Abstract
AIM: To investigate variations in the incidence of peptic ulcers (PUs) in Taiwan by day of the week within age subgroups.
METHODS: Ambulatory care data were retrieved from the Longitudinal Health Insurance Database 2000. There were 7204 subjects ≥ 18 years-old with an emergency room admission claim for the treatment of PUs, resulting in a total of 9234 emergency room visits for PUs between 2009 and 2011. Data was divided into the seven days of the week and an additional variable for holidays. One-way analysis of variance was used to examine associations among the daily mean number of PU emergency room admissions and holidays/weekends/weekdays.
RESULTS: One-way analysis of variance showed that there was a significant difference in emergency room admissions for PUs by the day of the week (P < 0.001), with admission more likely to occur on Sundays or holidays than weekdays within the total and working populations. The weekday patterns of admission were similar for the patients aged 18-64 years and ≥ 65 years of age. Holidays, followed by Sundays, had higher PU admissions than the mean daily PU emergency room admissions. Furthermore, inclusion of only those treated for PUs with hemorrhage or perforation, Sundays and holidays had higher mean emergency room admissions than other days. Inclusion of patients who diagnosed with Helicobacter pylori infection, only holidays had higher mean emergency room admissions than other days. Inclusion of patients who had been prescribed non-steroidal anti-inflammatory drugs (NSAIDs) for over 30 d, Sundays and holidays had higher mean PU ER admissions than other non-holiday weekdays.
CONCLUSION: There is a higher incidence of emergency room admission for PUs on weekends than on weekdays for the total and working populations.
Keywords: Chronology, Epidemiology, Peptic ulcer, Weekly pattern
Core tip: This study used a population-based dataset in Taiwan to investigate the variations in peptic ulcer (PU) incidence by day of the week within subgroups defined by age. We identified 7204 subjects ≥ 18 years-old with an emergency room (ER) admission claim for the treatment of PUs, resulting in a total of 9234 ER visits for PU between 2009 and 2011. There was a higher incidence of PU admission on weekends than on weekdays for the total and working populations. Furthermore, Sundays and holidays had higher mean ER admissions than other days for cases of PUs with hemorrhage or perforation.
INTRODUCTION
A peptic ulcer (PU) is a common gastrointestinal tract disorder that is mainly located in the stomach and proximal duodenum[1-3]. Previous studies show that the overall prevalence of PUs varies by country, e.g., 4.1% in northern Sweden[4], 8.4% in the United States[5], and 17.2% in China[6]. In addition, some studies have reported monthly or seasonal variations in PU-related disorders among various regions or countries. An Italian study shows that the number of PU cases is lower in summer than in winter, spring, or autumn[7]. Studies from China and Japan also report that cases of hemorrhage caused by PU increase during the winter and decrease during summer[8-10]. Furthermore, researchers in Turkey have observed a peak in the number of PU incidences in winter, consistent with findings of previous studies[11].
Although prior studies have reported the same pattern of seasonal variation in PU incidence, very few studies have focused on PU onset variation with respect to the daily rhythm of people’s lives. The majority of such studies were also performed in the 1980s. For example, studies in Canada and Israel show a higher incidence of perforated PUs on Tuesdays and Wednesdays[12,13], whereas a study in Scotland revealed a high incidence on Fridays and Saturdays[14], and a Norwegian study found a higher incidence on Thursdays and Fridays[15]. Thus, the results of such chronobiologic studies on the daily variation of PU incidence remain inconsistent.
The main purpose of this population-based study was to investigate the variations in PU incidence in Taiwan by day of the week within subgroups defined by age. If the weekly pattern associated with PU onset could be established, it might provide decisive information for clinicians and ultimately, guide in the development of preventive strategies.
MATERIALS AND METHODS
Data source
Ambulatory care data were retrieved from the Longitudinal Health Insurance Database (LHID2000) published by the Taiwan National Health Research Institute. The LHID2000 includes de-identified claims data on one million randomly selected enrollees of Taiwan’s National Health Insurance program that was designed to be representative of the total enrolled population as of December 2000 (n = 23.72 million), and thus was exempted from full review by the National Defense Medical Center’s Internal Review Board. The Taiwan National Health Research Institute and independent researchers have demonstrated the representative validity of the sample and the high data accuracy of the claims-based LHID2000 on the diagnostic and therapeutic documentation relative to patient charts[16,17].
