Abstract
AIM: To evaluate the diagnostic accuracy of magnetic resonance cholangiopancreatography (MRCP) in patients with choledocholithiasis.
METHODS: We systematically searched MEDLINE, EMBASE, Web of Science, and Cochrane databases for studies reporting on the sensitivity, specificity and other accuracy measures of diagnostic effectiveness of MRCP for detection of common bile duct (CBD) stones. Pooled analysis was performed using random effects models, and receiver operating characteristic curves were generated to summarize overall test performance. Two reviewers independently assessed the methodological quality of studies using standards for reporting diagnostic accuracy and quality assessment for studies of diagnostic accuracy tools.
RESULTS: A total of 25 studies involving 2310 patients with suspected choledocholithiasis and 738 patients with CBD stones met the inclusion criteria. The average inter-rater agreement on the methodological quality checklists was 0.96. Pooled analysis of the ability of MRCP to detect CBD stones showed the following effect estimates: sensitivity, 0.90 (95%CI: 0.88-0.92, χ2 = 65.80; P < 0.001); specificity, 0.95 (95%CI: 0.93-1.0, χ2 = 110.51; P < 0.001); positive likelihood ratio, 13.28 (95%CI: 8.85-19.94, χ2 = 78.95; P < 0.001); negative likelihood ratio, 0.13 (95%CI: 0.09-0.18, χ2 = 6.27; P < 0.001); and diagnostic odds ratio, 143.82 (95%CI: 82.42-250.95, χ2 = 44.19; P < 0.001). The area under the receiver operating characteristic curve was 0.97. Significant publication bias was not detected (P = 0.266).
CONCLUSION: MRCP has high diagnostic accuracy for the detection of choledocholithiasis. MRCP should be the method of choice for suspected cases of CBD stones.
Keywords: Choledocholithiasis, Diagnosis, Magnetic resonance cholangiopancreatography, Common bile duct, Meta-analysis
Core tip: Unlike endoscopic retrograde cholangiopancreatography, magnetic resonance cholangiopancreatography (MRCP) is noninvasive, can be performed rapidly and has demonstrated good results for the detection of common bile duct stones. Moreover, MRCP does not expose patients to ionizing radiation or iodinated contrast media, which is useful for evaluating biliopancreatic disease. However, the selective use of MRCP in clinically equivocal situations has not been explored until now. The goal of this study was to evaluate the effectiveness of MRCP for the detection of common bile duct stones in patients with suspected choledocholithiasis.
INTRODUCTION
The incidence of choledocholithiasis in patients with the common disorder, cholelithiasis, varies between 7% and 20%, of which 5% are asymptomatic[1,2]. Although common bile duct (CBD) stones may be silent, the development of complications such as cholangitis and acute pancreatitis is associated with major morbidity and mortality. Therefore, the detection and treatment of CBD stones is mandatory.
Usually, the diagnosis of choledocholithiasis is based on a combination of clinical suspicion (biliary colic, jaundice and cholangitis), biochemical analysis (raised conjugated bilirubin and alkaline phosphatase levels) and imaging findings. Individually, these indicators have varying levels of diagnostic accuracy and none represent a completely reliable method for identifying bile duct stones[3]. Intraoperative cholangiography (IOC) is standard procedure during open cholecystectomy that can detect CBD stones with a sensitivity of 100% and specificity of 98%[4]. It is an invasive investigation with intraoperative and postoperative morbidity of 6.3% and 15.9%, respectively. Its routine use is associated with increased cost and operating time[5].
Endoscopic retrograde cholangiopancreatography (ERCP) is the gold standard for both diagnosis and treatment of CBD stones. It also allows direct visualization of duct anatomy. However, the procedure is associated with an overall complication rate of 5%-10% and mortality rate of 0.02%-0.50%[6-8]. Ductal cannulation is difficult or impossible in patients who have undergone previous surgery, which includes Billroth type II gastrectomy and hepaticoenterostomy. Early ERCP and stone extraction after endoscopic sphincterotomy decrease morbidity in patients with severe biliary pancreatitis. However, ERCP and endoscopic sphincterotomy are invasive procedures that may cause serious complications[7,9] and can potentially exacerbate acute pancreatitis[6]. Therefore, an accurate, safe, and efficacious method is needed to diagnose CBD stones in a definitive manner.
The diagnostic accuracy of endoscopic ultrasonography (EUS) for biliary tract stone disease is > 95%, which is less invasive than ERCP and is reliable at identifying bile duct stones[10-13]. However, its results are highly dependent on the operator, and the procedure is not widely available in clinical practice. In addition, visualization of all segments of the biliary tract may be incomplete or unsuccessful during EUS[11].
In many institutions, magnetic resonance cholangiopancreatography (MRCP) is replacing ERCP as a diagnostic procedure for the investigation of benign biliary obstructions and chronic pancreatitis, in part due to its comparable accuracy[14]. MRCP has an advantage because of its technical versatility, multiplanar capability, superior soft tissue resolution, and the potential to evaluate choledocholithiasis accurately in the preoperative acute calculous cholecystitis setting. Unlike ERCP, MRCP is noninvasive, can be performed rapidly, does not expose the patients to ionizing radiation or iodinated contrast materials[15], which is useful for evaluating biliopancreatic disease, and has good results for detecting CBD stones[16]. All segments of the biliary tree can be visualized using MRCP. Although ERCP is considered the standard for diagnosis of bile duct stones, small bile duct stones can be overlooked[17]. However, the selective use of MRCP in clinically equivocal situations has not been explored until now. The goal of this study was, therefore, to rigorously evaluate the effectiveness of MRCP for detection of CBD stones in patients with suspected choledocholithiasis via systematic review and meta-analysis.
MATERIALS AND METHODS
Search strategy
In March 2014, we searched MEDLINE (1980-2014), EMBASE (1980-2014), Web of Science (1990-2014) and Cochrane databases to identify studies. Although no language restrictions were imposed initially, only English-language articles were included for the full-text review and final analysis. Additional articles were searched using the “Related articles” function in PubMed and by manually searching reference lists of identified articles and review articles. The following search terms were used: “magnetic resonance cholangiopancreatography” or “MRCP” and “common bile duct” or “choledocholithiasis” and “diagnosis” and “sensitivity” and “specificity.” We contacted experts in the field to ask about studies that we may have missed in the databases. Conference abstracts and letters to the editor were excluded because of the limited data they contained.
Study inclusion criteria
A study was included when it provided both the sensitivity (true-positive rate) and specificity (false-positive rate) of using MRCP for detection of CBD stones in patients of any age with suspected choledocholithiasis. Studies were also included if they reported the values of MRCP effectiveness in a scatter plot format that allowed patient data to be extracted. Studies were excluded if they involved fewer than ten patients with suspected choledocholithiasis to reduce selection bias due to small numbers of participants. Patients had to be diagnosed with choledocholithiasis based on ERCP and/or IOC. Two reviewers (Mo JJ, Lin L) independently determined study eligibility, and disagreements were resolved by consensus.
