Abstract
Objective
To determine if high-activity older adults are adversely affected by distal radius malunion.
Design
Cross-sectional study.
Setting
Hand clinics at a tertiary institution.
Participants
96 patients ≥60 years old at time of fracture evaluated at least 1 year following distal radius fracture.
Intervention
Physical Activity Scale of the Elderly (PASE) scores stratified participants into high- and low-activity groups. Malunions were defined radiographically by change of ≥20° of lateral tilt, ≥15° radial inclination, ≥4 mm of ulnar variance, or ≥4 mm intra-articular gap or step-off, compared to the uninjured wrist.
Main Outcome Measure
Patient-rated disability of the upper-extremity was measured by the QuickDASH and Visual Analog Scales (VAS) for pain/function. Strength and motion measurements objectively quantified wrist function.
Results
High-activity participants with a distal radius malunion were compared to high-activity participants with well-aligned fractures. There was no significant difference in QuickDASH scores, VAS function, strength, and wrist motion despite statistically, but not clinically relevant, increases in VAS pain scores (difference 0.5, p=0.04) between the groups. Neither PASE score (β= 0.001, 95%CI: −0.002 to 0.004) nor malunion (β=0.133, 95%CI: −0.26 to 0.52) predicted QuickDASH scores in regression modeling after accounting for age, sex, and treatment. Operative management failed to improve outcomes and resulted in decreased grip strength (p=0.05) and more frequent complications (26% vs 7%, p=0.01) when compared to nonoperatively management.
Conclusion
Even among highly active older adults, distal radius malunion does not impact functional outcomes. Judicious use of operative management is warranted provided heightened complication rates.
Keywords: distal radius fracture, Malunion, elderly, activity level, physiological age, older adults
Introduction
Approximately 250,000 distal radius fractures (DRF) occur annually among adults ≥65 years old in the United States,1 making it the second most common fracture among Medicare participants.2,3 With this incidence projected to increase as the population ages, it is critical to determine optimal treatment for patients ≥60 years old.4 Currently, it is unclear if malunion negatively impacts outcomes following DRF in older adults.5,6,7,8,9,10,11 Prior studies on this topic have categorized older adults by chronologic age without considering patient activity level. This has prompted investigators to suggest that patient activity level may be a better predictor of the impact of distal radius malunion.4,6,7
The purpose of this study was to determine if activity level in patients ≥65 years old affected upper-extremity disability after distal radius malunion. Our secondary aim was to determine if patient demographics or treatment type (operative, nonoperative) could predict patient-rated disability. We hypothesized that, in contrast to sedentary individuals, highly active older adults with distal radius malunions would demonstrate worse functional outcome than those with well-aligned fractures.
Patients and Methods
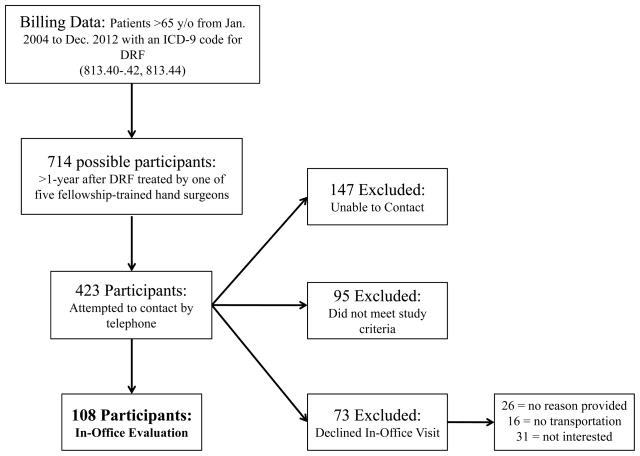
This cross-sectional study was approved by our institutional review board. Billing records of 5 fellowship-trained hand surgeons were queried to identify patients treated for a DRF (ICD 9: 813.40–.42, 813.44) between January 2004 and December 2012, irrespective of treatment method. For study inclusion patients were required to be both ≥60 years old at time of injury and ≥65 years old at time of this study We included patients with a unilateral DRF and minimum follow-up of one year. We attempted to contact 423 patients by telephone before reaching our target sample size determined through an a priori sample size analysis. Each patient was verbally screened for exclusion criteria: bilateral DRF, history of other upper-extremity musculoskeletal surgery or injury, and history of other diagnosis or neurologic impairment that could affect upper-extremity function or cognition. Among those contacted by telephone, 108 patients met the study criteria and volunteered to a study-related office visit; 73 declined an in-office evaluation (Figure 1).