Study sample
A total of 9234 emergency room (ER) admission claims for the treatment of PU (ICD-9-CM codes 530-531) from 7204 subjects ≥ 18 years-old between January 2009 and December 2011 were identified. Readmission to the ER within seven days of the first visit was not counted, but treated as part of the same episode.
Statistical analysis
The statistical methods of this study were reviewed by Yi-Hua Chen from the School of Public Health of Taipei Medical University. Data analyses were performed with SPSS 10.0 (SPSS Inc., Chicago, IL, United States) statistical software. Data were divided into the seven days of the week, with an additional variable for holidays (defined as national holidays in Taiwan) falling on weekdays or weekends. The daily mean number of incidences of PU ER admissions within the week for the total and each age group (18-64 years old and ≥ 65 years old) is presented.
Subgroup analyses were conducted to investigate daily mean incidences of PU ER admissions in patients who had been diagnosed with Helicobacter pylori (H. pylori) infection (ICD-9-CM code 04186) and in patients who had been prescribed non-steroidal anti-inflammatory drugs (NSAIDs) for > 30 d, which are important factors for young and elderly patients with PUs[18,19].
One-way analysis of variance was used to examine associations between the daily mean number of PU ER admissions and holidays/weekend days/work days. The percentage of variation from the mean daily figures was calculated as: (specific day ER visit number - mean daily visit number)/mean daily visit number. Data are presented as mean ± SD, and statistical significance was set at P ≤ 0.05.
This study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines[20].
RESULTS
Based on the distribution of sample subjects by demographic characteristics, the mean sample age was 57.5 ± 19.8 years (Table 1). Almost half (43.0%) of the sample subjects resided in northern Taiwan, where Taipei, the most populated city and region in Taiwan, is located. Moreover, the lowest income population (36.0%) was more likely to be affected with PU than the highest income population (18.1%). These results might be due to poor standards of hygiene, psychologic stress, and health risk behaviors in the low socioeconomic status population[21].
Table 1.
Demographic characteristics of patients with peptic ulcers admitted to an emergency room in Taiwan between 2009 and 2011 (n = 7204)
| Variable | n (%) |
| Age (yr) | |
| 18-44 | 2426 (33.7) |
| 45-64 | 2211 (30.7) |
| ≥ 65 | 2567 (35.6) |
| Sex | |
| Male | 3842 (53.3) |
| Female | 3362 (46.7) |
| Geographic region | |
| Northern | 3099 (43.0) |
| Central | 1878 (26.1) |
| Southern | 1898 (26.4) |
| Eastern | 329 (4.6) |
| Urbanization level | |
| 1 (most urbanized) | 1796 (24.9) |
| 2 | 1869 (25.9) |
| 3 | 1137 (15.8) |
| 4 | 1182 (16.4) |
| 5 (least urbanized) | 1220 (16.9) |
| Monthly income | |
| NTD 1-15840 | 3308 (45.9) |
| NTD 15841-25000 | 2593 (36.0) |
| ≥ NTD 25001 | 1303 (18.1) |
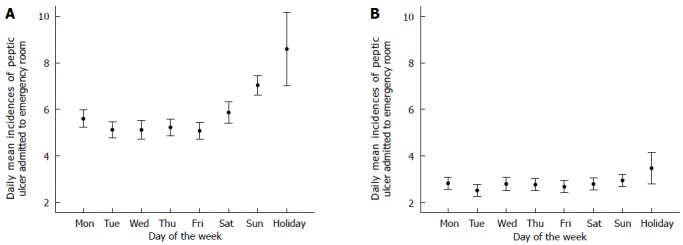
In the period of 2009-2011, there was a total of 9234 ER admissions for PU, with a mean of 8.4 ± 3.1 daily PU ER admissions. The daily mean numbers of PU ER admissions by weekday are presented in Table 2 and Figure 1. Sundays (9.98 ± 3.12) and holidays (12.07 ± 5.01) had higher mean PU ER admissions than other non-holiday weekdays.