Data extraction and quality assessment
Two reviewers (Mo JJ, Lin L) independently confirmed the eligibility of the final set of studies and extracted the following data: first author, publication year, participant characteristics, assay methods, sensitivity and specificity data, and methodological quality. The values of MRCP effectiveness provided in scatter plots were extracted by placing scalar grids over the plots. A receiver operating characteristic (ROC) curve was calculated for each study (IBM Inc., Armonk, NY, United States).
To enable us to assess the methodological quality of the included studies, we extracted data on the following study design characteristics: (1) cross-sectional or case-control design; (2) consecutive or random sampling of patients; (3) blinded (single or double) or non-blinded interpretation of experimental and reference measurements; and (4) prospective or retrospective data collection. The two reviewers (Mo JJ, Lin L) independently assessed the methodological quality of studies using the standards for reporting diagnostic accuracy (STARD) guidelines[18], which provide for a maximum score of 25, and quality assessment for studies of diagnostic accuracy (QUADAS) guidelines[19], which provide for a maximum score of 14. Average inter-rater agreement on the methodological quality checklists was 0.96. If primary studies did not report information needed to assess methodological quality, we contacted the authors in an effort to obtain the data. If the authors did not respond, we changed the response for the relevant items from “not reported” to “no” on the assessment instruments.
Statistical analysis
Standard methods recommended for meta-analyses of diagnostic test evaluations were used[20]. Analyses were performed using professional statistical software program (Meta-DiSc for Windows; XI Cochrane Colloquium; Barcelona, Spain) and Stata version 12.0 (Stata Corporation, College Station, TX, United States). The following measures of test accuracy were analyzed for each study: sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR) and diagnostic odds ratio (DOR). A summary ROC (SROC) curve[21] was generated for each study based on a single test threshold for sensitivity and specificity[20,22]. A random effects model was adopted to calculate the average sensitivity, specificity, and other measures across studies[23,24].
To assess the effects of STARD and QUADAS scores on the diagnostic power of MRCP, we included them as covariates in a univariate, inverse variance-weighted meta-regression. We also analyzed the effects of other covariates on DOR, such as cross-sectional design, consecutive or random sampling of patients, single- or double-blinded interpretation of experimental and reference measurements, and prospective or retrospective data collection. The relative DOR (RDOR) was calculated to analyze the change in diagnostic precision in each study per unit increase in the covariate[25,26].
The heterogeneity, or variability, across studies was assessed for statistical significance using the χ2 and Fisher’s exact tests. Publication bias can pose problems for meta-analyses of diagnostic studies, therefore, we tested for the potential presence of this bias with funnel plots and the Egger’s test[27].
RESULTS
Selection and summary of studies
We identified 292 citations via electronic searches, and 40 were retrieved for detailed analysis (Figure 1). Six studies were excluded for failing to satisfy the inclusion criteria[28-33], and another three were excluded because they failed to provide sufficient information[34-36]. Two articles were meta-analyses[37,38]. One paper was excluded because it was a Chinese study[39]. One study was a duplicate publication[3]. One study was excluded for being a reply letter[40] and one paper was excluded for involving fewer than 10 participants[41]. In the end, 25 publications were included in the analysis[42-66], involving 2310 patients with suspected choledocholithiasis and 738 with CBD stones. The average sample size of the studies was 69 patients (range: 27-278). Table 1 summarizes the clinical characteristics of participants in each study; numbers of true positives, false positives, false negatives and true negatives; and STARD and QUADAS scores.
Figure 1.
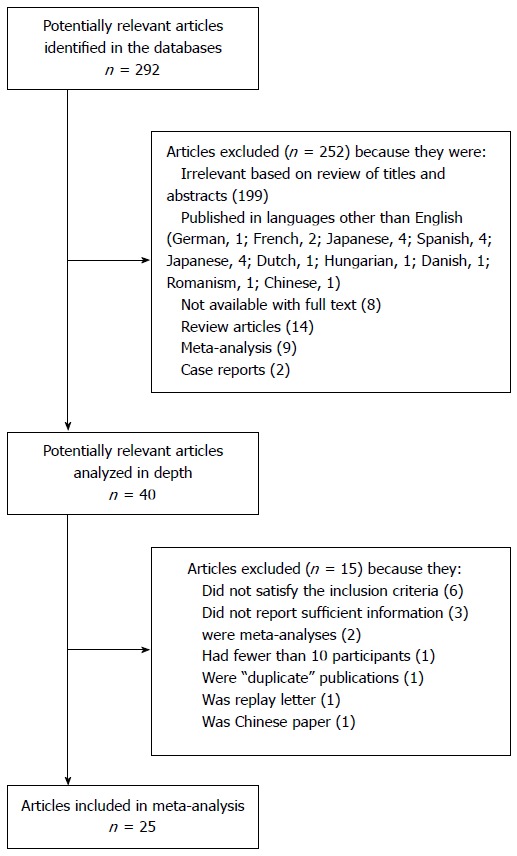
Flow chart of study selection.
Table 1.