Figure 1.
Flow Diagram of Patient Enrollment and Participation
All 108 participants completed a one-time, standardized in-person evaluation by a member of the research team (JGS or GNN). We collected data to characterize participants (demographics, Short Form-12, treatment method, fracture type at initial presentation) and their activity level (Physical Activity Scale of the Elderly [PASE]).12,13 The validated PASE questionnaire quantifies the amount and level of activity in patients ≥65 years old. Scores range from 0 to ≥400 (higher score indicate higher activity level). Participants were also asked, “What activities can you no longer perform because of the injury to your wrist?” to determine if their DRF caused a decrease in activity level. Our primary outcome was patient-rated upper extremity disability (QuickDASH, VAS-pain & function on scales of 0–10).14,15,16 After completing patient-rated outcome questionnaires, participants underwent a physical examination of bilateral wrists: palpation for tenderness, standardized goniometric measurements of wrist motion and forearm rotation. Maximum grip strength was measured with a dynamometer across five grip width settings. Pinch strength was measured by mean thumb-index pinch from three consecutive attempts. Neither strength measurement was adjusted for limb dominance. Finally, standardized posteroanterior and lateral radiographic images of both wrists were obtained.16 Radiographic imaging was performed last to minimize measurement bias imparted by the examiners based on their knowledge of fracture status (malunion or well-aligned).
Two fellowship-trained hand surgeons (RPC and DAO) reviewed all radiographs. Fractures were considered malunions if the injured wrist differed by ≥20° of dorsal tilt, ≥15° radial inclination, ≥4 mm of ulnar variance, or ≥4 mm intra-articular gap or step-off (measured by PA and lateral radial width) when compared to participants’ uninjured wrist.17 These parameters were chosen for consistency with AAOS guidelines for treatment of DRF based on dorsal tilt, radius shortening,18 and loss of radial inclination after modification to account for change from the contralateral side.19 Intra-articular gap and step-off was increased from 2 mm since these intra-articular changes are more subtle after fracture healing. Participants with radiographs meeting one or more of the above criteria were categorized as having a malunion. Inter-rater reliability measured by Cohen’s Kappa statistic was κ=.73 indicating a high-level of agreement between reviewers in classifying malunions. The original radiographic measurements were considered discordant if a patient was diagnosed with a malunion by only one reviewer or if radiographic measurements differed between reviewers by ≥3 mm or ≥4°. These measurements were re-analyzed by each reviewer independently; any remaining disagreement was resolved in conference based on consensus. Final length measurements were calibrated for magnification using a standardized radiographic marker. The reviewers were blinded to all patient data except surgical management due to radiographic evidence of operative fixation.
Electronic records (EMR) were reviewed to determine the incidence of complications. Complications included complex regional pain syndrome, skin damage resulting from immobilization, or any condition prompting recommendation for secondary surgical intervention (eg. carpal tunnel syndrome, tendonitis due to hardware).
Of the 108 participants that returned for an office-visit, 6 were excluded due to upper extremity injury or disease missed during telephone screening. Six patients were <60 years old at time of fracture and were excluded from the analysis. The remaining 96 participants contributed data for analysis (Table 1). Mean time since fracture was 42 months (range 13–100). Forty-eight fractures (50%) were classified as malunions.
Table 1.
