as supplying the pla gene in trans only partially restored Δlpp Δpla double mutant’s protease activity at 37°C (Fig. 2C), but it could fully restore the intracellular survival of the Δlpp Δpla double mutant in RAW 264.7 and MH-S macrophages (Fig. 1A&C). This question led us to the second part of our hypothesis that Pla might have a different mechanism than Lpp (not through GsrA) in terms of bacterial intracellular survival. To address this, we complemented Δlpp and Δpla single, and the Δlpp Δpla double mutant with the grsA gene using the pBR322v vector system. Our results for the Δlpp single mutant correlated with our earlier study [42] showing complete restoration of mutant’s ability to grow within MH-S macrophages when the Δlpp single mutant was complemented with the gsrA gene (Fig. 3). However, when the Δpla single mutant was complemented with the gsrA gene, there was no restoration of intracellular survival. Importantly, GsrA could only partially restore the intracellular survival of the Δlpp Δpla double mutant, suggesting that GsrA complemented the effect of Lpp deletion but not that of Pla (Fig. 3).
Figure 3. The role of GsrA in the intracellular survival of Δlpp and Δpla single, and the Δlpp Δpla double mutant of Y. pestis CO92.
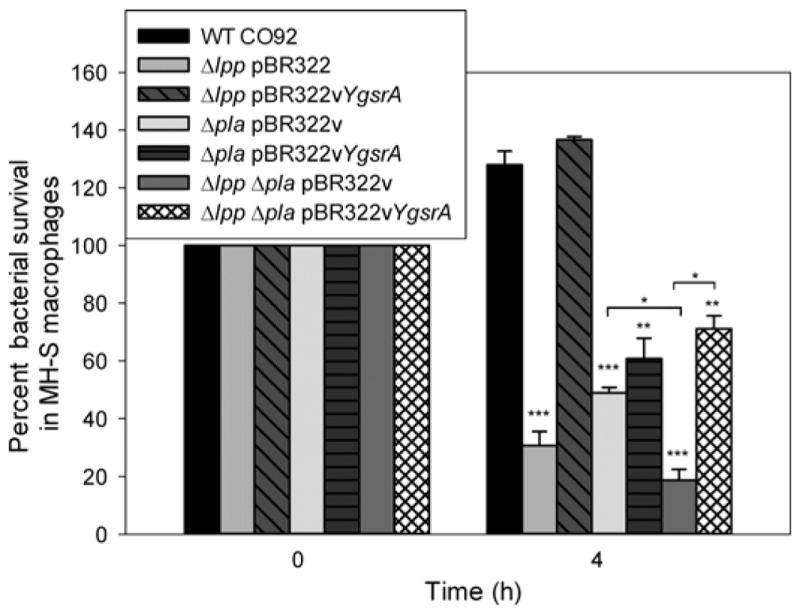
MH-S macrophages were infected with WT CO92, its single mutants (Δlpp and Δpla), the Δlpp Δpla double mutant, as well as their gsrA complemented strains. Intracellular survival was assessed via a gentamicin protection assay as described in Figure 1 legend. The experiments were performed in triplicate, and within each experiment three wells of macrophages for each bacterial strain were used for the infection and plated in duplicate to determine intracellular bacterial counts. The pooled data were shown and error bars indicated standard deviations for percent intracellular bacterial survival. The data were analyzed using One-way ANOVA with Bonferroni correction and p values ≤0.05 were considered significant. Asterisks indicate statistically significant differences when compared to WT CO92 infected MH-S cells or between the two groups indicated by a horizontal line (*p<0.05, **p<0.01, ***p<0.001).
We noted only a marginal and statistically insignificant increase in intracellular survival of WT CO92 when the gsrA gene was expressed from the plasmid pBR322v (data not shown). However, a substantial increase in the intracellular survival of the Δlpp mutant was observed when complemented with the gsrA gene (Fig. 3), clearing indicating Lpp operating through GsrA in modulating bacterial intracellular survival. Further, our published microarray data indicated that deletion of the lpp gene decreased transcript level of the gsrA gene [42]. These data confirmed that Lpp and Pla operated through separate mechanisms to control intracellular survival of Y. pestis CO92. However, it was still not clear why Pla could compensate the effect caused by Lpp deletion on the intracellular survival in macrophages of the Δlpp Δpla double mutant of Y. pestis CO92 (Fig. 1A&C).
Bacterial heat shock proteins, collectively termed as stress proteins, play an important role in allowing organisms to successfully adapt to the hostile environment of the host phagosome [14, 43]. HtrA, also known as DegP [44] or GsrA, has serine protease activity [45]. GsrA degrades abnormal peptides generated after exposure of bacteria to stress before they accumulate to toxic levels in the periplasmic space [45]. The production of GsrA is controlled by the sigma factor E (σE), a global stress response regulator, and the activity of σE is induced by either overproduction or misfolding of outer membrane proteins (OMPs), leading to the increased production of GsrA in E. coli and Y. enterocolitica [43, 46]. Therefore, it is possible that the misfolded Pla in the complemented Δlpp Δpla double mutant of Y. pestis CO92 (Fig. 2C) with low Pla protease activity could possibly activate the expression of the gsrA gene through σE to exhibit full complementation of the intracellular survival defect (Fig. 1A&C).
In addition to GsrA, other heat shock proteins such as DnaK, GroEL, and GroES are essential for bacterial growth and viability at all temperatures in bacteria [47, 48]. It has also been shown that DnaK and GroEL bind to unfolded polypeptides and function as “molecular chaperones” in cells [49]. Although the role of Pla in Y. pestis intracellular survival is not through GsrA; however, as an OMP, it is still possible that deletion of the pla gene would lead to decreased production of other stress response proteins, and our future studies will investigate this possibility.
2.3 Survival of WT Y. pestis CO92 and its Δlpp Δpla double mutant in human monocyte-derived macrophages (HMDMs)
To be a vaccine candidate, it was crucial to evaluate the Δlpp Δpla double mutant of Y. pestis CO92 in primary human macrophages from healthy individuals (section 4.2). As shown in Fig. 4A, the WT CO92 exhibited survival rates of 100% and 50% at 1 and 2 h, respectively, post-gentamicin treatment (section 4.4), the double mutant survival rates were 80% and 25%, respectively, at the designated times. We focused on the Δlpp Δpla double mutant in HMDMs, as we had earlier shown its potential as a viable plague vaccine candidate [26].