Summarized details of magnetic resonance cholangiopancreatography detections and overall methodological quality of included studies
| Ref. | Year | Patients, n | Assay method | Assay system |
Assay results |
Quality score |
||||
| TP | FP | FN | TN | STARD | QUADAS | |||||
| Hochwald et al[42] | 1998 | 48 | MRCP, ERCP | 1.5 T machine | 19 | 3 | 1 | 25 | 15 | 11 |
| Boraschi et al[43] | 1999 | 278 | MRCP, ERCP | 1.5 T MR unit | 71 | 5 | 5 | 197 | 16 | 11 |
| de Lédinghen et al[44] | 1999 | 32 | EUS, MRCP, ERCP | 1 T system | 10 | 6 | 0 | 16 | 20 | 13 |
| Lomas et al[45] | 1999 | 69 | MRCP, ERCP | 1.5 T MR system | 9 | 2 | 0 | 58 | 13 | 9 |
| Varghese et al[46] | 1999 | 100 | MRCP, ERCP | 1.5 GE unit | 28 | 1 | 2 | 69 | 17 | 12 |
| Stiris et al[47] | 2000 | 50 | MRCP, ERCP | 1.0 T | 28 | 1 | 4 | 17 | 17 | 12 |
| Taylor et al[48] | 2002 | 129 | MRCP, ERCP | 1.5 T MR system | 45 | 9 | 1 | 74 | 18 | 12 |
| Topal et al[49] | 2003 | 69 | MRCP, ERCP | 1.5 T MR system | 18 | 0 | 1 | 50 | 14 | 10 |
| Kejriwal et al[50] | 2004 | 81 | MRCP, ERCP | Vision 1.5T MRI | 20 | 1 | 2 | 58 | 13 | 10 |
| Simone et al[51] | 2004 | 65 | MRCP, ERCP, IOC | 1.0 T gyroscan NT | 13 | 6 | 8 | 38 | 13 | 9 |
| Dalton et al[52] | 2005 | 69 | MRCP, ERCP, IOC | 1.5 T MR unit | 16 | 2 | 1 | 50 | 11 | 7 |
| Hallal et al[53] | 2005 | 27 | MRCP, ERCP, IOC | Unknown | 4 | 2 | 0 | 21 | 14 | 10 |
| Kondo et al[54] | 2005 | 28 | EUS, MRCP, HCT-C | 1.5 T MR system | 21 | 1 | 3 | 3 | 18 | 13 |
| Moon et al[55] | 2005 | 29 | IDUS, MRCP, ERCP | 1.5T MR system | 16 | 1 | 4 | 8 | 17 | 11 |
| Okada et al[56] | 2005 | 40 | CTCh, MRCP | 1.5 T system | 12 | 3 | 3 | 22 | 13 | 9 |
| Shanmugam et al[57] | 2005 | 221 | MRCP, ERCP, EUS | 0.5 T MRI | 97 | 19 | 2 | 103 | 18 | 14 |
| De Waele et al[58] | 2007 | 104 | MRCP, ERCP, EUS | 1.5 T unit | 19 | 2 | 4 | 79 | 16 | 11 |
| Schmidt et al[59] | 2007 | 57 | MRCP, ERCP, EUS | 1 T magnet | 17 | 2 | 5 | 33 | 15 | 10 |
| Hekimoglu et al[60] | 2008 | 269 | MRCP, ERCP | 1.5 T unit | 16 | 0 | 2 | 251 | 19 | 14 |
| Nandalur et al[61] | 2008 | 95 | MRCP, ERCP | 1.5 T system | 21 | 1 | 7 | 66 | 18 | 13 |
| Norero et al[62] | 2008 | 125 | MRCP, ERCP, CT | 1.5 T MR system | 83 | 10 | 3 | 29 | 15 | 11 |
| Srinivasa et al[63] | 2010 | 117 | MRCP, ERCP, IOC | Siemens Vision 1.5 T | 15 | 2 | 8 | 102 | 16 | 12 |
| Bilgin et al[64] | 2012 | 108 | MRCP, ERCP, IOC | 1.5 T MR scanner | 28 | 3 | 6 | 71 | 16 | 11 |
| Zhang et al[65] | 2012 | 70 | MRCP, MDCT | 1.5 T MR system | 19 | 2 | 1 | 48 | 18 | 13 |
| Mandelia et al[66] | 2013 | 30 | MRCP, USG | 1.5 T MR system | 19 | 1 | 1 | 9 | 17 | 12 |
CT: Computed tomography; CTCh: Cholangiography computed tomography; ERCP: Endoscopic retrograde cholangiopancreatography; EUS: Endoscopic ultrasonography; FN: False-negative; FP: False-positive; HCT-C: Helical-computed-tomographic cholangiography; IDUS: Intraductal ultrasonography; IOC: Intraoperative cholangiography; MDCT: Multidetector-row computed tomography; MR: Magnetic resonance; MRCP: Magnetic resonance cholangiopancreatography; QUADAS: Quality assessment for studies of diagnostic accuracy; STARD: Standards for reporting diagnostic accuracy; TN: True-negative; TP: True-positive; USG: Ultrasonography.
Methodological quality of the included studies
Of the 25 studies in the meta-analysis, 23 had STARD scores ≥ 13, and 21 had QUADAS scores ≥ 10. All studies collected data from consecutive patients. There were nine randomized, prospective, blinded trials according to the corresponding reference measurements (Table 2).
Table 2.
Additional characteristics of patients and methodologies in the included studies
| Ref. | Year | Country | CBD/N-CBD, n | Reference standard | Cross-sectional design | Consecutive or random sampling | Blinded design | Prospective design |
| Hochwald et al[42] | 1998 | United States | 20/28 | ERCP | No | Yes | No | No |
| Boraschi et al[43] | 1999 | Italy | 76/202 | ERCP, PTC, IOC | No | Yes | No | No |
| de Lédinghen et al[44] | 1999 | France | 10/-22 | ERCP, IOC | Yes | Yes | Yes | Yes |
| Lomas et al[45] | 1999 | United Kingdom | 9/60 | ERCP | No | Yes | No | Yes |
| Varghese et al[46] | 1999 | Ireland | 30/70 | ERCP | No | Yes | Yes | Yes |
| Stiris et al[47] | 2000 | Norway | 32/18 | ERCP | Yes | Yes | Yes | Yes |
| Taylor et al[48] | 2002 | Australia | 46/83 | ERCP | Yes | Yes | Yes | Yes |
| Topal et al[49] | 2003 | Belgium | 19/50 | ERCP, IOC | No | Yes | No | No |
| Kejriwal et al[50] | 2004 | New Zealand | 22/59 | ERCP | No | Yes | No | No |
| Simone et al[51] | 2004 | France | 21/44 | ERCP, IOC | No | Yes | Yes | Yes |
| Dalton et al[52] | 2005 | United Kingdom | 17/52 | ERCP, IOC | No | Yes | No | Yes |
| Hallal et al[53] | 2005 | United States | 4/-23 | IOC | Yes | Yes | Yes | Yes |
| Kondo et al[54] | 2005 | Japan | 24/-4 | ERCP | Yes | Yes | Yes | Yes |
| Moon et al[55] | 2005 | South Korea | 20/-9 | ERCP, IDUS | No | Yes | Yes | Yes |
| Okada et al[56] | 2005 | Japan | 15/25 | IOC | No | Yes | Yes | No |
| Shanmugam et al[57] | 2005 | United Kingdom | 99/122 | ERCP, IOC | Yes | Yes | No | No |
| De Waele et al[58] | 2007 | Belgium | 23/81 | ERCP, IOC | No | Yes | No | Yes |
| Schmidt et al[59] | 2007 | Switzerland | 22/35 | EUS, ERCP | No | Yes | No | Yes |
| Hekimoglu et al[60] | 2008 | Turkey | 18/251 | ERCP | No | Yes | Yes | Yes |
| Nandalur et al[61] | 2008 | United States | 28/67 | ERCP, PTC | Yes | Yes | No | No |
| Norero et al[62] | 2008 | Chile | 86/39 | ERCP | No | Yes | No | No |
| Srinivasa et al[63] | 2010 | Australia | 23/104 | ERCP, IOC | No | Yes | No | No |
| Bilgin et al[64] | 2012 | Turkey, Germany | 34/74 | ERCP, PTC | No | Yes | No | No |
| Zhang et al[65] | 2012 | China | 20/50 | MDCT | No | Yes | Yes | No |
| Mandelia et al[66] | 2013 | India | 20/-10 | ERCP | No | Yes | No | Yes |
CBD: Common bile duct; ERCP: Endoscopic retrograde cholangiopancreatography; EUS: Endoscopic ultrasonography; IDUS: Intraductal ultrasonography; IOC: Intraoperative cholangiography; MDCT: Multidetector-row computed-tomography; PTC: Percutaneous transhepatic cholangiography.