Table 2.
Emergency room admissions by weekday of patients with peptic ulcers
| Variable | Mean | SD | Days | Minimum | Maximum |
| Monday | 8.42 | 2.86 | 149 | 2 | 18 |
| Tuesday | 7.63 | 2.74 | 153 | 2 | 15 |
| Wednesday | 7.91 | 3.04 | 152 | 1 | 15 |
| Thursday | 7.99 | 2.80 | 154 | 2 | 15 |
| Friday | 7.75 | 2.73 | 155 | 2 | 17 |
| Saturday | 8.65 | 3.09 | 150 | 2 | 18 |
| Sunday | 9.98 | 3.12 | 152 | 4 | 17 |
| Holiday | 12.07 | 5.01 | 30 | 5 | 22 |
Figure 1.

Daily mean incidences and 95%CI of peptic ulcer admitted to the emergency rooms.
Correspondingly, one-way analysis of variance showed a significant weekly variation of PU onset in the 18-64 years of age group (P < 0.001), but not for the ≥ 65 years of age group. The daily mean incidence of PU ER admissions by age group is presented in Figure 2.
Figure 2.
Daily mean incidences and 95%CI of peptic ulcer admitted to the emergency rooms, by different age groups: 18-64 (A) and ≥ 65 years old (B).
The percent variations of daily admissions of each age group from the mean daily admission during the three-year study period are shown in Figure 3. The patterns of weekday-wise variations were similar for the 18-64 and ≥ 65 years of age groups. The patterns showed an increase on Saturdays and a peak number on holidays; Sundays and holidays had 13.4% and 37.1% higher PU ER admissions, respectively, than the mean daily PU ER admissions.
Figure 3.

Mean daily average percentage variations in peptic ulcer emergency room visits according to age groups (2009-2011).
In addition, limiting the PU ER admissions to those treated for PU with hemorrhage or perforation, Sundays and holidays still had higher mean ER PU admissions than other non-holiday weekdays (Figure 4).
Figure 4.
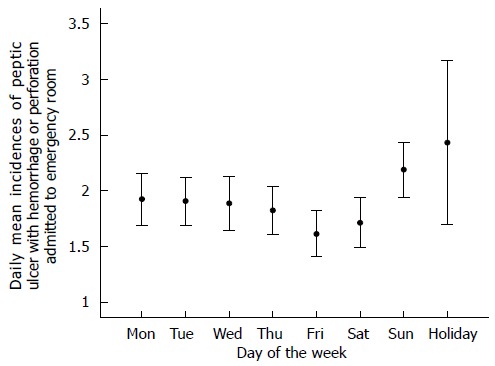
Daily mean incidences and 95%CI of peptic ulcer with hemorrhage or perforation admitted to emergency rooms.
Table 3 presents the daily mean incidences of PU ER admissions for patients diagnosed with H. pylori infection. Only holidays had higher mean PU ER admissions than other non-holiday weekdays and weekends.
Table 3.
Emergency room admissions by weekday of patients with peptic ulcers diagnosed with Helicobacter pylori infection
| Variable | Mean | SD | Days | Minimum | Maximum |
| Monday | 3.35 | 4.56 | 149 | 0 | 16 |
| Tuesday | 2.54 | 4.00 | 153 | 0 | 14 |
| Wednesday | 2.57 | 4.06 | 152 | 0 | 14 |
| Thursday | 3.05 | 4.41 | 154 | 0 | 15 |
| Friday | 2.90 | 4.38 | 155 | 0 | 16 |
| Saturday | 3.33 | 4.88 | 150 | 0 | 18 |
| Sunday | 3.63 | 5.40 | 152 | 0 | 16 |
| Holiday | 5.07 | 7.57 | 30 | 0 | 21 |
Daily mean incidences of PU ER admissions for patients who had been prescribed NSAIDs for over 30 d are shown in Table 4. Sundays and holidays had higher mean PU ER admissions than other non-holiday weekdays.
Table 4.
