Abstract
Introduction
Predicting severity of pancreatitis is an important goal. Clinicians are still searching for novel and simple biomarkers that can better predict persistent organ failure (OF). Lipoproteins, especially high-density lipoprotein (HDL), and apolipoprotein A-I (APO A-I), have been shown to have anti-inflammation effects in various clinical settings. Severe acute pancreatitis (SAP) is associated with hypo-lipoproteinemia. We studied whether the concentrations of HDL and APO A-I can predict persistent OF in patients with predicted SAP admitted to the ICU.
Methods
In 66 patients with predicted SAP, we prospectively evaluated the relationship between lipid levels, inflammatory cytokines and clinical outcomes, including persistent OF and hospital mortality. Blood samples were obtained within 24 hours of admission to the ICU.
Results
HDL and APO A-I levels were inversely correlated with various disease severity scores. Patients with persistent OF had lower levels of HDL and APO A-I, while those with transient OF had lower levels of interleukin-6, tumor necrosis factor-α and lower rates of hospital mortality. Meanwhile, hospital non-survivors had lower concentrations of HDL, and APO A-I compared to the survivors. By using the area under the receiver operating characteristic (AUROC) curve, both HDL and APO A-I demonstrated an excellent discriminative power for predicting persistent OF among all patients (AUROC 0.912 and 0.898 respectively) and among those with OF (AUROC 0.904 and 0.895 respectively). Pair-wise comparison of AUROC showed that both HDL and APO A-I had better discriminative power than C-reactive protein to predict persistent OF.
Conclusions
Serum levels of HDL and APO A-I at admission to the ICU are inversely correlated with disease severity in patients with predicted SAP and can predict persistent OF in this clinical setting.
Electronic supplementary material
The online version of this article (doi:10.1186/s13054-015-0832-x) contains supplementary material, which is available to authorized users.
Introduction
Acute pancreatitis represents an acute inflammatory disorder with variable severity ranging from mild, self-limited disease to a severe inflammatory cascade associated with multiple-organ failure. Despite the improvements in critical care, severe acute pancreatitis (SAP) is still associated with a high mortality rate [1]. Although the incidence of organ failure in the early phase (within the first week) varies among different studies [2-6], persistent organ failure (OF) has been shown to be the major determinant of clinical outcomes [6,7]. These observations have led to modified definitions of SAP, which recognize the importance of persistent OF and introduce a new sub-classification of moderately severe pancreatitis based on the presence of transient OF [8,9].
It is important to stratify the severity of acute pancreatitis. First, early identification of patients with potential SAP may facilitate timely referral to specialists. Second, for specialists, severity-stratification of those patients makes triage and comparison between different studies possible. However, when organ failure is present in the early phase, it may be difficult to determine the final degree of severity because it is unknown whether the patient will prove to have persistent or transient OF.
It has been shown that the concentrations of total cholesterol and lipoproteins decrease in the early stages of critical illness [10-12]. Indeed, the pattern of early rapid decline is found primarily in the high-density lipoprotein (HDL) [12]. Moreover, the protein composition of HDL is markedly altered as well, with the apolipoprotein A1 (APO A-I) depleted [12].
Apo A-I is the major protein component of HDL. APO A-I plays an essential role in cholesterol homeostasis by transporting excessive cholesterol from extra-hepatic tissues to the liver. Aside from this biological function, recently, more emphasis has been placed upon its anti-inflammatory effects. Apo A-I can attenuate lipopolysaccharide-induced cytokine secretion in a mode of protein-endotoxin interaction, even without its physiological lipid complement [13,14]. Furthermore, elevated cytokines can downregulate hepatic synthesis of HDL and APO A-I [15].
Although there have been studies of lipoprotein profile in acute pancreatitis [16-18], there has been no report on the specific role of lipoprotein in predicting severity using the most updated definition. The results of previous studies raise the possibility that the levels of lipoprotein may play a role in assessing disease severity [17,18]. However, these studies had several limitations, including retrospective design [17], and inconsistent definitions of severity ranging from severe pancreatitis based on the Atlanta criteria to mortality [17,18]. None of these studies evaluated persistent OF, which has become recognized as the most clinically relevant indicator of disease severity. Furthermore, these studies have mainly focused on the analysis of total cholesterol, triglycerides, LDL or HDL cholesterol. APO A-I levels have rarely been reported, even though APO A-I represents the major protein component of HDL, modulating inflammation.
We hypothesized that low levels of lipoprotein are associated with a more pronounced inflammatory state in patients with predicted SAP and may serve as a marker to discriminate persistent OF from transient OF upon admission to ICU. Therefore, we conducted this prospective observational investigation to study whether low concentrations of APO A-I and HDL are associated with persistent OF and hospital mortality. Other potential indicators of inflammation such as C-reactive protein (CRP), TNF-α and IL-6 were also measured.
Material and methods
Patient information, data collection and definitions
This study was conducted with the approval of the institutional review board of Chang Gung Memorial Hospital, Taiwan and in accordance with the Declaration of Helsinki of the World Medical Association. Formal consent was obtained from the patient or the next of kin. The study was performed in the ICU of two university-affiliated hospitals between February 2008 and September 2011. This study enrolled 66 patients with predicted SAP requiring intensive monitoring and/or treatment. Predicted SAP was defined by acute physiology, age, and chronic health evaluation (APACHE II) score ≥8 at admission [19]. All patients included in this study were admitted to hospital within 72 hours of onset of symptoms.