Diagnostic accuracy
A Forest plot of MRCP values in all 25 included studies showed that the sensitivity of MRCP in detection of CBD stones ranged from 0.38 to 1.0 (mean 0.90, 95%CI: 0.88-0.92, χ2 = 65.80; P < 0.001), while the specificity ranged from 0.19 to 1.0 (mean 0.95, 95%CI: 0.93-1.00, χ2 = 110.51; P < 0.001) (Figure 2). The PLR was 13.28 (95%CI: 8.85-19.94, χ2 = 78.95; P < 0.001), NLR was 0.13 (95%CI: 0.09-0.18, χ2 = 66.27; P < 0.001) and DOR was 143.82 (95%CI: 82.42-250.95, χ2 = 44.19; P < 0.001). These χ2 and associated P values indicate significant heterogeneity among studies. The ten randomized controlled trials (RCTs) showed that the sensitivity, specificity, PLR, NLR and DOR of MRCP in detection of CBD stones was 0.91, 0.95, 10.83, 0.13 and 136.32, respectively.
Figure 2.
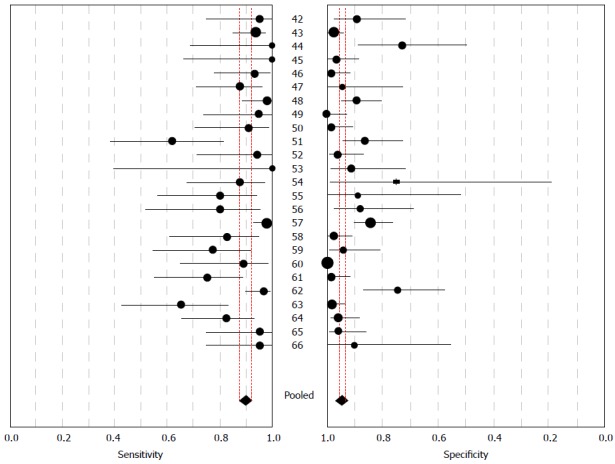
Forest plot showing sensitivity and specificity of magnetic resonance cholangiopancreatography in the diagnosis of choledocholithiasis. The point estimates of sensitivity and specificity from each study are shown as solid circles. Horizontal error bars indicate 95%CIs. Numbers between the plots refer to references. Pooled estimates for the magnetic resonance cholangiopancreatography detections were 0.90 for sensitivity (95%CI: 0.88-0.92) and 0.95 for specificity (95%CI: 0.93-1.0).
Unlike the traditional ROC plot for assessing diagnostic power, an SROC plot reveals the effect of varying thresholds on sensitivity and specificity in a single study. Different studies appear as different data points in an SROC plot. In this way, SROC curves provide a global summary of test performance and illustrate the trade-off between sensitivity and specificity. Figure 3 shows an SROC curve for rates of true and false positives from individual studies of MRCP detection. Using this plot, we determined the Q value, defined as the point of intersection of the SROC curve with a diagonal line extending from the left upper corner to the right lower corner of the plot. The Q value indicates the highest identical value of sensitivity and specificity, thereby serving as an overall measure of the discriminatory power of a test. Our SROC curve was desirably positioned near the upper left corner, and the maximum joint sensitivity and specificity was 0.92. The area under the curve was 0.97, indicating high overall accuracy.
Figure 3.
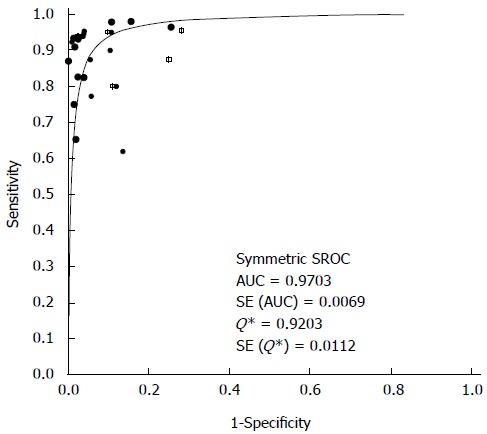
Summary receiver operating characteristic curves for magnetic resonance cholangiopancreatography detection. Solid circles represent each study included in the meta-analysis. The size of each study is indicated by the size of the solid circle. Summary receiver operating characteristic (SROC) curves summarize the overall diagnostic accuracy; AUC: Area under the curve.
Multiple regression analysis and publication bias
Quality scores based on the STARD[18] and QUADAS[19] guidelines were generated for every study on the basis of the title and introduction, methods, results and discussion (Table 1). These scores were used in a meta-regression to assess the effect of study quality on the RDOR of MRCP in the diagnosis of CBD stones. As shown in Table 3, studies of higher quality (STARD score ≥ 13; QUADAS score ≥ 10) produced RDOR values similar to those of lower-quality studies. In addition, RDOR values did not differ significantly as a function of blinding, cross-sectional or case-control design, consecutive or random sampling, prospective or retrospective design (all P > 0.05). These results suggest that study design did not significantly affect diagnostic accuracy and that the risk of detection bias was lower. The Egger’s test showed no evidence of significant publication bias in the reporting of MRCP detection as a method for diagnosis of CBD stones (P = 0.266).
Table 3.
Weighted meta-regression for the effects of design, methods and quality of studies on diagnostic accuracy of magnetic resonance cholangiopancreatography detections
| Covariate | Studies (n) | Coefficient | RDOR (95%CI) | P value |
| QUADAS ≥ 10 | 21 | 0.0830 | 1.09 (0.14-8.50) | 0.9334 |
| STARD ≥ 13 | 23 | 1.5100 | 4.53 (0.51-40.21) | 0.1637 |
| Prospective design | 14 | 0.1260 | 1.13 (0.27-4.82) | 0.8564 |
| Cross-sectional design | 7 | 0.0980 | 1.10 (0.24-5.06) | 0.8936 |
| Blinded design | 11 | -0.6850 | 0.50 (0.13-2.02) | 0.3130 |
| Consecutive/random sampling | 25 | - | - | - |
RDOR: Relative diagnostic odds ratio; STARD: Standards for reporting diagnostic accuracy; QUADAS: Quality assessment for studies of diagnostic accuracy.