Emergency room admissions by weekday of patients with peptic ulcers receiving non-steroidal anti-inflammatory drugs for > 30 d
| Variable | Mean | SD | Days | Minimum | Maximum |
| Monday | 3.97 | 4.83 | 149 | 0 | 16 |
| Tuesday | 2.71 | 4.23 | 153 | 0 | 15 |
| Wednesday | 3.81 | 4.80 | 152 | 0 | 15 |
| Thursdays | 3.23 | 4.51 | 154 | 0 | 15 |
| Friday | 3.15 | 4.46 | 155 | 0 | 17 |
| Saturday | 3.61 | 5.16 | 150 | 0 | 18 |
| Sunday | 5.22 | 5.69 | 152 | 0 | 17 |
| Holiday | 9.67 | 6.89 | 30 | 0 | 22 |
DISCUSSION
This population-based study demonstrates a statistically significant variation with days of the week for PU ER admissions. The highest ER admissions of PU with or without complications occur on Sundays and holidays. Similar patterns are also observed for ER admissions of PU with hemorrhage and perforation. Moreover, with further stratification by age, a significant weekly variation of PU onset is observed in the group aged 18-64 years, but not for the group of patients ≥ 65 years.
Numerous studies have investigated diurnal, weekly, or seasonal variations in the onset of different diseases, such as cardiovascular diseases[7,22-24], cerebrovascular diseases[25,26], and psychiatric disorders[27-29], as well as complicated (including hemorrhage and perforation) and uncomplicated PUs[8-11], for which the highest incidences are in winter. This seasonal fluctuation of PU may be affected by several factors, including climatic factors[30], increased intake of NSAIDs in winter[31], significantly increased number of H. pylori infections in winter[32], and variations in alcohol consumption[33]. The importance of the diurnal and weekly rhythms in people’s lives has been emphasized for many years and the associated physiologic variables have recently been identified[34].
The discrepancy of our results with previous studies may be due to several factors. First, all of the preceding studies focused on the onset of perforated PU, whereas the present study included both complicated and uncomplicated PUs. Second, the studies in Canada and Israel used data from selected hospitals, preventing the generalizability of their conclusions[12,13]. Third, most of the studies were conducted before H. pylori was identified. In recent years, the management of PU has improved and the prevalence of H. pylori infection has decreased[35]. Thus, the current fluctuations in PU onset may be different from those reported three decades ago. However, our results of increased PU admissions on weekends and on holidays (defined as off-hour in Taiwan) are in agreement with a recent study in Norway reporting that off-hour admission rates (Saturdays and Sundays and/or during evening and nighttime) of perforated PU are higher than during regular office hours (weekdays and/or daytime)[36].
There are different patterns of weekly variations in PU admission by age in this study. In contrast to the significantly higher PU incidence on weekends and holidays in those 18-64 years of age, the frequency of PU admission is not different between workdays and weekends/holidays in those ≥ 65 years-old. This phenomenon may be due to dissimilar lifestyles of patients in different age groups. In Taiwan, the retirement age for workers is approximately 65 years-old. Moreover, the lifestyle of people aged ≥ 65 years is more consistent across the whole week than in the working population. Thus, the weekly variation in PU admission is not observed in the elderly group.
The strengths of this study include the use of a nationwide population-based dataset, which has a single-payer system and covers 99.6% of the population (23 million) in Taiwan[37]. These features can avoid selection bias. This study also uses the diagnostic codes and medical information from the National Health Insurance database rather than the memory of PU patients, preventing recall bias. However, some limitations should also be noted. First, there is no clinical information or records regarding cigarette smoking, alcohol consumption, or emotional stress, which may all be risk factors for PU onset. Second, some PU patients with mild symptoms may not be admitted to the ER, and thus, will not be recorded in the database. This condition may underestimate the onset of PU in this study. It is difficult for patients with severe PUs to endure the pain and associated complications, such as hemorrhage and perforation. Moreover, it is easy for patients to access medical care in Taiwan due to the National Health Insurance system. In addition, most patients will be admitted to ERs immediately when severe PUs occur. ERs are the only medical care sources available on Saturday afternoons, Sundays, and holidays, which can result in an increase number of ER visits on such days. Nonetheless, ER admission is provided on all days of the week, even at night. Therefore, the working population could receive ER health service after getting off work. Furthermore, patients must have a serious symptom in order to be admitted to the ER for observation in Taiwan. In order to mitigate the potential effect of this issue, the weekly variation for only complicated PUs (including hemorrhage and perforation) was investigated, and its fluctuation is similar to that found for both complicated and uncomplicated PUs.