The diagnosis of acute pancreatitis was made based on two or more of the following: typical abdominal pain; serum amylase and/or lipase levels at least three times the upper limit of normal; and characteristic findings of acute pancreatitis on a contrast-enhanced computed tomography (CT) scan, or abdominal ultrasonography. Abdominal ultrasonography was performed for each case at presentation. Enhanced CT was performed when the disease was evaluated as predicted SAP. CT-guided aspiration was performed and bacterial cultures were obtained when infected necrosis was suspected.
Organ failure was defined as a score of ≥2 in one or more of the three (respiratory, renal, and cardiovascular) organ systems described in the modified Marshall score during the first week [20,21]. This definition is in accordance with the most updated revised Atlanta classification [8,9]. OF was defined as transient for duration <48 hours or persistent if >48 hours. Meanwhile, disease severity also was assessed by sequential organ failure assessment (SOFA) [22].
Patients with a history of prior acute pancreatitis or drug history of lipid-lowering agents, and patients those receiving total parenteral nutrition at the time of blood sampling were excluded from this study. All ICU admissions were followed until discharge from the hospital or hospital mortality.
Laboratory investigations
Blood cultures and appropriate cultures from the infection focus were obtained. Hematological and biochemical data including serum lipoprotein were also collected systemically within 24 hours of admission to ICU, with a median of 3 days (IQR 2 to 4 days) after the start of symptoms and a median of 2 days (IQR 1 to 3 days) after admission to hospital. For the scoring systems, the most abnormal value for each organ system on the day of blood sampling was recorded.
A fasting blood sample was obtained in the morning. The blood samples were allowed to clot and were spun immediately in a refrigerated centrifuge. The serum was obtained and frozen at −80°C. Total cholesterol (TC) and triglyceride (TG) were measured enzymatically using kits (Wako Pure Chemical, Osaka, Japan). The concentrations of HDL and LDL were directly measured using a homogenous assay (Daiichi Pure Chemical, Ibaraki, Japan). APO A-I was measured by means of immunoturbidimetry with the TurbiTime system (Dade Behring Inc, Newark, DE, USA). The concentrations of TNF-α and IL-6 were measured by an enzyme-linked immunosorbent assay (R & D Systems, Minneapolis, MN, USA). CRP was measured by a latex-enhanced immunoturbidimetric method (Daiichi Pure Chemical).
Statistical analysis
Descriptive statistics are expressed as mean ± SD. All variables were tested for normal distribution using the Kolmogorov-Smirnov test. The Student t-test was used to compare the means of continuous variables and the normality of data distribution. Otherwise, the Mann-Whitney U-test was used. Categorical data were tested using the chi-square (χ2) test. The Kruskall-Wallis test followed by Dunn’s post hoc test was used for multiple comparison. Correlation between the lipid levels, cytokines and the disease severity scores was analyzed with the Spearman rank method. Discrimination was tested using the area under a receiver operating characteristic (ROC) curve (AUROC) to assess the ability of HDL cholesterol and APO A-I to predict persistent OF. ROC analysis was also performed to calculate the cutoff values, sensitivity, specificity, overall correctness, and positive and negative predictive values (PPV and NPV). The best Youden index (sensitivity + specificity-1) [23] was also used to determine the best cutoff point of HDL and APO A-I to predict persistent OF. All statistical tests were two-tailed, and the significance level was set at P ≤0.05. Data were analyzed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA) except for comparisons of ROC curve. The comparisons between ROC curves were calculated with the MedCalc software (MedCalc Software 14.12.0, Belgium), using the Hanley and McNeil method [24].
Results
Subject characteristics
During the study period, 69 consecutive patients with predicted SAP were admitted to ICU: 3 patients were excluded because of prior history of acute pancreatitis, and 66 patients were enrolled in this investigation. Table 1 lists the patients’ demographic data and clinical characteristics. Overall, the in-hospital mortality for the entire group was 19.7%. Compared to hospital survivors, the hospital non-survivors had higher disease severity as evidenced by higher Ranson, APACHE II, SOFA, and modified Marshall scores.
Table 1.
Patients’ demographic data and clinical characteristics
| Hospital survivors | Hospital non-survivors | P -value | |
|---|---|---|---|
| (n = 53) | (n = 13) | ||
| Age, years | 60 (45 to 76.5) | 59 (45 to 84) | 0.640 |