Figure 4. Intracellular survival of WT Y. pestis CO92 and its mutant strains in human monocyte-derived macrophages (HMDMs).
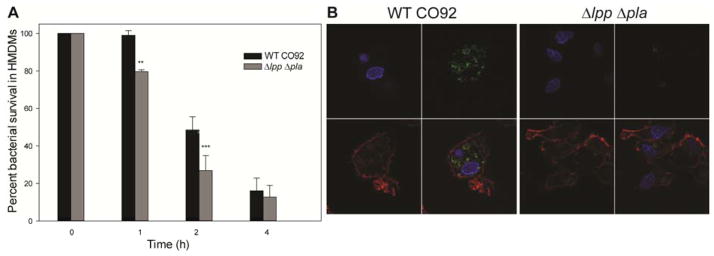
Macrophages from three individual donors were infected at an MOI of 0.5 with either the WT CO92 or Δlpp Δpla double mutant for 40 min following 1 h gentamicin treatment (10 μg/ml). At 0, 1, 2, and 4 h (post-gentamicin treatment), macrophages were harvested and the number of bacteria inside macrophages was counted. The percent survival rate was calculated based on the number of bacteria recovered at each specific time point over that of the 0 h time point. The pooled data were shown and error bars indicated standard deviations for percent intracellular bacterial survival (A). The data were analyzed using One-way ANOVA with Bonferroni correction and p values ≤0.05 were considered significant. Asterisks indicate statistically significant differences compared to WT CO92-infected HMDMs (**p<0.01, ***p<0.001). At the 1 h time point, the infected HMDMs were also fixed and the bacteria inside the macrophages were detected by specific anti-F1 (capsular antigen) antibodies follow by secondary Alexa Fluor 488 antibodies (green). The actin filaments were stained with Alexa Fluor 568 phalloidin (red), and the cell nucleus was visualized with DAPI (blue). The images were taken by confocal microscopy with the magnification of 1,000 (B).
In addition to cfu determination, the HMDMs infected with either the WT CO92 or the Δlpp Δpla double mutant (1 h post gentamicin treatment), were stained for visualization of bacteria by confocal microscopy (Fig. 4B). We chose to use antibodies specific to the F1 antigen to detect Y. pestis as we had previously shown that the production of F1 in the Δlpp Δpla double mutant was not altered compared to the WT CO92 [26]. Following the addition of fluorescently labeled secondary antibodies, we detected much reduced level of the Δlpp Δpla double mutant (green) in infected macrophages when compared to WT CO92, thereby corroborating our in vitro results that the Δlpp Δpla double mutant was unable to survive as effectively as WT CO92 in macrophages (Fig. 1A–C and 4A).
The inability of the Δlpp Δpla double mutant to survive within different macrophages (i.e., RAW 264.7, MH-S, and HMDMs) correlated with the mutant’s inability to disseminate to the peripheral organs of mice during initial 2–8 days post infection in both bubonic and pneumonic plague models [26]. Interestingly, WT Y. pestis and its various mutant strains survived and replicated to higher numbers in the murine alveolar macrophages (MH-S) compared to RAW 264.7 and HMDMs, indicating intrinsic differences between resident versus recruited macrophages and signifies the role of alveolar macrophages during pneumonic plague. Previous studies showed that the dissemination of Pla-deficient Y. pestis was more severely affected in bubonic plague mouse model than in the pneumonic plague model [26, 28, 50]. Consequently, better survival and replication of the plague bacilli in alveolar macrophages might contribute to this phenomenon in addition to the highly vascularized nature of the lungs [28].
The role of Pla in promoting bacterial dissemination during bubonic and pneumonic plague had been previously attributed to its fibrinolytic activity [28, 51]. However, considering the crucial role of macrophages in disseminating Y. pestis in vivo [2, 28], the role of Pla in aiding bacterial intracellular survival may also contribute significantly to this feature.
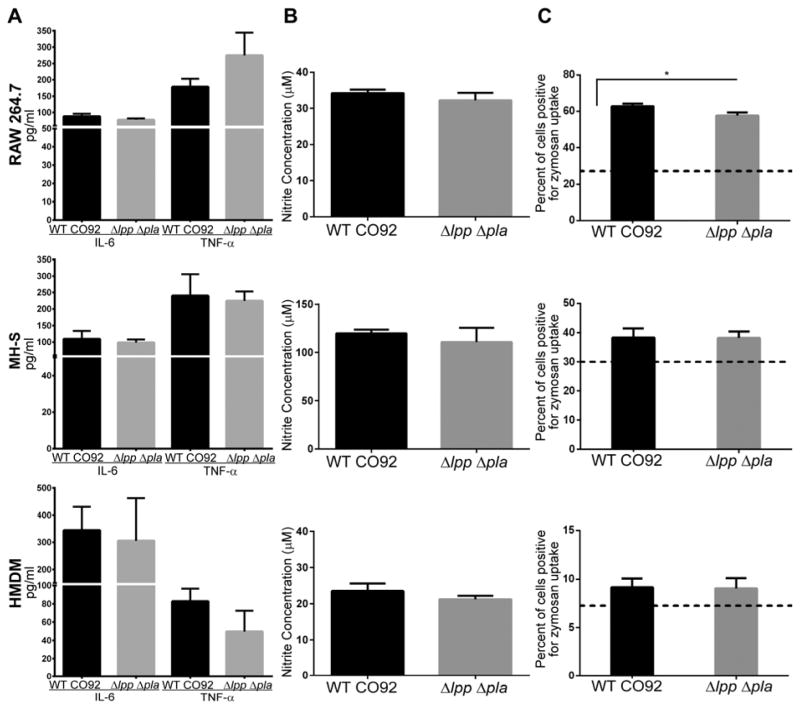
2.4 Cytokine secretion levels are comparable in different types of macrophages when infected with WT Y. pestis CO92 and its Δlpp Δpla double mutant
Three different types of macrophages were used to analyze whether their infection with WT CO92 or the Δlpp Δpla double mutant elicited similar levels of cytokines production. Supernatants from the infected macrophages were harvested immediately after an hour of gentamicin treatment (100–105 min post infection) and analyzed by 6-Bioplex from Bio-Rad (section 4.7). It should be mentioned that after initial infection of macrophages with the bacteria, the host cells were washed before gentamicin treatment to remove any cytokines that were formed by the interaction of macrophages with the extracellular bacteria. As shown in Fig. 5A, interleukin (IL)-6 and tumor necrosis factor (TNF)-α were the only two cytokines among the six analyzed, which were detected at the highest concentrations across the three macrophage types used. Importantly, similar levels of these cytokines were detected irrespective of whether the macrophages were infected with the WT CO92 or the Δlpp Δpla double mutant. These data indicated that despite rapid clearance of the Δlpp Δpla double mutant from macrophages, the innate immune effector cells were still responding to activation evoked by this highly attenuated strain. These observations complemented our detailed T-cell responses in terms of cytokine production by the WT CO92 and its double mutant (Δlpp Δpla), which were recently published (24). We also measured IL-1β, IL-10, IFN-γ and IL-17 which were detected at low levels both in WT CO92 and Δlpp Δpla double mutant-infected macrophages (data not shown).