In conclusion, daily fluctuations over the week are observed in PU ER admission. There is a higher incidence of PU admission on weekends than on weekdays for the total population and working populations. The findings may provide some information for clinicians and government officials. Public health authorities can tailor their health promotion events to include information on how to prepare for high-risk PU days and provide strategies to reduce the risk of PU on weekends and holidays.
COMMENTS
Background
A peptic ulcer (PU) is a common gastrointestinal tract disorder that is mainly located in the stomach and proximal duodenum. Many studies have reported monthly or seasonal variations in PU-related disorders within various regions or countries. However, very few studies have focused on the weekly pattern concerning PU onset.
Research frontiers
The importance of the diurnal and weekly rhythms in people’s lives has been emphasized in recent years, and the associated physiologic variables have been identified. However, relevant studies on the weekly fluctuation of PU onset are still limited.
Innovations and breakthroughs
This study demonstrates a statistically significant variation over the days of the week for PU emergency room (ER) admissions. The highest ER admissions for PU with or without complications occur on Sundays and holidays. Similar patterns are also observed for ER admissions of PU with hemorrhage and perforation. Moreover, with further stratification by age, a significant weekly variation of PU admission is observed in the working population.
Applications
Daily fluctuations over the week are observed in PU ER admission. There is a higher incidence of PU admission on weekends than on weekdays for the total and working populations. The findings may provide some information for clinicians and government officials. Public health authorities can tailor their health promotion events to include information on how to prepare for high-risk PU days, and to provide strategies to reduce the risk of PU on weekends and holidays.
Peer-review
This is a good population-based study in which the authors observed the fluctuation of PU ER admissions over the week. The results of this study showed that higher incidence of PU admission occurs on weekends than on weekdays for the total and working populations.
Footnotes
Ethics approval: This study was based on de-identified secondary data from the LHID2000 released to the public for research purposes, and thus was exempted from full review by the National Defense Medical Center’s Internal Review Board.
Informed consent: This study retrieved data from an administrative dataset. Therefore, informed consent was not needed.
Conflict-of-interest: The authors declare no conflicts of interest.
Data sharing: The LHID2000, which is open to researchers, is available from the National Health Research Institute of Taiwan (http://nhird.nhri.org.tw/date_01.html); dataset available from nhird@nhri.org.tw.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 8, 2014
First decision: November 26, 2014
Article in press: January 8, 2015
P- Reviewer: Matsuda A, Tripathi D, Xu JM S- Editor: Qi Y L- Editor: AmEditor E- Editor: Zhang DN
References
- 1.Najm WI. Peptic ulcer disease. Prim Care. 2011;38:383–394, vii. doi: 10.1016/j.pop.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician. 2007;76:1005–1012. [PubMed] [Google Scholar]
- 3.Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449–1461. doi: 10.1016/S0140-6736(09)60938-7. [DOI] [PubMed] [Google Scholar]
- 4.Aro P, Storskrubb T, Ronkainen J, Bolling-Sternevald E, Engstrand L, Vieth M, Stolte M, Talley NJ, Agréus L. Peptic ulcer disease in a general adult population: the Kalixanda study: a random population-based study. Am J Epidemiol. 2006;163:1025–1034. doi: 10.1093/aje/kwj129. [DOI] [PubMed] [Google Scholar]