| Gender, M/F, number | 29/24 | 9/4 | 0.532 |
| BMI, kg/m2 | 25.9 ± 4.0 | 25.2 ± 3.7 | 0.597 |
| Body weight, kg | 67.6 ± 12.1 | 69.2 ± 11.8 | 0.671 |
| Etiology, alcohol/biliary/ERCP/others | 19/31/0/3 | 6/6/1/0 | 0.145 |
| Leukocytes, ×109/l | 11.8 ± 5.7 | 14.6 ± 0.9 | 0.301 |
| Hemoglobin, g/dl | 10.4 ± 2.1 | 10.3 ± 2.6 | 0.893 |
| Platelets, ×109/l | 157.5 (88.3 to 241) | 62 (25 to 216) | 0.043 |
| BUN, mg/dl | 17.5 (10.8 to 26.5) | 44 (14.5 to 91.5) | 0.009 |
| Serum creatinine, mg/dl | 0.9 (0.7 to 1.9) | 3.1 (1.8 to 5.4) | 0.003 |
| Bilirubin, mg/dl | 1.5 (0.9 to 3) | 8 (2.7 to 22. 5) | <0.001 |
| INR | 1.2 (1.1 to 1.4) | 1.5 (1.2 to 1.8) | 0.007 |
| Ranson score | 5 (4 to 6) | 6 (6 to 8.5) | 0.001 |
| APACHE II score | 15 (11 to 20.8) | 28 (16.5 to 34.8) | 0.002 |
| SOFA score | 5 (3 to 8) | 13 (6.5 to 15.8) | 0.001 |
| Modified Marshall score | 3 (2 to 5.5) | 9.5 (7 to 10.8) | <0.001 |
| Organ failure | 42 (79.2%) | 13 (100%) | 0.104 |
| Number of organ failures | 1 (1 to 2) | 3 (2 to 3) | <0.001 |
| Respiratory failure | 38 (71.7%) | 12 (92.3%) | 0.162 |
| Renal failure | 21 (39.6%) | 11 (84.6%) | 0.005 |
| Cardiovascular failure | 13 (24.5%) | 11 (84.6%) | <0.001 |
| Infected necrosis, n | 10 (18.9%) | 8 (61.5%) | 0.002 |
| Persistent organ failure, n | 22 (41.5%) | 13 (100%) | <0.001 |
| Cholesterol, mg/dl | 122 (92 to 152) | 98 (81 to 139) | 0.256 |
| Triglyceride, mg/dl | 140 (107 to 239) | 180 (102 to 362) | 0.723 |
| HDL, mg/dl | 17 (11 to 31) | 6 (4 to 13) | <0.001 |
| LDL, mg/dl | 61 (40 to 79) | 43 (30 to 91) | 0.297 |
| APO A-I, mg/dl | 67 (50 to 83) | 40 (23 to 46) | <0.001 |
| IL-6, pg/ml | 73 (39.7 to 177.8) | 388 (125 to 831.5) | 0.015 |
| TNF-α, pg/ml | 6.2 (2.9 to 13.5) | 25 (20 to 42) | 0.011 |
| CRP, mg/l | 182.6 ± 115.6 | 151.6 ± 77.4 | 0.382 |
Results are presented as mean ± SD, or median (IQR) unless otherwise stated. M, male; F, female; BMI, body mass index; ERCP, endoscopic retrograde cholangiopancreagraphy; BUN, blood urea nitrogen; INR, international normalized ratio; APACHE, acute physiology, age, and chronic health evaluation; SOFA, sequential organ failure assessment; HDL, high-density lipoprotein; LDL, low-density lipoprotein; APO, A-I apolipoprotein A-I; CRP, C-reactive protein.
Lipid profile and mortality
The levels of HDL, and APO-A-I were significantly higher in those who survived (Table 1), while the levels of TNF-α and IL-6 were higher in those who died. Although weak, HDL and APO A-I were inversely correlated with Ranson, APACHE II, SOFA and modified Marshall scores (Table 2). Among these, HDL had the strongest negative correlation with the modified Marshall score. Inflammatory cytokines were also negatively correlated with HDL, and APO A-I. Of these, HDL had the strongest inverse relationship with serum IL-6 levels. The concentrations of APO A-I and HDL decreased progressively and significantly with the number of organ failures as defined by the modified Marshall score (Figure 1). The discriminating power of APO A-I and HDL to predict 28-day mortality was tested using the AUROC. The AUROC for APO A-I and HDL to predict 28-day mortality was 0.869 ± 0.047 (mean ± standard error of the mean (SEM)), 95% CI 0.764 to 0.940, and 0.791 ± 0.059, 95% CI 0.673 to 0.881, respectively.
Table 2.
Correlation between serum lipid, disease severity scores, and serum inflammatory cytokines
| Statistics | Ranson score | APACHE II score | SOFA score | Modified Marshall score | TNF-α | IL-6 | |
|---|---|---|---|---|---|---|---|
| Cholesterol | R | −0.198 | −0.321 | −0.367 | −0.349 | −0.335 | −0.196 |
| P | 0.115 | 0.010 | 0.003 | 0.004 | 0.025 | 0.192 | |
| HDL | R | −0.376 | −0.483 | −0.613 | −0.669 | −0.450 | −0.540 |
| P | 0.002 | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 | |
| LDL | R | −0.165 | −0.371 | −0.335 | −0.423 | −0.285 | −0.356 |
| P | 0.196 | 0.003 | 0.008 | 0.001 | 0.057 | 0.018 | |
| Triglyceride | R | 0.130 | 0.071 | 0.094 | 0.246 | −0.012 | 0.185 |
| P | 0.301 | 0.579 | 0.463 | 0.048 | 0.937 | 0.219 | |
| APO A-I | R | −0.378 | −0.467 | −0.569 | −0.597 | −0.467 | −0.471 |
| P | 0.002 | <0.001 | <0.001 | <0.001 | 0.001 | 0.001 |
HDL, high-density lipoprotein; LDL, low-density lipoprotein; APO A-I, apolipoprotein A-I; APACHE, acute physiology and chronic health evaluation; SOFA, sequential organ failure assessment.
Figure 1.
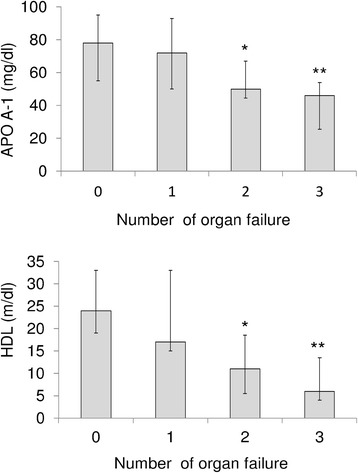
Association among apolipoprotein A-I (APO A-1), high-density lipoprotein (HDL) and organ failure. The levels of apolipoprotein A-I and HDL decrease progressively and significantly with the number of organ failures. *P <0.05 compared to the group with no organ system failure; **P <0.001 compared to the group with no organ system failure (Kruskall-Wallis test followed by Dunn’s post hoc test). Results are expressed as median, with error bars representing the IQR.