Patient Demographics and Outcome Measures*
| Overall (96) | High Active (38) | Low Active (58) | Malunion (48) | Well-aligned (48) | |
|---|---|---|---|---|---|
|
| |||||
| Age | 72 (5) | 70 (5) | 73 (5) | 72 (6) | 72 (5) |
| Gender (Female)† | 75 (78%) | 31 (82%) | 44 (76%) | 34 (71%) | 41 (85%) |
| Fracture to Dominant Wrist | 41 (43%) | 18 (47%) | 23 (40%) | 21 (44%) | 20 (42%) |
| Surgical Management† | 53 (52%) | 16 (42%) | 33 (57%) | 24 (50%) | 25 (52%) |
| PASE score | 146 (81) | 221 (70) | 96 (37) | 132 (79) | 159 (81) |
| Patient Rated Outcomes: | |||||
| QuickDASH score | 11.3 (12.3) | 7.5 (8.8) | 13.7 (13.6) | 13.5 (13.3) | 9.0 (10.9) |
| SF12MCS | 47.7 (10.0) | 51.6 (7.5) | 45.1 (10.7) | 46.9 (9.9) | 48.4 (10.2) |
| SF12PCS | 54.7 (7.0) | 55.2 (6.0) | 54.4 (7.6) | 54.0 (8.0) | 55.4 (5.8) |
| VAS pain (0–10) | 1.1 (1.9) | 0.8 (1.5) | 1.2 (2.1) | 1.5 (2.1) | 0.6 (1.6) |
| VAS function (0–10) | 1.3 (1.6) | 1.1 (1.3) | 1.4 (1.8) | 1.4 (1.7) | 1.1 (1.6) |
| Strength: | |||||
| Injured – Non Injured Grip Strength (kg-force) | −4.6 (12.5) | −2.4 (11.2) | −6.0 (13.1) | −5.6 (14.0) | −3.6 (10.8) |
| Injured - Non Injured Pinch Strength (kg-force) | −0.25 (2.5) | 0.28 (2.3) | −0.61 (2.6) | −0.26 (2.7) | −0.24 (2.4) |
| Range Of Motion: | |||||
| Injured - Non Injured Prono-Supination | −9 (17) | −8 (18) | −10 (16) | −12 (16) | −6 (16) |
| Injured - Non Injured Flexion-Extension | −10 (18) | −7 (16) | −12 (19) | −13 (19) | −7 (17) |
| Injured - Non Injured Radial-Ulnar Deviation | −3 (10) | −2 (8) | −4 (10) | −5 (10) | −1 (9) |
Mean (SD)
n (%)
Statistical Analysis
Following data collection, participants were categorized into two groups according to radiographic outcome (malunited or well-aligned) using the calibrated radiographic measurements (mean of two reviewers). For univariate contrasts, participants were divided into high- (PASE≥150) and low-activity groups (PASE<150) based on the mean PASE score.
To determine if high and low-activity patients were differentially affected by radius malunion we first compared patient-rated (QuickDASH, VAS pain, VAS function) and objective outcome measures (grip/pinch strength, wrist ROM as difference from uninjured wrist) in high-activity participants with malunions against the outcomes of high-activity participants with well-aligned DRF. Similar analysis was completed on the subgroup of low-activity participants (malunion versus well-aligned).
Fractures displaced at initial presentation (n=67) were selected for analysis to determine if objective or subjective patient outcomes differed according to treatment type (nonoperative vs operative). All comparisons were conducted using the two-tailed independent t-test for normal data and the Mann-Whitney U test for non-parametric data.
We constructed a linear regression model to determine predictors of upper-extremity disability (QuickDASH). The QuickDASH scores were right-skewed; natural log (ln QuickDASH) was used to normalize the data. We entered variables in two blocks. Our first block force entered our two primary independent variables, PASE score (continuous) and presence of malunion (yes/no). The second block used forward entry to include age, sex, management type (operative/nonoperative) and additional variables approaching significant (p<0.10) associations with the natural logarithm (ln) of QuickDASH (potential variables: SF-12 MCS, SF-12 PCS scores, difference in bilateral grip strength, pinch strength, prono-supination, flexion-extension, and radio-ulnar deviation.)