- 5.Garrow D, Delegge MH. Risk factors for gastrointestinal ulcer disease in the US population. Dig Dis Sci. 2010;55:66–72. doi: 10.1007/s10620-008-0708-x. [DOI] [PubMed] [Google Scholar]
- 6.Li Z, Zou D, Ma X, Chen J, Shi X, Gong Y, Man X, Gao L, Zhao Y, Wang R, et al. Epidemiology of peptic ulcer disease: endoscopic results of the systematic investigation of gastrointestinal disease in China. Am J Gastroenterol. 2010;105:2570–2577. doi: 10.1038/ajg.2010.324. [DOI] [PubMed] [Google Scholar]
- 7.Manfredini R, Manfredini F, Boari B, Bergami E, Mari E, Gamberini S, Salmi R, Gallerani M. Seasonal and weekly patterns of hospital admissions for nonfatal and fatal myocardial infarction. Am J Emerg Med. 2009;27:1097–1103. doi: 10.1016/j.ajem.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Du T, Lewin MR, Wang H, Ji X, Bohn HH, Xu T, Xu L, Zhang Y, Li Y. Circadian and seasonal rhythms of acute upper gastrointestinal bleeding in Beijing. Emerg Med J. 2010;27:504–507. doi: 10.1136/emj.2009.075820. [DOI] [PubMed] [Google Scholar]
- 9.Chen J, Li D, Xu S, Sun Z, Wang B, Deng C. Influence of meteorological factors on the seasonal onset of esophagogastric variceal bleeding. O J Gas. 2013;3:134–137. [Google Scholar]
- 10.Nomura T, Ohkusa T, Araki A, Chuganji Y, Momoi M, Takashimizu I, Watanabe M. Influence of climatic factors in the incidence of upper gastrointestinal bleeding. J Gastroenterol Hepatol. 2001;16:619–623. doi: 10.1046/j.1440-1746.2001.02486.x. [DOI] [PubMed] [Google Scholar]
- 11.Kocer B, Surmeli S, Solak C, Unal B, Bozkurt B, Yildirim O, Dolapci M, Cengiz O. Factors affecting mortality and morbidity in patients with peptic ulcer perforation. J Gastroenterol Hepatol. 2007;22:565–570. doi: 10.1111/j.1440-1746.2006.04500.x. [DOI] [PubMed] [Google Scholar]
- 12.Cohen MM. Perforated peptic ulcer in the Vancouver area: a survey of 852 cases. Can Med Assoc J. 1971;104:201–205. [PMC free article] [PubMed] [Google Scholar]
- 13.Lazarus S. Perforated peptic ulcer in israel. Gut. 1964;5:590–596. doi: 10.1136/gut.5.6.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jamieson RA. Acute perforated peptic ulcer; frequency and incidence in the West of Scotland. Br Med J. 1955;2:222–227. doi: 10.1136/bmj.2.4933.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Svanes C, Sothern RB, Sørbye H. Rhythmic patterns in incidence of peptic ulcer perforation over 5.5 decades in Norway. Chronobiol Int. 1998;15:241–264. doi: 10.3109/07420529808998687. [DOI] [PubMed] [Google Scholar]
- 16.Kang JH, Chen YH, Lin HC. Comorbidity profiles among patients with ankylosing spondylitis: a nationwide population-based study. Ann Rheum Dis. 2010;69:1165–1168. doi: 10.1136/ard.2009.116178. [DOI] [PubMed] [Google Scholar]
- 17.Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20:236–242. doi: 10.1002/pds.2087. [DOI] [PubMed] [Google Scholar]
- 18.Rosenstock S, Jørgensen T, Bonnevie O, Andersen L. Risk factors for peptic ulcer disease: a population based prospective cohort study comprising 2416 Danish adults. Gut. 2003;52:186–193. doi: 10.1136/gut.52.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet. 2002;359:14–22. doi: 10.1016/S0140-6736(02)07273-2. [DOI] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Bytzer P, Howell S, Leemon M, Young LJ, Jones MP, Talley NJ. Low socioeconomic class is a risk factor for upper and lower gastrointestinal symptoms: a population based study in 15 000 Australian adults. Gut. 2001;49:66–72. doi: 10.1136/gut.49.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herlitz J, Eek M, Holmberg M, Holmberg S. Diurnal, weekly and seasonal rhythm of out of hospital cardiac arrest in Sweden. Resuscitation. 2002;54:133–138. doi: 10.1016/s0300-9572(02)00097-7. [DOI] [PubMed] [Google Scholar]