Lipid profile and organ failure
Table 3 lists the demographic data, clinical characteristics and lipid profiles in patient subgroups stratified by the presence of OF. The levels of total cholesterol, HDL, LDL and APO A-I were significantly lower in patients with OF, while the levels of TNF-α, IL-6 and CRP were lower in those without OF. When persistency of organ failure was not taken into account, there was no difference in mortality rates between patient with OF and those without OF (Table 3).
Table 3.
Patients’ demographic data and clinical characteristics stratified by early organ failure
| Organ failure | No organ failure | P -value | |
|---|---|---|---|
| (n = 55) | (n = 11) | ||
| Age, years | 59 (45 to 76) | 69 (45 to 92) | 0.429 |
| Gender, M/F, n | 34/21 | 4/7 | 0.182 |
| BMI, kg/m2 | 25.7 ± 3.8 | 26.2 ± 4.4 | 0.748 |
| Body weight, kg | 68.3 ± 12.2 | 65.7 ± 10.9 | 0.545 |
| Etiology, alcohol/biliary/ERCP/others | 21/30/1/3 | 4/7/0/0 | 0.815 |
| Leukocytes, ×109/l | 13.1 ± 6.6 | 9.1 ± 4.6 | 0.058 |
| Hemoglobin, g/dl | 10.4 ± 2.3 | 10.3 ± 1.5 | 0.936 |
| Platelets, ×109/l | 138 (72 to 229) | 139.5 (58.5 to 247.3) | 0.935 |
| BUN, mg/dl | 23 (12.5 to 41.5) | 12 (7 to 22) | 0.023 |
| Serum Creatinine, mg/dl | 1.5 (0.9 to 3.2) | 0.7 (0.6 to 0.9) | <0.001 |
| Bilirubin, mg/dl | 1.6 (1.1 to 5.4) | 1.5 (1 to 4) | 0.642 |
| INR | 1.2 (1.1 to 1.5) | 1.05 (1 to 1.13) | 0.002 |
| Ransons score | 5.5 (4 to 7) | 4 (3 to 4) | 0.001 |
| APACHE II score | 18 (11 to 25.5) | 14 (10 to 15) | 0.028 |
| SOFA score | 6 (4.3 to 9.8) | 3 (2 to 5) | 0.005 |
| Modified Marshall score | 5 (3 to 7.25) | 1 (0 to 1) | <0.001 |
| Infected necrosis, n | 18 (32.7%) | 0 (0%) | 0.028 |
| Cholesterol, mg/dl | 117 (83 to 142) | 151 (109 to 172) | 0.046 |
| Triglyceride, mg/dl | 148 (105 to 285) | 132 (92 to 167) | 0.242 |
| HDL, mg/dl | 15 (6 to 22) | 24 (19 to 33) | 0.010 |
| LDL, mg/dl | 56 (37 to 75) | 82 (65 to 100) | 0.005 |
| APO A-I, mg/dl | 54 (41 to 74) | 78 (55 to 96) | 0.020 |
| IL-6, pg/ml | 129 (54 to 251.5) | 29 (10.4 to 101.5) | 0.005 |
| TNF-α, pg/ml | 10.8 (4.7 to 23) | 2.9 (1.1 to 3.7) | 0.001 |
| CRP, mg/l | 190.6 ± 108.9 | 111.0 ± 90.4 | 0.027 |
| Hospital mortality | 13 (23.6%) | 0 (0%) | 0.104 |
| ICU mortality | 9 (16.4%) | 0 (0%) | 0.337 |
| 28-day mortality | 11 (20%) | 0 (0%) | 0.188 |
| ICU stay, days | 8 (5 to 14.5) | 5 (5 to 11) | 0.510 |
Results are presented as mean ± SD, or median (IQR) unless otherwise stated. M, male; F, female; BMI, body mass index; ERCP, endoscopic retrograde cholangiopancreagraphy; BUN, blood urea nitrogen; INR, international normalized ratio; APACHE, acute physiology and chronic health evaluation; SOFA, sequential organ failure assessment; HDL, high-density lipoprotein; LDL, low-density lipoprotein; APO A-I, apolipoprotein A-I; CRP C-reactive protein.
HDL and APO A-I as markers to predict persistent organ failure
To further demonstrate the association among lipid profile, persistent OF and mortality, those patients with OF were sub-grouped into transient OF and persistent OF. Table 4 shows the clinical characteristics and outcomes in patient subgroups stratified by persistency of OF. The levels of total cholesterol, HDL, LDL and APO A-I were significantly lower in patients with persistent OF, while the levels of TNF-α, and IL-6 were higher in those with persistent OF. The mortality rates were significantly higher in patients with persistent OF, while ICU stay was shorter in patients with transient OF. The discriminating power of APO A-I and HDL to predict persistent OF was also tested using AUROC. When all patients with predicted SAP were analyzed, the AUROC for APO A-I and HDL to predict persistent OF was 0.898 ± 0.043 (mean ± SEM), 95% CI 0.813 to 0.983, and 0.912 ± 0.036, 95% CI: 0.842 to 0.982, respectively. There was no significant difference in discriminating power between HDL and APO A-I (P = 0.587). When those patients with OF were analyzed, the AUROC for APO A-I and HDL to predict persistent OF was 0.895 ± 0.045 (mean ± SEM), 95% CI 0.808 to 0.983, and 0.904 ± 0.037, 95% CI 0.832 to 0.976 respectively (P = 0.838). These results indicate that both HDL and APO A-I are good markers in this clinical setting. Meanwhile, we also evaluated the discriminating ability of CRP because it has been used as a biomarker to predict severity [1]. The area under ROC curve for CRP obtained by analyzing all patients or patients with OF was 0.603 ± 0.061, and 0.568 ± 0.076, respectively. Pair-wise comparisons of AUROC showed that both HDL and APO A-I gave significantly higher AUROC and thus, better predictive accuracy than CRP when analyzing all patients (P <0.001 relative to both HDL and APO A-I) or patients with OF (P <0.001 relative to both HDL and APO A-I). The best cutoff points of HDL and APO A-I to predict persistent OF remained the same when analyzing all patients or patients with OF. Table 5 shows the predictive values of the chosen cutoff points (16.5 mg/dl for HDL, 64 mg/dl for APO A-I), which gave the best Youden index, for prediction of persistent OF.