Due to our cross-sectional design, we performed additional analysis assessing for potential sampling bias and bias due to reverse-causality (resulting in patient misclassification). No participant in our population undergoing surgical management had previously failed conservative therapy. To evaluate if this was due to sampling bias, we conducted a separate review of the EMR of all patients ≥65 years old who underwent surgery for DRF at our institution between January of 2007 and June of 2012. From this data, we determined the incidence of revision surgery after failed conservative treatment in the population from which our study sample was drawn. Second, to investigate potential bias from DRF malunions resulting in decreased activity levels and therefore leading to misclassification of previously highly active patients into the low-activity group (reverse-causality), we re-categorized participants providing a positive answer to the question “What activities can you no longer perform because of the injury to your wrist?” Seven participants noted activities they could no longer perform; two were already classified as high-activity and five were classified as low-activity participants. The low-activity participants were re-categorized into the high-activity group (given mean PASE score for regression analysis). We then conducted a sensitivity analysis repeating our univariate analysis and regression analysis using the re-categorized patients.
Based on a conservative minimal clinically important difference (MCID) of 12 points on the QuickDASH survey and a standard deviation of 12 points20, a priori sample size estimation (alpha = 0.05 and 80% power) using a Mann-Whitney U determined a need to recruit a minimum of 18 participants per group. A target of 100 participants with a predicted malunion rate of 40% was set to ensure enough participants with malunions for stratification to high- and low-activity groups (i.e. 20 per group).
Results
When comparing high-activity participants with or without malunion, there was no difference in QuickDASH, VAS function, strength, or range of motion between participants (Table 2). There was a statistically significant, but not clinically relevant, higher VAS pain score (0.0 vs 0.5, p=0.04) in the malunion group.21,22 After our sensitivity analysis, this difference was no longer statistically significant (p=0.21) with no change in significance of any other outcome measures.
Table 2.
Comparison of malunions and unions according to activity level
| HIGH ACTIVE | LOW ACTIVE | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Well-aligned (23) | Malunion (15) | p-value | Well-aligned (25) | Malunion (33) | p-value | |
|
| ||||||
| Age* | 71 (5) | 68 (4) | 0.08 | 73 (4) | 74 (6) | 0.28 |
| Sex (Females)† | 22 (96%) | 9 (60%) | 0.01 | 19 (76%) | 25 (76%) | 1 |
| Surgical Management† | 11 (48%) | 5 (33%) | 0.51 | 14 (56%) | 19 (58%) | 1 |
| Patient Rated Outcomes: | ||||||
| QuickDASH | 4.5 | 4.5 | 0.86 | 6.8 | 11.3 | 0.21 |
| VAS Pain Score (0–10 cm) | 0.0 | 0.5 | 0.04 | 0.0 | 0.5 | 0.08 |
| VAS Function Score (0–10 cm) | 0.0 | 0.6 | 0.25 | 0.1 | 0.0 | 0.79 |
| Strength: | ||||||
| Injured - Non Injured Grip (kg-force)‡ | −0.9 (8.7) | −4.5 (14.3) | 0.40 | −6.0 | −4.0 | 0.88 |
| Injured - Non Injured Pinch (kg force)* | 0.0 (2.0) | 0.71 (2.7) | 0.36 | −0.47 (2.8) | −0.72 (2.6) | 0.72 |
| Range of Motion: | ||||||
| Injured - Non Injured Prono-Supination | −5 | −8 | 0.60 | −5 | −10 | 0.04 |
| Injured - Non Injured Flexion-Extension* | −6 (17) | −9 (14) | 0.60 | −8 (17) | −14 (20) | 0.26 |
| Injured - Non Injured Radial-Ulnar Deviation | 0 | −7 | 0.38 | 0 | −3 | 0.10 |
Normal Data for High and Low Active: mean (sd)
Chi-squared tests
Normal Data for High Active group only
There was no difference in patient-rated outcomes among low-activity participants with and without malunion (Table 2). There was, however, a statistically significant decrease in the prono-supination arc in participants with malunions, though the difference (10° loss vs 5° loss) is not believed to be clinically relevant and could be due to variation in measuring.