Figure 5. The cytokine and nitrite production as well as the zymosan uptake of macrophages elicited by infection with WT CO92 and its Δlpp Δpla double mutant.
Macrophages were infected with WT CO92 and its Δlpp Δpla double mutant at MOI of 1, washed, and then subjected to gentamicin treatment. Culture supernatants were collected immediately after gentamicin treatment for analyzing cytokine production by using 6-plex Bio-Rad multiplex assay (A) or at 12 h post infection for the production of nitrite by using the Griess assay (B). For the zymosan uptake (C), the above infected macrophages were incubated with 1 × 106 (1 μm) of Texas-Red zymosan particles after the gentamicin treatment. The number of macrophages positive for beads was enumerated by flow cytometry. The dotted line represents percent of uninfected macrophages positive for zymosan uptake. Statistical analysis was performed by One-way ANOVA with Tukey’s post-hoc test, and the statistical significant difference is indicated by an asterisk with p<0.05 when compared to the uninfected control macrophages (*p<0.05). The pooled data from three independent experiments were shown and error bars indicated standard deviations.
IL-6 is a notable pro-inflammatory cytokine secreted by various cell types, including the activated macrophages [52]. It has been shown that recombinant plant-derived Y. pestis F1, LcrV (also termed V) and F1-V, the key components of the next generation plague subunit vaccine, are TLR-2 agonists, and, importantly, they significantly increase IL-6 production in human monocytes [20]. In addition, IL-6 switches the differentiation of monocytes from dendritic cells to macrophages, and, therefore, is essential in molecularly controlling antigen presentation and cell development [53]. IL-6 has also been reported to enhance polarization of alternatively activated macrophages, and, thus would promote resolution of inflammation and wound healing [24].
On the other hand, TNF-α is one of the most important pro-inflammatory cytokines which limits severity of bacterial infection [20]. Interestingly, both IL-6 and TNF-α could act synergistically in prolonging plasma cell survival, leading to better antibody responses [54], which correlates with our previously published data indicating a robust humoral immune response generated by the Δlpp Δpla double mutant in mice [26]. Thus, it is clear that both IL-6 and TNF-α play an important role in the host against Y. pestis infections, and the ability of Δlpp Δpla double mutant in eliciting high levels of these cytokines signifies the mutant’s potential as a vaccine candidate.
2.5 Nitric oxide production is similar when macrophages are stimulated with WT Y. pestis CO92 or the Δlpp Δpla double mutant
Nitric oxide (NO) production is an essential bacterial killing mechanism employed by the professional macrophages and neutrophils, the two major primary cells of the host innate immune system. NO is produced by the inducible NO synthase (iNOS), which catalyzes the oxidation of L-arginine into NO and L-citrulline. NO has been shown to be important for killing or controlling the proliferation of many intracellular pathogens, such as Leishmania major [55], Toxoplasma gondii [56], and Mycobacterium tuberculosis [57] and the facultatively intracellular Y. pestis [32].
The Griess assay was used (section 4.8) to determine if the inability of the Δlpp Δpla double mutant to survive within macrophages was due to its increased killing by NO. In this assay, nitrite was the readout as opposed to NO, which is an unstable free radical. As shown in Fig. 5B, MH-S macrophages stimulated by infection with either the WT CO92 or its Δlpp Δpla double mutant produced 10 times higher levels of nitrite compared to RAW 264.7 and HMDMs. Surprisingly, all three types of macrophages (RAW 264.7, MH-S, and HMDMs) infected with either the WT CO92 or the Δlpp Δpla double mutant produced similar levels of nitrite in the supernatants after 12 h of infection (Fig. 5B).
In contrast, an earlier study indicated that the pigmentation (pgm) locus deletion mutant strain of Y. pestis stimulated robust production of NO, and, hence, was unable to survive within macrophages that were activated with interferon-γ post infection [32]. This study further showed that the ripA gene encoded on the pgm locus was responsible allowing Y. pestis to combat NO killing [32]. However, the Δlpp Δpla double mutant we used had an intact pgm locus and we also did not activate the macrophages during infection. Since the Δlpp Δpla double mutant was cleared from macrophages quickly (Fig. 1&4) but it still induced similar levels of nitrite as the WT CO92, these data suggested that other mechanisms operating in macrophages might play a major role in Δlpp Δpla double mutant’s clearance. Our future studies would delineate how resting macrophages (resident versus recruited) would differ from IFN-γ activated ones in terms of clearing WT CO92 and its Δlpp Δpla double mutant.
2.6 Zymosan particle uptake is increased in the WT Y. pestis CO92 and the Δlpp Δpla double mutant-infected macrophages versus uninfected cells
Zymosan (synthetic particle) uptake was examined (section 4.9) to delineate whether phagocytic ability of macrophages was altered after infection with either WT CO92 or the Δlpp Δpla double mutant. HMDMs in general had the lowest uptake of the zymosan beads even when the cells were uninfected, however, only approximately 8–9% of the macrophages were positive for zymosan uptake after infection with Y. pestis (Fig. 5C). In comparison, MH-S and RAW 264.7 murine macrophages both exhibited greater zymosan bead uptake (25 to 60%), and this difference was most likely related to the source of macrophages: human versus murine. A similar uptake rate of zymosan beads (~23.6%) was reported for the murine peritoneal macrophages [58].
As expected, all three types of macrophages exhibited increase uptake of beads after infection compared to the uninfected ones. However, the uptake of zymosan particles was statistically significant only for the RAW 264.7 cells when comparing infected versus non-infected controls (p<0.01). Most importantly, there was essentially no difference in zymosan bead uptake across all three types of macrophages when they were infected with either the WT CO92 or its Δlpp Δpla double mutant (Fig. 5C). We could recover similar numbers of WT CO92 and the Δlpp Δpla double mutant bacteria from these infected macrophages after the initial gentamicin treatment (data not shown), indicating that the T3SS was not altered in the Δlpp Δpla double mutant, which was in agreement with our previous report [26].