Table 4.
Patients’ demographic data and clinical characteristics stratified by persistent organ failure
| Organ failure (transient) | Organ failure (persistent) | P -value | |
|---|---|---|---|
| (n = 20) | (n = 35) | ||
| Age, years | 70.5 (46.5 to 80.3) | 54 (44 to 71) | 0.159 |
| Gender, M/F, n | 10/10 | 24/11 | 0.173 |
| BMI, kg/m2 | 26.5 ± 4.3 | 25.3 ± 3.6 | 0.300 |
| Body weight, kg | 66.4 ± 12.7 | 69.3 ± 12.3 | 0.415 |
| Etiology, alcohol/biliary/ERCP/others | 4/15/0/1 | 17/15/1/2 | 0.126 |
| Leukocytes, ×109/l | 12.9 ± 5.6 | 13.20 ± 7.3 | 0.888 |
| Hemoglobin, g/dl | 10.5 ± 2.6 | 10.30 ± 2.2 | 0.718 |
| Platelets, ×109/l | 157.5 (104.5 to 240) | 112 (49 to 229) | 0.178 |
| BUN, mg/dl | 16.5 (7.5 to 26) | 26.5 (14 to 50.5) | 0.011 |
| Serum Creatinine, mg/dl | 0.9 (0.8 to 1.3) | 2.6 (1.1 to 3.8) | 0.003 |
| Bilirubin, mg/dl | 1.5 (0.8 to 1.9) | 2.6 (1.2 to 8.0) | 0.081 |
| INR | 1.2 (1.1 to 1.4) | 1.3 (1.2 to 1.6) | 0.044 |
| Ranson score | 5 (4 to 5.5) | 6 (5 to 7) | 0.009 |
| APACHE II score | 12 (10 to 17.8) | 22 (15 to 28) | <0.001 |
| SOFA score | 4.5 (2 to 6) | 8 (6 to 12.3) | <0.001 |
| Modified Marshall score | 3 (2 to 3) | 6.5 (4.8 to 10) | <0.001 |
| Number of organ failures | 1 (1 to 1.8) | 2 (2 to 3) | <0.001 |
| Respiratory failure | 17 (85%) | 33 (94.3%) | 0.342 |
| Renal failure | 6 (30%) | 26 (4.3%) | 0.001 |
| Cardiovascular failure | 3 (15%) | 21 (60%) | 0.002 |
| Infected necrosis | 0 (0%) | 17 (51.4%) | <0.001 |
| Cholesterol, mg/dl | 131.5 (117 to 170) | 94 (83 to 135) | 0.017 |
| Triglyceride, mg/dl | 144 (116 to 242) | 153 (103 to 290) | 0.868 |
| HDL, mg/dl | 30 (17 to 36) | 8 (5 to 15) | <0.001 |
| LDL, mg/dl | 66 (56 to 74) | 42 (30 to 77) | 0.029 |
| APO A-I, mg/dl | 81 (69 to 100) | 48 (31 to 54) | <0.001 |
| IL-6, pg/ml | 63.5 (43 to 136.5) | 211 (104 to 552) | 0.005 |
| TNF-α pg/ml | 6.3 (2.9 to 15) | 12 (6.1 to 25) | 0.048 |
| CRP, mg/l | 195.0 ± 91.4 | 188.3 ± 118.3 | 0.833 |
| Hospital mortality | 0 (0%) | 13 (35.3%) | 0.002 |
| ICU mortality | 0 (0%) | 9 (25.7%) | 0.019 |
| 28-day mortality | 0 (0%) | 11 (31.4%) | 0.004 |
| ICU stay, days | 5 (3 to 9) | 11 (5.8 to 17.3) | 0.009 |
Results are presented as mean ± SD, or median (IQR) unless otherwise stated. M male; F female; BMI body mass index; ERCP endoscopic retrograde cholangiopancreagraphy; BUN blood urea nitrogen; INR international normalized ratio; APACHE acute physiology and chronic health evaluation; SOFA sequential organ failure assessment; HDL high-density lipoprotein; LDL low-density lipoprotein; APO A-I apolipoprotein A-I; TNF tumor necrosis factor; CRP C-reactive protein.
Table 5.
HDL and APO A-I for prediction of persistent organ failure
| Sensitivity | Specificity | PPV | NPV | Accuracy | |
|---|---|---|---|---|---|
| All patients | |||||
| HDL <16.5 mg/dl | 0.886 | 0.839 | 0.861 | 0.867 | 0.864 |
| APO A-I <64 mg/dl | 0.943 | 0.806 | 0.846 | 0.926 | 0.879 |
| Patients with organ failure | |||||
| HDL <16.5 mg/dl | 0.886 | 0.850 | 0.912 | 0.810 | 0.873 |
| APO A-I <64 mg/dl | 0.943 | 0.850 | 0.917 | 0.895 | 0.909 |
HDL, high-density lipoprotein; APO A-I, apolipoprotein A-I; PPV, positive predictive value; NPV, negative predictive value.