DISCUSSION
Although MRCP can provide an accurate diagnosis of CBD stones, only a few investigators have evaluated its utility in the preoperative evaluation of symptomatic gallstones. Accordingly, the precise role of MRCP in this regard has yet to be determined. Some authors recommend MRCP for patients with a moderate risk of CBD stones and ERCP before any other imaging examination for patients who are at high risk[67,68]. Others recommend MRCP for patients with a high or moderate risk for CBD stones and ERCP for patients in whom stones have been depicted by other imaging modalities[69].
MRCP has recently been developed as a noninvasive, yet highly sensitive, method for diagnosing diseases of the biliary tract. One meta-analysis that included 15 studies concluded that the sensitivity of MRCP for diagnosis of choledocholithiasis ranged from 0.5 to 1.0, while specificity ranged from 0.83 to 1.0[37]. Another systematic review including five RCTs showed that the aggregated sensitivity and specificity of MRCP for the detection of choledocholithiasis were 0.85 and 0.93, respectively[38]. In this review, we provide high-quality systematic evidence for MRCP as a predictor of choledocholithiasis, demonstrating high sensitivity and specificity for predicting CBD stones with high overall accuracy.
DOR is an indicator of test accuracy that combines sensitivity and specificity data into a single number[70]. The DOR is the ratio of the odds of positive test results in patients with disease relative to the odds of positive test results in patients without disease. The value of a DOR ranges from 0 to infinity, with higher values indicating better discriminatory test performance (higher accuracy). A DOR of 1.0 indicates that a test does not discriminate between patients with the disorder and those without it. Thus, higher DOR values indicate better discriminatory test performance. The mean DOR in our study was 143.82, indicating a high level of overall accuracy.
The SROC curve and DOR are difficult to interpret and relate to clinical practice, whereas likelihood ratios are more clinically meaningful[71], therefore, we also calculated PLRs and NLRs to assess diagnostic accuracy. Likelihood ratios of > 10.0 or < 0.1 indicate high accuracy. The overall PLR value in our meta-analysis indicates that patients with CBD stones have an approximately 13-fold higher chance of being positive for MRCP detection compared with patients without choledocholithiasis. This high probability is considered sufficient to begin or continue ERCP/IOC treatment of choledocholithiasis patients. In contrast, the NLR value in our meta-analysis indicates that a patient without choledocholithiasis would still have a 13% chance of having CBD stones, which is insufficient to rule out choledocholithiasis. These findings suggest that a negative MRCP detection result should not be used alone as a justification to deny or discontinue CBD stone therapy. A better approach may be a combined diagnostic strategy drawing on clinical information as well as findings from clinical symptoms, ERCP, EUS, and/or serum bilirubin, alkaline phosphatase, aspartate aminotransferase, and alanine aminotransferase levels.
An exploration of the reasons for heterogeneity rather than the computation of a single summary measure is an important goal of meta-analyses[72]. In our study, both STARD and QUADAS scores were used in the meta-regression analysis to assess the effect of study quality on RDOR. Most of the studies were high quality (STARD score ≥ 13 or QUADAS score ≥ 10). We found that there was no statistical heterogeneity for sensitivity, specificity, PLR, NLR, or DOR among the studies, which indicates that the differences for studies with or without blinded, cross-sectional, consecutive/random and prospective designs did not reach statistical significance, and the study design did not substantially affect diagnostic accuracy.
The present meta-analysis had several limitations. First, the exclusion of conference abstracts, letters to editors, and non-English-language studies may have led to publication bias, although our bias analysis suggests that this was not a significant problem. Second, nonrandom misclassification bias may have occurred due to the fact that different studies used various approaches to diagnose choledocholithiasis, including ERCP, IOC and/or EUS. Third, we did not identify multicenter and large, blinded RCTs that satisfied our inclusion criteria.
In conclusion, MRCP is a noninvasive investigation with fewer complications and it has high sensitivity, specificity and positive and negative predictive values for detection of CBD stones. We propose MRCP as the best method of choice for suspected cases of CBD stones, instead of ERCP, IOC and EUS, because of its high diagnostic accuracy and excellent features with technical versatility, multiplanar capability, and noninvasive nature.
COMMENTS
Background
Endoscopic retrograde cholangiopancreatography (ERCP) is applied both as a diagnostic and therapeutic tool. However, ERCP has significant morbidity of l%-7% and mortality of 0.2%-1.0%. Unlike ERCP, magnetic resonance cholangiopancreatography (MRCP) is noninvasive, can be performed rapidly, and does not expose the patients to ionizing radiation or iodinated contrast materials, which is useful for evaluating biliopancreatic disease. Moreover, MRCP has demonstrated good results for detecting common bile duct (CBD) stones. However, the selective use of MRCP in clinically equivocal situations has not been explored until now.
Research frontiers
MRCP is a noninvasive method for diagnosing choledocholithiasis. The selective use of MRCP in clinically equivocal situations has not been explored until now.
Innovations and breakthroughs
This study is believed to be the first rigorous evaluation of the effectiveness of MRCP for detection of CBD stones in patients with suspected choledocholithiasis, using a meta-analysis.
Applications
MRCP should be the method of choice for suspected cases of CBD stones because of its technical versatility, multiplanar capability, and noninvasive nature.
Peer-review
This is a very interesting and useful paper. The manuscript is well written and the method for statistical evaluation is properly used. In the clinical situation, it is sometimes difficult to correctly detect small stones or sludge as well as multiple stones by MRCP.