3 Conclusion and Future Directions
The Δlpp Δpla double mutant represents an excellent candidate to be further developed into a viable live-attenuated plague vaccine. The double mutant was highly attenuated in evoking bubonic and pneumonic plague while retaining its ability to generate strong humoral and cell-mediated immunity, and to maintain innate immune responses similar to that of the WT CO92. In future studies, we aim to determine the optimal dose of the Δlpp Δpla double mutant as well as number of boosters needed which would elicit a long-lasting protective humoral and cell-mediated immune responses when administrated by different routes in mice (e.g., intramuscular versus subcutaneous). Neutrophil activity after infection with the WT CO92 and its double mutant would also be assessed as we observed a robust pro-inflammatory cytokine response that was triggered by WT Y. pestis infection in a mouse model that could recruit PMNs (polymorphonuclear leukocytes). Our previous study showed a gross decrease in histopathological inflammatory differences in the lung tissue when mice were infected with the double mutant (Δlpp Δpla) compared to that of the WT CO92 strain. Therefore, a detailed study on the role of neutrophils and PMNs during infection with Y. pestis and its mutants would be undertaken. We would also investigate the possibility of attenuating this strain further by other gene deletions, to make it safer for use in a diverse human population.
4 Materials and Methods
4.1 Bacterial strains and plasmids
All of the bacterial strains and plasmids used in this study are listed in Table 1. Y. pestis was grown in heart infusion broth (HIB) (Difco, Voigt Global Distribution Inc., Lawrence, KS) at 26 to 28°C with constant agitation (180 rpm). On the solid surface, Y. pestis was grown on either HIB agar or 5% sheep blood agar (SBA) plates (Teknova, Hollister, CA). All of our studies were performed in a CDC-approved Tier-1 select agent facility located in the Galveston National Laboratory within the University of Texas Medical Branch (UTMB).
4.2 Human monocyte isolation and derivation of macrophages
Human buffy coats were obtained separately from three healthy individuals in 10 ml Vacutainer tubes without additive (Becton Dickinson Labware, Franklin Lakes, NJ) from the UTMB blood bank under an Institutional Review Board-approved protocol. EDTA-treated blood from the donors was handled under endotoxin-free conditions; diluted 1:1 with phosphate-buffered saline (PBS), and peripheral blood mononuclear cells (PBMCs) were purified by centrifugation over a Ficoll-sodium diatrizoate solution (Ficoll-Paque™ PLUS, GE Healthcare Bio-sciences AB, Uppsala, Sweden). Monocytes were then purified from PBMCs by positive selection, using human CD14 microbeads and a magnetic column separation system (Miltenyi Biotec, Auburn, CA). Human monocyte-derived macrophages (HMDMs) were generated from purified CD14+ monocytes.
Briefly, monocytes were cultured in RPMI-1640 medium supplemented with 10% heat-inactivated fetal bovine serum (FBS), L-glutamine, HEPES, sodium pyruvate, penicillin-streptomycin, plus granulocyte macrophage-colony stimulating factor (GM-CSF) at 100 ng/ml (Leukine, Genzyme, Cambridge, MA). Monocytes were seeded in 6-or 24-well tissue-culture plates at 106 cells/ml. Adherent HMDMs were obtained at 6 days post culture. Viability of HMDMs was determined by trypan blue staining, and cells were only used when viability exceeded 95%.
4.3 Survival of WT Y. pestis CO92, its mutants, and complemented strains in murine RAW 264.7 bone marrow-derived macrophages, murine MH-S alveolar macrophages, and HMDMs
MH-S and RAW 264.7 macrophages (American Type Culture Collection [ATCC], Manassas, VA) were plated at a concentration of 1 × 106 cells/well in a 12-well tissue culture plate to establish confluent monolayers. MH-S cells were grown in RPMI-1640 supplemented with 10% FBS and 0.5 mM 2-mercaptoethanol, whereas RAW 264.7 cells were grown in Dulbecco modified eagle medium (DMEM) supplemented with 10% FBS. Both of the cell lines were infected with WT CO92, its mutants, or the complemented strains at a multiplicity of infection (MOI) of 1. The infected macrophages were incubated at 37°C with 5% CO2 for 45 min followed by 1 h of treatment with 10 μg/ml gentamicin for MH-S cells and 100 μg/ml gentamicin for RAW 264.7 cells to kill extracellular bacteria. The dose of the antibiotic used was empirically determined based on the host cell sensitivity, and an effective bactericidal range of gentamicin is from 7.5–200 μg/ml [59, 60]. The surviving bacteria inside the macrophages were enumerated immediately after the gentamicin treatment (0 h time point) and subsequently at 4h or at 8 to 24 h by serial dilution and plating on SBA plates [27, 36].
HMDMs were infected with WT CO92 and the Δlpp Δpla double mutant at an MOI of 0.5. The infected macrophages were incubated at 37°C with 5% CO2 for 40 min followed by 1 h of treatment with 10 μg/ml gentamicin to kill extracellular bacteria. The surviving bacteria inside the macrophages were enumerated immediately after the gentamicin treatment (0 h time point) and subsequently at 1, 2, and 4 h by serial dilution and plating [27, 36].
4.4 Visualization of intracellular WT Y. pestis CO92 and its Δlpp Δpla double mutant in HMDMs by confocal microscopy
Post-infection (40 min of infection followed by 1 h of gentamicin treatment) with WT CO92 or its Δlpp Δpla double mutant at an MOI of 0.5, 4% freshly prepared paraformaldehyde and 0.5% Triton X-100 were used to fix and permeabilize the HMDMs. The fixed macrophages were then stained with primary mouse anti-F1 antibodies (1:1,000) (Santa Cruz Biotechnology, Santa Cruz, CA) followed by secondary Alexa Fluor 488 (green) donkey anti-mouse antibodies (Molecular Probes, Carlsbad, CA). Uninfected macrophages were used as negative controls. Mounting medium with DAPI (blue) (Vector Laboratories, Burlingame, CA) and Alexa Fluor 568 (red) phalloidin (Molecular Probes) were used to stain the nucleus and actin, respectively, of macrophages.