We also evaluated the performance of different scores. We found that there is no difference in discriminating power of predicting persistent OF among HDL, APO A-I and different scores (Additional file 1: Table S1).
Discussion
The major findings of this study are as follows: (1) low levels of APO A-I and HDL are associated with high levels of inflammatory cytokines, persistent OF, infected necrosis and hospital mortality in patients with predicted SAP admitted to ICU; (2) APO A-I and HDL can serve as biomarkers to differentiate persistent OF from transient OF in this clinical setting.
In acute patients with pancreatitis, inflammatory reaction initially takes place within the pancreas. Subsequently, inflammatory cytokines induce hepatic synthesis of acute-phase proteins and mediate distant organ failure in the setting of SAP [25]. Despite improvements in critical care, the mortality rate of SAP remains high and is closely associated with the development of persistent OF and subsequent sepsis [26]. Gut barrier failure with ensuing endotoxin translocation has been proposed as a major contributor to the development of OF in SAP [26]. Increased intestinal permeability occurs early after onset of acute pancreatitis and closely correlates with disease severity, levels of endotoxemia, and release of inflammatory cytokines, which initiate and propagate the deleterious consequences of severe inflammation, such as organ failure and mortality [26,27]. Recently, the capability of lipoprotein to bind and neutralize endotoxin has drawn more and more attention. When endotoxin was added to normal human whole blood in vitro, the binding of endotoxin to lipoproteins displays high specificity, with HDL binding the majority of endotoxin (60%) [28]. In this regard, serum lipoprotein may represent an integral part of innate immunity against organ injury in SAP.
In addition to the ability to neutralize endotoxin, HDL has also been shown to have antioxidant and anti-inflammatory properties [29]. In this regard, free radicals and oxidative stress have been implicated in the pathogenesis of acute pancreatitis and have been shown to correlate with the severity of pancreatitis [30,31]. Consistent with previous reports on critically ill patients [32-34], we showed that the levels of HDL and APO A-I at admission to ICU were significantly lower in non-survivors. We also demonstrated that the levels HDL and APO A-I were significantly lower in patients with persistent OF, while the levels of TNF-α, and IL-6 were lower in those with transient OF. Although hypolipidemia is a well-recognized phenomenon in critical illness [32,33], the mechanisms are incompletely understood and probably multi-factorial. Both decreased synthesis and enhanced catabolism may be involved. It has been shown that TNF-α and IL-6 can dose-dependently inhibit synthesis of apolipoprotein in hepatic cell lines [15]. On the other hand, over-expression of secretory phospholipase A2, an acute-phase protein, can induce rapid catabolism of HDL and APO A-I [35]. Taken together, high levels of inflammatory cytokines in patients with SAP may not only impair the biosynthesis of APO A-I and HDL but also facilitate the degradation of lipoprotein, rendering these patients even more susceptible to harmful consequences of inflammation. Additionally, increased levels of endotoxin in SAP may overwhelm the already impaired neutralization ability provided by low levels of HDL and APO A-I and subsequently become even more unopposed, thus perpetuating the overproduction of inflammatory cytokines. A vicious cycle ensues and leads to further failure of multiple organ functions. Agreeing with this hypothesis, we showed that serum levels of APO A-I were inversely correlated with systemic inflammatory states, which was indicated by serum levels of TNF-α and IL-6 (Table 2). We also demonstrated that the concentrations of APO A-I and HDL decreased progressively as the number of organ failures increased (Figure 1).
Another novel finding of our study is that APO A-I and HDL can differentiate persistent OF from transient OF. In this regard, the existing scoring systems have shown moderate accuracy in predicting persistent OF [36]. However, these scoring systems are cumbersome to use and appeared to have reached their maximal efficacy in this clinical setting. To improve the capability of predicting persistent OF, clinicians need to develop new approaches. In addition to recognized scoring systems, recent attention has also focused on simple biomarkers that could give predictive information [37,38], such as blood urea nitrogen (BUN) and creatinine. Despite these encouraging results, there are drawbacks in currently available data that these markers are not necessarily patho-physiologically linked to the development of the OF and therefore, elevation of these markers simply reflects ongoing OF. Theoretically, patho-physiologically relevant biomarkers may perform better in this clinical setting. In this regard, blood lipoprotein may provide important prognostic information and help risk stratification.
There are limitations of our study. First of all, we studied these markers in patients admitted to ICU, therefore, our results may not be generalizable in those patients with less severe illness. Second, the number of patients studied was small. Further studies with larger cohorts are needed to validate our results.
Conclusions
The concentrations of HDL and APO A-I are inversely related to disease severity in patients with predicted SAP admitted to ICU. Serum levels of HDL and APO A-I at admission to ICU can predict persistent OF in this clinical setting. Whether lipid-based treatment can play a therapeutic role in the management of SAP deserves further investigation.
Key messages
Low levels of APO A-I and HDL are associated with high levels of inflammatory cytokines, persistent OF, infected necrosis and hospital mortality in patients with predicted SAP admitted to ICU
APO A-I and HDL can serve as biomarkers to differentiate persistent OF from transient OF in this clinical setting
Acknowledgements
This work is partially supported by a grant from the Chang Gung Medical Research Fund CMRPG680421, Chang Gung Memorial Hosipital, Chia-Yi, Taiwan.