Footnotes
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 7, 2014
First decision: August 15, 2014
Article in press: October 15, 2014
P- Reviewer: Cardinale V, Kikuyama M, Tan HJ, Yagi H S- Editor: Gou SX L- Editor: AmEditor E- Editor: Ma S
References
- 1.Mitchell SA, Jacyna MR, Chadwick S. Common bile duct stones: a controversy revisited. Br J Surg. 1993;80:759–760. doi: 10.1002/bjs.1800800635. [DOI] [PubMed] [Google Scholar]
- 2.Del Santo P, Kazarian KK, Rogers JF, Bevins PA, Hall JR. Prediction of operative cholangiography in patients undergoing elective cholecystectomy with routine liver function chemistries. Surgery. 1985;98:7–11. [PubMed] [Google Scholar]
- 3.Varghese JC, Liddell RP, Farrell MA, Murray FE, Osborne H, Lee MJ. The diagnostic accuracy of magnetic resonance cholangiopancreatography and ultrasound compared with direct cholangiography in the detection of choledocholithiasis. Clin Radiol. 1999;54:604–614. doi: 10.1016/s0009-9260(99)90023-5. [DOI] [PubMed] [Google Scholar]
- 4.Montariol T, Msika S, Charlier A, Rey C, Bataille N, Hay JM, Lacaine F, Fingerhut A. Diagnosis of asymptomatic common bile duct stones: preoperative endoscopic ultrasonography versus intraoperative cholangiography--a multicenter, prospective controlled study. French Associations for Surgical Research. Surgery. 1998;124:6–13. [PubMed] [Google Scholar]
- 5.Demartines N, Eisner L, Schnabel K, Fried R, Zuber M, Harder F. Evaluation of magnetic resonance cholangiography in the management of bile duct stones. Arch Surg. 2000;135:148–152. doi: 10.1001/archsurg.135.2.148. [DOI] [PubMed] [Google Scholar]
- 6.Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1–10. doi: 10.1016/s0016-5107(98)70121-x. [DOI] [PubMed] [Google Scholar]
- 7.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 8.Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423. doi: 10.1111/j.1572-0241.2001.03594.x. [DOI] [PubMed] [Google Scholar]
- 9.Sherman S, Ruffolo TA, Hawes RH, Lehman GA. Complications of endoscopic sphincterotomy. A prospective series with emphasis on the increased risk associated with sphincter of Oddi dysfunction and nondilated bile ducts. Gastroenterology. 1991;101:1068–1075. [PubMed] [Google Scholar]
- 10.Amouyal P, Amouyal G, Lévy P, Tuzet S, Palazzo L, Vilgrain V, Gayet B, Belghiti J, Fékété F, Bernades P. Diagnosis of choledocholithiasis by endoscopic ultrasonography. Gastroenterology. 1994;106:1062–1067. doi: 10.1016/0016-5085(94)90768-4. [DOI] [PubMed] [Google Scholar]
- 11.Palazzo L, Girollet PP, Salmeron M, Silvain C, Roseau G, Canard JM, Chaussade S, Couturier D, Paolaggi JA. Value of endoscopic ultrasonography in the diagnosis of common bile duct stones: comparison with surgical exploration and ERCP. Gastrointest Endosc. 1995;42:225–231. doi: 10.1016/s0016-5107(95)70096-x. [DOI] [PubMed] [Google Scholar]
- 12.Shim CS, Joo JH, Park CW, Kim YS, Lee JS, Lee MS, Hwang SG. Effectiveness of endoscopic ultrasonography in the diagnosis of choledocholithiasis prior to laparoscopic cholecystectomy. Endoscopy. 1995;27:428–432. doi: 10.1055/s-2007-1005735. [DOI] [PubMed] [Google Scholar]
- 13.Sugiyama M, Atomi Y. Endoscopic ultrasonography for diagnosing choledocholithiasis: a prospective comparative study with ultrasonography and computed tomography. Gastrointest Endosc. 1997;45:143–146. doi: 10.1016/s0016-5107(97)70237-2. [DOI] [PubMed] [Google Scholar]
- 14.Brisbois D, Plomteux O, Nchimi A, Hock D, Dupont P, Delforge M, Bastens B, Weerts J, Magotteaux P. [Value of MRCP for detection of choledocholithiasis in symptomatic patients: one-year experience with a standardized high resolution breath-hold technique] JBR-BTR. 2001;84:258–261. [PubMed] [Google Scholar]
- 15.Sperlongano P, Pisaniello D, Del Viscovo L, De Falco M, Parmeggiani D, Piatto A, Parmeggiani U. Efficacy of magnetic resonance cholangiopancreatography in detecting common bile duct lithiasis: our experience. Chir Ital. 2005;57:635–640. [PubMed] [Google Scholar]
- 16.Chan YL, Chan AC, Lam WW, Lee DW, Chung SS, Sung JJ, Cheung HS, Li AK, Metreweli C. Choledocholithiasis: comparison of MR cholangiography and endoscopic retrograde cholangiography. Radiology. 1996;200:85–89. doi: 10.1148/radiology.200.1.8657949. [DOI] [PubMed] [Google Scholar]
- 17.Prat F, Amouyal G, Amouyal P, Pelletier G, Fritsch J, Choury AD, Buffet C, Etienne JP. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis. Lancet. 1996;347:75–79. doi: 10.1016/s0140-6736(96)90208-1. [DOI] [PubMed] [Google Scholar]
- 18.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. The Standards for Reporting of Diagnostic Accuracy Group. Croat Med J. 2003;44:635–638. [PubMed] [Google Scholar]
- 19.Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Devillé WL, Buntinx F, Bouter LM, Montori VM, de Vet HC, van der Windt DA, Bezemer PD. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2002;2:9. doi: 10.1186/1471-2288-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lau J, Ioannidis JP, Balk EM, Milch C, Terrin N, Chew PW, Salem D. Diagnosing acute cardiac ischemia in the emergency department: a systematic review of the accuracy and clinical effect of current technologies. Ann Emerg Med. 2001;37:453–460. doi: 10.1067/mem.2001.114903. [DOI] [PubMed] [Google Scholar]
- 22.Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med. 1993;12:1293–1316. doi: 10.1002/sim.4780121403. [DOI] [PubMed] [Google Scholar]
- 23.Irwig L, Tosteson AN, Gatsonis C, Lau J, Colditz G, Chalmers TC, Mosteller F. Guidelines for meta-analyses evaluating diagnostic tests. Ann Intern Med. 1994;120:667–676. doi: 10.7326/0003-4819-120-8-199404150-00008. [DOI] [PubMed] [Google Scholar]
- 24.Vamvakas EC. Meta-analyses of studies of the diagnostic accuracy of laboratory tests: a review of the concepts and methods. Arch Pathol Lab Med. 1998;122:675–686. [PubMed] [Google Scholar]