Among study participants with fractures displaced initially (Table 3), patients that underwent surgery were more likely to have decreased grip strength (p=0.05) than those who were treated nonoperatively (Table 4). Complications were more frequent in the surgical group (p=0.01) (Table 5).
Table 3.
Baseline data on displaced fracture characteristics according to treatment type*
| Operative (n=42)† | Nonoperative (n=21)† | |
|---|---|---|
|
| ||
| AO Type A | 17/41 (41%) | 8 (38%) |
| AO Types B/C | 24/41 (59%) | 13 (62%) |
| Fall From Standing | 33/39 (85%) | 16/19 (84%) |
| High Energy Injury | 6/39 (15%) | 3/19 (16%) |
| Dominant Extremity Affected | 22 (52%) | 11/20 (55%) |
| Patient Age | 72 ± 5 | 72 ± 5 |
| Female | 36 (86%) | 18 (86%) |
No significant difference noted between groups on any factor
No missing data in cells without fractions
Table 4.
Outcomes of displaced fractures treated operatively vs nonoperatively*
| Displaced Distal Radius Fractures
|
|||
|---|---|---|---|
| Operative (n=42) | Nonoperative (n=21) | p-value | |
|
| |||
| Malunion† | 19 (45%) | 10 (48%) | 1.00 |
| Fracture to Dominant Wrist | 22 (52%) | 11 (55%) | 1.00 |
| Patient Rated Outcomes:‡ | |||
| QuickDASH | 6.8 | 6.8 | 0.89 |
| VAS Pain Score (0–10 cm) | 0.2 | 0.2 | 0.67 |
| VAS Function Score (0–10 cm) | 1.2 | 0.4 | 0.67 |
| Strength: | |||
| Injured - Non Injured Grip Strength (kg-force) | −6.0 (13.1) | 0.6 (11.5) | 0.05 |
| Injured - Non Injured Pinch Strength (kg-force) | 0.1 (2.4) | −0.1 (2.9) | 0.83 |
| Range of Motion: | |||
| Injured – Non Injured Prono-Supination | −13 (15) | −6 (14) | 0.11 |
| Injured - Non Injured Flexion-Extension | −14 (19) | −9 (15) | 0.31 |
| Injured - Non Injured Radial-Ulnar Deviation | −5 (11) | −1 (8) | 0.10 |
mean (sd)
Chi-squared tests
Non-normal data (median values used)
Table 5.
Distribution of complications according to treatment group.
| OPERATIVE (N=53) | Number | NONOPERATIVE (N=43) | Number |
|---|---|---|---|
| Extensor rupture | 2 | Skin irritation requiring cast change | 1 |
| Flexor tendon adhesions requiring tenolysis | 1 | Ulnar wrist pain requiring Darrach | 1 |
| Carpal tunnel syndrome requiring release | 4 | Radius osteotomy | 1 |
| Tendonitis requiring hardware removal | 2 | ||
| Complex regional pain syndrome | 3 | ||
| Lost reduction requiring revision fixation | 2 | ||
| TOTAL | 14 (26%) | 3 (7%) |
For all participants with malunions, those that underwent surgery had decreased prono-supination arc (decrease of 14° vs. 6°; p=0.01) and radial-ulnar deviation (decrease of 10° vs. increase of 1°; p=0.02) compared to those who were treated nonoperatively. There were no differences in QuickDASH, VAS scores, grip strength, or flexion-extension arc between patients with malunions following operative versus nonoperative management.