4.5 Western blot analysis
Bacterial cultures were grown in 3 ml of HIB at 28°C and 37°C overnight with shaking. The bacteria were harvested, dissolved by boiling in 1x SDS-PAGE sample buffer, and then checked for sterility. Western blot analysis was performed with specific primary anti-Lpp or anti-Pla antibodies (1:1,000 dilution), followed by horseradish peroxidase-labeled goat anti-mouse secondary antibodies (1:5,000 dilution), with anti-DnaK antibodies (Stressgen Biotechnologies Inc, San Diego, CA, 1:250 dilution) being used as an internal loading control [61]. The blots were developed using Clarity Western ECL Substrate (Bio-Rad, Hercules, CA). The antibodies to Lpp and Pla were available in the laboratory.
4.6 Pla protease activity assay
All tested cultures (WT CO92, its mutants, and the complemented strains) were plated on HIB agar plates from −80°C glycerol stocks and incubated at 28°C for 36 h. Single colonies of each culture were then re-plated on fresh HIB agar plates and incubated at 28°C or 37°C for 20–22 h. Bacteria from each plate were suspended and diluted in PBS to obtain absorbance values (OD600) of 0.1 (5 × 107 cfu/ml) and 0.5 (2.5 × 108 cfu/ml) in a spectrophotometer (SmartSpecTm 300, Bio-Rad). For each strain, 50 μl suspensions were added to wells of a black microtiter plate (Costar Corning Inc., Corning, NY) in triplicate. The hexapeptide substrate (5.0 μg/μl) in dimethyl sulfoxide (DMSO) [38], was diluted to a final concentration of 2.5 μg/50 μl, and added to each well containing bacterial cells. Pla activity was then measured in a fluorometric assay (Excitation/Emission 360/460nm) at 37°C on BioTek Synergy HT spectrophotometer (BioTek Instruments Inc., Winooski, VT). The substrate (DABCYL-Arg-Arg-Ile-Asn-Arg-Glu (EDANS)-NH2) was synthesized on Sieber amide resin [38]. The kinetics of substrate cleavage by Pla was measured every 15 min for 2 h. The increase in relative fluorescence units (RFU) as a function of time for WT CO92, its mutants, and the complemented strains was recorded and the kinetics of substrate cleavage plotted using Prism (GraphPad, La Jolla, CA).
4.7 Measurement of cytokines in the supernatants of WT Y. pestis CO92 and the Δlpp Δpla double mutant-infected macrophages
The supernatants from infected macrophages were collected for each cell line at 100–105 min (post-infection and gentamicin treatment), and filtered using 0.1 μm centrifuge tube filters from Costar (Corning Inc.). The host cells were washed before gentamicin treatment and then replenished with the fresh medium. The cytokine levels in undiluted supernatant samples produced by the intracellular bacteria were analyzed by 6-plex Bio-Rad (Bio-Rad, Hercules, CA) Bioplex (IL-6, TNF-α, IL-1β, IL-10, interferon [IFN]-γ, and IL-17) as we previously described [26, 62].
4.8 Measurement of nitric oxide levels in the supernatants of macrophages infected with WT Y. pestis CO92 and its Δlpp Δpla double mutant
Nitric oxide (NO) levels in WT CO92 and its Δlpp Δpla double mutant activated macrophages was determined by measuring the accumulation of nitrite, a stable metabolite of the reaction of NO with oxygen, using the Griess reaction assay kit (Molecular Probes). The supernatants were collected 12 h after infection, and an aliquot (130 μl) of each supernatant was mixed with 20 μl of Griess reagent (0.5% sulfanilamide; 0.05% N-[1-naphthyl] ethylenediamine in 2.5% acetic acid), and 150 μl deionized water. The accumulation of nitrite was then measured spectrophotometrically (SpectraMax M5e, Molecular Devices, Sunnyvale, CA) at 548 nm. The concentration of nitrite was calculated by using a standard curve prepared with sodium nitrite.
4.9 Phagocytosis of zymosan particles by macrophages infected with WT Y. pestis CO92 and its Δlpp Δpla double mutant
Macrophages (RAW 264.7, MH-S, and HMDMs) were infected with WT CO92 and the Δlpp Δpla double mutant as described above. After 1 h of gentamicin treatment, infected host cells were incubated with serum-opsonized synthetic latex beads (1 μm size) at an MOI of 1 (Life Technologies, Carlsbad, CA). The plates were incubated for 1.5 h at 37°C with slow agitation (80 rpm). After incubation with the beads, the macrophages were washed with PBS, also collecting all of the supernatants for floating cells, and spun to collect a pellet at 1,200 rpm for 10 min. Macrophages were then re-suspended in trypan blue, fixed with 10% formalin, and examined for sterility. The samples were read on the LSRII Fortessa (BD Biosciences, San Jose, CA) (Excitation/Emission 580/605nm) and analyzed with FlowJo (Ashland, OR).
4.10 Statistical analyses
Whenever appropriate, one-way analysis of variance (ANOVA) with the Bonferroni correction or Tukey’s post hoc test was employed for data analysis. The p values of ≤0.05 were considered significant. At least 3 biological replicates for each of the experiment were performed.
Highlights.
Δlpp Δpla Y. pestis mutant minimally survived in resting resident and recruited mΦs.
Lpp and Pla operated via different mechanisms to control Y. pestis survival in mΦs.
Δlpp Δpla mutant stimulated innate immune responses comparable to WT Y. pestis.
Δlpp Δpla mutant or its derivatives could serve as live-attenuated vaccines.
Acknowledgments
This research was supported by the NIH/NIAID grant AI064389 awarded to A.K.C. We also acknowledge a UC7 grant (AI070083) which facilitated our research in the Galveston National Laboratory, Galveston, TX. CJ van Lier was supported in part by the T32 Biodefense Training Grant (AI060549). Duraisamy Ponnusamy was supported in part by the James W. McLaughlin postdoctoral fellowship, UTMB.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.(CDC) Centers for Disease Control and Prevention. [Accessed October 12th, 2014];Protecting the American public by ensuring the safe and secure possession, use, and transfer, of select agents and toxins that pose a public health threat. 2008 http://www.cdc.gov/phpr/documents/DSAT_brochure_July2011.pdf.