- 25.Suzuki S, Moro-oka T, Choudhry NK. The conditional relative odds ratio provided less biased results for comparing diagnostic test accuracy in meta-analyses. J Clin Epidemiol. 2004;57:461–469. doi: 10.1016/j.jclinepi.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 26.Westwood ME, Whiting PF, Kleijnen J. How does study quality affect the results of a diagnostic meta-analysis? BMC Med Res Methodol. 2005;5:20. doi: 10.1186/1471-2288-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shamiyeh A, Lindner E, Danis J, Schwarzenlander K, Wayand W. Short- versus long-sequence MRI cholangiography for the preoperative imaging of the common bile duct in patients with cholecystolithiasis. Surg Endosc. 2005;19:1130–1134. doi: 10.1007/s00464-004-2167-6. [DOI] [PubMed] [Google Scholar]
- 29.Anderson SW, Rho E, Soto JA. Detection of biliary duct narrowing and choledocholithiasis: accuracy of portal venous phase multidetector CT. Radiology. 2008;247:418–427. doi: 10.1148/radiol.2472070473. [DOI] [PubMed] [Google Scholar]
- 30.McMahon CJ. The relative roles of magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound in diagnosis of common bile duct calculi: a critically appraised topic. Abdom Imaging. 2008;33:6–9. doi: 10.1007/s00261-007-9304-3. [DOI] [PubMed] [Google Scholar]
- 31.Chang JH, Lee IS, Lim YS, Jung SH, Paik CN, Kim HK, Kim TH, Kim CW, Han SW, Choi MG, et al. Role of magnetic resonance cholangiopancreatography for choledocholithiasis: analysis of patients with negative MRCP. Scand J Gastroenterol. 2012;47:217–224. doi: 10.3109/00365521.2011.638394. [DOI] [PubMed] [Google Scholar]
- 32.Epelboym I, Winner M, Allendorf JD. MRCP is not a cost-effective strategy in the management of silent common bile duct stones. J Gastrointest Surg. 2013;17:863–871. doi: 10.1007/s11605-013-2179-4. [DOI] [PubMed] [Google Scholar]
- 33.Richard F, Boustany M, Britt LD. Accuracy of magnetic resonance cholangiopancreatography for diagnosing stones in the common bile duct in patients with abnormal intraoperative cholangiograms. Am J Surg. 2013;205:371–373. doi: 10.1016/j.amjsurg.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 34.Kim HJ, Park DI, Park JH, Cho YK, Sohn CI, Jeon WK, Kim BI, Kim SK. Multidetector computed tomography cholangiography with multiplanar reformation for the assessment of patients with biliary obstruction. J Gastroenterol Hepatol. 2007;22:400–405. doi: 10.1111/j.1440-1746.2006.04503.x. [DOI] [PubMed] [Google Scholar]
- 35.Wong HP, Chiu YL, Shiu BH, Ho LC. Preoperative MRCP to detect choledocholithiasis in acute calculous cholecystitis. J Hepatobiliary Pancreat Sci. 2012;19:458–464. doi: 10.1007/s00534-011-0456-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhat M, Romagnuolo J, da Silveira E, Reinhold C, Valois E, Martel M, Barkun JS, Barkun AN. Randomised clinical trial: MRCP-first vs. ERCP-first approach in patients with suspected biliary obstruction due to bile duct stones. Aliment Pharmacol Ther. 2013;38:1045–1053. doi: 10.1111/apt.12481. [DOI] [PubMed] [Google Scholar]
- 37.Kaltenthaler EC, Walters SJ, Chilcott J, Blakeborough A, Vergel YB, Thomas S. MRCP compared to diagnostic ERCP for diagnosis when biliary obstruction is suspected: a systematic review. BMC Med Imaging. 2006;6:9. doi: 10.1186/1471-2342-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Verma D, Kapadia A, Eisen GM, Adler DG. EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006;64:248–254. doi: 10.1016/j.gie.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 39.Chen Y. Diagnosis of common bile duct stones before ERCP: An analysis of 238 cases. Shijie Huaren Xiaohua Zazhi. 2013;21:1811. [Google Scholar]
- 40.Lindsell DR. The diagnostic accuracy of magnetic resonance cholangiopancreatography (MRCP) and ultrasound compared with direct cholangiography in the detection of choledocholithiasis. Clin Radiol. 2000;55:579. doi: 10.1053/crad.1999.0426. [DOI] [PubMed] [Google Scholar]
- 41.Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, Francis IR, Nandi PS. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. Am J Gastroenterol. 2001;96:2900–2904. doi: 10.1111/j.1572-0241.2001.04245.x. [DOI] [PubMed] [Google Scholar]
- 42.Hochwald SN, Dobryansky M BA, Rofsky NM, Naik KS, Shamamian P, Coppa G, Marcus SG. Magnetic resonance cholangiopancreatography accurately predicts the presence or absence of choledocholithiasis. J Gastrointest Surg. 1998;2:573–579. doi: 10.1016/s1091-255x(98)80059-0. [DOI] [PubMed] [Google Scholar]
- 43.Boraschi P, Neri E, Braccini G, Gigoni R, Caramella D, Perri G, Bartolozzi C. Choledocolithiasis: diagnostic accuracy of MR cholangiopancreatography. Three-year experience. Magn Reson Imaging. 1999;17:1245–1253. doi: 10.1016/s0730-725x(99)00075-2. [DOI] [PubMed] [Google Scholar]
- 44.de Lédinghen V, Lecesne R, Raymond JM, Gense V, Amouretti M, Drouillard J, Couzigou P, Silvain C. Diagnosis of choledocholithiasis: EUS or magnetic resonance cholangiography? A prospective controlled study. Gastrointest Endosc. 1999;49:26–31. doi: 10.1016/s0016-5107(99)70441-4. [DOI] [PubMed] [Google Scholar]
- 45.Lomas DJ, Bearcroft PW, Gimson AE. MR cholangiopancreatography: prospective comparison of a breath-hold 2D projection technique with diagnostic ERCP. Eur Radiol. 1999;9:1411–1417. doi: 10.1007/s003300050859. [DOI] [PubMed] [Google Scholar]
- 46.Varghese JC, Farrell MA, Courtney G, Osborne H, Murray FE, Lee MJ. A prospective comparison of magnetic resonance cholangiopancreatography with endoscopic retrograde cholangiopancreatography in the evaluation of patients with suspected biliary tract disease. Clin Radiol. 1999;54:513–520. doi: 10.1016/s0009-9260(99)90848-6. [DOI] [PubMed] [Google Scholar]
- 47.Stiris MG, Tennøe B, Aadland E, Lunde OC. MR cholangiopancreaticography and endoscopic retrograde cholangiopancreaticography in patients with suspected common bile duct stones. Acta Radiol. 2000;41:269–272. doi: 10.1080/028418500127345226. [DOI] [PubMed] [Google Scholar]
- 48.Taylor AC, Little AF, Hennessy OF, Banting SW, Smith PJ, Desmond PV. Prospective assessment of magnetic resonance cholangiopancreatography for noninvasive imaging of the biliary tree. Gastrointest Endosc. 2002;55:17–22. doi: 10.1067/mge.2002.120324. [DOI] [PubMed] [Google Scholar]
- 49.Topal B, Van de Moortel M, Fieuws S, Vanbeckevoort D, Van Steenbergen W, Aerts R, Penninckx F. The value of magnetic resonance cholangiopancreatography in predicting common bile duct stones in patients with gallstone disease. Br J Surg. 2003;90:42–47. doi: 10.1002/bjs.4025. [DOI] [PubMed] [Google Scholar]