- 23.Eng H, Mercer JB. Seasonal variations in mortality caused by cardiovascular diseases in Norway and Ireland. J Cardiovasc Risk. 1998;5:89–95. [PubMed] [Google Scholar]
- 24.Arntz HR, Willich SN, Schreiber C, Brüggemann T, Stern R, Schultheiss HP. Diurnal, weekly and seasonal variation of sudden death. Population-based analysis of 24,061 consecutive cases. Eur Heart J. 2000;21:315–320. doi: 10.1053/euhj.1999.1739. [DOI] [PubMed] [Google Scholar]
- 25.Manfredini R, Casetta I, Paolino E, la Cecilia O, Boari B, Fallica E, Granieri E. Monday preference in onset of ischemic stroke. Am J Med. 2001;111:401–403. doi: 10.1016/s0002-9343(01)00836-1. [DOI] [PubMed] [Google Scholar]
- 26.Wang H, Sekine M, Chen X, Kagamimori S. A study of weekly and seasonal variation of stroke onset. Int J Biometeorol. 2002;47:13–20. doi: 10.1007/s00484-002-0147-x. [DOI] [PubMed] [Google Scholar]
- 27.Marriott PF, Greenwood KM, Armstrong SM. Seasonality in panic disorder. J Affect Disord. 1994;31:75–80. doi: 10.1016/0165-0327(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 28.Bulbena A, Pailhez G, Aceña R, Cunillera J, Rius A, Garcia-Ribera C, Gutiérrez J, Rojo C. Panic anxiety, under the weather? Int J Biometeorol. 2005;49:238–243. doi: 10.1007/s00484-004-0236-0. [DOI] [PubMed] [Google Scholar]
- 29.Geoffroy PA, Bellivier F, Scott J, Etain B. Seasonality and bipolar disorder: a systematic review, from admission rates to seasonality of symptoms. J Affect Disord. 2014;168:210–223. doi: 10.1016/j.jad.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Liu DY, Gao AN, Tang GD, Yang WY, Qin J, Wu XG, Zhu DC, Wang GN, Liu JJ, Liang ZH. Relationship between onset of peptic ulcer and meteorological factors. World J Gastroenterol. 2006;12:1463–1467. doi: 10.3748/wjg.v12.i9.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Langman MI. The seasonal incidence of bleeding from the upper gastrointestinal tract. Gut. 1964;5:142–144. doi: 10.1136/gut.5.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moshkowitz M, Konikoff FM, Arber N, Peled Y, Santo M, Bujanover Y, Gilat T. Seasonal variation in the frequency of Helicobacter pylori infection: a possible cause of the seasonal occurrence of peptic ulcer disease. Am J Gastroenterol. 1994;89:731–733. [PubMed] [Google Scholar]
- 33.Manfredini R, De Giorgio R, Smolensky MH, Boari B, Salmi R, Fabbri D, Contato E, Serra M, Barbara G, Stanghellini V, et al. Seasonal pattern of peptic ulcer hospitalizations: analysis of the hospital discharge data of the Emilia-Romagna region of Italy. BMC Gastroenterol. 2010;10:37. doi: 10.1186/1471-230X-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tuomisto MT, Terho T, Korhonen I, Lappalainen R, Tuomisto T, Laippala P, Turjanmaa V. Diurnal and weekly rhythms of health-related variables in home recordings for two months. Physiol Behav. 2006;87:650–658. doi: 10.1016/j.physbeh.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 35.Sung JJ, Kuipers EJ, El-Serag HB. Systematic review: the global incidence and prevalence of peptic ulcer disease. Aliment Pharmacol Ther. 2009;29:938–946. doi: 10.1111/j.1365-2036.2009.03960.x. [DOI] [PubMed] [Google Scholar]
- 36.Thorsen K, Søreide JA, Kvaløy JT, Glomsaker T, Søreide K. Epidemiology of perforated peptic ulcer: age- and gender-adjusted analysis of incidence and mortality. World J Gastroenterol. 2013;19:347–354. doi: 10.3748/wjg.v19.i3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bureau of National Health Insurance. Universal Health Coverage in Taiwan, May 2012. Available from: http://www.nhi.gov.tw/Resource/webdata/21717_1_20120808UniversalHealthCoverage.pdf.