- 2.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Koerner JF, Layton M, McDade J, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Schoch-Spana M, Tonat K Working Grp Civilian B. Plague as a biological weapon - Medical and public health management. J Amer Med Assoc. 2000;283 (17):2281–2290. doi: 10.1001/jama.283.17.2281. http://www.bt.cdc.gov/agent/plague/consensus.pdf. [DOI] [PubMed] [Google Scholar]
- 3.Reijniers J, Begon M, Ageyev VS, Leirs H. Plague epizootic cycles in Central Asia. Biol Lett. 2014;10(12) doi: 10.1098/rsbl.2014.0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.(WHO) World Health Organization. Epidemic and pandemic alert and response; Interregional meeting on prevention and control of plague; April 1–11; Antananarivo, Madagascar. 2006. http://www.who.int/csr/resources/publications/WHO_HSE_EPR_2008_3w.pdf. [Google Scholar]
- 5.Hinnebusch BJ, Fischer ER, Schwan TG. Evaluation of the role of the Yersinia pestis plasminogen activator and other plasmid-encoded factors in temperature-dependent blockage of the flea. J Infect Dis. 1998;178 (5):1406–1415. doi: 10.1086/314456. [DOI] [PubMed] [Google Scholar]
- 6.Smiley ST. Current challenges in the development of vaccines for pneumonic plague. Exper Rev Vaccines. 2008;7 (2):209–221. doi: 10.1586/14760584.7.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui Y, Yang X, Xiao X, Anisimov AP, Li D, Yan Y, Zhou D, Rajerison M, Carniel E, Achtman M, Yang R, Song Y. Genetic variations of live attenuated plague vaccine strains (Yersinia pestis EV76 lineage) during laboratory passages in different countries. Infect Genet and Evol. 2014;26:172–179. doi: 10.1016/j.meegid.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 8.(CDC) Centers for Disease Control and Prevention. Fatal laboratory-acquired infection with an attenuated Yersinia pestis Strain--Chicago, Illinois, 2009. MMWR Morb Mortal Wkly Rep. 2011;60 (7):201–205. [PubMed] [Google Scholar]
- 9.Williamson ED, Packer PJ, Waters EL, Simpson AJ, Dyer D, Hartings J, Twenhafel N, Pitt MLM. Recombinant (F1+V) vaccine protects cynomolgus macaques against pneumonic plague. Vaccine. 2011;29 (29–30):4771–4777. doi: 10.1016/j.vaccine.2011.04.084. [DOI] [PubMed] [Google Scholar]
- 10.Williamson ED, Flick-Smith HC, LeButt C, Rowland CA, Jones SM, Waters EL, Gwyther RJ, Miller J, Packer PJ, Irving M. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infection and Immunity. 2005;73 (6):3598–3608. doi: 10.1128/IAI.73.6.3598-3608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smiley ST. Cell-mediated Defense against Yersinia pestis infection. In: Perry RD, Fetherston JD, editors. Genus Yersinia: from Genomics to Function. Vol. 603. 2007. pp. 376–386. [DOI] [PubMed] [Google Scholar]
- 12.Lukaszewski RA, Kenny DJ, Taylor R, Rees DG, Hartley MG, Oyston PC. Pathogenesis of Yersinia pestis infection in BALB/c mice: effects on host macrophages and neutrophils. Infect Immun. 2005;73 (11):7142–7150. doi: 10.1128/IAI.73.11.7142-7150.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spinner JL, Winfree S, Starr T, Shannon JG, Nair V, Steele-Mortimer O, Hinnebusch BJ. Yersinia pestis survival and replication within human neutrophil phagosomes and uptake of infected neutrophils by macrophages. J Leukoc Biol. 2014;95 (3):389–398. doi: 10.1189/jlb.1112551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamamoto T, Hanawa T, Ogata S, Kamiya S. Identification and characterization of the Yersinia enterocolitica gsrA gene, which protectively responds to intracellular stress induced by macrophage phagocytosis and to extracellular environmental stress. Infect Immun. 1996;64 (8):2980–2987. doi: 10.1128/iai.64.8.2980-2987.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perry RD, Fetherston JD. Yersinia pestis etiologic agent of plague. Clin Microbiol Rev. 1997;10 (1):35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pujol C, Bliska JB. The ability to replicate in macrophages is conserved between Yersinia pestis and Yersinia pseudotuberculosis. Infect Immun. 2003;71 (10):5892–5899. doi: 10.1128/IAI.71.10.5892-5899.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peters KN, Dhariwala MO, Hughes Hanks JM, Brown CR, Anderson DM. Early apoptosis of macrophages modulated by injection of Yersinia pestis YopK promotes progression of primary pneumonic plague. PLoS Pathog. 2013;9 (4):e1003324. doi: 10.1371/journal.ppat.1003324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pechous RD, Sivaraman V, Price PA, Stasulli NM, Goldman WE. Early host cell targets of Yersinia pestis during primary pneumonic plague. PLoS Pathog. 2013;9 (10):e1003679. doi: 10.1371/journal.ppat.1003679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sebbane F, Lemaître N, Sturdevant DE, Rebeil R, Virtaneva K, Porcella SF, Hinnebusch BJ. Adaptive response of Yersinia pestis to extracellular effectors of innate immunity during bubonic plague. Proc Natl Acad Sci U S A. 2006;103 (31):11766–11771. doi: 10.1073/pnas.0601182103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amedei A, Niccolai E, Marino L, D’Elios MM. Role of immune response in Yersinia pestis infection. J Infect Dev Ctries. 2011;5 (9):628–639. doi: 10.3855/jidc.1999. [DOI] [PubMed] [Google Scholar]
- 21.Gennery AR, Cant AJ. Applied physiology: immune competence. Curr Paediatrics. 2001;11:458–464. doi: 10.1054/cupe.2001.0235. [DOI] [Google Scholar]