Univariate correlation analysis with QuickDASH revealed that the difference in flexion-extension arc, SF12 MCS, and SF12 PCS approached statistical significance (p≤0.10). These variables were included into the regression model with age, sex, treatment, malunion, and PASE score. The overall model was significant (p=0.006) explaining 36% of the variance in ln QuickDASH scores. Neither malunion (β=0.133, 95%CI: −0.26 to 0.52) nor PASE score (β= 0.001, 95%CI: −0.002 to 0.004) significantly predicted the ln QuickDASH scores. A decrease both in SF-12 MCS (β= −0.07, 95%CI: −0.09 to −0.05) and flexion-extension arc in the injured hand (β= −0.02, 95%CI: −0.03 to −0.005) significantly predicted more disability (higher ln QuickDASH scores). In the final model, age, sex, treatment method, and SF-12 PCS were not significant predictors of the ln QuickDASH scores. After conducting a sensitivity analysis, both PASE score and presence of malunion remained non-significant.
During the review assessing potential sampling bias, we identified 106 patients ≥65 years of age who underwent surgery for distal radius fracture at our institution between January of 2007 and June of 2012. Only one of the 106 patients (0.9%) underwent surgery for persistent disability after initially failing nonoperative treatment for ≥6 weeks.
Discussion
It is debated whether malunion negatively impacts outcomes following DRF in older adults. Young and Rayan evaluated the effect of nonoperative treatment in sedentary older adults after distal radius fracture.5 They reported satisfactory patient outcomes with nonoperative treatment and that radiographic outcome was not associated with improvement in clinical outcome. Our study confirms these results; in a low-activity population, there is no association between radiographic malunion and functional outcomes. Young and Rayan, however, did not evaluate older adult patients with higher activity levels and recommended operative treatment in that population. Our data indicate that outcomes in high-activity older patients do not differ after malunion compared to a well-aligned DRF.
Two randomized trials are relevant to our investigation. Arora et al. conducted a randomized trial comparing nonoperative treatment to volar locking plate fixation in 73 patients ≥65 years old with displaced and unstable DRF’s.23 They demonstrated that although surgery improved radiographic parameters and increased grip strength it did not improve range of motion, pain, or patient-rated outcome at 1 year, and was associated with significantly more complications. Roumen et al. evaluated DRF’s in patients ≥55 initially treated with closed reduction and casting.10 The 43% of fractures that displaced at 2 weeks were randomized to either continued nonoperative treatment or external fixation. There was no difference in functional outcome between these groups. Our data support these results, however, unlike Arora et al. we found decreased grip strength in operatively compared to nonoperatively managed patients. Due to the non-randomized nature of our study, standard clinical care would bias results in favor of nonoperative management, as less severe fractures are more likely to be treated nonoperatively. For this reason, when assessing outcomes according to treatment, we excluded non-displaced fractures to improve the comparability of the groups.
In our regression model, general health (SF-12) and wrist flexion-extension arc were the only significant predictors of QuickDASH scores. A previous study of 733 manufacturing and service workers also demonstrated correlation between QuickDASH and SF-12 scores.24 It may be that patients with better-perceived overall health have less bodily pain and accomplish upper extremity tasks on the QuickDASH with greater ease. Second, decreased flexion-extension arc in the injured wrist is likely to make certain activities of daily living more difficult, thus increasing QuickDASH scores. Notably, neither a well-aligned fracture nor surgery led to greater flexion-extension arcs.
Our use of the validated PASE scale in a DRF population was unique. It was possible that our study cohort would prove more sedentary than the population at large, thus obscuring the negative impact of malunion on our high-activity group. However, the mean PASE score in our study population (146; 65–87 years old) was higher than the reported population averages of the youngest age category established during PASE validation (144 men, 113 women; 65–69 years old).25 We still concede that our study may not include the rare older adult patient who places extreme demands on their hands on a consistent basis.