Abbreviations
- APACHE
acute physiology age, and chronic health evaluation
- APO A-I
apolipoprotein A-I
- AUROC
area under a receiver operating characteristic curve
- BMI
body mass index
- BUN
blood urea nitrogen
- CRP
C-reactive protein
- CT
computed tomography
- ERCP
endoscopic retrograde cholangiopancreagraphy
- HDL
high-density lipoprotein
- IL-6
interleukin-6
- INR
international normalized ratio
- LDL
low-density lipoprotein
- NPV
negative predictive value
- OF
organ failure
- PPV
positive predictive value
- ROC
receiver operating characteristic curve
- SAP
severe acute pancreatitis
- SOFA
sequential organ failure assessment
- TG
triglyceride
- TNF
tumor necrosis factor
Additional file
Pair-wise comparisons of area under the receiver operating characteristic curve (AUROC) for high-density lipoprotein (HDL), apolipoprotein A-I (APO A-I) and scores to predict persistent organ failure.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MHT conceived the study. YSP participated in its design and coordination and drafted the manuscript. YCC, YCT, CWY, JML, JTF, MSL, YHT, TLH, CFH, and CSW participated in its design and coordination. All authors approved the manuscript after critical reading.
Contributor Information
Yun-Shing Peng, Email: pengys66@gmail.com.
Yung-Chang Chen, Email: cyc2356@hotmail.com.
Ya-Chung Tian, Email: dryctian@yahoo.com.
Chih-Wei Yang, Email: cwyang@ms1.hinet.net.
Jau-Min Lien, Email: lienoski@seed.net.tw.
Ji-Tseng Fang, Email: fangjits@gmail.com.
Cheng-Shyong Wu, Email: kib_992002@yahoo.com.tw.
Chien-Fu Hung, Email: hcf5514@cgmh.org.tw.
Tsan-Long Hwang, Email: hwangtl@cgmh.org.tw.
Ying-Huang Tsai, Email: chestmed@adm.cgmh.org.tw.
Mel S Lee, Email: mellee@adm.cgmh.org.tw.
Ming-Hung Tsai, Email: mhtsai@cgmh.org.tw.
References
- 1.De Waele JJ. Acute pancreatitis. Curr Opin Crit Care. 2014;2:189–95. doi: 10.1097/MCC.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 2.McKay CJ, Curran F, Sharples C, Baxter JN, Imrie CW. Prospective placebo-controlled randomized trial of lexipafant in predicted severe acute pancreatitis. Br J Surg. 1997;84:1239–43. doi: 10.1002/bjs.1800840912. [DOI] [PubMed] [Google Scholar]
- 3.Uhl W, Buchler MW, Malfertheiner P, Beger HG, Adler G, Gaus W. A randomised, double blind, multicentre trial of octreotide in moderate to severe acute pancreatitis. Gut. 1999;45:97–104. doi: 10.1136/gut.45.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tenner S, Sica G, Hughes M, Noordhoek E, Feng S, Zinner M, et al. Relationship of necrosis to organ failure in severe acute pancreatitis. Gastroenterology. 1997;113:899–903. doi: 10.1016/S0016-5085(97)70185-9. [DOI] [PubMed] [Google Scholar]
- 5.Johnson CD, Kingsnorth AN, Imrie CW, McMahon MJ, Neoptolemos JP, McKay C, et al. Double blind, randomised, placebo controlled study of a platelet activating factor antagonist, lexipafant, in the treatment and prevention of organ failure in predicted severe acute pancreatitis. Gut. 2001;48:62–9. doi: 10.1136/gut.48.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002;89:298–302. doi: 10.1046/j.0007-1323.2001.02025.x. [DOI] [PubMed] [Google Scholar]
- 7.Johnson CD, Abu-Hilal M. Persistent organ failure during the first week as a marker of fatal outcome in acute pancreatitis. Gut. 2004;53:1340–4. doi: 10.1136/gut.2004.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–11. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 9.Dellinger EP, Forsmark CE, Layer P, Lévy P, Maraví-Poma E, Petrov MS, et al. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg. 2012;256:875–80. doi: 10.1097/SLA.0b013e318256f778. [DOI] [PubMed] [Google Scholar]
- 10.Alvarez C, Ramos A. Lipids, lipoproteins, and apoproteins in serum during infection. Clin Chem. 1986;32:142–5. [PubMed] [Google Scholar]
- 11.Chenaud C, Merlani PG, Roux-Lombard P, Burger D, Harbarth S, Luyasu S, et al. Low apolipoprotein A-I level at intensive care unit admission and systemic inflammatory response syndrome exacerbation. Crit Care Med. 2004;32:632–7. doi: 10.1097/01.CCM.0000114820.47460.0A. [DOI] [PubMed] [Google Scholar]
- 12.van Leeuwen HJ, Heezius EC, Dallinga GM, van Strijp JA, Verhoef J, van Kessel KP. Lipoprotein metabolism in patients with severe sepsis. Crit Care Med. 2003;31:1359–66. doi: 10.1097/01.CCM.0000059724.08290.51. [DOI] [PubMed] [Google Scholar]
- 13.Emancipator K, Csako G, Elin RJ. In vitro inactivation of bacterial endotoxin by human lipoproteins and apolipoproteins. Infect Immun. 1992;60:596–601. doi: 10.1128/iai.60.2.596-601.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flegel WA, Baumstark MW, Weinstock C, Berg A, Northoff H. Prevention of endotoxin-induced monokine release by human low- and high-density lipoproteins and by apolipoprotein A-I. Infect Immun. 1993;61:5140–6. doi: 10.1128/iai.61.12.5140-5146.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ettinger WH, Varma VK, Sorci-Thomas M, Parks JS, Sigmon RC, Smith TK, et al. Cytokines decrease apolipoprotein accumulation in medium from Hep G2 cells. Arterioscler Thromb. 1994;14:8–13. doi: 10.1161/01.ATV.14.1.8. [DOI] [PubMed] [Google Scholar]