- 22.Kummer LW, Szaba FM, Parent MA, Adamovicz JJ, Hill J, Johnson LL, Smiley ST. Antibodies and cytokines independently protect against pneumonic plague. Vaccine. 2008;26 (52):6901–6907. doi: 10.1016/j.vaccine.2008.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janssen WJ, Barthel L, Muldrow A, Oberley-Deegan RE, Kearns MT, Jakubzick C, Henson PM. Fas determines differential fates of resident and recruited macrophages during resolution of acute lung injury. Am J Respir Crit Care Med. 2011;184 (5):547–560. doi: 10.1164/rccm.201011-1891OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernando MR, Reyes JL, Iannuzzi J, Leung G, McKay DM. The pro-inflammatory cytokine, interleukin-6, enhances the polarization of alternatively activated macrophages. PLoS One. 2014;9 (4):e94188. doi: 10.1371/journal.pone.0094188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bayer C, Varani S, Wang L, Walther P, Zhou S, Straschewski S, Bachem M, Söderberg-Naucler C, Mertens T, Frascaroli G. Human cytomegalovirus infection of M1 and M2 macrophages triggers inflammation and autologous T-cell proliferation. J Virol. 2013;87 (1):67–79. doi: 10.1128/JVI.01585-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Lier CJ, Sha J, Kirtley ML, Cao A, Tiner BL, Erova TE, Cong Y, Kozlova EV, Popov VL, Baze WB, Chopra AK. Deletion of Braun Lipoprotein and Plasminogen-Activating Protease-Encoding Genes Attenuates Yersinia pestis in Mouse Models of Bubonic and Pneumonic Plague. Infection and Immunity. 2014;82 (6):2485–2503. doi: 10.1128/IAI.01595-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sha J, Agar SL, Baze WB, Olano JP, Fadl AA, Erova TE, Wang S, Foltz SM, Suarez G, Motin VL, Chauhan S, Klimpel GR, Peterson JW, Chopra AK. Braun lipoprotein (Lpp) contributes to virulence of yersiniae: potential role of Lpp in inducing bubonic and pneumonic plague. Infect Immun. 2008;76 (4):1390–1409. doi: 10.1128/IAI.01529-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lathem WW, Price PA, Miller VL, Goldman WE. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science. 2007;315 (5811):509–513. doi: 10.1126/science.1137195. [DOI] [PubMed] [Google Scholar]
- 29.Galindo CL, Moen ST, Kozlova EV, Sha J, Garner HR, Agar SL, Chopra AK. Comparative analyses of transcriptional profiles in mouse organs using a pneumonic plague model after infection with wild-type Yersinia pestis CO92 and its Braun lipoprotein mutant. Comp Funct Genomics. 2009;2009:914762. doi: 10.1155/2009/914762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Straley SC, Harmon PA. Growth in mouse peritoneal macrophages of Yersinia pestis lacking established virulence determinants. Infect Immun. 1984;45 (3):649–654. doi: 10.1128/iai.45.3.649-654.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Straley SC, Harmon PA. Yersinia pestis grows within phagolysosomes in mouse peritoneal macrophages. Infect Immun. 1984;45 (3):655–659. doi: 10.1128/iai.45.3.655-659.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pujol C, Grabenstein JP, Perry RD, Bliska JB. Replication of Yersinia pestis in interferon gamma-activated macrophages requires ripA, a gene encoded in the pigmentation locus. Proc Natl Acad Sci U S A. 2005;102 (36):12909–12914. doi: 10.1073/pnas.0502849102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu G, Xia XP, Gong SL, Zhao Y. The macrophage heterogeneity: difference between mouse peritoneal exudate and splenic F4/80+ macrophages. J Cell Physiol. 2006;209 (2):341–352. doi: 10.1002/jcp.20732. [DOI] [PubMed] [Google Scholar]
- 34.Laskin DL, Weinberger B, Laskin JD. Functional heterogeneity in liver and lung macrophages. J Leuko Biol. 2001;70 (2):163–170. [PubMed] [Google Scholar]
- 35.Berghaus LJ, Moore JN, Hurley DJ, Vandenplas ML, Fortes BP, Wolfert MA, Boons GJ. Innate immune responses of primary murine macrophage-lineage cells and RAW 264.7 cells to ligands of Toll-like receptors 2, 3, and 4. Comp Immunol Microbiol Infect Dis. 2010;33 (5):443–454. doi: 10.1016/j.cimid.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agar SL, Sha J, Baze WB, Erova TE, Foltz SM, Suarez G, Wang S, Chopra AK. Deletion of Braun lipoprotein gene (lpp) and curing of plasmid pPCP1 dramatically alter the virulence of Yersinia pestis CO92 in a mouse model of pneumonic plague. Microbiology. 2009;155 (Pt 10):3247–3259. doi: 10.1099/mic.0.029124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eddy JL, Gielda LM, Caulfield AJ, Rangel SM, Lathem WW. Production of outer membrane vesicles by the plague pathogen Yersinia pestis. PLoS One. 2014;9 (9):e107002. doi: 10.1371/journal.pone.0107002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Agarkov A, Chauhan S, Lory PJ, Gilbertson SR, Motin VL. Substrate specificity and screening of the integral membrane protease Pla. Bioorg Med Chem Lett. 2008;18 (1):427–431. doi: 10.1016/j.bmcl.2007.09.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rebeil R, Ernst RK, Jarrett CO, Adams KN, Miller SI, Hinnebusch BJ. Characterization of late acyltransferase genes of Yersinia pestis and their role in temperature-dependent lipid A variation. J Bacteriol. 2006;188 (4):1381–1388. doi: 10.1128/JB.188.4.1381-1388.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kolodziejek AM, Schnider DR, Rohde HN, Wojtowicz AJ, Bohach GA, Minnich SA, Hovde CJ. Outer Membrane Protein X (Ail) Contributes to Yersinia pestis virulence in pneumonic plague and its activity is dependent on the lipopolysaccharide core length. Infect Immun. 2010;78(12):5233–43. doi: 10.1128/IAI.00783-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rajanna C, Revazishvili T, Rashid MH, Chubinidze S, Bakanidze L, Tsanava S, Imnadze P, Bishop-Lilly KA, Sozhamannan S, Gibbons HS, Morris JG, Sulakvelidze A. Characterization of pPCP1 Plasmids in Yersinia pestis strains isolated from the former Soviet Union. Inter J Microbiol. 2010;2010:760819. doi: 10.1155/2010/760819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Galindo CL, Sha J, Moen ST, Agar SL, Kirtley ML, Foltz SM, McIver LJ, Kozlova EV, Garner HR, Chopra AK. Comparative global gene expression profiles of wild-type Yersinia pestis CO92 and its Braun lipoprotein mutant at flea and human body temperatures. Comp Funct Genomics. 2010:342168. doi: 10.1155/2010/342168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mecsas J, Rouviere PE, Erickson JW, Donohue TJ, Gross CA. The activity of sigma E, an Escherichia coli heat-inducible sigma-factor, is modulated by expression of outer membrane proteins. Genes Dev. 1993;7 (12B):2618–2628. doi: 10.1101/gad.7.12b.2618. [DOI] [PubMed] [Google Scholar]