There are several limitations to this study. Inherent to our cross-sectional study design, we can only determine that final outcomes (>1 year after DRF) were similar between patient groups. We cannot comment on potential benefits of surgery during early recovery such as shortened duration of immobilization or reduced pain from fracture stabilization. It is also possible that despite similar fracture classification and injury mechanisms, those fractures treated operatively may have been more severely angulated or displaced. Additionally, we do not assume our results generalize to specific infrequent fracture patterns that are routinely treated surgically (e.g., displaced volar shear fractures with carpal subluxation or the non-comminuted intra-articular fracture with a single large stepoff) as we do not have sufficient nonoperative experience to determine the natural history of such fractures in the older adult. This limitation is one inherent to any non-randomized investigation. In reviewing our surgeon’s recommendations for surgery, operative treatment was offered in part based on AAOS guidelines for acceptable reduction but influenced by impressions of general health, activity level, and the presences of other injuries. This use of overall clinical impression to guide decision making may have optimized results for both groups but the overall similarity in outcomes between patient groups (surgery versus nonoperative treatment and union versus malunion) are consistent with results from the randomized trials of Arora and Roumen.10,23 In our series we were unable to identify any threshold for radiographic parameters beyond which poor function was expected. However, that does not preclude the possibility that such a threshold exists. Finally, the preponderance of our patients were female so our data may not generalize to all male patients.
We believe that examining for sampling and misclassification bias strengthened our cross-sectional investigation. When designing this study, our IRB limited the approved enrollment to the number of participants determined to be sufficient for statistical analysis. Provided a much larger available population of older adults treated for distal radius fracture, we needed to confirm that our sampling was not misrepresentative. After identifying only a single operation to correct for radius malunion by our surgeons over a 5-year period in patients ≥65 years old, we are confident that we did not miss a substantial number of patients who were dissatisfied with a radius malunion. However, we cannot exclude the possibility that patients may have sought care elsewhere. Despite this review, we are unable to completely rule out sampling bias. Seventy-three patients declined office visits, and it is unknown if these patients differed systematically from the study population. Only one of the 73, however, declined participation due to dissatisfaction with care.
We also considered the possibility of reverse causality (i.e., poor wrist outcome resulting in lower overall activity). This would present bias towards acceptance of the null hypothesis. To address this, we asked patients which activities they were no longer able to perform. Performing a sensitivity analysis based on assigning these patients with activities prohibited by the radius fracture to the high-activity group, however, failed to affect our conclusions. However, it is possible that patients did not remember activities they were able to perform previously that were affected by their DRF at a mean of 3.5 years later. Despite this, even if activity levels were decreased at the time of follow-up, our study population demonstrated higher than average activity levels for their age, as discussed previously.
Distal radius fractures in the older adult appear to impart minimal upper extremity impairment and infrequently prevent return to activity despite frequent malunion. Our data indicate no difference in outcomes following malunion versus well-aligned fractures in highly active older patients. We counsel older patients that operative management often permits earlier wrist motion and improved appearance. However, it is unlikely to change the ultimate functional outcome and is associated with greater risk of complication. We inform older adults that distal radius malunion is typically associated with visible deformity but rarely requires corrective surgery in our practice.
Acknowledgments
Funding Sources:
This study was completed through funding supplied by a grant from the Orthopedic Research and Education Fund.
This publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448, sub-award TL1 TR000449, from the National Center for Advancing Translational Sciences.
Footnotes
Presented at the Annual Meeting of ASSH, San Francisco, CA, October 2–5 2013.
This study has undergone IRB approval.