- 16.Khan J, Solakivi T, Seppänen H, Lappalainen-Lehto R, Järvinen S, Ronkainen J, et al. Serum lipid and fatty acid profiles are highly changed in patients with alcohol induced acute pancreatitis. Pancreatology. 2012;12:44–8. doi: 10.1016/j.pan.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 17.Khan J, Nordback I, Sand J. Serum lipid levels are associated with the severity of acute pancreatitis. Digestion. 2013;87:223–8. doi: 10.1159/000348438. [DOI] [PubMed] [Google Scholar]
- 18.Bugdaci MS, Sokmen M, Zuhur SS, Altuntas Y. Lipid profile changes and importance of low serum α-lipoprotein fraction (high-density lipoprotein) in cases with acute pancreatitis. Pancreas. 2011;40:1241–4. doi: 10.1097/MPA.0b013e3182211bbf. [DOI] [PubMed] [Google Scholar]
- 19.Bradley EL., 3rd A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586–90. doi: 10.1001/archsurg.1993.01420170122019. [DOI] [PubMed] [Google Scholar]
- 20.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–52. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Singh VK, Wu BU, Bollen TL, Repas K, Maurer R, Mortele KJ, et al. Early systemic inflammatory response syndrome is associated with severe acute pancreatitis. Clin Gastroenterol Hepatol. 2009;7:1247–51. doi: 10.1016/j.cgh.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 22.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 23.Youden WJ. Index for rating diagnosis tests. Cancer. 1950;3:32–5. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 24.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–48. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 25.Schütte K, Malfertheiner P. Markers for predicting severity and progression of acute pancreatitis. Best Pract Res Clin Gastroenterol. 2008;22:75–90. doi: 10.1016/j.bpg.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 26.Beger HG, Rau BM. Severe acute pancreatitis: Clinical course and management. World J Gastroenterol. 2007;13:5043–51. doi: 10.3748/wjg.v13.i38.5043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ammori BJ, Leeder PC, King RF, Barclay GR, Martin IG, Lavin M, et al. Early increase in intestinal permeability in patients with severe acute pancreatitis: correlation with endotoxemia, organ failure, and mortality. J Gastrointest Surg. 1999;3:252–62. doi: 10.1016/S1091-255X(99)80067-5. [DOI] [PubMed] [Google Scholar]
- 28.Levels JH, Abraham PR, van den Ende A, van Deventer SJ. Distribution and kinetics of lipoprotein-bound endotoxin. Infect Immun. 2001;69:2821–8. doi: 10.1128/IAI.69.5.2821-2828.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murch O, Collin M, Hinds CJ, Thiemermann C. Lipoproteins in inflammation and sepsis. I. Basic science. Intensive Care Med. 2007;33:13–24. doi: 10.1007/s00134-006-0432-y. [DOI] [PubMed] [Google Scholar]
- 30.Unal E, Uzun H, Kusaslan R, Dogan M, Genc H, Gunes P, et al. Serum paraoxonase (a high-density lipoprotein-associated lipophilic antioxidant) activity and lipid profile in experimental acute pancreatitis. Pancreas. 2005;31:84–7. doi: 10.1097/01.mpa.0000168227.74203.e4. [DOI] [PubMed] [Google Scholar]
- 31.Leung PS, Chan YC. Role of oxidative stress in pancreatic inflammation. Antioxid Redox Signal. 2009;11:135–65. doi: 10.1089/ars.2008.2109. [DOI] [PubMed] [Google Scholar]
- 32.Chien JY, Jerng JS, Yu CJ, Yang PC. Low serum level of high-density lipoprotein cholesterol is a poor prognostic factor for severe sepsis. Crit Care Med. 2005;33:1688–93. doi: 10.1097/01.CCM.0000171183.79525.6B. [DOI] [PubMed] [Google Scholar]
- 33.Gordon BR, Parker TS, Levine DM, Saal SD, Wang JC, Sloan BJ, et al. Relationship of hypolipidemia to cytokine concentrations and outcomes in critically ill surgical patients. Crit Care Med. 2001;29:1563–8. doi: 10.1097/00003246-200108000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Tsai MH, Peng YS, Chen YC, Lien JM, Tian YC, Fang JT, et al. Low serum concentration of apolipoprotein A-I is an indicator of poor prognosis in cirrhotic patients with severe sepsis. J Hepatol. 2009;50:906–15. doi: 10.1016/j.jhep.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 35.Tietge UJ, Maugeais C, Lund-Katz S, Grass D. deBeer FC, Rader DJ. Human secretory phospholipase A2 mediates decreased plasma levels of HDL cholesterol and apoA-I in response to inflammation in human apoA-I transgenic mice. Arterioscler Thromb Vasc Biol. 2002;22:1213–8. doi: 10.1161/01.ATV.0000023228.90866.29. [DOI] [PubMed] [Google Scholar]
- 36.Mounzer R, Langmead CJ, Wu BU, Evans AC, Bishehsari F, Muddana V, et al. Comparison of existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Gastroenterology. 2012;142:1476–82. doi: 10.1053/j.gastro.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 37.Wu BU, Bakker OJ, Papachristou GI, Besselink MG, Repas K, van Santvoort HC, et al. Blood urea nitrogen in the early assessment of acute pancreatitis: an international validation study. Arch Intern Med. 2011;171:669–76. doi: 10.1001/archinternmed.2011.126. [DOI] [PubMed] [Google Scholar]
- 38.Muddana V, Whitcomb DC, Khalid A, Slivka A, Papachristou GI. Elevated serum creatinine as a marker of pancreatic necrosis in acute pancreatitis. Am J Gastroenterol. 2009;104:164–70. doi: 10.1038/ajg.2008.66. [DOI] [PubMed] [Google Scholar]