- 44.Strauch KL, Johnson K, Beckwith J. Characterization of degP, a gene required for proteolysis in the cell envelope and essential for growth of Escherichia coli at high temperature. J Bacteriol. 1989;171 (5):2689–2696. doi: 10.1128/jb.171.5.2689-2696.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lipinska B, Zylicz M, Georgopoulos C. The HtrA (DegP) protein, essential for Escherichia coli survival at high temperatures, is an endopeptidase. J Bacteriol. 1990;172 (4):1791–1797. doi: 10.1128/jb.172.4.1791-1797.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yamamoto T, Hanawa T, Ogata S, Kamiya S. The Yersinia enterocolitica GsrA stress protein, involved in intracellular survival, is induced by macrophage phagocytosis. Infect Immun. 1997;65 (6):2190–2196. doi: 10.1128/iai.65.6.2190-2196.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fayet O, Ziegelhoffer T, Georgopoulos C. The groES and groEL heat shock gene products of Escherichia coli are essential for bacterial growth at all temperatures. J Bacteriol. 1989;171 (3):1379–1385. doi: 10.1128/jb.171.3.1379-1385.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bukau B, Walker GC. Cellular defects caused by deletion of the Escherichia coli dnaK gene indicate roles for heat shock protein in normal metabolism. J Bacteriol. 1989;171 (5):2337–2346. doi: 10.1128/jb.171.5.2337-2346.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ellis RJ. The molecular chaperone concept. Semin Cell Biol. 1990;1 (1):1–9. [PubMed] [Google Scholar]
- 50.Sebbane F, Jarrett CO, Gardner D, Long D, Hinnebusch BJ. Role of the Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proc Natl Acad Sci U S A. 2006;103 (14):5526–5530. doi: 10.1073/pnas.0509544103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Korhonen TK, Haiko J, Laakkonen L, Jarvinen HM, Westerlund-Wikstrom B. Fibrinolytic and coagulative activities of Yersinia pestis. Front Cell Infect Microbiol. 2013;26(3):35. doi: 10.3389/fcimb.2013.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martin CA, Dorf ME. Differential regulation of interleukin-6, macrophage inflammatory protein-1, and JE/MCP-1 cytokine expression in macrophage cell lines. Cell Immunol. 1991;135 (1):245–258. doi: 10.1016/0008-8749(91)90269-h. [DOI] [PubMed] [Google Scholar]
- 53.Chomarat P, Banchereau J, Davoust J, Palucka AK. IL-6 switches the differentiation of monocytes from dendritic cells to macrophages. Nat Immunol. 2000;1 (6):510–514. doi: 10.1038/82763. [DOI] [PubMed] [Google Scholar]
- 54.Cassese G, Arce S, Hauser AE, Lehnert K, Moewes B, Mostarac M, Muehlinghaus G, Szyska M, Radbruch A, Manz RA. Plasma cell survival is mediated by synergistic effects of cytokines and adhesion-dependent signals. J Immunol. 2003;171(4):1684–1690. doi: 10.4049/jimmunol.171.4.1684. [DOI] [PubMed] [Google Scholar]
- 55.Liew FY, Millott S, Parkinson C, Palmer RM, Moncada S. Macrophage killing of Leishmania parasite in vivo is mediated by nitric oxide from L-arginine. J Immunol. 1990;144 (12):4794–4797. [PubMed] [Google Scholar]
- 56.Scharton-Kersten TM, Yap G, Magram J, Sher A. Inducible nitric oxide is essential for host control of persistent but not acute infection with the intracellular pathogen Toxoplasma gondii. J Exp Med. 1997;185 (7):1261–1273. doi: 10.1084/jem.185.7.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.MacMicking JD, North RJ, LaCourse R, Mudgett JS, Shah SK, Nathan CF. Identification of nitric oxide synthase as a protective locus against tuberculosis. Proc Natl Acad Sci U S A. 1997;94 (10):5243–5248. doi: 10.1073/pnas.94.10.5243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carvalho MD, Tobias VE, Vendrame CM, Shimabukuro AF, Gidlund M, Quintão EC. Zymosan phagocytosis by mouse peritoneal macrophages is increased by apoHDL- and not by intact HDL-covered particles. Braz J Med Biol Res. 2000;33 (3):313–316. doi: 10.1590/s0100-879x2000000300009. [DOI] [PubMed] [Google Scholar]
- 59.Wendte JM, Ponnusamy D, Reiber D, Blair JL, Clinkenbeard KD. In vitro efficacy of antibiotics commonly used to treat human plague against intracellular Yersinia pestis. Antimicrob Agents Chemother. 2011;55 (8):3752–3757. doi: 10.1128/AAC.01481-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Galimand M, Carniel E, Courvalin P. Resistance of Yersinia pestis to antimicrobial agents. Antimicrob Agents Chemother. 2006;50 (10):3233–3236. doi: 10.1128/AAC.00306-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schiano CA, Koo JT, Schipma MJ, Caulfield AJ, Jafari N, Lathem WW. Genome-wide analysis of small RNAs expressed by Yersinia pestis identifies a regulator of the Yop-Ysc type III secretion system. J Bacteriol. 2014;196 (9):1659–1670. doi: 10.1128/JB.01456-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sha J, Kirtley ML, van Lier CJ, Wang S, Erova TE, Kozlova EV, Cao A, Cong Y, Fitts EC, Rosenzweig JA, Chopra AK. Deletion of the Braun lipoprotein-encoding gene and altering the function of lipopolysaccharide attenuate the plague bacterium. Infect Immun. 2013;81 (3):815–828. doi: 10.1128/IAI.01067-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Doll JM, Zeitz PS, Ettestad P, Bucholtz AL, Davis T, Gage K. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am J Trop Med Hyg. 1994;51 (1):109–114. doi: 10.4269/ajtmh.1994.51.109. [DOI] [PubMed] [Google Scholar]
- 64.Parkhill J, Wren BW, Thomson NR, Titball RW, Holden MT, Prentice MB, Sebaihia M, James KD, Churcher C, Mungall KL, Baker S, Basham D, Bentley SD, Brooks K, Cerdeño-Tárraga AM, Chillingworth T, Cronin A, Davies RM, Davis P, Dougan G, Feltwell T, Hamlin N, Holroyd S, Jagels K, Karlyshev AV, Leather S, Moule S, Oyston PC, Quail M, Rutherford K, Simmonds M, Skelton J, Stevens K, Whitehead S, Barrell BG. Genome sequence of Yersinia pestis, the causative agent of plague. Nature. 2001;413 (6855):523–527. doi: 10.1038/35097083. [DOI] [PubMed] [Google Scholar]