- 50.Kejriwal R, Liang J, Anderson G, Hill A. Magnetic resonance imaging of the common bile duct to exclude choledocholithiasis. ANZ J Surg. 2004;74:619–621. doi: 10.1111/j.1445-1433.2004.03114.x. [DOI] [PubMed] [Google Scholar]
- 51.Simone M, Mutter D, Rubino F, Dutson E, Roy C, Soler L, Marescaux J. Three-dimensional virtual cholangioscopy: a reliable tool for the diagnosis of common bile duct stones. Ann Surg. 2004;240:82–88. doi: 10.1097/01.sla.0000129493.22157.b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dalton SJ, Balupuri S, Guest J. Routine magnetic resonance cholangiopancreatography and intra-operative cholangiogram in the evaluation of common bile duct stones. Ann R Coll Surg Engl. 2005;87:469–470. doi: 10.1308/003588405X51137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hallal AH, Amortegui JD, Jeroukhimov IM, Casillas J, Schulman CI, Manning RJ, Habib FA, Lopez PP, Cohn SM, Sleeman D. Magnetic resonance cholangiopancreatography accurately detects common bile duct stones in resolving gallstone pancreatitis. J Am Coll Surg. 2005;200:869–875. doi: 10.1016/j.jamcollsurg.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 54.Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, Yamamoto N, Hirano K, Komatsu Y, Tada M, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005;54:271–275. doi: 10.1016/j.ejrad.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 55.Moon JH, Cho YD, Cha SW, Cheon YK, Ahn HC, Kim YS, Kim YS, Lee JS, Lee MS, Lee HK, et al. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005;100:1051–1057. doi: 10.1111/j.1572-0241.2005.41057.x. [DOI] [PubMed] [Google Scholar]
- 56.Okada M, Fukada J, Toya K, Ito R, Ohashi T, Yorozu A. The value of drip infusion cholangiography using multidetector-row helical CT in patients with choledocholithiasis. Eur Radiol. 2005;15:2140–2145. doi: 10.1007/s00330-005-2820-z. [DOI] [PubMed] [Google Scholar]
- 57.Shanmugam V, Beattie GC, Yule SR, Reid W, Loudon MA. Is magnetic resonance cholangiopancreatography the new gold standard in biliary imaging? Br J Radiol. 2005;78:888–893. doi: 10.1259/bjr/51075444. [DOI] [PubMed] [Google Scholar]
- 58.De Waele E, Op de Beeck B, De Waele B, Delvaux G. Magnetic resonance cholangiopancreatography in the preoperative assessment of patients with biliary pancreatitis. Pancreatology. 2007;7:347–351. doi: 10.1159/000107269. [DOI] [PubMed] [Google Scholar]
- 59.Schmidt S, Chevallier P, Novellas S, Gelsi E, Vanbiervliet G, Tran A, Schnyder P, Bruneton JN. Choledocholithiasis: repetitive thick-slab single-shot projection magnetic resonance cholangiopancreaticography versus endoscopic ultrasonography. Eur Radiol. 2007;17:241–250. doi: 10.1007/s00330-006-0380-5. [DOI] [PubMed] [Google Scholar]
- 60.Hekimoglu K, Ustundag Y, Dusak A, Erdem Z, Karademir B, Aydemir S, Gundogdu S. MRCP vs. ERCP in the evaluation of biliary pathologies: review of current literature. J Dig Dis. 2008;9:162–169. doi: 10.1111/j.1751-2980.2008.00339.x. [DOI] [PubMed] [Google Scholar]
- 61.Nandalur KR, Hussain HK, Weadock WJ, Wamsteker EJ, Johnson TD, Khan AS, D’Amico AR, Ford MK, Nandalur SR, Chenevert TL. Possible biliary disease: diagnostic performance of high-spatial-resolution isotropic 3D T2-weighted MRCP. Radiology. 2008;249:883–890. doi: 10.1148/radiol.2493080389. [DOI] [PubMed] [Google Scholar]
- 62.Norero E, Norero B, Huete A, Pimentel F, Cruz F, Ibáñez L, Martínez J, Jarufe N. [Accuracy of magnetic resonance cholangiopancreatography for the diagnosis of common bile duct stones] Rev Med Chil. 2008;136:600–605. [PubMed] [Google Scholar]
- 63.Srinivasa S, Sammour T, McEntee B, Davis N, Hill AG. Selective use of magnetic resonance cholangiopancreatography in clinical practice may miss choledocholithiasis in gallstone pancreatitis. Can J Surg. 2010;53:403–407. [PMC free article] [PubMed] [Google Scholar]
- 64.Bilgin M, Toprak H, Burgazli M, Bilgin SS, Chasan R, Erdogan A, Balcı C. Diagnostic value of dynamic contrast-enhanced magnetic resonance imaging in the evaluation of the biliary obstruction. ScientificWorldJournal. 2012;2012:731089. doi: 10.1100/2012/731089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang ZY, Wang D, Ni JM, Yu XR, Zhang L, Wu WJ, Gong L, Hu MH. Comparison of three-dimensional negative-contrast CT cholangiopancreatography with three-dimensional MR cholangiopancreatography for the diagnosis of obstructive biliary diseases. Eur J Radiol. 2012;81:830–837. doi: 10.1016/j.ejrad.2011.02.036. [DOI] [PubMed] [Google Scholar]
- 66.Mandelia A, Gupta AK, Verma DK, Sharma S. The Value of Magnetic Resonance Cholangio-Pancreatography (MRCP) in the Detection of Choledocholithiasis. J Clin Diagn Res. 2013;7:1941–1945. doi: 10.7860/JCDR/2013/6158.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dwerryhouse SJ, Brown E, Vipond MN. Prospective evaluation of magnetic resonance cholangiography to detect common bile duct stones before laparoscopic cholecystectomy. Br J Surg. 1998;85:1364–1366. doi: 10.1046/j.1365-2168.1998.00957.x. [DOI] [PubMed] [Google Scholar]
- 68.Liu TH, Consorti ET, Kawashima A, Ernst RD, Black CT, Greger PH, Fischer RP, Mercer DW. The efficacy of magnetic resonance cholangiography for the evaluation of patients with suspected choledocholithiasis before laparoscopic cholecystectomy. Am J Surg. 1999;178:480–484. doi: 10.1016/s0002-9610(99)00224-x. [DOI] [PubMed] [Google Scholar]
- 69.Zidi SH, Prat F, Le Guen O, Rondeau Y, Rocher L, Fritsch J, Choury AD, Pelletier G. Use of magnetic resonance cholangiography in the diagnosis of choledocholithiasis: prospective comparison with a reference imaging method. Gut. 1999;44:118–122. doi: 10.1136/gut.44.1.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129–1135. doi: 10.1016/s0895-4356(03)00177-x. [DOI] [PubMed] [Google Scholar]
- 71.Deeks JJ. Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ. 2001;323:157–162. doi: 10.1136/bmj.323.7305.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med. 2001;20:3625–3633. doi: 10.1002/sim.1091. [DOI] [PubMed] [Google Scholar]