The authors report no conflict of interest
Level of Evidence: Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Vogt MT, Cauley JA, Tomaino MM, et al. Study of descriptive characteristics and risk factors. The study of osteoporotic fractures. J Am Geriatr Soc. 2002;50:97–103. doi: 10.1046/j.1532-5415.2002.50014.x. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein JN, Birkmeyer JD. The Dartmouth Atlas of Musculoskeletal Health Care. Chicago: AHA Press; 2000. [PubMed] [Google Scholar]
- 3.Koval KJ, Harrast JJ, Anglen JO, et al. Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90:1855–1861. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 4.Gehrmann S, Windolf J, Kaufmann R. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33:421–429. doi: 10.1016/j.jhsa.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Jaremko JL, Lambert RGW, Rowe BH, et al. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62:65–72. doi: 10.1016/j.crad.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Anzarut A, Johnson J, Rowe BH, et al. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29:1121–1127. doi: 10.1016/j.jhsa.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25:19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 8.Board T, Kocialkowski A, Andrew G. Does Kapandji wiring help in older patients? A retrospective comparative review of displaced intra-articular distal radial fractures in patients over 55 years. Injury. 1999;30:663–669. doi: 10.1016/s0020-1383(99)00167-9. [DOI] [PubMed] [Google Scholar]
- 9.Fujii K, Henmi T, Kanematsu Y, et al. Fractures of the distal end of radius in elderly patients: a comparative study of anatomical and functional results. J Orthop Surg. 2002;10:9–15. doi: 10.1177/230949900201000103. [DOI] [PubMed] [Google Scholar]
- 10.Roumen R, Hesp W, Bruggink E. Unstable colles’ fractures in elderly patients: A randomised trial of external fixation for redisplacement. J Bone Joint Surg (Br) 1991;73:301–311. doi: 10.1302/0301-620X.73B2.2005162. [DOI] [PubMed] [Google Scholar]
- 11.McQueen M, Caspers J. Colles’ fracture: does the anatomical result affect the final function. J Bone Joint Surg (Br) 1988;70:649–651. doi: 10.1302/0301-620X.70B4.3403617. [DOI] [PubMed] [Google Scholar]
- 12.Schuit A, Schouten E, Westerterp K, et al. Validity of the physical activity scale for the elderly (PASE): according to energy expenditure assessed by the doubly labeled water method. J Clin Epidemiol. 1997;50:541–546. doi: 10.1016/s0895-4356(97)00010-3. [DOI] [PubMed] [Google Scholar]
- 13.Washburn R, McAuley E, Katula J, et al. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 14.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskel Dis. 2006;7:44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mintken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18:920–926. doi: 10.1016/j.jse.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Boyer MI, Korcek KJ, Gelberman RH, et al. Anatomic tilt x-rays of the distal radius: an ex vivo analysis of surgical fixation. J Hand Surg Am. 2004;29:116–122. doi: 10.1016/j.jhsa.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Graham T. Surgical correction of malunited fractures of the distal radius. J Am Acad Orthop Surg. 1997;5:270–281. doi: 10.5435/00124635-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Orthopaedic Surgeons. [Accessed June 13, 2013];The treatment of distal radius fractures: Guideline and evidence report [AAOS web site] 2009 Available at http://www.aaos.org/research/guidelines/drfguideline.pdf.
- 19.Trumble T, Culp R, Hanel D, et al. Intra-articular fractures of the distal aspect of the radius. Instr Course Lect. 1999;48:465–480. [PubMed] [Google Scholar]
- 20.Sorensen A, Howard D, Tan WH, et al. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38:641–649. doi: 10.1016/j.jhsa.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tashjian RZ, Deloach J, Porucznik CA, et al. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18:927–932. doi: 10.1016/j.jse.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 22.Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18:205–7. doi: 10.1136/emj.18.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arora R, Lutz M, Deml C, et al. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011 Dec 7;93(23):2146–53. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 24.Fan ZJ, Smith CK, Silverstein BA. Assessing validity of the QuickDASH and SF-12 as surveillance tools among workers with neck or upper extremity musculoskeletal disorders. J Hand Ther Hanley & Belfus. 2008;21:354–365. doi: 10.1197/j.jht.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 25.New England Research Institutes. PASE: Physical Activity Scale for the elderly Administration and Scoring Instruction Manual. Watertown, MA: New England Research Institutes, Inc; 1991. [Google Scholar]